Abstract
Purpose
Anterior cruciate ligament (ACL) injury is one of the most common injuries that occur in the knee, and ACL reconstruction (ACLR) is commonly performed for preventing aggravation of degenerative changes and restoring of knee stability in young, athletic patients. This metaanalysis has a purpose of evaluating the clinical and arthrometrical outcomes of ACLR in a group of middle age patients (40 years and older) and comparing with patients under 40 years of age.
Methods
MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials, Web of Science, and SCOPUS electronic databases were searched for relevant articles comparing the outcomes of ACLR between younger and older than 40 years of age until December 2016. Data searching, extraction, analysis, and quality assessment were performed based on the Cochrane Collaboration guidelines. Clinical outcomes were evaluated and compared between groups. The results were presented as mean difference for continuous outcomes with 95% confidence intervals whereas risk ratio for binary outcomes.
Results
Seven studies were included in the meta-analysis. Based on International Knee Documentation Committee classification, side-to-side difference, Tegner activity score, Lysholm knee score, there were no significant clinical and mechanical differences between the groups.
Conclusions
This meta-analysis confirmed that after ACLR, middle age (>40 years) and young age (<40 years) patients did not present with significant difference in clinical and arthrometric results.
Keywords: Knee, Anterior cruciate ligament, Reconstruction, Age, Meta-analysis
Introduction
Anterior cruciate ligament (ACL) ruptures are one of the most common sports-related knee injuries. ACL reconstruction is usually reserved for young, athletic patients and is commonly performed to restore knee stability and reduce the risk of further injuries and progression of degenerative changes1). Recreational athletes of more than 40 years of age are increasing steadily, and they frequently participate in physically demanding sports2,3).
Early reports on the treatment of ACL injuries suggested a non-surgical regimen for middle-aged patients. Patients were advised to modify their physical activities, along with physical therapy and functional bracing. This conservative treatment approach was based on concerns of higher rates of postoperative arthrofibrosis, loss of extension, and poorer results following ACL reconstruction in middle aged patients; thus, they are initially indicated for physiotherapy, and the need for surgery is considered afterwards4). Generally, due to ongoing degenerative changes of intraarticular soft tissues, concomitant chondral damage, and meniscal injury, the prognosis is not favorable after ACL reconstruction in middle age patients (>40 years). However, it is well known that especially active patents of any age are increasingly unwilling to change their sports activities and request restoration of intact overall knee function. Recent data have shown that the results of ACL reconstruction in patients over the age of 40 years, with or without concomitant degenerative changes, are comparable to those in younger patients4). Good results of ACL reconstruction in patients over 40 years have been widely documented as much as those in younger patients. Although several authors reported no statistically significant difference in clinical results between the two different age groups5), few systematically reviewed the literature for comparison on the efficacy of ACL reconstruction between over 40 and under 40 years of age.
The purpose of this study is to compare the outcomes of ACL reconstruction between middle age patients (>40 years) and younger patients (<40 years) through systematic review of data extracted from all the included studies. We hypothesized that patients older than 40 years of age would achieve clinical outcomes of ACL reconstruction comparable to those in patients younger than 40 years of age.
Methods
1. Data and Literature Sources
The study design was based on Cochrane review methods. A systematic search of MEDLINE, EMBASE, Cochrane, SCOPUS and Web of science (January 1996 to December 2016) was conducted to identify results of ACL reconstruction in over 40 years (middle age patients) and under 40 years (younger patients). These databases were searched for the relevant articles by use of the following keywords: “anterior cruciate ligament”, “reconstruction”, “age”, and “middle age”. References of each selected article were manually searched for any article that may have been missed during the database search. Authors performed the search for the relevant articles, and the identified articles were included in this study based on consensus. Articles identified were assessed individually for inclusion.
2. Study Selection
We used multiple comprehensive databases to find literatures that compared outcomes of ACL reconstruction in over 40 years and under 40 years old. This study was based on the Cochrane methods of review, and reporting was in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. To identify relevant studies, we used the controlled vocabulary and free text words described in Appendix 1 to search MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials, Web of Science, and SCOPUS databases; we attempted to identify all relevant studies regardless of language, publication type (article, poster, conference paper, instructional course lecture, etc.), publication journal, or publication year. This search was updated in December 2016 and includes reference lists of the studies and any review articles identified. Study inclusion was decided by 2 independent researchers in accordance with selection criteria, and when it was difficult to evaluate the pertinence of the subject after reading titles and abstracts, the full article was perused. This meta-analysis included studies that meet the following criteria: (1) ACL reconstruction was done regardless of the presence of meniscal/chondral damage in addition to an ACL injury; (2) clinical outcomes (Tegner score, International Knee Documentation Committee [IKDC] classification, and Lysholm knee score) or an arthrometric evaluation with KT-1000 arthrometer (MEDmetric, San Diego, CA, USA) were described and compared between middle age and younger age groups with means and standard deviations (SDs) presented; (3) ACL reconstruction was performed after 1990s. We excluded studies that did not compare the outcomes of ACL reconstruction over 40 years and under 40 years old and single-arm studies that only described ACL reconstruction in one group. Cadaver studies and concomitant ligament injuries (medial/latera collateral ligament and posterior cruciate ligament) were excluded as well.
3. Data Extraction
Two investigators (SCH and DKM) independently recorded following data based on predefined data extraction form: (1) surgical technique, (2) type of graft (allograft: bone patella tendon, Achilles tendon, or tibialis anterior tendon; autograft: semitendinosus or gracilis tendon), (3) postoperative clinical score, radiologic finding, and side-to-side difference, (4) sample size of each group, age, and sex, (5) concomitant degenerative change, and (6) type of complication. For records that the two investigators did not reach consensus on, they were reviewed by the third investigator.
4. Data Collection and Analysis
We (SCH and DKM) independently assessed the titles or abstracts of studies identified by the search strategy and then reviewed full papers for final inclusion; we resolved uncertainties through discussion and consensus. We independently abstracted eligible data onto predefined forms and checked them for accuracy. We also collected information on study characteristics (authors, journal title, and publication year), patient demographic data (sex, age, number of subjects in each group, and graft type), concomitant degenerative change, results of studies including Tegner score, IKDC classification, Lysholm knee score, and arthrometric evaluation with KT-1000 arthrometer. Then, we determined the number of subjects and the means and SDs of the demographic data and clinical outcomes in the two age groups. If theses variables were not reported in the articles, the study authors were contacted by email to request these data.
5. Assessment of Methodological Quality
For qualified analysis, the Newcastle-Ottawa quality assessment scale was adopted. The Newcastle-Ottawa assessment scale is a tool for evaluating clinical cohort studies, awarding a maximum of 9 stars on total 3 items including selection of subjects, comparison between the two groups, and the evaluation of results for assessing validity of the research. In this analysis, studies with 1 star through 9 stars were all included. We did not conduct publication bias test using the funnel plot of the 7 studies included in this meta-analysis, as the number of included studies was <10 in each field of research.
6. Statistical Analysis
The main purpose of this review was to compare clinical outcomes between a group of patients under 40 years old and a group of patients over 40 years old following ACL reconstruction. To compare the functional outcome between groups, we assessed the side-to-side differences, the IKDC classification, Lysholm knee score, and Tegner activity score. We used Review Manager ver. 5.3 (The Cochrane Collaboration, Oxford, United Kingdom) to estimate the overall pooled effect size for each outcome, and we conducted a meta-analysis of the included studies using a random-effects model. For the continuous outcomes, we calculated MDs with 95% confidence intervals (CIs) using an inverse variance method. For binary outcomes, the risk ratio (RR) was calculated. We assessed statistical heterogeneity among the studies using I-squared (I2), with values of 25%, 50%, and 75% considered low, moderate, and high, respectively. Cochrane’s Q statistic (chi-square test) was used for heterogeneity and p<0.10 was considered significant for heterogeneity.
Results
1. Identification of Studies
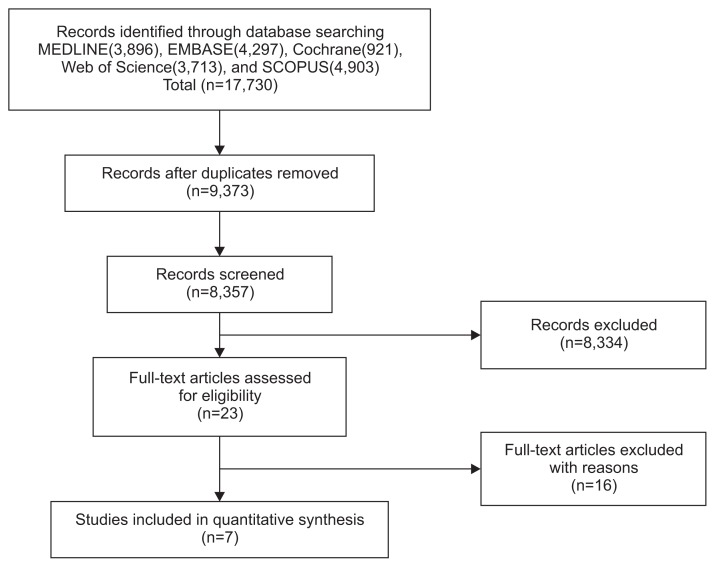
Fig. 1 shows the details of study identification, inclusion, and exclusion. We initially identified a total of 17,730 relevant articles. Of these, 8,357 were duplicates in the databases. After screening the remaining 9,373 articles using titles and abstracts, we excluded 9,350 because they were not relevant to the purpose of the present study. Then, we excluded 16 articles following thorough a full-text review of all 23 articles because they were published prior to 1990s, duration of follow-up period was less than 2 years, ACL reconstruction was performed after mid-50s, and the knee joint injury was accompanied by other joint injuries. Finally, we included 7 studies where such commonly used parameters as arthrometric evaluation (side-to-side difference), IKDC classification, Lysholm knee score, and Tegner activity score were adopted and groups were divided by age 40.
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) flow diagram of identification and selection of the studies included in this metaanalysis.
2. Quality and Publication Bias of the Included Studies
All 7 studies1,4,6–10) were included for meta-analysis, and the risk of selection bias between the two groups was low. Assessable confounding factors did not exist for evaluation of demographic data. Follow-up period was recorded: the longer the period, the lower the risk of bias. All 7 studies included in this meta-analysis had a low risk of selection bias and compared demographic data of subjects undergoing ACL reconstructions in over 40 and under 40 years of age, with none assessing possible confounding factors. Follow-up was defined as the interval between surgery and outcome evaluation. A longer interval was associated with a higher risk of bias, because clinical score may change over time because of correction loss.
3. Outcomes of ACL Reconstruction in Age-Based Comparative Studies
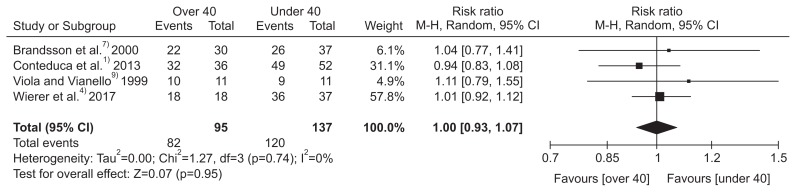
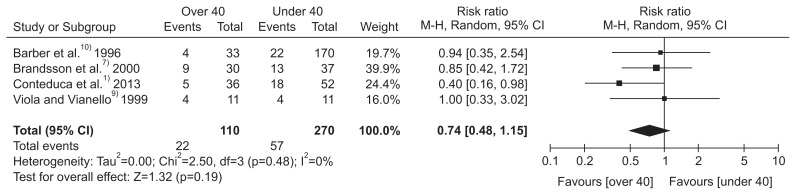
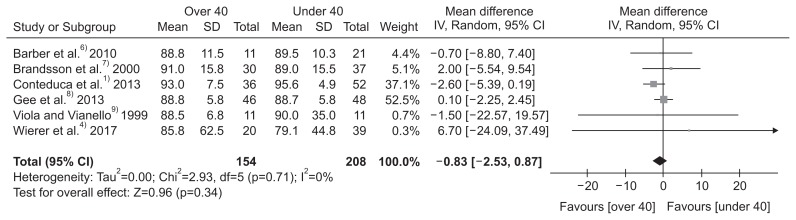
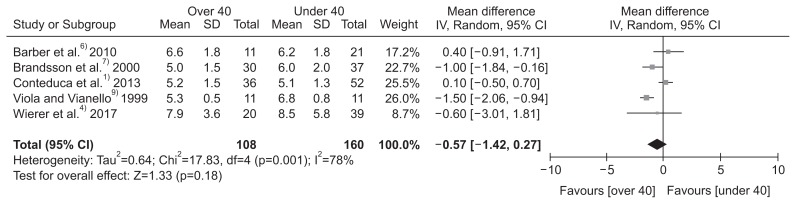
A total of 369 ACL reconstructions were performed (170 in young patients; 199 in middle age patients) in the entire studies included. Among the 199 middle age patients, ACL injury only patients were 64 and the remaining 135 patients had degenerative changes with a meniscus tear or chondral damage accompanying the ACL injury. As for the surgical technique, anatomical single- or double-bundle endoscopic ACL reconstruction, arthroscopically-assisted two incision technique, and isolated ACL reconstruction with hamstring tendon graft were performed. Regarding the graft, autograft (hamstring, gracilis tendon, and bone-patellar tendon-bone graft) and allograft (Achilles tendon and tibialis anterior tendon) were used. The follow-up period was 24–60 months. The most critical evaluation basis for prognostic outcomes in the seven included studies were arthrometric evaluation (side-to-side difference), IKDC classification, Lysholm knee score, and Tegner activity score. Radiologic change was evaluated after ACL reconstruction: middle age groups mostly presented with occurrence of osteoarthritis (OA). With regard to complications, knee stiffness, arthrofibrosis, postoperative infection, wound healing problems, and deep vein thrombosis were observed; re-surgery was performed due to meniscal injury and screw problem in many of these cases (Tables 1–3). The IKDC classification, side-to-side difference yielded relative ratios for dichotomous variables, which did not significantly differ and a CI was generated for the side-to-side difference in only over 40 years of age (IKDC: RR, 1.00; 95% CI, 0.93 to 1.07; I2=0%; side-to side difference: RR, 0.74; 95% CI, 0.48 to 1.15; I2=0%). This is reported to be due to loss of elasticity in the middle age group1,11,12) (Figs. 2 and 3). For continuous outcome variables including the Tegner activity score and Lysholom knee score, mean differences did not significantly differ between the two age groups (Tegner activity score: MD, −0.57; 95% CI, −1.42 to 0.27, I2=75%; Lysholm knee score: MD, −0.83; 95% CI, −2.53 to 0.87; I2=0%) (Figs. 4 and 5).
Table 1.
The Characteristics of Clinical Studies
| Study | Journal | Study design | Level of evidence | Year | Study period | Age (yr), mean (no.) | Graft | Concomitant injury | Follow-up time (mo) |
|---|---|---|---|---|---|---|---|---|---|
| Conteduca et al.1) | Int Orthop | Retrospective cohort study | 3 | 2013 | 2002–2010 | >40: 45.4 (36) <40: NP (52) |
Autograft (semitendinosus, gracilis tendon) | Inclusion | 42 |
| Viola and Vianello9) | Knee Surg Sports Traumatol Arthrosc | Retrospective cohort study | 3 | 1999 | 1991–1994 | >40: 42.6 (11) <40: 20.3 (11) |
Allograft (bone-patellar tendon-bone) | Exclusion | 29 |
| Brandsson et al.7) | Arthroscopy | Retrospective cohort study | 3 | 2000 | 1991–1994 | >40: 43 (30) <40: 37 (37) |
Autograft (bone-patellar tendon-bone) | Inclusion | 31 |
| Gee et al.8) | Phys Sportsmed | Retrospective cohort study | 3 | 2013 | 2000–2008 | <40: 21 (48) >40: 45 (46) |
Autograft (bone-patellar tendon-bone, Achilles tendon), allograft (tibialis anterior) | Inclusion | 60 |
| Wierer et al.4) | Knee Surg Sports Traumatol Arthrosc | Retrospective cohort study | 3 | 2017 | 2010–2016 | >40: 45 (20) <40: 27 (39) |
Autograft (semitendinosus, gracillis tendon) | Exclusion | 24 |
| Barber et al.6) | Arthroscopy | Retrospective cohort study | 3 | 2010 | 2002–2005 | <40: 31 (21) >40: 46 (11) |
Allograft (bone-patellar tendon-bone) | Inclusion | 35 |
| Barber et al.10) | Arthroscopy | Retrospective cohort study | 3 | 1996 | 1992–1994 | <40: 27 (170) >40: 44 (33) |
Allograft, autograft (bone-patellar tendon-bone, Achilles tendon) | Exclusion | 12 |
NP: not provide.
Table 2.
The Characteristics of Clinical Studies
| Study | Technique | Complication | Radiologic findings |
|---|---|---|---|
| Conteduca et al.1) | Arthroscopic ACL reconstruction | Both group: knee stiffness, arthrofibrosis, postoperative infection, wound healing problems, deep vein thrombosis >40: failure (11%) |
>40: osteoarthritis development |
| Viola and Vianello9) | Arthroscopic ACL reconstruction | NP | >40: normal or minimal change (small osteophytes without joint line narrowing) |
| Brandsson et al.7) | Arthroscopic ACL reconstruction | >40: postoperative bleeding, meniscal injury | >40: OA development |
| Gee et al.8) | Arthroscopic ACL reconstruction | >40: graft failure, arthrofibrosis, infection (8.7%) | No definite signs of OA |
| Wierer et al.4) | Arthroscopic ACL reconstruction | NP | No definite signs of OA |
| Barber et al.6) | Arthroscopic ACL reconstruction | NP | No definite signs of OA |
| Barber et al.10) | Arthroscopic ACL reconstruction | >40: joint stiffness | No definite signs of OA |
ACL: anterior cruciate ligament, NP: not provide, OA: osteoarthritis.
Table 3.
Comparison of Clinical Outcomes between Groups in Included Studies
| Study | Group (no.) | Lysholm knee score (SD) | Tegner score (SD) | IKDC (objective evaluation) | KT-1000 arthrometer (side-to-side difference) |
|---|---|---|---|---|---|
| Conteduca et al.1) | <30 (27) | 97 (3.0) | 6.3 (3–10)/5.3 (3–7) | A (12, 42.9%), B (14, 50%), C (2, 7.1%), D (0, 0%) | <3 mm : 63% 3–5 mm: 22% >5 mm: 15% |
| 30–40 (25) | 94 (6.4) | 5.4 (1–9)/4.8 (1–7) | A (13, 52%), B (10, 40%), C (2, 8%), D (0, 0%) | <3 mm: 68% 3–5 mm: 20% >5 mm: 12% |
|
| >40 (36) | 93 (7.5) | 4 (2–8)/5.2 (2–8) | A: 25 (69.5), B: 7 (19.5), C: 3 (8.3), D: 1 (2.7) | <3 mm: 86% 3–5 mm: 3% >5 mm: 11% |
|
| Viola and Vianello9) | >40 (11) | 88.5 (73–100) | 3.7 (3–5)/5.3 (4–6) | A (1), B (8), C (2), D (0) | 30 lb/max<3 mm: 7 3–5 mm: 4 >5 mm: 0 |
| <40 (11) | 90 (86–100) | 4.4 (3–6)/6.8 (6–9) | A (3), B (7), C (1), D (0) | 30 lb/max<3 mm: 7 3–5 mm: 4 >5 mm: 0 |
|
| Brandsson et al.7) | <40 (37) | 89 (38–100) | 9 (4–9)/6 (1–9) | A (8), B (18), C (10), D (1) | 13/37 (35%) |
| >40 (30) | 91 (37–100) | 6 (4–9)/5 (3–9) | A (10), B (12), C (6), D (2) | 9/30 (30%) | |
| Gee et al.8) | <40 (48) | 88.7 (5.81) | Not measured | Not measured | Not measured |
| >40 (46) | 88.8 (5.76) | ||||
| Wierer et al.4) | <40 (39) | 90 (68–100) | 6 (2–9) | A (21), B (15), C (1), D (0) | Not measured |
| >40 (20) | 94.5 (63–100) | 5.5 (3–8) | A (9), B (9) | ||
| Barber et al.6) | <40 (21) | 46.8 (2–88)/89.5 (59–100) | 3.9 (1–7)/6.2 (3–10) | Not measured | Not measured |
| >40 (11) | 50.1 (21–71)/88.8 (54–100) | 3.9 (2–8)/6.6 (2–9) | |||
| Barber et al.10) | <40 (170) | 56/95 | 2.4/6.1 | Not measured | <3 mm: 56 3–5 mm: 18 >5 mm: 4 |
| >40 (33) | 54/95 | 2.4/5.7 | <3 mm: 15 3–5 mm: 2 >5 mm: 2 |
SD: standard deviation, IKDC: International Knee Documentation Committee.
Fig. 2.
Forest plot of International Knee Documentation Committee (IKDC). CI: confidence interval.
Fig. 3.
Forest plot of side-to-side difference. CI: confidence interval.
Fig. 4.
Forest plot of Lysholm knee score. SD: standard deviation, CI: confidence interval.
Fig. 5.
Forest plot of Tegner activity score. SD: standard deviation, CI: confidence interval.
Discussion
In this meta-analysis, we tried to assess the efficaciousness of ACL reconstruction in the middle age patients (over 40 years). We evaluated clinical outcomes using such parameters as the IKDC score, Tegner activity score, Lysholm knee score, and arthrometric examination (side-to-side difference), radiologic findings, and complications after ACL reconstruction between younger patients (under 40 years) and middle age patients (over 40 years). In general, middle age patients undergo conservative treatment in case of an ACL injury4). However, we noted in this study that there were no statistically significant differences in the outcomes of ACL reconstruction between the middle age group and young age group, confirming our hypothesis. The middle age group did not have high demand for physical activity and they obtained high scores in an assessment which does not fully reflect clinical outcome and great improvement in sports that do not involve knee activity. Isolated ACL injury patients with chronic knee instability and degenerative change presented with long-term stability and symptomatic relief after ACL reconstruction; however, a higher prevalence of OA was noted in the long-term radiologic follow-up13). Significantly poorer synovial coverage was observed in middle age patients through second-look arthroscopy14) and they were more susceptible to postoperative OA than younger patients after ACL reconstruction11). However, with regard to the postoperative Knee injury and Osteoarthritis Outcome Score, they did not significantly differ from young patients and obtained better improvement. This may reflect the tendency, among the middle age group, of the low overall demand for optimal knee function and better compliance with rehabilitation12). In contrast, younger patients have an expectation for full recovery of knee function, and they tend to be dejected with unsatisfactory outcomes more frequently13). Three studies included only isolated ACL injury, and concomitant degenerative changes, such as meniscus tear and chondral damage, were excluded. Even after exclusion of data from these studies, the results did not differ significantly. Therefore, it can be deduced that concomitant degenerative changes do not have to be considered a decisive factor in ACL reconstruction, although this has to be confirmed by large-scale randomized controlled trials (RCTs). Seven studies were included in the meta-analysis, and the results showed that there were no significant differences in clinical outcomes and arthrometric examination (side-to-side difference) after ACL reconstruction between the two age groups, but one study demonstrated better results in the middle age group. On the analysis of Tegner activity score, 2 studies7,9) reported confidence intervals in over 40 years of patients. In the studies, Tegner activity score, vastly dependent on individual satisfaction, showed statistically significance difference7,9). However, overall, studies showed no statistically significant difference. It is reported due to scar tissue formation, initial OA, different hormonal patterns (especially in women), and loss of tissue elasticity which also led to statistically significant difference in the mean side-to-side difference in the middle age group, and it assumed to be ascribable to change in underlying structures and mechanical properties of tendon and myotendinous junction according to aging process1,15,16).
Based upon the outcomes of this study, there was no significant statistical difference in results between the two age groups, and it can be concluded that the prognosis of ACL reconstruction does not necessarily depend on age9). This is because, first of all, middle age patients were not in as much need for physical activity, and, thus, higher satisfaction was demonstrated in the subjective assessment of clinical outcomes and more knee-involving activities were available following ACL reconstruction. Second, long-term stability and symptomatic relief were acquired after ACL reconstruction in isolated ACL injury patients with chronic instability of the knee and degenerative changes17). However, they presented with more clinical characteristics consistent with OA on X-ray13). We wonder if there is a prophylactic effect for OA from ACL reconstruction, which should be investigated in further studies. Third, several studies1,4,11) including patients with concomitant injuries to the meniscus, posterior cruciate ligament, and collateral ligament were excluded. However, even after excluding these data, outcome did not significantly differ, and concomitant injuries were not considered a crucial factor. In other studies, clinical outcomes of ACL reconstruction were not associated with the type of graft or fixation device18).
The timing of surgical treatment primarily depends on the age of patients as middle age patients are initially managed with conservative treatment such as physiotherapy and decision as to whether they become indicated for surgical treatment is usually procrastinated. Prolonged time span between the time of injury and that of surgical treatment predisposes a patient to aggravation of concomitant injuries, which is why young athletic patients who are in for great demand for optimal knee function are indicated for early surgical treatment. Despite the difference in the timing of surgical treatment between the two age groups, the subjective and functional outcomes did not significantly differ11). Even though the selected type of graft differed by age, availability, and many other determinants, the Lysholm knee score in turn was not affected by such disparity. Therefore, physiological age, activity level, desire for knee-involving sports, symptoms of instability, and associated knee lesions need to be taken into consideration in performing ACL reconstruction8).
One of the limitations of this study is that although outcome measures used in this study such as clinical scores were validated by many orthopedic surgeons, it was difficult to rule out the influence of subject components on the evaluation of clinical outcome. Second, there were not many patients enrolled, and a vast amount of time is required to evaluate long-term outcomes in these patients. In addition, the mean age of the patients in the middle age group was 44.4 years old, which indicates that the results do not represent possible outcomes in patients over the mean age. Therefore, further studies targeting patients over 50 years old are required. Third, comparison of degenerative changes and complications such as infection and graft failure and confounding factors between the two groups was not fully performed. Fourth, we could not control confounding factors such as demographic data (meniscal injury, cartilage injury, muscle strength, etc.). There was a mention of degenerative meniscus tear and chondral injury in the included papers, but there was no data comparing clinical outcomes. Fifth, techniques related to ACL reconstruction were being developed in the meantime, which was not included as a cofounding factor in this study. Advanced ACL reconstruction techniques could have contributed to better results in the middle age group. Prognostic evaluation through long-term follow-up is required. To verify and strengthen our results, more high-quality RCTs are required.
Conclusions
ACL reconstruction is a valid option for middle age patients (>40 years) and it is not absolutely age-dependent. The presence of OA, tendon stiffness, and concomitant injury should be considered in determining ACL reconstruction for middle age patients; however, in terms of greater possibility of more activities and better knee stability, surgical treatment may be helpful for middle age patients with ACL injury.
Supplementary Information
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Conteduca F, Caperna L, Ferretti A, Iorio R, Civitenga C, Ponzo A. Knee stability after anterior cruciate ligament reconstruction in patients older than forty years: comparison between different age groups. Int Orthop. 2013;37:2265–9. doi: 10.1007/s00264-013-2050-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ciccotti MG, Lombardo SJ, Nonweiler B, Pink M. Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients: results after long-term follow-up. J Bone Joint Surg Am. 1994;76:1315–21. doi: 10.2106/00004623-199409000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Barrett G, Stokes D, White M. Anterior cruciate ligament reconstruction in patients older than 40 years: allograft versus autograft patellar tendon. Am J Sports Med. 2005;33:1505–12. doi: 10.1177/0363546504274202. [DOI] [PubMed] [Google Scholar]
- 4.Wierer G, Runer A, Hoser C, Herbst E, Gfoller P, Fink C. Acute ACL reconstruction in patients over 40 years of age. Knee Surg Sports Traumatol Arthrosc. 2017;25:1528–34. doi: 10.1007/s00167-016-4363-z. [DOI] [PubMed] [Google Scholar]
- 5.Legnani C, Terzaghi C, Borgo E, Ventura A. Management of anterior cruciate ligament rupture in patients aged 40 years and older. J Orthop Traumatol. 2011;12:177–84. doi: 10.1007/s10195-011-0167-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barber FA, Aziz-Jacobo J, Oro FB. Anterior cruciate ligament reconstruction using patellar tendon allograft: an age-dependent outcome evaluation. Arthroscopy. 2010;26:488–93. doi: 10.1016/j.arthro.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Brandsson S, Kartus J, Larsson J, Eriksson BI, Karlsson J. A comparison of results in middle-aged and young patients after anterior cruciate ligament reconstruction. Arthroscopy. 2000;16:178–82. doi: 10.1016/S0749-8063(00)90033-1. [DOI] [PubMed] [Google Scholar]
- 8.Gee AO, Kinsella S, Huffman GR, Sennett BJ, Tjoumakaris FP. Anterior cruciate ligament reconstruction in patients aged >40 years: a case-control study. Phys Sportsmed. 2013;41:30–4. doi: 10.3810/psm.2013.02.1996. [DOI] [PubMed] [Google Scholar]
- 9.Viola R, Vianello R. Intra-articular ACL reconstruction in the over-40-year-old patient. Knee Surg Sports Traumatol Arthrosc. 1999;7:25–8. doi: 10.1007/s001670050116. [DOI] [PubMed] [Google Scholar]
- 10.Barber FA, Elrod BF, McGuire DA, Paulos LE. Is an anterior cruciate ligament reconstruction outcome age dependent? Arthroscopy. 1996;12:720–5. doi: 10.1016/S0749-8063(96)90177-2. [DOI] [PubMed] [Google Scholar]
- 11.Desai N, Bjornsson H, Samuelsson K, Karlsson J, Forssblad M. Outcomes after ACL reconstruction with focus on older patients: results from The Swedish National Anterior Cruciate Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2014;22:379–86. doi: 10.1007/s00167-013-2803-6. [DOI] [PubMed] [Google Scholar]
- 12.Singh J, Sloan JA, Johanson NA. Challenges with health-related quality of life assessment in arthroplasty patients: problems and solutions. J Am Acad Orthop Surg. 2010;18:72–82. doi: 10.5435/00124635-201002000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22:632–44. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 14.Kinugasa K, Mae T, Matsumoto N, Nakagawa S, Yoneda M, Shino K. Effect of patient age on morphology of anterior cruciate ligament grafts at second-look arthroscopy. Arthroscopy. 2011;27:38–45. doi: 10.1016/j.arthro.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 15.Reeves ND. Adaptation of the tendon to mechanical usage. J Musculoskelet Neuronal Interact. 2006;6:174–80. [PubMed] [Google Scholar]
- 16.Waugh CM, Blazevich AJ, Fath F, Korff T. Age-related changes in mechanical properties of the Achilles tendon. J Anat. 2012;220:144–55. doi: 10.1111/j.1469-7580.2011.01461.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shelbourne KD, Stube KC. Anterior cruciate ligament (ACL)-deficient knee with degenerative arthrosis: treatment with an isolated autogenous patellar tendon ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 1997;5:150–6. doi: 10.1007/s001670050043. [DOI] [PubMed] [Google Scholar]
- 18.Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013;25:165–73. doi: 10.5792/ksrr.2013.25.4.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.