Abstract
Hypothermia is associated with a higher risk of perioperative complications and occurs frequently after total joint arthroplasty (TJA). The incidence of hypothermia following total joint arthroplasty was assessed with its risk factors and its correlation with PJI.
Correlation of hypothermia with age, gender, BMI, type of arthroplasty surgery, type of anesthesia, operation time, blood loss, date of surgery and PJI was evaluated in 2600 patients.
Female gender and spinal anesthesia increased the risk for hypothermia whereas an increased BMI and surgery duration correlated decreased the risk of hypothermia. The incidence of hypothermia decreased over time without a correlation with PJI.
Keywords: Inadvertent hypothermia, Hypothermia, Total hip arthroplasty, Total knee arthroplasty, Total joint arthroplasty, Prosthetic joint infection
1. Introduction
Perioperative hypothermia can be an inadvertent effect of major arthroplasty surgery, and may result in possibly avoidable complications. In a previous study we found that the incidence of hypothermia (a core temperature below 36 °C directly after surgery) was high, 26.7%.1 There is scarce literature on the effects of hypothermia after total knee or hip replacement. Other authors have described the negative effect of hypothermia after other major surgery, like abdominal surgery. They found that even mild perioperative hypothermia can increase the incidence of post-operative complications (increased mortality, sepsis, stroke, surgical site infection).2 These effects can be considerable, a decrease of 1.9 °C in core temperature triples the relative risk of surgical site infection (SSI) and increases the duration of hospitalization by 20%.3 Taking protective measures to prevent the negative cascade caused by hypothermia may be particularly important in patients undergoing elective total joint arthroplasty (TJA) because patients are typically older and at risk for similar complications and infection. Periprosthetic joint infection (PJI) after primary total hip arthroplasty (THA) or total knee arthroplasty (TKA) has considerable medical consequences and a mortality rate as high as 2.5%.4
Despite the consequences, hypothermia remains an underrated and unresolved issue. The World Health Organization 2009 guideline (among other national and international guidelines) advise perioperative normothermia to prevent unintended complications but offer no specific guides to achieve that goal.5 Since then, several studies have attempted to establish effective methods to maintain normothermia in patients undergoing surgery in different surgical fields. A recent Cochrane review showed that most technical methods for preventing hypothermia are ineffective, only forced air warming seems to increase the patients core temperature after surgery.6
We felt that the incidence of hypothermia in our previous study was unacceptably high and decided to do a follow-up study. We hoped to reduce the incidence of hypothermia, not by technical measures, but by raised awareness of hypothermia among the medical and nursing staff on the orthopedic ward and in the operating room (OR). In this current prospective observational cohort study we describe the long-term results, using the incidence of hypothermia as a primary outcome. We evaluated the correlation of hypothermia with both its risk factors and with PJI.
2. Methods
The study was approved by the institutional review board (IRB). We included all consecutive patients in our hospital undergoing elective primary unilateral total knee or total hip arthroplasty for osteoarthritis from January 2011 till December 2014. We excluded patients undergoing bilateral surgery or revision surgery. Mild hypothermia is defined as a core temperature between 35 and 36 °C, severe hypothermia as a core temperature below 35 °C. The core temperature was measured at the tympanic membrane (Genius™ 2) in the operation room directly after wound closure. Correlation with age, BMI, gender, type of arthroplasty surgery, type of anesthesia, operation time, blood loss, date of surgery was evaluated.
All patients were treated using the same measures to prevent hypothermia. The warming protocol was not changed during the study period. The use of a forced-air warming system (Bair-hugger©) was already implemented in our hospital, and no other warming system proved to be superior in preventing hypothermia in previous studies.7, 8, 9, 10 Our algorithm included the following measures:
-
•
Use forced air warming (Bair hugger) placed over the patient's chest and arms as long as the operation took, irrespective of core temperature. The Bair hugger was set on maximum temperature (42 °C) and adjusted for comfort of the patient
-
•
No other warming devices were used
-
•
Core temperature was measured before and directly after surgery in the OR
-
•
Maintain ambient temperature between 18 and 21 °C
-
•
Before and after surgery patients were covered with two double folded half cotton blankets.
We informed all medical and nursing professionals on the orthopedic ward and in the OR of the temperature measurement program. In another previous study we found that the largest decrease in body temperature occurred preoperatively on the orthopedic ward and during transport from the ward to the OR.10 Therefore, we introduced routine measurement of preoperative core temperature and started pre-warming with an electric above-patient warmer if indicated (i.e. if temperature was below 36 °C).
Operating technique was not changed during the years. All TKA patients were operated on using a tourniquet. All TKA's were cemented, all THA's were uncemented. General or spinal anesthesia was used in all patients depending on the patients personal favor and possible risk factors as assessed by an anesthesiologist. Reported operation time is the time between skin incision and closure of the operation wound.
Patients were diagnosed to have a PJI based on MSIS major and minor criteria.11 In case of an early infection, as defined in the IDSA guidelines4, debridement with implant retention was performed and six cultures were obtained. Until cultures were definitive, patients were treated with intravenous antibiotics (Cefazoline). If cultures proved positive antibiotic therapy was adjusted accordingly and administered for a total of 12 weeks. If this treatment was not sufficient, a one- or two stage revision of the prosthetic joint was performed. We considered patients to have a PJI when two or more cultures were positive or when patients were treated for 12 weeks based on clinical symptoms and consensus of the orthopedic surgeon, medical microbiologist and infectiologist during our weekly meeting.
Statistical analyses were carried out using the statistical package SPSS© version 23.0. Baseline characteristics of the patients with a THA or TKA were compared using the chi square and the Mann-Whitney U test since the Kolmogorov-Smirnov test showed that age, BMI and surgery duration were not normally distributed. The difference between mean core temperature in the hypothermia versus the normothermia group was tested with an independent sample t-test. Difference in incidence of mild hypothermia and PJI between THA and TKA was tested with chi square test. The influence of type of anesthesia, operation time, age, gender, BMI and more recent surgery date on the difference in mean core temperature in both groups was analyzed with linear regression analysis. Results with a p-value of less than 0.05 were considered to be statistically significant.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
3. Results
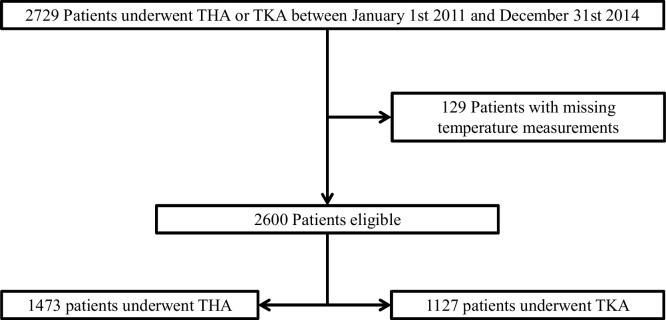
During the study period, a total of 2729 consecutive patients underwent TKA or THA. Subsequently, 129 patients were excluded because of missing temperature measurements (Fig. 1). Table 1 shows the baseline characteristics of the 2600 patients in our study population, 1127 undergoing TKA and 1473 undergoing THA. There was no significant difference in type of anesthesia. However, there was a significant difference in gender, mean age, BMI and mean operation time between the two groups (Table 1). 39% of the TKA patients were male versus 33.4% in the THA group. In the TKA group 74.9% received spinal anesthesia versus 77.5% in the THA group. Mean operation time was 13 min longer in the TKA group than in the THA group, 59.18 vs. 46.11 min respectively. Furthermore, the mean BMI was 29.90 in the TKA group and 27.43 in the THA group.
Fig. 1.
Flow-chart illustrating the patient inclusion process.
Table 1.
Baseline characteristics. Percentages are given between brackets, ranges are given between square brackets. S = spinal anesthesia; G = general anesthesia.
| n = 2600 | TKA n = 1127 (43,3%) | THA n = 1473 (56,7%) | p-value |
|---|---|---|---|
| Gender M: F (%) | 440: 687 (39%: 61%) | 492: 981 (33.4%: 66.6%) | 0.003 |
| Mean Age (years) | 67.57 [38–92] | 69.34 [32–92] | 0.000 |
| Type of Anesthesia S: G | 839: 281 (74,9%: 25,1%) | 1132: 328 (77.5%: 22.5%) | 0.120 |
| Mean Operation time (min) | 67,55 [25–131] | 69,32 [18–200] | 0.000 |
| Mean Body Mass Index | 29.97 [18–48] | 27.46 [15–47] | 0.000 |
Our primary outcome was an overall incidence of 11.7% of mild hypothermia. The incidence of mild hypothermia in the TKA group was 1.8% lower than in the THA group (10.7 vs. 12.5% respectively). This difference was not significant, p = 0.172. We did not observe moderate or severe hypothermia. Mean core temperature directly after arthroplasty surgery was 36.5 °C in both groups (SD = 0.5149). In the TKA group the standard deviation was 0.0144 and in the THA group 0.0140. There was no significant statistical difference (p = 0.521). A chi-square test showed a significant difference between the incidences of hypothermia between the years 2011 and 2012 (p = 0.000), 2012 and 2013(p = 0.042), but not between the years 2013 and 2014. A linear regression analysis shows a negative linear relationship between gender and core temperature (p = 0.000) and type of anesthesia and core temperature(p = 0.033). A positive linear relationship was shown between core temperature and BMI (p = 0.000), female gender (p = 0.000) and the date of surgery (p = 0.000). Both patient age (p = 0.062) and blood loss (in the THA group, all TKA were placed using a tourniquet) were not related with core temperature (p = 0.221). Please refer to Table 2, Table 3 for more details.
Table 2.
Mean postoperative body temperature and incidence of hypothermia and infections.
| n = 2600 | Total (n = 2600) | TKA (n = 1127) | THA (n = 1473) | p-value |
|---|---|---|---|---|
| % < 36 °C | 305 (11.7%) | 121 (10.7%) | 184 (12.5%) | 0.168 |
| Mean temp | 36,5 °C | 36.5 °C | 36.5 °C | 0.990 |
| % Infections | 46 (1.8%) | 17 (1.5%) | 29 (2.0%) | 0.378 |
Table 3.
Multivariate linear regression analysis model of the relation between the type of anesthesia, BMI, duration of surgery, gender, arthroplasty type (hip or knee), age and the postoperative core temperature. B = regression coefficient; 95% CI = 95% confidence interval for B; P = significance.
| n = 2600 | B | 95% CI | P |
|---|---|---|---|
| Gender | −0.103 | −0.148 to −0.059 | 0.000 |
| Type of Anesthesia | −0.054 | −0.105 to −0.004 | 0.035 |
| Body Mass Index | 0.008 | 0.004–0.013 | 0.000 |
| Duration of surgery | 0.001 | 0.000–0.003 | 0.110 |
| Date of surgery | 1.975E-9 | 0.000–0.000 | 0.000 |
| Age | −0.002 | −0.004 to 0.000 | 0.062 |
| Arthroplasty type | −0.018 | −0.065 to 0.029 | 0.452 |
Forty-six patients (1.8%) had a PJI. In the TKA group the incidence of PJI was 1.5% PJI, in the THA group the incidence was 1.9%. This difference was non-significant (p = 0.378). The incidence of PJI was 1.0% in hypothermic patients versus 1.9% in normothermic patients. This yields a non-significant (p = 0.27) relative risk ratio of 0.52. In the THA group, in the normothermic subgroup the incidence of PJI was 2.2%, the incidence of PJI in the hypothermic subgroup was 0%. This difference was significant, p = 0.041. After TKA, the incidence of PJI was 1.4% in the normothermic subgroup and 2.5% in the hypothermic subgroup. This difference was not significant (p = 0.354).
4. Discussion
This study indicates that the incidence of inadvertent hypothermia can be reduced. We found that the incidence of mild hypothermia decreased over the study period, with a ceiling effect after two years. We suspect that increased awareness among the staff on the ward and the OR combined with pre-operative heating may be an explanation for the decline in the incidence of hypothermia. We found an overall incidence of 11.7% in primary total knee or hip arthroplasty. This is much lower than the incidence we found in our previous 2013 study, which was 26.7%.
A higher BMI is positively correlated with a higher post-operative core temperature. Females appear to be at greater risk of developing hypothermia after TJA. Spinal anesthesia seems negatively correlated with post-operative body temperature. A previous study did not find significant differences between spinal or general anesthesia, but this could be due to the relative smaller sample sizes in those studies compared to this study.12 Spinal anesthesia is believed to lead to hypothermia because of a decreased shivering- and vasoconstriction threshold and vasodilatation in the lower extremities.12 Our data indicates spinal anesthesia may result in greater decrease in body temperature than general anesthesia, but show no difference in mean post-operative core temperature after TKA or THA.
Mild hypothermia was not associated with a higher incidence of PJI. This is contradictory to the findings in other fields of surgery.2, 13 This difference might be explained by the severity of hypothermia. Perhaps only severe hypothermia leads to an increased risk of infection. Another possible explanation is that in patients with a high risk of PJI more attention is given to the prevention of hypothermia. A third possibility is that other factors are more important in the development of a PJI. A higher BMI is correlated to a higher core temperature but also leads to a higher chance of a PJI.14 The international consensus group on PJI has identified certain host (or patient) factors for PJI, which include male gender, previous surgery, uncontrolled diabetes mellitus, malnutrition, morbid obesity, active liver or renal disease, smoking or excessive alcohol consumption, intravenous drug abuse, recent hospitalization, active infection, inflammatory arthropathy and severe immunodeficiency.11
Previous studies have tried to establish effective methods to prevent inadvertent hypothermia. These methods mainly consisted of equipment to either warm the patient actively or to passively keep the patient warm during surgery with intensified temperature monitoring. Large scale results show that only forced-air warming seems effective in preventing inadvertent hypothermia and that the use of thermal insulation methods are not effective in maintaining normothermia.6, 7, 9 Combined strategies, including preoperative commencement of warming devices, are more effective then isolated measures in vulnerable groups (higher age or longer duration of surgery).8 One study showed that an underbody warming system could reduce the incidence of hypothermia in laparoscopic gastrointestinal surgery.15 The latter might be useful as an additional method to warm patients during TJA, but to date no studies have been published on its use in orthopedic surgery. It remains doubtful if it has additional value, since arthroplasty procedures require less operating time then most laparoscopic procedures.
We conclude that creating awareness among the medical and nursing staff can result in a lower incidence of hypothermia in patients undergoing TKA or THA, but this does not influence the incidence of PJI. However, hypothermia does not seem to be correlated with PJI, neither does it result in a reduction of PJI.
Authors contribution
R. Scholten contributed to the initial setup for the study, the process of data collection, data analysis and writing of the paper.
B. Leijtens contributed to the initial setup for the study, the process of data collection, data analysis and writing of the paper.
K. Kremers contributed to the process of data collection and writing the paper.
M. Snoeck contributed to writing the paper.
S. Koëter was responsible for the supervision of the complete study process and contributed to the writing of the paper.
Conflict of interest
None.
Funding
All authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- 1.Leijtens B., Koëter M., Kremers K., Koëter S. High incidence of postoperative hypothermia in total knee and total hip arthroplasty: a prospective observational study. J Arthroplasty. 2013;28(June 6):895–898. doi: 10.1016/j.arth.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Billeter A.T., Hohmann S.F., Druen D., Cannon R., Polk H.C. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery. 2014;156(November (5)):1245–1252. doi: 10.1016/j.surg.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 3.Kurz A. Thermal care in the perioperative period. Best Pract Res Clin Anaesthesiol. 2008;22(March (1)):39–62. doi: 10.1016/j.bpa.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Osmon D.R., Berbari E.F., Berendt A.R. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(January (1)):1–10. doi: 10.1093/cid/cis966. [DOI] [PubMed] [Google Scholar]
- 5.WHO . World Health Organization; 2009. Guidelines for Safe Surgery: Safe Surgery Saves Lives. [PubMed] [Google Scholar]
- 6.Alderson P., Campbell G., Smith A.F., Warttig S., Nicholson A., Lewis S.R. Thermal insulation for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. 2014;6:CD009908. doi: 10.1002/14651858.CD009908.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berti M., Casati A., Torri G., Aldegheri G., Lugani D., Fanelli G. Active warming, not passive heat retention, maintains normothermia during combined epidural-general anesthesia for hip and knee arthroplasty. J Clin Anesth. 1997;9(September (6)):482–486. doi: 10.1016/s0952-8180(97)00105-0. [DOI] [PubMed] [Google Scholar]
- 8.Moola S., Lockwood C. Effectiveness of strategies for the management and/or prevention of hypothermia within the adult perioperative environment. Int J Evid Based Healthc. 2011;9(December (4)):337–345. doi: 10.1111/j.1744-1609.2011.00227.x. [DOI] [PubMed] [Google Scholar]
- 9.Ng S.F., Oo C.S., Loh K.H., Lim P.Y., Chan Y.H., Ong B.C. A comparative study of three warming interventions to determine the most effective in maintaining perioperative normothermia. Anesth Analg. 2003;96(January (1)):171–176. doi: 10.1097/00000539-200301000-00036. [table of contents] [DOI] [PubMed] [Google Scholar]
- 10.Koëter M., Leijtens B., Koëter S. Effect of thermal reflective blanket placement on hypothermia in primary unilateral total hip or knee arthroplasty. J Perianesth Nurs. 2013;28(December (6)):347–352. doi: 10.1016/j.jopan.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Parvizi J., Gehrke T., Chen A.F. Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J. 2013;95-B(November (11)):1450–1452. doi: 10.1302/0301-620X.95B11.33135. [DOI] [PubMed] [Google Scholar]
- 12.Cattaneo C.G., Frank S.M., Hesel T.W., El-Rahmany H.K., Kim L.J., Tran K.M. The accuracy and precision of body temperature monitoring methods during regional and general anesthesia. Anesth Analg. 2000;90(April (4)):938–945. doi: 10.1097/00000539-200004000-00030. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds L., Beckmann J., Kurz A. Perioperative complications of hypothermia. Best Pract Res Clin Anaesthesiol. 2008;22(December (4)):645–657. doi: 10.1016/j.bpa.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Kunutsor S.K., Whitehouse M.R., Blom A.W., Beswick A.D., Team I. Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS One. 2016;11(3):e0150866. doi: 10.1371/journal.pone.0150866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pu Y., Cen G., Sun J. Warming with an underbody warming system reduces intraoperative hypothermia in patients undergoing laparoscopic gastrointestinal surgery: a randomized controlled study. Int J Nurs Stud. 2014;51(February (2)):181–189. doi: 10.1016/j.ijnurstu.2013.05.013. [DOI] [PubMed] [Google Scholar]