1. Introduction
Acute patellar dislocations, most commonly in the lateral direction, carry high risk of recurrent patellar instability. The medial patellofemoral ligament (MPFL) is one of multiple ligaments found surrounding the patella and is one of the primary stabilizers of the patella. Up to 94–100% of patients suffer from medial patellofemoral ligament rupture after first time patellar dislocation.1 Due to a six degree valgus angle between the femur and tibia in the coronal plane along with a similar angle between the trochlear groove and the tibial tubercle, there is a lateral force vector acting on the patella with the contraction of the quadriceps.2 The primary role of the MPFL1 is to resist this lateral migration of the patella and to keep the patella centered within the patellofemoral groove.
The MPFL is the primary ligamentous restraint of the patella, providing 50–60% of the restraining force against lateral displacement.3 It is most effective between 0–30° of flexion, with the trochlea becoming the primary restraint to lateral migration beyond this range. The MPFL is most commonly injured during lateral patellar dislocation. This typically occurs when the foot is planted and an internal rotatory force is applied to the flexed knee in valgus.4 It is the most important structure that is injured in cases of acute dislocation of the patella.5
2. Anatomy
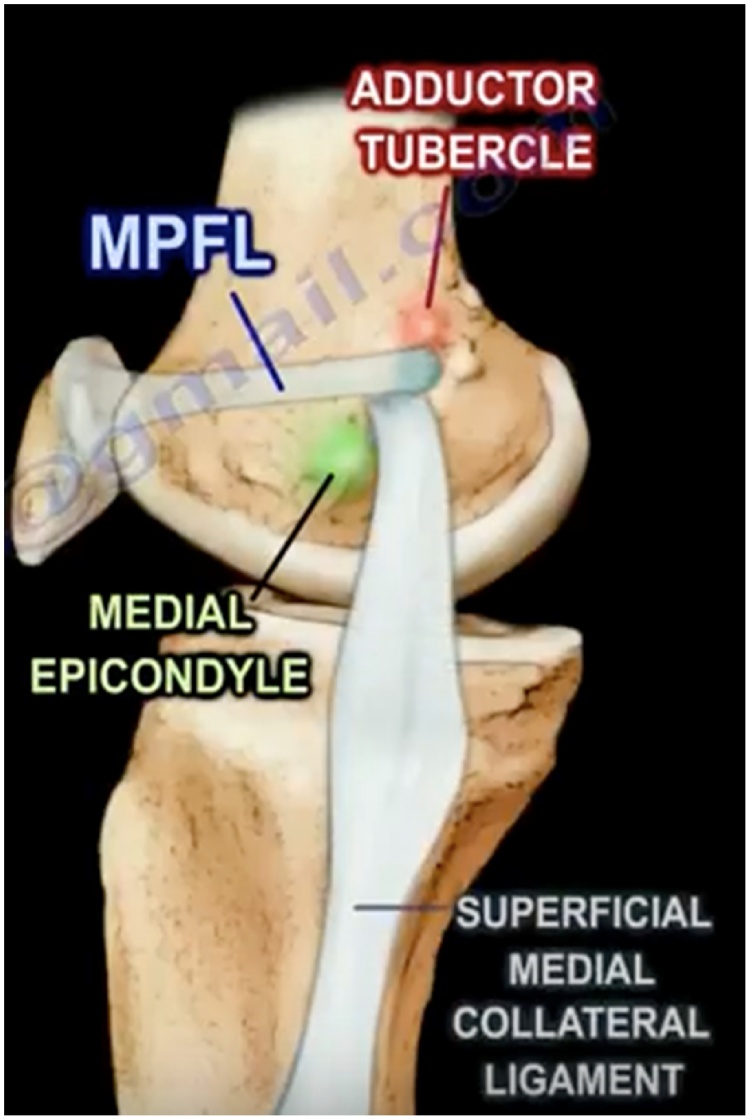
The MPFL is located within layer two of the three soft tissue layers of the medial aspect of the knee.2 It originates between the medial epicondyle of the femur and the adductor tubercle, superior to the superficial medial collateral ligament origin (Fig. 1). The patellar attachment occupies 2/3 of the proximal patellar border in 56.9% of cases, the proximal half in 41.2%, the distal end in 1.3% and extends across the entire patella in 1.3% of patients.6,7 The proximal insertion of the MPFL extends to the quadriceps tendon while distally the ligament passes deep to the distal vastus medialis obliquus (VMO) that also inserts on the medial border of the patella. The MPFL contacts the aponeurosis of the vastus intermedius as well as the VMO2. This creates an anatomical aponeurosis that is important for medial patellofemoral joint stability, as it facilitates a dynamic system that guides and pushes the patella into the trochlear groove during active flexion.6,7
Fig. 1.
Medial view of the tibial-femoral articulation highlighting the femoral insertion of the MPFL inferior to the adductor tubercle of the femur, but superior to the medial epicondyle of the femur.
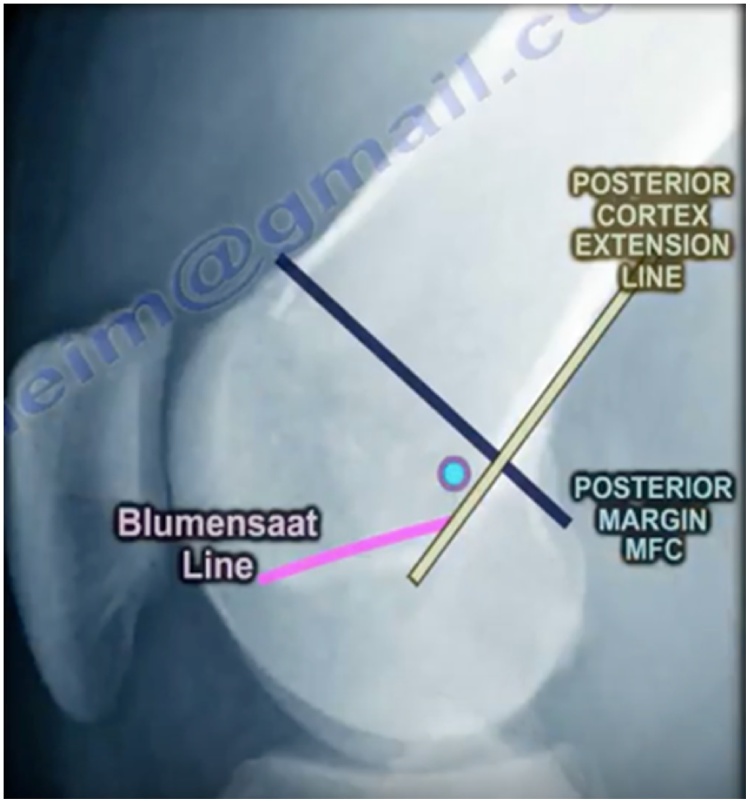
The location of the ligament’s origin can be identified radiographically at “Schottle’s point.”8 On a lateral x-ray, this is found anterior to the intersection of the posterior femoral cortical line and the posterior margin of the medial femoral condyle or anterior to the posterior cortex of the femur and proximal to Blumensaat’s line (Fig. 2). It is found one millimeter anterior to the posterior cortical line, 2.5 mm distal to the posterior margin of the medial femoral condyle, and proximal to the level of the posterior point of Blumensaat’s line.
Fig. 2.
Lateral view of “Schottle’s point” which represents the femoral insertion of the MPFL. It is located just distal and anterior to the intersection of the posterior femoral cortical line and posterior margin of the medial femoral condyle.
3. Etiology
The incidence of primary patellar dislocation is 6 in every 100,000 and may approach 29 in 100,000 in patients between 10 and17 years of age.9,10 Lateral patellar dislocations occur frequently in teenage athletes and young adults, with patients younger than 20 years of age being at the highest risk. Taller adolescent females appear to be at increased risk compared to a shorter age-matched cohort. Overweight males and children younger than 15 are at high risk for recurrence.4,11 Other predisposing factors for patellar dislocation may include patella alta, lateral patellar tilt, trochlear dysplasia, increased Q-angle, genu valgum, vastus medialis muscle hypoplasia, ligament hyperlaxity, external tibial torsion, subtalar joint pronation and increased femoral anteversion.3,12
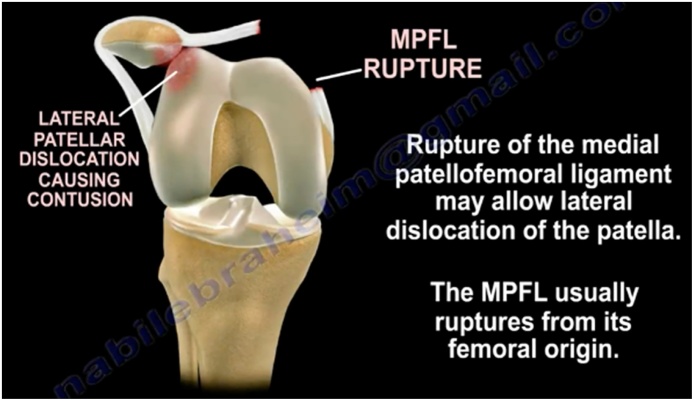
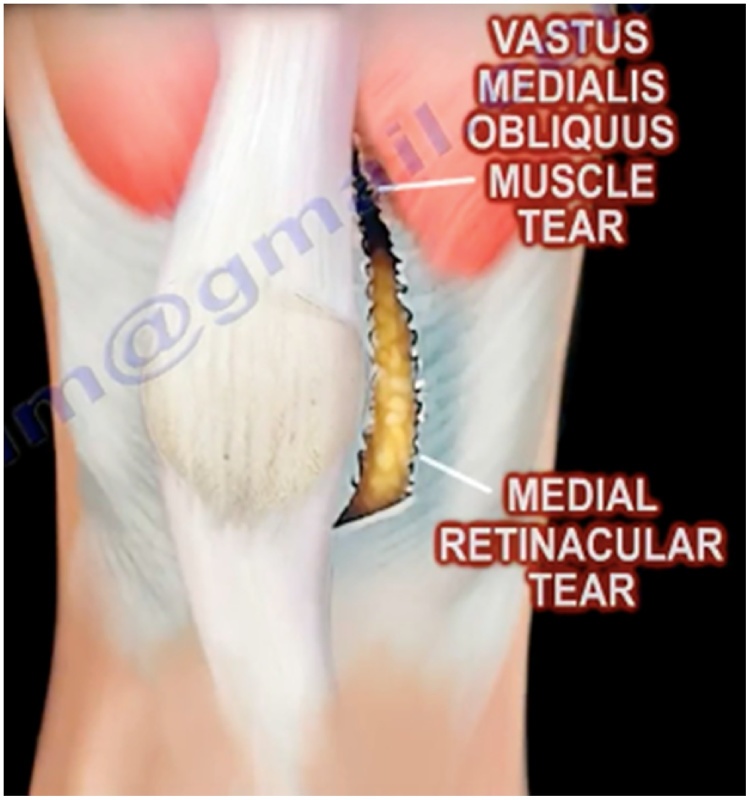
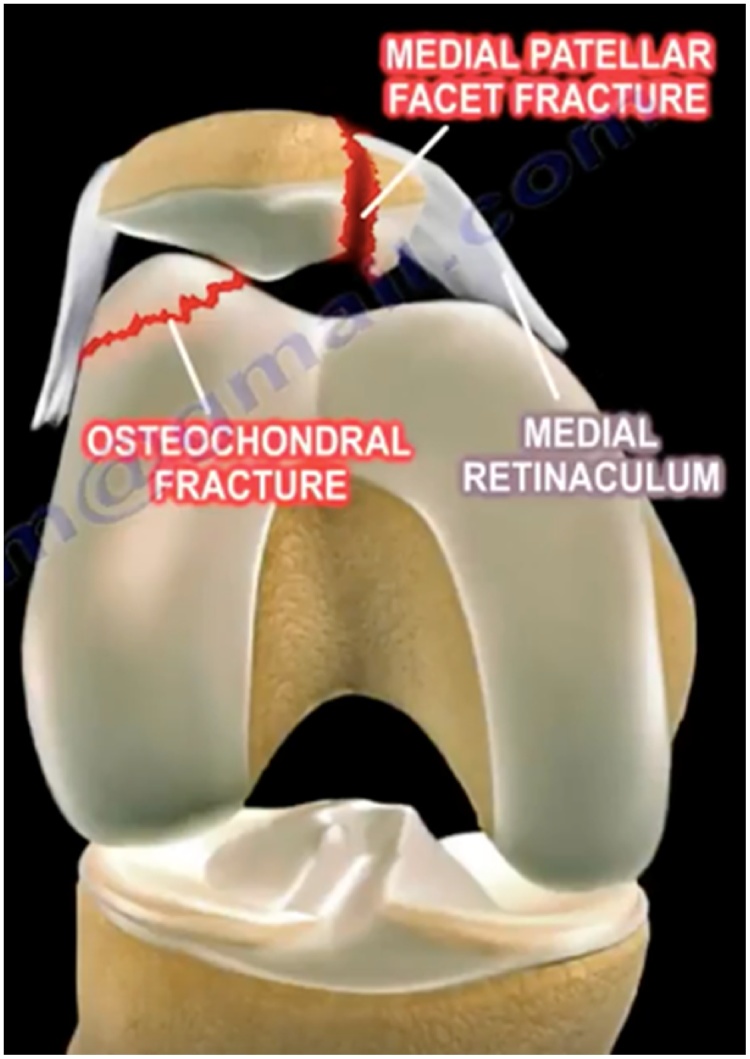
Rupture of the MPFL typically occurs at the femoral origin, resulting in lateral dislocation with injury to the medial patella and lateral femoral condyle (Fig. 4). Associated tearing of the VMO and the medial retinaculum may also occur with dislocation of the patella, as the MPFL and VMO share common meshing fibers (Fig. 5).1 Additionally, osteochondral fractures may be seen with dislocation as the trochlea of the patella impacts the femur (Fig. 6).
Fig. 4.
Bony contusion patterns commonly observed with lateral patellar dislocations.
Fig. 5.
Anterior depiction of the right knee illustrating associated tearing of the medial retinaculum and vastus medialis obliquus muscle following disruption of the MPFL.
Fig. 6.
Medial patellar facet fracture and lateral osteochondral injury as a result of lateralization of the patella due to MPFL mechanism disruption.
4. Clinical presentation
Acutely, patients with MPFL rupture will present with pain and tenderness along the medial retinaculum. They typically have a large hemarthrosis and tenderness to palpation at the medial border of the patella or at the ligament’s femoral origin. There may also be a block to motion should a displaced osteochondral fragment be present.13 In addition to patellar instability, the presence of apprehension with lateralization of the patella and the absence of a firm end point to lateral translation suggests previous dislocation and damage to the MPFL.14
MPFL injuries have been classified into four categories based on location either at the level of the MPFL patellar insertion, within the midsubstance of the ligament, at the femoral origin, or in more than one location.1 Patellar insertion MPFL injuries can be further subdivided into three categories: type P0 with purely ligamentous disruption, type P1 with a bony avulsion fragment, and type P2 with bony avulsion involving the articular surface from the medial facet of the patella.15
5. Diagnosis
Rupture of the MPFL can be diagnosed by lateral and sunrise view radiographs along with MRI for identification of associated soft tissue injury or bony contusions. Lateral subluxation of the patella will be seen on sunrise views with tearing of the MPFL (Fig. 3). MRI is particularly useful in demonstrating the specific region of the MPFL that is injured. As previously mentioned, injury patterns have been identified and categorized into 4 types based on MRI findings: injuries located at the patellar insertion, within the mid-substance, at the femoral origin or injury in multiple locations.16 MRI appears to be more accurate than arthroscopy in identifying femoral disruption of the MPFL and has proven a reliable test for the detection of injury patterns with a sensitivity and accuracy of 85% and 80%, respectively, when compared to open exploration.1,3,16 While there is still no definitive evidence that primary MPFL repair following first-time dislocation reduces the incidence of recurrent dislocation, determination of the site of injury is crucial to achieve satisfactory results.
Fig. 3.
Sunrise view radiograph of a lateral patellar dislocation with associated MPFL disruption.
6. Treatment
Conservative management has traditionally been widely regarded as the most appropriate treatment after an initial lateral patellar dislocation. In general, rehabilitation with physical therapy and bracing tends to be the mainstay of treatment, and surgical interventions are employed upon failure of non-operative management. Late MPFL reconstruction with an autologous tendon has been widely accepted for the treatment of chronic patellar instability caused by MPFL dysfunction. Although first-time traumatic patellar dislocations have traditionally been treated non-operatively, there has been a recent increase in the rate of initial surgical management in the acute setting due to high rates of redislocation and findings of late symptoms such as anterior knee pain.1
While conservative treatment after a first-time dislocation is typically pursued, several circumstances may warrant surgical intervention. These include the presence of osteochondral fragments suitable for repair, significant cartilage damage, disruption of the medial ligamentous stabilizers with subluxation of the patella and normal patellar tracking in the contralateral knee, or in instances of substantial disruption of the MPFL-VMO mechanism.12 MPFL reconstruction may be a more reliable method of stabilizing the patella than MPFL repair, which has limitations related to MPFL injury location.1 Failure to reconstruct the medial structures, including the MPFL, can result in a high risk of recurrent dislocation and suboptimal outcomes following patellar dislocation.5 Other causes of patellar instability may need to be addressed at the time of ligamentous repair in order to improve outcomes. These causes may include the previously mentioned anatomic factors such as trochlear dysplasia and patella alta that can predispose a patient to recurrent patellar instability regardless of MPFL injury location.15
When indicated, a number of different procedures can be undertaken in order to surgically correct an MPFL disruption and subsequent patellar instability. Among the most common are chondroplasty, tibial or femoral osteotomy, tendon transfers, MPFL repair, or MPFL graft reconstruction. Chondroplasty and osteotomies are performed primarily in the setting of underlying anatomic abnormalities that have led to patellar instability. These techniques do not address some of the primary pathology of traumatic patellar instability, such as medial retinaculum damage.17 Many surgeons recommend primary osseous procedures with or without MPFL reconstruction in the setting of high-grade trochlear dysplasia.18
As mentioned above, reconstruction of the MPFL is indicated with recurrent patellar instability following dislocation or failure of conservative management.18 Graft reconstruction recreates the passive restraint to lateral displacement of the patella by utilizing bone tunnels and/or anchors for graft fixation on the patella. Complications such as implant breakage, patellar fracture through bone tunnels, and loss of motion have all been described with reconstruction procedures.19
A number of MPFL reconstruction techniques have been described with no general consensus as to which is best. Several different types of grafts have been described in the literature, including semitendinosus, gracilis, quadriceps or adductor magnus tendons, part of the patellar tendon, allografts, and synthetic grafts. Hamstring grafts consisting of semitendinosus tendon are currently the most commonly utilized type of graft and can be single or double bundle.18,19 Although the gracilis tendon is weaker than the semitendinosus tendon, its strength is sufficient for reconstructive procedures and the stiffness is similar to that of the native MPFL.7 In recent times, using a portion of the quadriceps tendon for ligamentous reconstruction has been popularized. This option may be better for patients with trochlear dysplasia and the gross morphological appearance of the “MPQFL” more closely resembles the native MPFL than a hamstring graft.17,19 Harvesting of quadriceps tendon grafts has traditionally resulted in less cosmetic surgical scars, but newer subcutaneous harvesting techniques have reduced these concerns.19 In general, the literature demonstrates that reconstruction of the MPFL provides equal or superior functional outcomes to other operative techniques, with less peri-operative morbidity and fewer complications.20
7. Summary
The MPFL is one of the primary ligamentous stabilizers of the patella, playing an essential role in resisting the natural lateral migration of the patella. It is often ruptured in patellar dislocations, especially lateral dislocations occurring in younger patients subjecting the flexed knee to inward twisting forces. Disruption of the MPFL most commonly occurs from its femoral origin, but injuries of the mid-substance region and patellar insertion may be seen as well. The clinical presentation of lateral patellar instability along with lateral migration of the patella on sunrise view x-rays can be used to diagnose MPFL disruption, with MRI and arthroscopy being used as more specific means of determining ligamentous injury. Injury to the MPFL can result in an increased risk for future patellar instability and recurrence of patellar dislocation. For this reason, surgical repair or reconstruction of the MPFL has been gaining attention, although further clinical studies are needed to demonstrate the long-term benefits of surgical versus non-operative management. Successful surgical outcomes are seen with various types of grafts for reconstruction, with no general consensus as to which specific type is best.
Conflict of interests
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Medial Patellofemoral Ligament
Vastus Medialus Obliquus
Contributor Information
Collin Krebs, Email: john.krebs@rockets.utoledo.edu.
Meaghan Tranovich, Email: meaghan.tranovich@utoledo.edu.
Kyle Andrews, Email: kyle.andrews@utoledo.edu.
Nabil Ebraheim, Email: nabil.ebraheim@utoledo.edu.
References
- 1.Panni A.S., Vasso M., Cerciello S. Acute patellar dislocation. What to do? Knee Surg Sport Traumatol Arthrosc. 2013;21(2):275–278. doi: 10.1007/s00167-012-2347-1. [DOI] [PubMed] [Google Scholar]
- 2.Guerrero P., Li X., Patel K., Brown M., Busconi B. Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: an MRI study. Sport Med Arthrosc Rehabil Ther Technol. 2009;1(1):17. doi: 10.1186/1758-2555-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sillanpaa P.J., Maenpaa H.M. First-time patellar dislocation: surgery or conservative treatment? Sport Med Arthrosc. 2012;20(3):128–135. doi: 10.1097/JSA.0b013e318256bbe5. [DOI] [PubMed] [Google Scholar]
- 4.Sillanpaa P., Mattila V.M., Iivonen T., Visuri T., Pihlajamaki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–611. doi: 10.1249/MSS.0b013e318160740f. [DOI] [PubMed] [Google Scholar]
- 5.Mochizuki T., Nimura A., Tateishi T., Yamaguchi K., Muneta T., Akita K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sport Traumatol Arthrosc. 2013;21(2):305–310. doi: 10.1007/s00167-012-1993-7. [DOI] [PubMed] [Google Scholar]
- 6.Placella G., Tei M., Sebastiani E. Anatomy of the medial patello-femoral ligament: a systematic review of the last 20 years literature. Musculoskelet Surg. 2015;99(2):93–103. doi: 10.1007/s12306-014-0335-y. [DOI] [PubMed] [Google Scholar]
- 7.Kyung H.-S., Kim H.-J. Medial patellofemoral ligament reconstruction: a comprehensive review. Knee Surg Relat Res. 2015;27(3):133–140. doi: 10.5792/ksrr.2015.27.3.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 9.Colvin A.C., West R.V. Patellar instability. J Bone Jt Surg Am. 2008;90(12):2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 10.Smith T.O., Song F., Donell S.T., Hing C.B. Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sport Traumatol Arthrosc. 2011;19(6):988–998. doi: 10.1007/s00167-010-1355-2. [DOI] [PubMed] [Google Scholar]
- 11.Hsiao M., Owens B.D., Burks R., Sturdivant R.X., Cameron K.L. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38(10):1997–2004. doi: 10.1177/0363546510371423. [DOI] [PubMed] [Google Scholar]
- 12.Stefancin J.J., Parker R.D. First-time traumatic patellar dislocation. Clin Orthop Relat Res. 2007;455:93–101. doi: 10.1097/BLO.0b013e31802eb40a. [DOI] [PubMed] [Google Scholar]
- 13.Laidlaw M.S., Diduch D.R. Current concepts in the management of patellar instability. Indian J Orthop. 2017;51(5):493–504. doi: 10.4103/ortho.IJOrtho_164_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh J.L., Stewart C. Patellar instability. Clin Sports Med. 2014;33(3):461–476. doi: 10.1016/j.csm.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Sillanpää P.J., Salonen E., Pihlajamäki H., Mäenpää H.M. Medial patellofemoral ligament avulsion injury at the patella: classification and clinical outcome. Knee Surg Sport Traumatol Arthrosc. 2014;22(10):2414–2418. doi: 10.1007/s00167-014-3174-3. [DOI] [PubMed] [Google Scholar]
- 16.Balcarek P., Walde T.A., Frosch S., Schüttrumpf J.P., Wachowski M.M., Stürmer K.M. MRI but not arthroscopy accurately diagnoses femoral MPFL injury in first-time patellar dislocations. Knee Surg Sport Traumatol Arthrosc. 2012;20(8):1575–1580. doi: 10.1007/s00167-011-1775-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teitge R.A., Torga-Spak R. Medial patellofemoral ligament reconstruction. Orthopedics. 2004;27(10):1037–1040. doi: 10.3928/0147-7447-20041001-09. [DOI] [PubMed] [Google Scholar]
- 18.Amin N.H., Lynch T.S., Patel R.M., Patel N., Saluan P. Medial patellofemoral ligament reconstruction. JBJS Rev. 2015;3(7):e3. doi: 10.2106/JBJS.RVW.N.00089. [DOI] [PubMed] [Google Scholar]
- 19.Fink C., Veselko M., Herbort M., Hoser C. MPFL reconstruction using a quadriceps tendon graft part 2: Operative technique and short term clinical results. Knee. 2014;21(6):1175–1179. doi: 10.1016/j.knee.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Howells N.R., Barnett A.J., Ahearn N., Ansari A., Eldridge J.D. Medial patellofemoral ligament reconstruction: a prospective outcome assessment of a large single centre series. J Bone Jt Surg Br. 2012;94(9):1202–1208. doi: 10.1302/0301-620X.94B9.28738. [DOI] [PubMed] [Google Scholar]