Abstract
Aim
The aim of this study was to determine whether computer assisted surgery (CAS) can provide a more accurate, reproducible technique to achieve equal leg lengths in total hip arthroplasty (THA) and to compare the clinical outcome with conventional on table judgement of leg lengths in unilateral total hip replacement.
Methods
A collective review of the literature was undertaken utilizing applicable databases. Research criteria were the following: (1) Developing and developed country studies, (2) level II, III, IV and V studies, (3) human subjects only, (4) period of study from 1996 to 2017 - English text only. The identified publications were assessed for their relevance and methodology and 20 articles were selected.
Results
The overall evaluation of the results demonstrates that CAS provides a more accurate reproduction of limb length in THA compared to conventional freehand THA. Short to medium-term studies have demonstrated no benefit in clinical outcome scores. There is a high degree of correlation between measurements provided by CAS intraoperatively and radiographic measurements postoperatively.
Conclusion
CAS provides a more accurate, reproducible technique to achieve limb length equality in THA compared to conventional freehand THA, however more intensive long-term studies are required to establish the effect on implant longevity and revision surgery rates in the two groups.
Keywords: Computer assisted surgery, Computer navigated surgery, Total hip arthroplasty, Leg length correction, Leg length discrepancy
1. Introduction
The burden of degenerative hip disease in our population has increased dramatically in recent years and total hip arthroplasty (THA) is one of the most successful orthopaedic procedures performed to alleviate pain, improve motion and increase patient quality of life. Leg length discrepancy (LLD) is a common cause of patient dissatisfaction following total hip arthroplasty (THA) and one of the leading causes of litigation in orthopaedic practice.1 A LLD of less than 1 cm is generally well tolerated and in order to achieve this consistently, one needs to be familiar with the various surgical techniques and the accuracy of each one in clinical practice. Achieving equal leg lengths is often dependent on a careful preoperative assessment of the patient, and utilizing a reproducible technique to translate the preoperative plan into a good clinical result. Many techniques are described in the literature, and computer assisted surgery (CAS) is one of the more novel approaches which has piqued interest in orthopaedic hip arthroplasty in recent years.
The main objectives of THA are pain relief, hip stability and mobility, equal leg lengths and implant longevity. Implant longevity is directly related to the accuracy of positioning of the various components during surgery and the reproduction of normal hip biomechanics to prevent excessive wear of the implant. CAS is currently not utilized in mainstream orthopaedic practice due to the high initial setup costs and the increased surgical time required. In addition, it has a steep learning curve, and requires that the surgeon is familiar with the freehand technique in the event of computer malfunction.2,3
A collective review of the literature was performed to determine whether CAS provides a more accurate reproduction of limb length equality compared with conventional freehand technique and whether this has an impact on clinical outcome scores in the short to medium-term.
2. Materials and methods
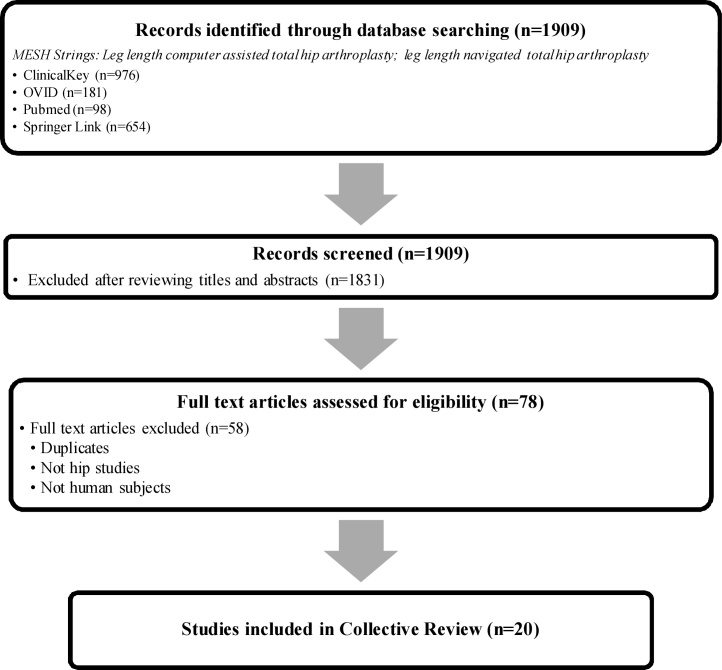
A collective review of the literature was undertaken utilizing applicable databases viz. ClinicalKey, OVID, Pubmed and Springer Link. Research criteria were the following: (1) Developing and developed country studies, (2) level II, III, IV and V studies, (3) human subjects only, (4) period of study from 1996 to 2017 - English text only. The search strategy is presented below (Fig. 1).
Fig. 1.
Flow chart of the study selection and inclusion process.
The following Medical Subject Heading (MeSH) terms were used: “Leg length computer assisted total hip arthroplasty”; “Leg length navigated total hip arthroplasty”. 1909 Search results were obtained, which identified 79 relevant publications. The identified publications were assessed for their relevance and methodology and 20 articles were selected. Published literature of level II, III, IV and V human studies were included from the year 1996 to 2017. The contents of featured articles were appraised qualitatively with regards to CAS used as well as quantitatively regarding limb lengths achieved and clinical outcomes using standardized scoring systems.
3. Workflow to achieve equal leg lengths using CAS
According to Wasterlain et al.4 CAS has the potential to improve the accuracy and reproducibility of implant positioning in THA. CAS can be performed using two different techniques viz. imageless and image-based (CT, MRI or intra-operative Fluoroscopy). These systems register anatomical landmarks with sensors that are placed on the patient intraoperatively to translate the patient data onto a 3D computer model which is displayed on a high definition computer monitor. CT-based systems allow visualization of a patient-specific model whereas imageless systems rely on a generic simulated model.4
The first step in the registration process is to define the anterior pelvic plane, by attaching an optical tracking array (static reference frame) to the patient’s iliac crest, usually with a Steinmann pin. The femoral reference plane is determined by probing anatomical landmarks such as the greater trochanter, patella and femoral condyles. The accuracy of the navigation system relies on the surgeons ability to accurately define these planes.2,4,5 To calculate the 3D relationship between the implants and the patient’s anatomy, the surgeon controls instruments which have an optical tracking array attached to them (dynamic reference frames). The interaction between the static reference frame, and the dynamic reference frames is what allows the surgeon to adjust the leg length, femoral offset, inclination angle and anteversion of the cup with dynamic live values displayed on a computer monitor.2,4 The definition of outliers varies in the literature from a LLD > 5 mm to a LLD > 10 mm.6, 7, 8, 9, 10, 11
4. Results
4.1. CAS versus conventional freehand technique
Data was extracted from 14 studies and a synopsis is presented in Table 1. Manzotti et al. performed a matched-pair study and assessed the clinical outcome using the Harris Hip Score (HHS) and Western Ontario and McMaster Universities (WOMAC) Arthritis Index.7 The post-operative LLD in the CAS group was significantly lower and had fewer outliers (10.42%) compared to the freehand group (27.08%).7 Their short term follow up (minimum of 6 months), revealed no statistically significant difference in clinical outcome scores and they advocated a longer follow-up.7
Table 1.
Synopsis of clinical studies.
| Outcome | Leg length change can be well controlled using CAS even when minimally invasive techniques are used | CAS group: less variance in limb-length inequality and less stress shielding of the proximal femur at 5 years. | No significant difference in clinical scores. Less outliers in CAS group. | Ct-based navigation is reliable for leg length adjustment | New Software added to accuracy and reproducibility | No significant difference in clinical scores. No outliers in CAS group. | CAS improves precision of acetabular component and decreases leg length discrepancy. |
|---|---|---|---|---|---|---|---|
| Clinical Scores CAS | JOA 96 ± 5 | HHS 88.87 WOMAC 9.33 | HHS 84.8 | ||||
| Clinical Scores Control | JOA 95 ± 6 | HHS 89.73 WOMAC 13.21 | HHS 84.2 | ||||
| Limb Length CAS (mm) | 1.3 ± 5.3 (−20.3 to 15.3) | 5 ± 3 (0–12) | 5.06 (0–12) >10:5 patients | <6: 15 patients >6: 1 patient | 0.9 (−5–5) <5: 50 patients | 0.3 ± 0.3 | Mean Difference between CAS and Freehand: −4.61 (−7.74 to −1.48) |
| Limb Length Control (mm) | 6 ± 6 (0–29) | 7.64 (0–20) >10:13 patients | 2.9 (−13 to 20) <5: 24 patients >10: 10 patients | 1.8 ± 0.7 | |||
| Follow-up | 5 years | 6 months | No data | 12 months | |||
| Number of Patients | 344 (317 included) | 68 Freehand 75 CAS | 48 Freehand 48 CAS | 30 CAS (16 included) | 50 CAS Old Software 50 CAS New Software | 75 Freehand 75 CAS | 13 Studies: 1071 Hips |
| Control Group | No | Yes | Yes | No | Yes | Yes | |
| Navigation System | Ct-based, Vector Vision, Brainlab | Robodoc, Integrated Surgical Systems | Imageless, Vector Vision, Brainlab | CT based, Stryker CT-Hip System | Imageless, Orthopilot THAPlus | Imageless, Orthosoft Hip, Zimmer | |
| Level of Evidence | Level IV, therapeutic study | Level II, therapeutic study. | Matched-Pair Study | Level IV, therapeutic study | Retrospective Review | Retrospective review | Meta-Analysis of randomized control trials |
| Authors, Year | Ecker et al.20 | Nakamura et al.17 | Manzotti et al.7 | Kitada et al.16 | Nishio et al.8 | Licini et al.12 | Xu et al.9 |
| Outcome | No significant difference in outcome. Significantly longer operating time and blood loss. | Both methods provide acceptable equalization of leg length | Fewer outliers in CAS group. Both techniques recommended | Increased accuracy in acetabulum cup position and limb length. No significant difference in clinical scores. | Substantial agreement between radiographic and Femoral Pinless navigation system. | THA using CAS can accurately restore the hip offset and leg length. | The leg length objective was achieved within ± 5 mm > 80% of cases and within ± 3 mm in 70% of cases. |
|---|---|---|---|---|---|---|---|
| Clinical Scores CAS | HHS 97 | HHS 90.9WOMAC 2.7 | |||||
| Clinical Scores Control | HHS 98 | HHS 90.2WOMAC 2.3 | |||||
| Limb Length CAS (mm) | 5.2 ± 0.4 | 3 ± 2 (0–8) | 1.7 ±0.3 < 5: 54 patients | 2.7 (0-15) | Mean X-ray: +6.3 ±4.7 Mean CAS: +6.7 ± 6 | <6: 146 patients >6: 6 patients | 4 (−28–29) |
| Limb Length Control (mm) | 5.8 ± 0.3 | 2.9 ± 3 (0–10) | 3.5 ±0.2 < 5: 47 patients | 4.4 (0-20) | |||
| Follow-up | Minimum 2.8 years | 0.15–3.5 years | 1 year | ||||
| Number of Patients | 198 Freehand 119 CAS | 40 PCA limb lengthening gauge 30 CAS | 61 Fluoroscopy 55 CAS | 65 Freehand 65 CAS | 50 CAS | 152 CAS | 321 CAS (280 included) |
| Control Group | Yes | Yes | Yes | Yes | No | No | No |
| Navigation System | Imageless, Ci Cas, Depuy | CT-based, Stryker | Imageless, Brainlab | Imageless, Navitrack, Orthosoft | Imageless, Brainlab | Imageless, Orthopilot, Braun | Imageless, THS surgetics, Hiploc, Praxim |
| Level of Evidence | Retrospective Review | Retrospective Review | Prospective Randomized Control Trial | Prospective, Randomized Controlled study | Level IV, therapeutic study | Level IV, therapeutic study | Retrospective Review |
| Authors, Year | Brown et al. 14 | Ogawa et al.19 | Weber et al.11 | Lass et al.13 | Renkawitz et al.15 | Ellapparadja et al.10 | Clavé et al.3 |
A retrospective study by Licini et al. found at a minimum follow-up of 1 year, that CAS was able to restore the leg length more accurately with fewer outliers than the non-navigated group.12 However, this did not translate into a better clinical score (HHS) and the perception of LLD was not diminished in the CAS group.12 They also recommended longer follow-up.
In a prospective randomized study by Lass et al., significant improvement in the HHS and WOMAC index was noted in both groups and no significant difference was found at a minimum follow-up of 1.5 years.13 The authors also investigated the angles of inclination and anteversion of the acetabular component and found significantly more accurate anteversion angles in the navigated group.13 Accurate placement of the acetabular cup using CAS is in keeping with other studies analyzed in a meta-analysis by Xu et al. and aids in the restoration of leg length.9
Brown et al. found no difference in accuracy of components, leg length and clinical outcome(HHS) in their series of patients comparing CAS to freehand technique.14 Their main drawbacks for CAS were increased operative time (average 18 min), increased blood loss (average 69 ml), high financial impact on both the hospital and the patient, and no measureable benefit over conventional THA.14 First generation software was used in their study, and they anticipated evolution of the technology to enable a quicker registration of anatomical landmarks and a more cost-effective solution.14 Nishio et al. reported that new generation software enabled them to achieve a far more accurate reproduction of limb length equality with a LLD <5 mm in 100% of patients versus 48% in the first generation software group.8
4.2. Accuracy of computer navigation in THA
A meta-analysis of randomized controlled trials(RCT) by Xu et al., with a total sample size of 1071 hips, concluded that the use of CAS for THA decreases the LLD postoperatively and improves the accuracy of acetabular component placement by reducing the number of outliers.9 They recommended further high quality RCTs with long term follow-up to confirm their results as their meta-analysis included only 13 articles, many of which had methodological flaws.9
Ellapparadja et al. were able to produce excellent accuracy in their series of 152 hips, whereby they restored the leg length to <6 mm in 94.73% and native hip offset in 95.39% of patients.10 In contrast to the study by Brown et al., they cited minimal cost expenditure and a negligible amount of extra time required in their navigation workflow.10,14
To assess the accuracy of the live computer values for limb length and offset adjustment displayed on-screen intra-operatively, Renkawitz et al. compared these values to the post-operative values measured on plain film radiographs.15 They found a high degree of correlation between the two methods of measurement, and recommended CAS as a technical assistant to the surgeon who performs a thorough pre-operative limb length assessment.15 Kitada et al. in a smaller series of 16 patients found that the measurement error between intra-operative values and post-operative CT values were insignificant (1.3 mm) and 94% of their patients had a post-operative LLD <6 mm.16
Navigation systems, like all other technological advancements, are not immune to failure, and in their series of 321 cases, Clavé et al. reported abandonment of their navigation workflow intra-operatively in 23 cases (7.08%) due to various reasons such as failure to calibrate and movement of the sensor arrays.3 Despite this, they were able to report leg length and offset restoration in 83.3% and 88.7% of patients respectively.3
4.3. Alternative technology
In a prospective randomized trial, Weber et al. were able to achieve accurate results using intra-operative fluoroscopy in minimally invasive (MIS) THA.11 The mean difference between the CAS group and fluoroscopy group was 0.2 mm for leg length, and 1.7 mm for femoral offset, however there were fewer outliers in the CAS group.11 Fluoroscopy serves as a cost-effective solution in centers where navigation systems are not installed, and surgeons are unfamiliar with the CAS workflow.
Nakamura et al. compared a robotic–assisted system with manual rasping of the proximal femur and found less variance in limb length inequality and less stress shielding of the proximal femur at a minimum of 5 years follow up.17 The main disadvantage of the robotic system is the potential injury to the abductor muscles during the robotic-milling procedure, which can lead to gait abnormalities and higher rates of dislocation. They reported a dislocation rate of 5.3% (4 hips) compared to 1.4% (1 hip) in the manual rasping group.17
Intellijoint HIP is a miniaturized 3D optical navigation tool which is currently being used in clinical trials to evaluate the accuracy of this technology in measuring leg length, offset and cup position. In non-clinical trials, it has proven to be an accurate tool, while reducing the added time and cost burden of current navigation systems.18
Ogawa et al.19 studied the accuracy of the PCA limb lengthening gauge (Stryker, USA) and found it to be a reliable cost-effective tool in achieving equal limb lengths.19 Compared to CAS, the only drawback was loosening of the pins on the femoral side in osteoporotic bone, and the position of the limb in abduction and adduction can alter accuracy.19 The CAS group also had fewer outliers which is in keeping with the other studies in this review.7,11, 12, 13,16,19
5. Discussion
The incidence of osteoarthritis (OA) of the hip ranges from 5.9% in adults aged 45–54 to 17% in the elderly population (>75 years).6 Improvement in the management and control of chronic diseases has led to an exponential increase in our geriatric population and patients living with OA of the hip is projected to increase from 21.4 million in 2005 to 41.1 million by 2030.6
The successful outcome of THA is dependent on implant longevity, a good and painless range of movement, stability of the hip, and the experience and skill of the surgeon. Advancements in modern medicine have equipped orthopaedic surgeons with a wide variety of tools to enable precision and accuracy when performing THA. This collective review of the literature has attempted to show that CAS can enable the surgeon to achieve near equal leg lengths, hip offset and acetabular cup position. It is more accurate than the conventional freehand technique and produces results with far fewer outliers.7,11, 12, 13,16,19 These factors are important in ensuring implant longevity, good range of motion, lower dislocation rates and preventing revision hip surgery. LLD following THA can lead to gait disturbances, lower back pain, sciatica, and overall dissatisfaction. The threshold for a successful restoration of limb length ranges from 5 mm–10 mm and is a major concern for the arthroplasty surgeon in an ever-increasing litigious society.
Failed THA due to instability and inaccurate implant positioning places a huge economic burden on the healthcare system. The annual cost estimates in the United States is $2.7 billion per annum for revision THA.6 CAS certainly improves accuracy of THA thereby minimizing the need for revision hip surgery, however it is still prohibitively expensive to install and requires specialized surgeon training.
In order to achieve equal leg lengths using the conventional freehand technique, the surgeon is required to make use of pre-operative templates using plain radiographs, implant specific templates, or digital software. However, this requires the surgeon to have the ability to precisely translate a pre-operative plan into an intra-operative result using spatial orientation. Studies using freehand techniques and mechanical jigs showed that even experienced surgeons had difficulty in achieving a reliable and reproducible implant position.2,5
Clinical outcome scores (HHS, WOMAC index and Japanese orthopaedic association(JOA) score) were evaluated in 5 studies, all of which showed no statistical difference between CAS and control groups at short to medium term follow-up.7,12, 13, 14,17 The period of follow-up varied from 6 months to 5 years and the clinical outcome scores improved significantly in both patient groups in all 5 studies, thus highlighting the high success rate of THA in improving patient quality of life in the short to medium term, even in patients with a LLD outside of the acceptable range.7,12, 13, 14,17 The limitations of the studies by Manzotti et al., Brown et al. and Licini et al. were non-randomization, non-blinded, retrospective analysis and short follow up period.7,12,14 Lass et al. published the largest prospective randomized study comparing imageless CAS with freehand THA, but their follow-up period was also too short to determine if the increased accuracy of CAS will have any long term clinical benefit.13 The longest follow up period of 5 years was by Nakamura et al., however they used the JOA score, which is not validated as an outcome measure despite its wide use in Japan for the past 40 years.17 More intensive RCTs are required, specifically looking at long-term outcome.
Complications of navigation systems intra-operatively include failure to calibrate the CAS station and fracture of the iliac crest, greater trochanter and distal femur when inserting the pins for the sensor arrays. Post-operative CAS complications include fracture at pin sites on the iliac crest or femur, pin site infection, pain at insertion sites, and dislocation of the implant due to failure to restore limb length and stability. Manzotti et al., Lass et al., and Ogawa et al. reported no navigation related complications in their patient studies respectively.7 Clavé et al. reported two patients with an unexplained shortening of 20 mm post CAS, which resulted in revision hip surgery due to instability and 4 patients (0.01%) who complained of pain and discomfort at the pin sites.3 To alleviate the complication of distal femur pin site pain, Renkawitz et al. used a pinless femoral array which was attached to the skin with an adhesive dressing and they reported only two failures (0.04%) whereby the dressing came loose and they had to revert to the manual technique.15 While navigation offers a reliable method to achieve accuracy during THA, it is important to counsel patients on the potential complications and to be able to switch to the conventional freehand technique in the event of computer malfunction.
One of the major limitations of current navigation systems is the increased surgical time required for registration of anatomical landmarks. Theoretically, increased surgical time (range 5.00–19.78 min) can lead to an increase in infection rates and deep venous thrombosis. However, this was not shown in any of the studies in this review.5,7,9,10,14 Brown et al. also reported that CAS was associated with an increase in blood loss, but this did not translate into an increased need for blood transfusion in their patient group.14 There were 3 patients in his study who also developed transient sciatic nerve palsies attributed to the increased surgical time in CAS.14
The prohibitively high cost of navigation hardware ($250,000) and software ($40,000) is one of the primary reasons that this technology has not been adopted widely (1–3% off all THA is performed with CAS).6 It is currently not a cost-friendly option for low volume centers, and Brown et al.14 found no measurable benefit enough to warrant the additional expenditure. Their estimated expenditure per case was $1100 (USD) which included the disposable instruments and increased operative time. In contrast, Ellapparadja et al.10 reported that their only additional cost per case was approximately $40 as the hardware was provided to their institution free of charge.
With the continuous evolution of technology, the data presented in studies performed 5–10 years ago may not accurately reflect the advancements of current computer assisted systems.4 Computer processing power has increased dramatically in the last decade and this improves on the slow and cumbersome software experienced in the first generation systems. As the technology improves, drawbacks such as cost, availability and increased theatre time are likely to be diminished. While CAS did not differ significantly to freehand THA with regards to clinical outcome scores in the short to medium term, it can be assumed that the effects of accurate implant positioning are likely to produce a better clinical result in the long term.
6. Conclusion
In summary, compared to freehand THA, the use of CAS enables the surgeon to achieve a more accurate, reproducible THA with fewer outliers and no significant difference in complication rates. The improved accuracy did not translate into significantly different clinical outcome scores, but more high quality long term studies are required to determine its effect on implant longevity and revision rates.
Conflict of interest
The author declares that there is no conflict of interest and that no financial support was received for this study.
Ethics approval
Exemption of ethics review was granted by our institution’s ethics review board prior to commencement of the study (BREC: EXM515/17).
References
- 1.McWilliams A., Stewart T.D., Grainger A.J., O’Connor P.J., White D., Redmond A. Leg length inequality following total hip replacement. Orthop Trauma. 2011;25(1):37–42. [Google Scholar]
- 2.Deep K., Picard F. (v) Computer assisted navigation in primary total hip arthroplasty. Orthop Trauma. 2014;28(5):309–314. [Google Scholar]
- 3.Clavé A., Sauleau V., Cheval D., Williams T., Lefèvre C., Stindel E. Can computer-assisted surgery help restore leg length and offset during THA? A continuous series of 321 cases. Orthop Traumatol Surg Res. 2015;101(7):791–795. doi: 10.1016/j.otsr.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Wasterlain A.S., Buza J.A., Thakkar S.C., Meere P., Vigdorchik J. Navigation and robotics in total hip arthroplasty. JBJS Rev. 2017;5(2):1. doi: 10.2106/JBJS.RVW.16.00046. [DOI] [PubMed] [Google Scholar]
- 5.Renner L., Janz V., Perka C., Wassilew G.I. What do we get from navigation in primary THA? EFORT Open Rev. 2016;1(5):205–210. doi: 10.1302/2058-5241.1.000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gross A., Muir J.M. Identifying the procedural gap and improved methods for maintaining accuracy during total hip arthroplasty. Med Hypotheses. 2016;94(2016):93–98. doi: 10.1016/j.mehy.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Manzotti A., Cerveri P., De Momi E., Pullen C., Confalonieri N. Does computer-assisted surgery benefit leg length restoration in total hip replacement? Navigation versus conventional freehand. Int Orthop. 2011;35(1):19–24. doi: 10.1007/s00264-009-0903-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishio S., Fukunishi S., Fukui T., Fujihara Y., Yoshiya S. Adjustment of leg length using imageless navigation THA software without a femoral tracker. J Orthop Sci. 2011;16(2):171–176. doi: 10.1007/s00776-011-0038-2. [DOI] [PubMed] [Google Scholar]
- 9.Xu K., Ym Li, Hf Zhang, Cg Wang, Yq Xu, Li Zj. Computer navigation in total hip arthroplasty: a meta-analysis ofrandomized controlled trials. Int J Surg. 2014;12(5):528–533. doi: 10.1016/j.ijsu.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 10.Ellapparadja P., Mahajan V., Deakin A.H., Deep K. Reproduction of hip offset and leg length in navigated total hip arthroplasty: how accurate are we? J Arthroplasty. 2015;30(6):1002–1007. doi: 10.1016/j.arth.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 11.Weber M., Woerner M., Springorum R., Sendtner E., Hapfelmeier A., Grifka J. Fluoroscopy and imageless navigation enable an equivalent reconstruction of leg length and global and femoral offset in THA. Clin Orthop Relat Res. 2014;472(10):3150–3158. doi: 10.1007/s11999-014-3740-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Licini D.J., Burnikel D.J., Meneghini R.M., Ochsner J.L. Comparison of limb-length discrepancy after THA: with and without computer navigation. Orthopedics. 2013;36(5):543–547. doi: 10.3928/01477447-20130426-13. [DOI] [PubMed] [Google Scholar]
- 13.Lass R., Kubista B., Olischar B., Frantal S., Windhager R., Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty. 2014;29(4):786–791. doi: 10.1016/j.arth.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 14.Brown M.L., Reed J.D., Drinkwater C.J. Imageless computer-assisted versus conventional total hip arthroplasty: one surgeon’s initial experience. J Arthroplasty. 2014;29(5):1015–1020. doi: 10.1016/j.arth.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Renkawitz T., Sendtner E., Schuster T., Weber M., Grifka J., Woerner M. Femoral pinless length and offset measurements during computer-assisted, minimally invasive total hip arthroplasty. J Arthroplasty. 2014;29(5):1021–1025. doi: 10.1016/j.arth.2013.09.034. [DOI] [PubMed] [Google Scholar]
- 16.Kitada M., Nakamura N., Iwana D., Kakimoto A., Nishii T., Sugano N. Evaluation of the accuracy of computed tomography-based navigation for femoral stem orientation and leg length discrepancy. J Arthroplasty. 2011;26(5):674–679. doi: 10.1016/j.arth.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura N., Sugano N., Nishii T., Kakimoto A., Miki H. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res. 2010;468(4):1072–1081. doi: 10.1007/s11999-009-1158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paprosky W.G., Muir J.M. Intellijoint HIP: a 3D mini-optical navigation tool for improving intraoperative accuracy during total hip arthroplasty. Med Devices. 2016;9:401–408. doi: 10.2147/MDER.S119161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogawa K., Kabata T., Maeda T., Kajino Y., Tsuchiya H. Accurate leg length measurement in total hip arthroplasty: a comparison of computer navigation and a simple manual measurement device. Clin Orthop Surg. 2014;6(2):153–158. doi: 10.4055/cios.2014.6.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ecker T.M., Tannast M., Murphy S.B. Computed tomography-based surgical navigation for hip arthroplasty. Clin Orthop Relat Res. 2007;465(00):100–105. doi: 10.1097/BLO.0b013e3181591c7d. [DOI] [PubMed] [Google Scholar]