Abstract
Background
Although many studies have evaluated the success of porous tantalum component in primary and revision cementless total knee arthroplasty (TKA) cases, few studies have reported the breakage of porous tantalum monoblock patella component (PTMP). The purpose of this study was to investigate the radiographic outcomes of breakage of PTMP at short-term follow up.
Methods
This was a retrospective study of 49 consecutive knees in 43 patients who underwent TKA surgery between September 2012 and March 2014. Bone marrow contents/tissue volumes (BMC/TV. mg/cm3) were evaluated using 2-dimensional osteomorphometry software with 2D- multi-detector-row computed tomography (2D-MDCT) to measure fixation of the bone-prosthesis interface with patella at 6, 12, and 24 months after surgery. Clinical follow up was obtained by reviewing each patient at orthopedic record.
Results
We experienced a case that resulted in breakage of PTMP without traumatic episode at 26 months after surgery. Relative changes of Bone Mineral Contents per Tissue Volume. (BMC/TV mg/cm3) at ROI. 1 (superior border of the patella) and ROI. 2 (peg of patella) were significantly higher than ROI.3 (inferior border of patella) at 6, 12 and 24 months after surgery (p < 0.001. p < 0.01). Patient with breakage of PTMP has patella baja (Insall- Salvati ratio: 0.72), and the relative change of BMC/TV at ROI.1 and 2 for patients who experienced a breakage of PTMP was higher than any other patients.
Conclusion
The present study revealed that the use of PTMP should be avoided for patients with patella baja.
Abbreviations: TKA, total knee arthroplasty; PTMP, porous tantalum monoblock patella; 2D-MDCT, two-dimensional multi-detector-row computed tomography; BMC/TV, bone mineral contents per tissue volume; BMI, body mass index; UHMWPE, ultra high molecular weight polyethylene); AP, anteroposterior; ROI, regions of interest; CT, computed tomography; BMD, bone mineral density; BV, bone volume; TV, total volume
Keywords: Total knee arthroplasty, Porous tantalum monoblock patella component, Breakage, 2D-multi-detector-row computed tomography
1. Background
Patellofemoral complications continue to be among the most prevalent causes of unsatisfactory results following total knee arthroplasty (TKA)1,2. These account for almost 50% of re-operations for various reasons such as anterior pain, maltracking, component wear, fracture, and loosening1, 2, 3, 4, 5, 6, 7, 8. Prosthetic fixation and failures, including component migration and prosthetic fracture are related to bone mineral density. Bone mineral density continues to decrease 5% per year, for as long as 2 years after TKA9, 10, 11, 12, 13, 14, 15, 16. Stress shieldings are observed under circumstances that the prosthesis of 30 MPa or more of the modulus of elasticity becomes rigidly fixed. Trabecular metal, the material utilized in our study, is characterized to have 1/5 (3–4 Gpa) of the modulus of elasticity that cortical bone has; therefore, stress shieldings are not likely to occur. Followed by the theory “Bone adapts its morphology (density/micro- architecture) in response to the local loading conditions in such a way that a uniform tissue loading is achieved” described by Wolff17, the changes in bone quality parameters of trabecular patterns under Porous tantalum monoblock patella component (PTMP) were assessed. Noyama et al.18 reported that an oriented groove structure for controlling stress distribution was introduced to the proximal medial region of the femoral stem.
There are many dynamic analyses about load distribution after TKA. Computer simulations such as Knee SIM simulates various lower extremity movements such as gait, deep flexion, stepping up and down the stairs, and squats. Also, it is capable of measuring intra-articular kinetics, intra-articular stress, and muscle strength/ligament tension necessary to achieve these series of movement, while users can maneuver parameters to make comparisons of implant locations, ligament location, degree of tension, etc. under the controlled condition. Therefore, with all the reasons above, computer simulation is effective for the discussion of surgical technique. In addition, the contact stress between polyethylene and patella can be understood using Finite Element Analysis (FEA) together with computer simulation19, 20, 21, 22, 23, 24: However, we need to be careful on the interpretation of computer simulation for the dynamic analysis of knee kinematics because this is an analysis “in the computer”.
Recently, intraoperative measurement of tibiofemoral forces using sensor-integrated tibial tray has been taken25, 26, 27, 28; however, subjects in these studies were under anesthesia when manual stress were applied.
PTMP has been introduced as metallic implant material for cementless TKA and increased initial stability and accelerated bone ingrowth29. Thus, PTMP was expected to facilitate the increase in bone mineral density in the bone-prosthesis interface with patella after TKA; however, we experienced a case that resulted in breakage of PTMP without traumatic episode.
To our knowledge, there are no published studies about the breakage of PTMP between the bone internal structure due to load distribution under PTMP using two-dimensional multi-detector-row computed tomography (2D-MDCT). For post-operative TKA patients, our static analyses utilized 2D-MDCT to periodically measure BMC/TV (Bone Mineral Contents per Tissue Volume. mg/cm3) at right underneath PTMP in accordance with component alignment. We measured bone quality (BMC/TV) instead of BMD with useful clinical parameter.
The aim of this study was to investigate the origin of the breakage of PTMP and the bone internal structure around patella component at 6.12 and 24 months after the operation.
2. Methods
2.1. Study design
This was a retrospective study of 49 consecutive knees in 43 patients (20 knees in 18 men, 29 knees in 25 female) who underwent TKA surgery at our institution between September 2012 and March 2014. The mean age at the time of surgery was 79.5 years (range: 55–89 years). The mean body mass index (BMI) was 24.6 (range: 18.2–27.9). All surgeries in this study were performed using PTMP (trabecular metal; Zimmer Inc.Warsaw, Indiana). PTMP has a single fixation lug (interference fit and hexagonal peg) with direct compression molding of UHMWPE (Ultra High Molecular Weight polyethylene) and ease of revision (Fig. 1). Subjects in the present study were approved by the Institutional Review Board of our hospital, and they were informed on the risk of radiation exposure required to implement this study. Inclusion criteria were pre-operative medial osteoarthritis of the knee. Exclusion criteria were preoperative rheumatoid arthritis, lateral knee osteoarthritis, patients with the history of patella dislocation, knee synthesis and/or high tibia osteotomy.
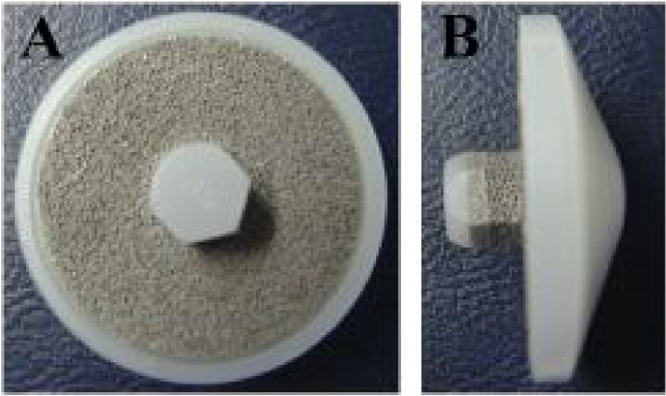
Fig. 1.
Photograph of the cementless porous tantalum monoblock patella component (PTMP: Trabecular Metal; Zimmer Inc.Warsaw, Indiana). Note a single fixation lug (interference fit and hexagonal peg) with direct compression molding of Ultra High Molecular Weight polyethylene. The Advantages are easier revision surgery (A: patella joint facet site. B: lateral view).
2.2. Surgical techniques
In all cases, the TKA surgical procedure was performed by one surgeon (T.K) and was minimally invasive surgery; with a skin incision of 8–11 cm. At first, the distal femoral cutting guide block was aligned using an intra-medullary guide, and the proximal tibia cutting block was aligned using an extramedullary guide. For the femur and tibia, a standard 6° valgus angle guide and 7° posterior inclination guide were used for all patients. The rotational alignment was adjusted to the surgical epi-condylar axis for the femoral component, and medial one third of tibia tuberosity at the level of patellar-tendon attachment for the tibia component. We confirmed the tension and appearance of posterior cruciate ligament. The femoral components were cemented and the tibial components were fixed with cementless porous tantalum modular components and patella components were fixed with cementless PTMP with onlay fixation. All the patients followed the same post-operative rehabilitation protocol.
2.3. Outcome measures
The Knee Society Score (KSS)30 and Hospital for Special Surgery patella score31 were measured by one author (N.K) who was not involved with any of the surgical procedure. The standard standing anteroposterior (AP), lateral, and skyline patellar radiographs were measured for pre- operative and twenty-four months after the operation. Knees were fully extended and located so that the patella was centered between the femoral condyles and facing forward. The Insal-Salvati ratio and posterior condylar offset/patella length ratio were measured on the lateral radiograph. The patellar tilting angle and congruence angle and displacement of patella were measured by drawing a line on the anterior aspect of the femoral condyle and another line along the posterior aspect of the articular surface of the patella32. We took MDCT with Phantom (Taisho-Toyama Pharm. Co, Ltd, Tokyo. Japan) consisting of a cylindrical material that reproduces the bone density of cortical bone on the outer surface, and that of cancellous bone internally to determine the bone volumes at 6, 12, 24 months postoperatively (Fig. 2). From the obtained images, the cancellous trabecular structure was visualized three-dimensionally with 2D-osteo-morphometry software (TRI/2D-BON64; RATOC System Engineering Co., Ltd. Tokyo, Japan), and the structural parameters were calculated. The structural parameters targeted for this analysis were those recommended by the American Society for Bone and Mineral Research: Bone Mineral Contents/Tissue Volume (BMC/TV.mg/cm3) values, representing quantification of bone formation in total volumes, representing mineralized bone volume as a percentage of total volume. In the assessment of BMC/TV values by 2D-MDCT imaging of the PTMP, bone quality (BMC/TV) was measured in regions not affected by the artifact of prosthesis.
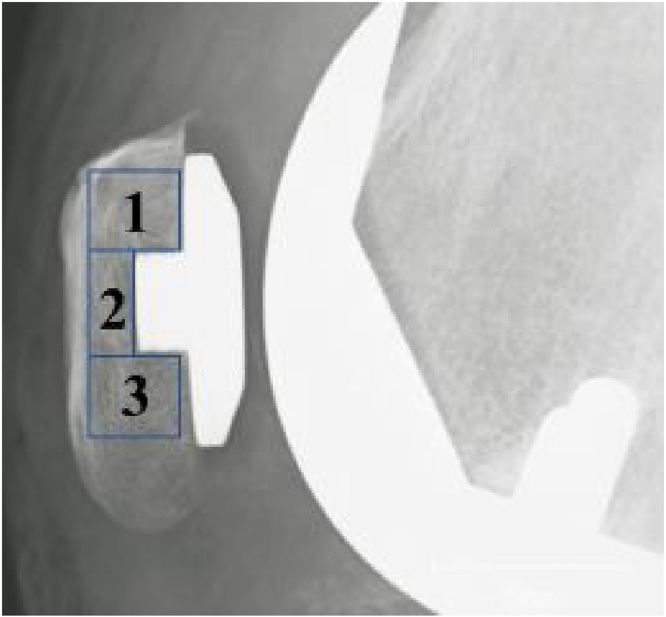
Fig. 2.
We took MDCT with Phantom (Taisho-Toyama Pharm. Co, Ltd, Tokyo. Japan) consisting of a cylinder composed of a material corresponding to cortical bone and filled with a material having a bone density corresponding to cancellous bone for determination of the bone volumes at postoperatively at 6.12 and 24 months after surgery.
The overall region was divided into 3 regions of interest (ROIs): ROI 1: superior border of the patella, ROI 2: peg of patella, ROI 3: inferior border of patella (Fig. 3). The relative change of the BMC/TV in Region 1–3 was defined as the ratio of change in bone formation at 6, 12 and 24 months after surgery.
Fig. 3.
Region of interest (Region)1 (superior border of the patella) is 1 cm distal to the superior of PTMP within anterior cortex of the patella, (Region)2 (peg of patella) is 0.5 cm distal to the peg of PTMP within anterior cortex of the patella, (Region)3 (inferior border of the patella) is 1 cm distal to the inferior of PTMP within anterior cortex of the patella.
2.4. Statistics
Statistical analysis was performed using SPSS software (SPSS version 17.0 software: SPSS, Chicago, IL, USA). The nonparametric data were presented as median (interquartile range) and the Mann- Whitney U test was used for analysis, while parametric data were presented as mean (standard deviation) and the Student’s t-test was used for analysis. Statistical significance was defined as p < 0.05.
3. Results
The mean Knee Society scores and function scores and Hospital for Special Surgery patella scores were significantly improved at the final follow-up examination (24 months post-operatively). The mean ranges of motion, both extension and flexion were significantly improved postoperatively (Table 1). No joint infection was detected during the follow-up period. At skyline patellar views, type 2 (41knees) was the most common in wyberg classification (type 1: 5knees. type 3: 3knees) and the mean sulcus angle was 133.4 ± 4.6°, pre-operatively. At lateral views, the mean Insall-Salvati ratio was 1.1 ± 0.13 (6 knees in 3 men. 3 women with patella alta, 1 knee in men with patella baja), pre-operatively. There were no cases of hypoplasia on the femoral groove. The tilting angle, congruence angle and patellar displacement were significantly improved at the last follow-up examination (p < 0.05: Table 2). The mean posterior condylar offset/patella length ratios were significantly decreased postoperatively, however, there were no cases of the anterior knee pain and reduction in flexion angle. The mean condylar twist angle was 3.7 ± 0.7° at axial plane with computed tomography (CT) image, and there were no patient with malrotation of femoral component.
Table 1.
Pre-operative and postoperative Knee Society scores and Hospital for Special Surgery. Patella Scores and knee range of motion.
| Variables | Pre-operative | Final follow-up | P |
|---|---|---|---|
| Knee Society knee score (Point) | 38 ± 4 | 94 ± 2 | <0.01* |
| Knee Society function score (Point) | 37 ± 2 | 81 ± 1 | <0.01* |
| Hospital for Special Surgery | 18 ± 3 | 27 ± 2 | <0.01* |
| Patella Score (Point) | |||
| Range of motion (ROM) | 102 ± 21 | 118 ± 22 | <0.01* |
| Extension angle (°) | −9 ± 8 | −1 ± 3 | <0.01* |
| Flexion angle (°) | 110 ± 19 | 119 ± 21 | <0.01* |
Data are presented as Mean and standard deviation.
Statistically significant P < 0.05.
Table 2.
Pre-operative and postoperative Tilting angle, Congruence angle and Patellar displacement.
| Variables | Pre-operative | Final follow-up | P |
|---|---|---|---|
| Tilting angle (°) | 5.10 ± 3.3 | 3.0 ± 1.7 | <0.05* |
| Congruence angle (°) | −2.7 ± 1.4 | 0.7 ± 2.1 | <0.05* |
| Patellar displacement(mm) | 1.772 ± 3.51 | 0.1 ± 1.6 | <0.05* |
Data are presented as Mean and standard deviation.
Statistically significant P < 0.05.
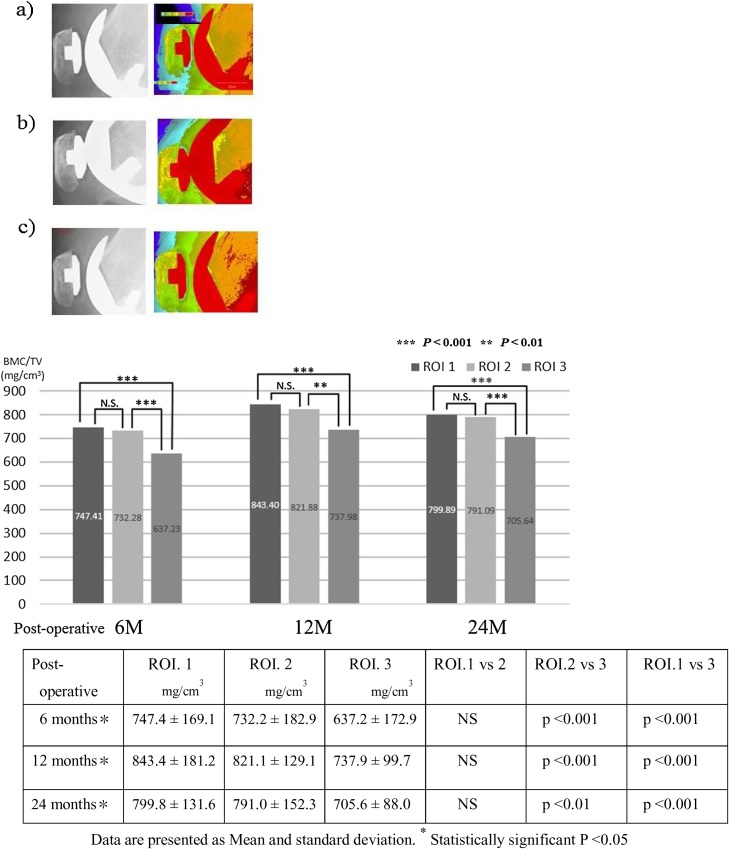
No significant differences were observed in the relative change of BMC/TV in between ROI. 1 and 2 groups at all follow-up examination. The relative change of BMC/TV in ROI. 1 and 2 were significant higher than ROI.3 at 6, 12 and 24 months after surgery (p < 0.001. p < 0.01. Fig. 4).
Fig. 4.
The cancellous trabecular structure were visualized with 2D-MDCT osteomorphometry lateral images. No significant difference was observed in the relative change of BMC/TV in ROI. 1 and 2 between two groups at all follow-up examination. However, the relative change of BMC/TV in ROI. 1 and 2 were significant higher than ROI.3 at 6, 12 and 12 months after surgery (p < 0.001. p < 0.01.
(a) 6 months post-operatively.
(b) 12 months post-operatively.
(c) 24 months post-operatively.
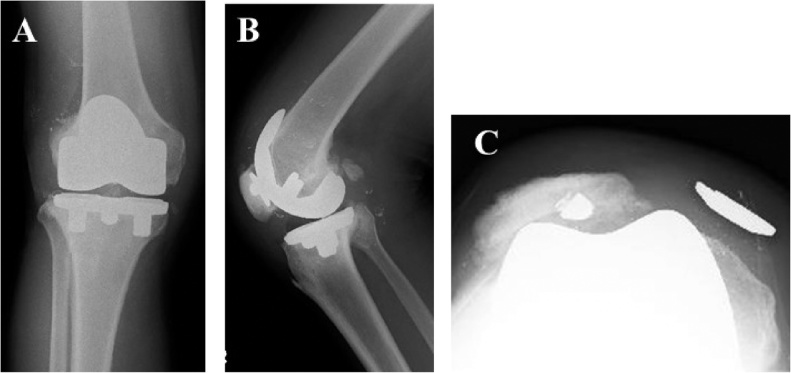
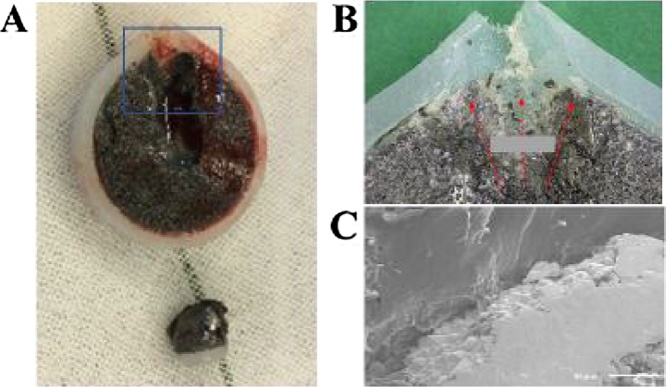
One patient (57-year-old. male. body mass index, 23.1 kg/m2) without traumatic episode underwent revision surgery due to breakage at the bottom of peg of PTMP at 26 months after surgery (Fig. 5). At revision surgery, metallosis within soft tissues in supra patellar pouch were recognized (Fig. 6), then we resurfaced using cemented patella component with onlay fixation. The relative change of BMC/TV in ROI.1.2 of patient who took breakage of PTMP was higher than any other patients at 6, 12 and 24 months after surgery (Table 3) and it was the only patient that exhibited patella baja (Insall- Salvati ratio: 0.72) in the present study. The origin of damage was observed in direction towards the upper edge of the surface of patella by Scanning electron microscopy (SEM S-4800; Hitachi, Chiba. Japan) (Fig. 7).
Fig. 5.
(A) Anterior-posterior, (B) lateral and (C) skyline views.
Radiographs of a 57-year-old male (Insall- Salvati ratio: 0.72) showing breakage at the bottom of peg of PTMP at 26 months after surgery. Scattered metal particles around femoral component.
Fig. 6.
Photograph showing the metellosis in supra patellar pouch at revision surgery.
Table 3.
The relative change of BMC/TV in ROI.1.2 of patient (57-year-old. male) who took breakage of PTMP was higher than any other patients at 6, 12 and 24 months after surgery.
| Post-operative | ROI. 1 mg/cm3 | ROI. 2 mg/cm3 | ROI. 3 2 mg/cm3 |
|---|---|---|---|
| 6 months | 924.1 | 938.6 | 492.2 |
| 12 months | 970.8 | 1043.4 | 666.4 |
| 24 months | 903.3 | 920.9 | 583.8 |
Fig. 7.
Photograph showing (A) the breakage of PTMP (B) Macro (enlarged) view (c) Scanning electron microscopy. The origin of damage was observed in direction of the upper edge of the surface of patella. Crack fracture surface along grain boundary was observed without corrosion.
4. Discussion
The most important finding of the present study was that patients showed excellent clinical results at least until 24 months after surgery. At 26 months after surgery, however, a breakage of PTMP of patella was found (2%), which required a revision surgery with cemented patella component. The relative change of BMC/TV in ROI. 1and 2 were significantly higher than ROI.3 at 6, 12 and 24 months after surgery. Especially the patient with patella baja showed the highest relative changes in ROI.1 and 2. In scanning electron microscopy, the damage of PTMP was confirmed the load distribution in direction towards the upper edge of the surface of patella component. The present study revealed that the use of PTMP for patients with patella baja may lead to breakage of PTMP.
It is well known that bone mineral density (BMD) only partly explains bone strength. However future osteoporosis can be better predicted with bone microstructure analysis than BMD measurement alone33. 2D and 3-MDCT has been demonstrated to be the first device to be able to non-destructively “reveal “trabecular architecture and is an x-ray based technique that provides 2D-3 images of very high isotropic spatial resolution33, 34, 35, 36, 37, 38. Most metric parameters, such a bone volume (BV), total volume (TV), one volume fraction (BV/TV), bone mineral contents (BMC), and tissue volumes (TV) are directly determined38.
Some investigations have been reported using the same 2D or 3-osteo-morphometry software (TRI/2D or 3-BON 64). Wang et al. revealed significant bone loss of trabecular bone in femur under unloading conditions by dissecting the sciatic nerve39. Kuroshima et al.40 reported that the optimal design of grooves on the neck of dental implants improve bone quality parameters. Prior study evaluating the porous tantalum cementless TKA implant have primarily focused on the PTMP. Unger et al.41 retrospectively reviewed 95 patients with 108 TKAs at an average of 4.5 years follow-up and found that 90 TKAs used the cementless metal backed patella. Among these patients with the metal-backed patellar component, 1 required open reduction internal fixation for a patellar fracture sustained from a fall, 2 patients were noted to have anterior knee pain with patellar component aseptic loosening, and another patient had revision of the patella due to an oblique bony cut resulting in patellar mal-tracking. Successful outcomes were also reported by Kwong et al.42 in their series of 117 PTMP, which noted no radiographic evidence of component loosening and no revisions due to aseptic loosening at an average of 7 years, while Jeremy et al.43 reported that they found the breakage of PTMP rate of at least 20% at over 5 years follow-up. Compared with the normal PTMP group, the cohort with breakage of PTMP were noted to be significantly taller with a mean height of 72.5 in. compared with 69.8 in.
We revealed that the changes in the form and the function of a bone are followed by changes in its internal structure with load distribution, therefore the load distribution concentrated on superior and central border of PTMP. The breakage of PTMP was recognized by load distribution from the center of PTMP to upward. We confirmed that use of PTMP should be avoided for patients with patella baja.
The present study had several limitations that should be considered. First, this study was retrospective study without the patient being randomized. Additional research is required to determine the long-term benefits of PTMP. Second, the population of this study was relatively small for short term follow up. Despite these limitations, data of excellent short terms results for the PTMP were provided, but patients with patella baja should be used cemented patella instead of PTMP to avoid breakage of PTMP. A long-term follow-up will be necessary to verify the very long-term advantages of the PTMP.
5. Conclusion
In conclusion, the present study presented a minimun 2% rate for the breakage of PTMP at short term follow-up. We should avoid using PTMP for patients with patella baja.
Ethics approval and consent to participate
This study followed the Declaration of Helsinki and was approved by the ethics committee of Toho University School of Medicine, Japan.
Consent for publication
Not applicable.
Availability of data and materials
The detasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
The study was not funded.
Authors’ contributions
TK and NK designed the study. YM helped in the data curation. MH carried out the formal analysis. HI supervised the study. TK wrote, reviewed, and edited the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Hiroaki Suzuki, Eriko Kuroiwa and Nobuhito Nango for their assistance in this study.
Contributor Information
Takao Kaneko, Email: takao-knee@oha.toho-u.ac.jp.
Norihiko Kono, Email: banzai.nippon@hotmail.co.jp.
Yuta Mochizuki, Email: yuta.mochizuki@med.toho-u.ac.jp.
Hiroyasu Ikegami, Email: hiroyasu.ikegami@med.toho-u.ac.jp.
Yoshiro Musha, Email: musha@oha.toho-u.ac.jp.
References
- 1.Chew J.T., Stewart N.J., Hanssen A.D., Luo Z.P., Rand J.A., An K.N. Differences in patellar tracking and knee kinematics among three different total knee designs. Clin Orthop Relat Res. 1997;345:87–98. [PubMed] [Google Scholar]
- 2.Berger R.A., Lyon J.H., Jacobs J.J., Barden R.M., Berkson E.M., Sheinkop M.B. Problems with cementless total knee arthroplasty. Clin Orthop Relat Res. 2001;392:196–207. doi: 10.1097/00003086-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Ritter M.A., Pierce M.J., Zhou H., Meding J.B., Faris P.M., Keating E.M. Patellar complications (total knee arthroplasty). Effect of lateral release and thickness. Clin Orthop Relat Res. 1999;367:149–157. [PubMed] [Google Scholar]
- 4.Barrack R.L., Burak C. Patella in total knee arthroplasty. Clin Orthop Relat Res. 2001;389:62–73. doi: 10.1097/00003086-200108000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Berger R.A., Crossett L.S., Jacobs J.J., Rubash H.E. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Dennis D.A. Patellofemoral complications in total knee arthroplasty. Am J Knee Surg. 1992;5:156–166. [Google Scholar]
- 7.Harwin S.F. Patellofemoral complications in symmetrical total knee arthroplasty. J Arthroplasty. 1998;13:753–762. doi: 10.1016/s0883-5403(98)90026-2. [DOI] [PubMed] [Google Scholar]
- 8.Moreland J.R. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988;226:49–64. [PubMed] [Google Scholar]
- 9.Furnes O., Espehaug B., Lie S.A., Vollset S.E., Engesaeter L.B., Havelin L.I. Early failures among 7174 primary total knee replacements: a follow up study from the Norwegian arthroplasty register 1994–2000. Acta Orthop Scand. 2002;73:117–129. doi: 10.1080/000164702753671678. [DOI] [PubMed] [Google Scholar]
- 10.Levine B.R., Della Valle C.J., Jacobs J.J. Applications of porous tantalum in total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:646–655. doi: 10.5435/00124635-200611000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Martino I.D., D’Apolito R., Sculco P.K., Poultsides L.A., Gasparini G. Total knee arthroplasty using cementless porous tantalum monoblock tibial component: a minimum 10-year follow-up. J Arthroplasty. 2016;31:2193–2198. doi: 10.1016/j.arth.2016.03.057. [DOI] [PubMed] [Google Scholar]
- 12.Kamath A.F., Lee G.C., Sheth N.P., Nelson C.L., Garino J.P., Israelite C.L. Prospective results of un-cemented tantalum mono-block tibia in total knee arthroplasty: minimum 5-year follow-up in patient younger than 55 years. J Arthroplasty. 2011;26(8):1390–1395. doi: 10.1016/j.arth.2011.06.030. [DOI] [PubMed] [Google Scholar]
- 13.Niemelainen M., Skytta E.T., Remes V., Makela K., Eskelinen A. Total knee arthroplasty with an un-cemented trabecular metal tibia component: a registry-based analysis. J Arthroplasty. 2014;29(1):57–60. doi: 10.1016/j.arth.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Pulido L., Abdel M.P., Lewallen D.G. The Mark Coventry Award: trabecular metal tibial components were durable and reliable in primary total knee arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2015;473(1):34. doi: 10.1007/s11999-014-3585-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Martino I., De Santis V., Sculco P.K., D’Apolito R., Assini J.B., Gasparini G. Tantalum cones provide durable midterm fixation in revision TKA. Clin Orthop Relat Res. 2015;473(10):3176. doi: 10.1007/s11999-015-4338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamath A.F., Lewallen D.G., Hanssen A.D. Porous tantalum metaphyseal cones for severe tibial bone loss in revision knee arthroplasty: a five to nine-year follow-up. J Bone Jt Surg Am. 2015;97(3):216. doi: 10.2106/JBJS.N.00540. [DOI] [PubMed] [Google Scholar]
- 17.Wolff J. 1892. Das Gaetz der Transformation, Transformation der Knochen. Hirschwald, Berlin. [Google Scholar]
- 18.Noyama Y., Nakano T., Ishimoto T., Sakai T., Yoshikawa H. Design and optimization of the oriented groove on the hip implant surface to promote bone microstructure integrity. Bone. 2013;52:659–667. doi: 10.1016/j.bone.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Victor J., Bellemans J. Physiologic kinematics as a concept for better flexion in TKA. Clini Orthop Relat Res. 2006;452:53–58. doi: 10.1097/01.blo.0000238792.36725.1e. [DOI] [PubMed] [Google Scholar]
- 20.D’Lima D.D., Patil S., Steklov N., Colwell C.W., Jr. The 2011 ABJS Nicolas Andry Award: ‘lab’-in-a-knee: in vivo knee forces, kinematics, and contact analysis. Clini Orthop Relat Res. 2011;469(10):2953–2970. doi: 10.1007/s11999-011-1916-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colwell C.W., Jr., Chen P.C., D’Lima D.D. Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating-bearing. Clin Biomech. 2011;26(1):52–57. doi: 10.1016/j.clinbiomech.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 22.Mizu-uchi H., Colwell C.W., Jr., Matsuda S., Flores-Hernandez C., Iwamoto Y., D’Lima D.D. Effect of total knee arthroplasty implant position on flexion angle before implant-bone impingement. J Arthroplasty. 2011;26(5):721–727. doi: 10.1016/j.arth.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 23.Kuriyama S., Ishikawa M., Furu M., Ito H., Matsuda S. Malrotated tibial component increases medial collateral ligament tension in total knee arthroplasty. J Orthop Res. 2014;32(2):1658–1666. doi: 10.1002/jor.22711. [DOI] [PubMed] [Google Scholar]
- 24.Nakamura S., Tanaka Y., Kuriyama S. Superior-inferior position of patella component affects patellofemoral kinematics and contact forces in computer simulation. Clin Biomech. 2017;45:19–24. doi: 10.1016/j.clinbiomech.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 25.Gustke K.A., Golladay G.J., Roche M.W., Elson L.C., Anderson C.R. A new method for defining balance: promosing short-term clinical outcomes od sensor-guided TKA. J Arthroplasty. 2014;29(5):955–960. doi: 10.1016/j.arth.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 26.Gustke K.A., Golladay G.J., Roche M.W., Jerry G.J., Elson L.C., Anderson C.R. Increased satisfaction after total knee replacement using sensor-guided technology. Bone Jt J. 2014;96-B(10):1333–1338. doi: 10.1302/0301-620X.96B10.34068. [DOI] [PubMed] [Google Scholar]
- 27.Nodzo S.R., Franceschini V., Gonzalez Della Valle A. Intraoperative load-sensing variability during cemented, posterior-stabilized total knee arthroplasty. J Arthroplasty. 2017;32(1):66–70. doi: 10.1016/j.arth.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 28.Manning W.A., Ghosh K., Blain A., Longstaff L., Deehan D.J. Tibiofemoral forces for the native and post-arthroplasty knee: relationship to maximal laxity through a functional arc of motion. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1669–1677. doi: 10.1007/s00167-016-4093-2. [DOI] [PubMed] [Google Scholar]
- 29.Lachiewicz P.F., Bolognesi M.P., Henderson R.A., Soileau E.S., Vail T.P. Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res. 2012;470(1):199. doi: 10.1007/s11999-011-1888-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Insall J., Dorr L.D., Scott R.D., Scott W.N. Rationale of the knee soiety clinical rating system. Clini Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 31.Fellar J.A., Bartlett R.J., Lang D.M. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Jt Surg Br. 1996;78-B:226–228. [PubMed] [Google Scholar]
- 32.Chan K.C., Gill G.S. Postoperative tilt in total knee arthroplasty. J Arthroplasty. 1999;14(3):300. doi: 10.1016/s0883-5403(99)90055-4. [DOI] [PubMed] [Google Scholar]
- 33.Ito M., Ikeda K., Nishiguchi M., Uetani M., Hosoi T., Orimo H. Multi-detector row imaging of vertebral microstructure for evaluation of fracture risk. J Bone Miner Res. 2005;20(10):1828–1836. doi: 10.1359/JBMR.050610. [DOI] [PubMed] [Google Scholar]
- 34.Kaneko T., Otani T., Kono N. Weekly injection of teriparatide for bone ingrowth after cementless total knee arthroplasty. J Orthop Surg (Hong Kong) 2016;2481:16–21. doi: 10.1177/230949901602400106. [DOI] [PubMed] [Google Scholar]
- 35.Inoue K., Hamano T., Nango N. Mulitidetector-row computed tomography is useful to evaluate the therapeutiv effects of bisphosphonates in glucocorticoid-induced osteoporposis. J Bone Miner Metab. 2014;32(3):271–280. doi: 10.1007/s00774-013-0485-2. [DOI] [PubMed] [Google Scholar]
- 36.Okazaki N., Chiba K., Taguchi K. Trabecular microfractures in the femoral head with osteoporosis: analysis of microcallus formations by synchrotron radiation micro CT. Bone. 2014;64:82–87. doi: 10.1016/j.bone.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 37.Iwamoto J., Seki A., Nango N. Influence of teriparatide and ibandronate on cortical bone in New Zealand white rabbits: a HR-QCT study. Calci Tissue Int. 2016;99(5):535–542. doi: 10.1007/s00223-016-0180-0. [DOI] [PubMed] [Google Scholar]
- 38.Ito M. Recent progress in bone imaging for osteoporosis research. J Bone Miner Metab. 2011;29(2):131–140. doi: 10.1007/s00774-010-0258-0. [DOI] [PubMed] [Google Scholar]
- 39.Wang J., Ishimoto T., Nakano T. Unloading-induced degradation of the anisotropic arrangement of collagen/apatite in rat femurs. Carcified Tissue Int. 2017;100:87–94. doi: 10.1007/s00223-016-0200-0. [DOI] [PubMed] [Google Scholar]
- 40.Kuroshima S., Nakano T., Ishimoto T. Optimally oriented grooves on dental implants improve bone quality around implants under repetitive mechanical loading. Acta Biomater. 2017;48:433–444. doi: 10.1016/j.actbio.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 41.Unger A.S., Duggan J.P. Midterm results of a porous tantalum monoblock tibia comoment clinical and radiographic results of 108 knees. J Arthroplasty. 2011;26:855–860. doi: 10.1016/j.arth.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 42.Kwong L.M., Nielsen E.S., Ruiz D.R., Hsu A.H., Dines M.D., Mellano C.M. Cementless total knee replacement fixation: a contemporary durable solution- affirms. Bone Jt J. 2014;96-B(11 Supple A):87–92. doi: 10.1302/0301-620X.96B11.34327. [DOI] [PubMed] [Google Scholar]
- 43.Jeremy Y.C., Nicholas J.G. Uncemented mtal-bcked tantalum patellar components in total knee arthroplasty have a high fracture rate at midterm follow-up. J Arthroplasty. 2017;32:2427–2430. doi: 10.1016/j.arth.2017.02.062. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The detasets used and/or analysed during the current study are available from the corresponding author on reasonable request.