Abstract
The purpose of this study was to compare clinical outcomes and retear rate between arthroscopic double row (DR) and suture bridge (SB) repair for rotator cuff tears. Postoperative Constant score and MRI findings were compared between 52 patients underwent DR repair and 63 patients underwent SB repair with medium tear of the supraspinatus. There was no significant difference in Constant score between the two groups. Postoperative MRI revealed that retear rate of SB group was significantly lower than DR group. This study suggests that SB repair can provide better clinical and structural outcomes compared with DR repair.
Level of evidence: Level Ⅳ, Case series, Treatment study
Keywords: Rotator cuff tear, Retear, Double row repair, Suture bridge repair, Repair integrity
1. Introduction
Arthroscopic rotator cuff repair (ARCR) is widely known in general as a surgical method that can deliver good improvement of pain and functional recovery. A variety of ARCR methods are performed due to the development and modification of the suture anchor, and reports are available on the successes of these treatment methods. In the early days, single row (SR) repair using suture anchors, was reported to have generally good clinical results, but a high rate of retear or non-healing of the rotator cuff was observed, because of a restricted area of contact with the footprint of the rotator cuff.13 In comparison with SR repair, a significant decline in the rate of retear was observed with double row (DR) repair, which is assumed to have a larger area of contact with the rotator cuff footprint,4, 14 but no difference in clinical outcomes has been reported.10, 11 In recent years, suture bridge (SB) repair has been devised as a transosseous-equivalent method, and it has been reported that we can expect less retear and non-healing from this treatment method.7 According to biomechanical researches of SB repair, the area of its contact with the footprint at the edge of a rotator cuff tear is approximately two times larger than that of DR repair, and its contact pressure has also been reported to be approximately 30% higher. Moreover, SB repair is significantly higher with regard to load to failure as well; furthermore, stress and distortion during shoulder motion are distributed among the anchors, and it has been reported that the distribution of stress is uniform among the anchors, especially during external rotation.15 Therefore, SB repair is considered to be a method capable of delivering good tendon-bone healing, due to its strong initial rigidity, and contact pressure and area. Many reports have been made about good clinical results obtained from ARCR through SB repair. Also, with regard to retear, it has been reported that SB repair has significantly lower retear compared to SR repair. Several reports have seen that the clinical results of SB repair are equivalent to those of SR repair and DR repair, and that its rate of retear is equivalent or slightly lower, but opinion is divided with regard to the correlation between repair integrity and clinical results.12, 17
Meanwhile, age, diabetes mellitus, smoking, size of cuff tear, atrophy and fatty infiltration of muscle have been cited as factors that affect healing process after rotator cuff repair.1, 2, 3 In assessments of postoperative results and retear that have been included in previous reports, not enough factors influencing retear have been excluded, and therefore we believe these reports are not sufficient to compare treatment results by repair methods.
The purpose of this study was to compare the clinical results of two arthroscopic repair procedures (DR and SB repair) with respect to rotator cuff tears of equal size, excluding factors that influence healing, based on the hypothesis that SB repair can achieve better postoperative clinical results and repair integrity.
2. Materials and methods
2.1. Patient selection
This retrospective study was approved by the ethics committee at our hospital, and consent was obtained from all patients for the research. We reviewed a database of all arthroscopic rotator cuff repairs performed by a single surgeon between 2006 and 2013. From among patients in which direct repair was performed in a primary rotator cuff surgery, we sorted patients according to various factors in order to conduct a strict examination of retear according to repair methods. Regarding age, patients were under 70 years of age. Regarding the size of rotator cuff tears, we selected only medium tear of the supraspinatus tendon with a width from 1.5 to 2.0 cm by intraoperative findings, and only those patients that were grade 2 or lower for fatty infiltration according to the Goutallier’s classification8 which were evaluated by MRI scan before surgery. We excluded cases that had a history of steroid injection, smoking, diabetes mellitus, long head of the biceps (LHB) tear, or tear of the subscapularis tendon, which could affect healing process and become risk factors for retearing.
2.2. Patient assessment
We made regular observations from the preoperative period until the final follow-up. In the range of motion of the shoulder joint, we examined active and passive abduction, flexion, external rotation, and internal rotation. We used the Constant score to evaluate clinical results. We also investigated intraoperative and postoperative complications.
2.3. Surgical procedure
Surgery was performed under general anesthesia in the lateral position. Diagnostic arthroscopy was performed on the glenohumeral joint, and a check was performed for intra-articular lesions, including the labrum and LHB. Next, the arthroscope was placed in the subacromial bursa, and pathological synovial bursa were excised to ensure better visibility. A rotator cuff tear was checked and observed for area, size, and delamination. The repair design was determined by conducting release and mobilization of the cuff. The footprint was prepared by removing the soft tissue and conducting bone abrasion. Subacromial decompression was performed in all cases.
The method of cuff repair, according to the DR method, used Corkscrew metal anchors (4.5 mm, double-loaded) (Arthrex, Naples, FL, USA) as both medial and lateral row anchors. One medial row anchor was inserted precisely on the border of the lateral cartilage of the humeral head, and two sutures were secured on the cuff so that each would create a horizontal mattress configuration. A simple suture was performed with two anchors inserted on the lateral row, and four threads secured at the edge of the cuff tear. After tying the sutures of the lateral row anchors, the sutures of the medial row anchors were tied. For the SB method, Corkscrew metal anchors (4.5 mm, double-loaded) (Arthrex) were used as medial row anchors, and Versalok metal anchors (Depuy-Mitek, Warsaw, IN, USA) were used as lateral anchors. One medial row anchor was inserted precisely on the border of the lateral cartilage of the humeral head, and two sutures were secured on the cuff so that each would create a horizontal mattress configuration. Then, two different ends were drawn to the lateral portal, and while adjusting tension on the tendon tissue, they were fixed on a lateral anchor approximately 1 cm distal from the lateral border of the greater tuberosity. The remaining suture threads were drawn to the lateral portal, and they were likewise fixed to a lateral anchor while making adjustments so that there would be no slack in the thread, and so that the tension on the tendon tissue would not be excessive. When the SB repair was first begun, the suture threads of the medial anchor were made into mattress sutures on the cuff, but the medial mattress sutures were not performed in patients after 2011 when medial cuff failure was a concern.
2.4. Postoperative rehabilitation
After surgery, immobilization was provided for three weeks for the both groups, with a shoulder abduction brace. The rehabilitation program began from the second postoperative day, with the patient supported by a physiotherapist to begin bowing and pendulum exercises, and passive range of motion exercise (ROMex). In the second week, the abduction pillow was removed, and assisted-active ROMex. Active ROMex was permitted from the third week. From the eighth week, a program was provided to start functional exercise of the rotator cuff and muscular strengthening around the shoulder girdle. A complete return to occupation and daily activity, including lifting heavy objects, was permitted beginning three months after surgery. For a return to sports, improvement of range of motion and muscular strength was evaluated on an individual basis, and permitted some time later more than three months after surgery.
2.5. Assessment of repair integrity
Evaluation of the postoperative repair integrity of the rotator cuff was conducted by MRI. MRI was performed with a 1.5 T scanner (GE Healthcare). Repair integrity was classified according to the five stages of the Sugaya’s classification,13 using the sagittal section, coronal section, and transverse section of T2-weighted images. Types 4 and 5 according to Sugaya’s classification were considered as retear or non-healing. Following Cho et al5 with regard to the pattern of retear, they were classified as “retracted type,” in which no residual cuff tissue could be observed at the footprint of the greater tuberosity; or as “medial failure type,” in which cuff tissue remained at the footprint of the greater tuberosity, but retear had occurred at the medial musculotendinous junction.
2.6. Statistical analysis
For statistical analysis, IBM SPSS Statistics 21 (IBM Japan, Tokyo, Japan) was used as software. The Mann-Whitney U test was used to compare differences between the two groups. Pre- and postoperative Constant scores were examined by the paired t-test, and postoperative cuff integrity was compared by the chi-square test. P value less than 5% was considered to be a significant difference.
3. Results
3.1. Patient demographics
115 patients of a full-thickness cuff tear that matched the criteria were examined. According to the method of ARCR, there were 52 patients in the DR group, and 63 patients in the SB group (Table 1). No significant difference was observed in terms of age or duration of the symptoms. The postoperative follow-up period was 37.2 (range, 24–88) months on average for the DR group, and 35.1 (range, 26–48) months on average for the SB group. Proportion of history of trauma in the SB group was significantly higher than in the DR group.
Table 1.
Patient Demographics.
| DR group (n = 52) | SB group (n = 63) | P value | |
|---|---|---|---|
| Age at surgery (range) | 61.6 (39–68) | 62.1 (42–69) | 0.06 |
| Female/male | 24/28 | 26/37 | 0.08 |
| History of trauma | 37 | 50 | <0.05 |
| Symptomatic period (months) (range) | 8.4 (1–84) | 8.6 (1–60) | 0.91 |
| Preoperative Constant score (SD) | 63.6 ± 10.8 | 55.9 ± 10.9 | 0.24 |
| Follow-up period (range) | 37.2 (24–88) | 35.1 (26–48) | <0.05 |
DR, double row; SB, suture bridge.
3.2. Clinical outcomes
There were no intra- and postoperative complications such as loosening of suture anchors, infection and neurovascular injuries. No significant difference was observed between the two groups, with the average preoperative Constant score at 63.6 ± 10.8 (range, 41–73) points for the DR group, and 55.9 ± 10.9 (range, 38–76) points for the SB group, whereas the average Constant score at the final follow-up was 89.5 ± 9.8 points (range, 64–100) for the DR group, and 88.4 ± 8.1 (range, 81–100) points for the SB group.
3.3. MRI findings and clinical outcomes
MRI scan was 13.7 (range, 12–24) months after surgery on average. As for postoperative MRI findings according to the Sugaya’s classification, the DR group included 42 patients of types 1 and 2, three patients of type 3, and seven patients of types 4 and 5, whereas the SB group included 57 patients of types 1 and 2, two patients of type 3, and four patients of types 4 and 5. Numbers of type 4 and 5 patients in the SB group were significantly fewer than in the DR group (P < 0.05) (Table 2). In a comparison of clinical results and postoperative MRI findings, the average Constant score for types 1, 2, and 3 was 89.9 ± 3.7 points (range, 84–100) for the DR group and 89.3 ± 4.17.7 (range, 77–100) points for the SB group, whereas the average Constant score for types 4 and 5 in retear patients was 89.4 ± 3.6 (range, 85–100) points for the DR group and 86.7 ± 7.7 (range, 64–100) points for the SB group. Patients with retear and non-healing in the SB group showed a tendency for lower postoperative Constant score, but no significant difference was observed between retear and repair methods.
Table 2.
Repair Integrity by Postoperative MRI (Sugaya classification).
| Type 1 | Type 2 | Type 3 | Type 4 | Type 5 | |
|---|---|---|---|---|---|
| DR group (n = 52) | 25 | 17 | 3 | 5 | 2 |
| SB group (n = 63) | 34 | 23 | 2 | 1 | 3 |
DR, double row; SB, suture bridge.
Numbers of type 4 and 5 patients in the SB group were significantly fewer than in the DR group (P < 0.05).
3.4. Retear pattern
In a comparison of the patterns of retear and non-healing, among seven retear patients in the DR group, retracted type which did not show healing of the torn cuff at the footprint was demonstrated in six patients, and medial failure type which showed healing of the torn cuff at the footprint in one patient (Fig. 1). Meanwhile, in the SB group, retracted type was in one patient, and medial failure type was in three patients. In retear pattern of the SB group according to suture method, retracted type was observed in one patient and no medial failure type among the 46 patients in which medial mattress suture was not performed, whereas pattern of all three patients with retear was medial failure type in the 17 patients in which medial mattress suture was performed (Table 3).
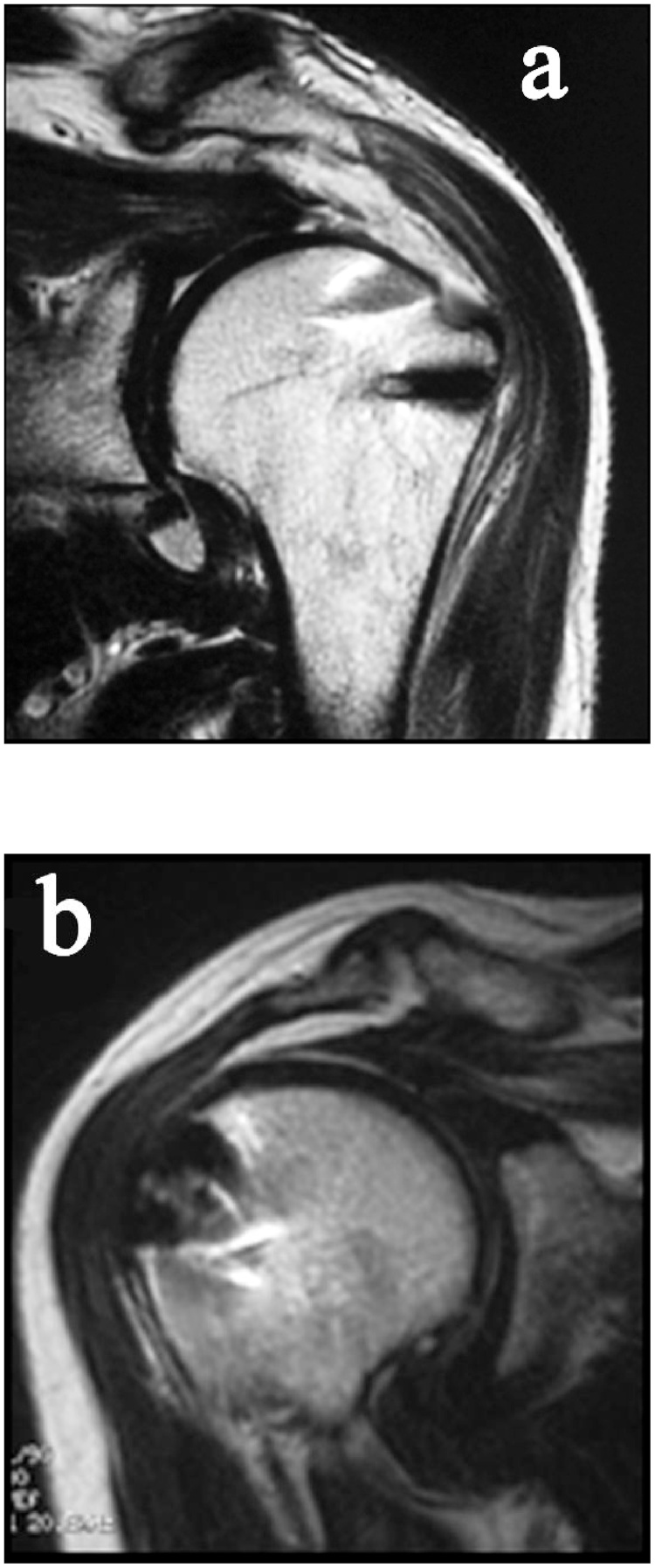
Fig. 1.
Retear Pattern.
Medial failure type (a) showed cuff tissue remained at the footprint of the greater tuberosity, and retear was observed at the medial musculotendinous junction. Retracted type (b) showed no residual cuff tissue at the footprint.
Table 3.
Retear in SB Group with or without Medial Mattress Suture.
Medial suture, threads of the medial anchor were made into horizontal mattress tying on the cuff.
Retear pattern of one patient with type 4 was retracted type.
Retear pattern of three patients with type 5 was medial failure type.
4. Discussion
The aims of surgery on rotator cuff tears are improvement of pain and function, and healing of the torn cuff. In previous reports, even if rotator cuff healing was not obtained, the clinical results were considered to be no different from patients in which there was healing. However, in recent years, patients with intact repair have been reported to improve pain and muscle weakness and to have better clinical results to a significant degree when compared with patients of retear and non-healing.2, 5 Thus, with the objective of achieving reliable healing of a torn cuff, it is natural to select a repair method that can reliably deliver cuff healing. In comparison to the conventional SR and DR repair, the SB repair is a method that can deliver a wider contact area and higher contact pressure of the footprint with the rotator cuff. Thus, the SB repair has become a popular method in recent years, but opinion is divided with regard to cuff integrity after the SB repair, with some reports claiming that it is superior to conventional methods, and some reports claiming that these methods are equivalent.7, 12, 15, 17 Meanwhile, among patient factors, the factors that affect cuff healing include age, smoking habits, diabetes mellitus, and osteoporosis, while factors related to the state of the rotator cuff include tear size, subscapularis tendon rupture, fatty degeneration of muscle, and muscular atrophy; moreover, complications such as LHB tear have also been cited.1, 2, 3, 9, 17
In the present examination, we excluded cases with risk factors for retear and non-healing such as subscapularis tendon tear or smoking; furthermore, we restricted age to under 70 years, and ensured that all tear sizes were the same. Thereby, we were able to conduct a comparative assessment of the superiority or inferiority of rotator cuff healing due to differences between the SB and DR repair. From this, we obtained clinical outcomes from the SB repair that were equivalent to those of the DR repair, and obtained the result that SB repair has a lower rate of retear and more reliable fusion than DR repair in terms of repair integrity.
On the other hand, it is conceivable that the reason that all patients of retear were of the medial failure type under SB repair was caused by a problem in the repair method.5, 17 In the SB repair, the medial mattress sutures have been used as a technique to pressure-bind and fix the rotator cuff to the footprint along the medial row. However, if the suture threads of the suture anchor are passed through the rotator cuff on the medial side, this site becomes damaged and fragile due to penetration by instruments such as the penetrate grasper and suture passer; firmly fastening the suture thread also produces distortion, and there is a risk of provoking a medial cuff tear. Furthermore, friction caused by the sliding of the suture threads also weaken the rotator cuff, increasing the risk of retear.16 In particular, if a suture knot tying is secured to the fragile musculotendinous junction, the risk of producing tear in this area increases. There are also concerns regarding the possibility of stress concentrating on the medial sutured area, and producing knot impingement, during internal and external rotation of the shoulder joint. Medial failure may provoke pain and dysfunction over time, and furthermore, another concern is the occurrence of arthritis changes due to expansion of the torn area. Because it is presumed from postoperative MRI findings that all medial failure occurred due to tear in the medial mattress suture area, the application of medial mattress sutures is a technique to be used with caution in conjunction with the suture bridge method. When performing medial mattress sutures, sutures should be passed the tendon a few millimeters away from the musculotendinous junction, and knot tying should be performed with moderate tension.
In addition, some authors have indicated that blood flow is affected by the compression of the rotator cuff under the SB repair. It was also reported that when the usual SB repair was performed in 18 cases, if the suture threads were bridged outward to be fixed to the lateral anchors, the result of doppler blood flow measurement was that the rate of blood flow in the rotator cuff significantly decreased.6 The application of excessive tension or compression on the rotator cuff is not recommended from the perspective of cuff healing, either.
5. Limitations
This study was retrospective and the surgeries were not randomized, resulting in influence of a learning curve. Moreover, as there were so few cases, it is a limitation that we have not also conducted an examination regarding sports or occupation in each group. Nevertheless, as we can find no other study than our own that has compared repair methods for certain tear size by excluding risk factors of retear, it is useful research that yields suggestions for the selection of repair methods.
6. Conclusion
Herein, we conducted a comparison and assessment of postoperative clinical outcomes and the retear rate between DR and SB repair as methods of ARCR. The postoperative Constant scores of SB repair were equivalent to those of DR repair. The retear rate of SB repair was significantly lower than of DR repair. SB repair provided satisfactory clinical outcomes and cuff healing. Considering that retear pattern of SB repair was only medial failure type, medial mattress sutures may be a technique to be avoided as much as possible in conjunction with SB repair.
Funding
No funds were received for the preparation of this manuscript.
Conflict of interest
The authors have none to declare.
Disclaimer
The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- 1.Bedi A., Fox A.J.S., Harris P.E. Diabetes mellitus impairs tendon-bone healing after rotator cuff repair. J Shoulder Elbow Surg. 2010;19:978–988. doi: 10.1016/j.jse.2009.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boileau P., Brassart N., Watkinson D.J., Carles M., Hatzidakis A.M., Krishnan S.G. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal. J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 3.Carbone S., Gumina S., Arceri V., Campagna V., Fagnani C., Postacchini F. The impact of preoperative smoking habit on rotator cuff tear: cigarette smoking influences rotator cuff tear sizes. J Shoulder Elbow Surg. 2012;21:56–60. doi: 10.1016/j.jse.2011.01.039. [DOI] [PubMed] [Google Scholar]
- 4.Carbonel I., Martinez A.A., Calvo A., Ripalda J., Herrera A. Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop. 2012;36:1877–1883. doi: 10.1007/s00264-012-1559-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho N.S., Lee B.G., Rhee Y.G. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained. Am J Sports Med. 2011;39:2108–2116. doi: 10.1177/0363546510397171. [DOI] [PubMed] [Google Scholar]
- 6.Christoforetti J.J., Krupp R.J., Singleton S.B., Kissenberth M.J., Cook C., Hawkins R.J. Arthroscopic suture – bridge transosseous equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Shoulder Elbow Surg. 2012;21:523–530. doi: 10.1016/j.jse.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Frank J.B., ElAttrache N.S., Dines J.S., Blackburn A., Crues J., Tibone J.E. Repair site integrity after arthroscopic transosseous-equivalent suture-bridging rotator cuff repair. Am J Sports Med. 2008;36:1496–1503. doi: 10.1177/0363546507313574. [DOI] [PubMed] [Google Scholar]
- 8.Goutallier D., Postel J., Bernageau J., Lavau L., Voisin M.C. Fatty muscle degeneration in cuff ruptures: pre – and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 9.Ianotti J.P. Full thickness rotator cuff tears – factors affecting surgical outcome. J Am Acad Orthop Surg. 1994;2:87–95. doi: 10.5435/00124635-199403000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Park M.C., ElAttrache N.S., Tibone J.E., Ahmad C.S., Jun B., Lee T.Q. Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Park M.C., Tibone J.E., ElAttrache N.S., Ahmad C.S., Jun B., Lee T.Q. Part II: biomechanical assessment for a footprint-restoring arthroscopic transosseous-equivalent rotator cuff repair technique compared with a double-row technique. J Shoulder Elbow Surg. 2007;16:469–476. doi: 10.1016/j.jse.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Park J.Y., Siti H.T., Keum J.S., Moon S.G., Oh K.S. Does an arthroscopic suture bridge technique maintain repair integrity? A serial evaluation by ultrasonography. Clin Ortho Relat Res. 2010;468:1578–1587. doi: 10.1007/s11999-009-0990-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugaya H., Maeda K., Matsuki K., Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single row repair versus dual row fixation. Arthroscopy. 2005;21:1307–1316. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Sugaya H., Maeda K., Matsuki K., Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2005;89:953–960. doi: 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 15.Toussaint B., Schnaser E., Bosley J., Lefebvre Y., Gobezie R. Early structural and functional outcomes for arthroscopic double-row transosseous-equivalent rotator cuff repair. Am J Sports Med. 2011;39:1217–1225. doi: 10.1177/0363546510397725. [DOI] [PubMed] [Google Scholar]
- 16.Trantalis J.N., Boorman R.S., Pletsch K., Lo I.K.Y. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2008;24:727–731. doi: 10.1016/j.arthro.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 17.Voigt C., Bosse C., Vosshenrich R., Schulz A.P., Lill H. Arthroscopic supraspinatus tendon repair with suture-bridging technique: functional outcome and magnetic resonance imaging. Am J Sports Med. 2010;38:983–991. doi: 10.1177/0363546509359063. [DOI] [PubMed] [Google Scholar]