Abstract
This article aims to provide a systematic review of the limited literature and clinical knowledgebase available on the Hoffa fractures. It is inclusive of the normal anatomy, pathology, diagnosis, treatment options comprising of non-operative and operative protocols, and postoperative findings.
Keywords: Hoffa, Fracture, Review, Lateral, Femoral, Condyle, Coronal
1. Introduction
The Hoffa fracture of the distal femur is a rare injury described as a coronal fracture of the femur involving one or both of the condyles. The distal, condylar end of the femur has a trapezoid shaped anatomy and articulates with both the tibial plateau and the patella. Before Albert Hoffa described the fracture pattern in 1904, the initial descriptions of this fracture can be traced back to 1869 where it was first documented by Busch.6 These fractures are quite rare and often go unobserved during the routine assessment of distal femur fracture. The surgeon must have a high index of suspicion to investigate for coronal plane fracture.2 In fact, the occurrence of isolated femoral condylar fractures is about 0.65% of all femoral fractures.7 Among the different possible types of Hoffa fractures, lateral condylar and bilateral condylar fractures are more common than medial condylar fractures.8 Lateral condylar fractures account for about 78%–85% of Hoffa fractures.5,8 After radiographic identification of the Hoffa fracture, the injury should be classified. As per the AO/OTA classification, Hoffa fractures are Type 33-B3 injuries, and according to Letenneur these are classified as Type I injury.9 The Letenneur classification scheme illustrates the different fractures (Fig. 1).
Fig. 1.
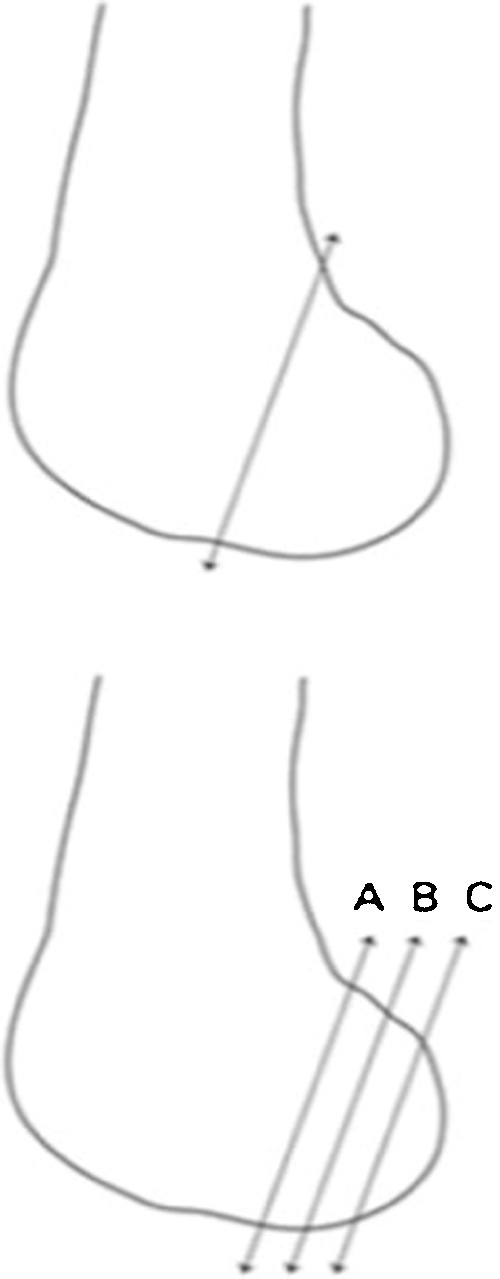
The Letenneur classification scheme for Hoffa fractures.
Hoffa fractures tend to be associated with high-energy trauma injuries such as motor vehicle accidents, which exert an axial load on a flexed knee. They involve the intra-articular portion of a major weight-bearing joint, and are at significant risk of displacement.10 Due to the nature and location of the injury, the fracture tends to be missed on initial standard radiographic evaluation. For example, in 82% of distal femoral condylar fractures, the fracture line was sagittal, which could be identified easily on an anteroposterior (AP) radiograph, whereas 18% of fractures were coronal and not readily apparent.11 Therefore, a computed topography (CT) scan is required to understand fully the anatomy of the distal femur and investigate for coronol fracture lines.2,12 Interestingly the current literature available on the Hoffa fracture is comprised mostly of case reports and single-center studies. The goal of this article is to provide a systematic review of the literature on Hoffa fractures.
2. Anatomy and injury assessment
Isolated occurrences of the Hoffa fracture are quite rare, as they tend to be associated with high-energy impacts and involve other bone and soft tissue injuries. Motor vehicle collisions accounted for four out of five cases in one study, and they are a major mechanism that result in Hoffa injuries partly due to the flexed knee position of a driver.13 Nork et al reports that from 77 supracondylar-intercondylar fractures, 80.5% were associated with motor vehicle collisions, whereas only 9.1% resulted from falling from a height.8 However, sports and other activities where combined rotational and axial forces are applied to the knee joint may also contribute to the injury. Arastu et al suggest that a possible reason for the fracture could be the application of force in the vertical plane on the posterior femoral condyle corresponding to varying degrees of a flexed knee.3 Another study by Manfredini et al indicates that the trochlear-condylar groove may be a potential structurally unstable point where the fracture could originate and spread into other planes. The normal valgus physiology of the knee joint may further contribute to an abduction force against the tibial plateau, which could explain the higher frequency of lateral condylar fractures.7,13 However, the exact mechanism of the injury remains unclear.
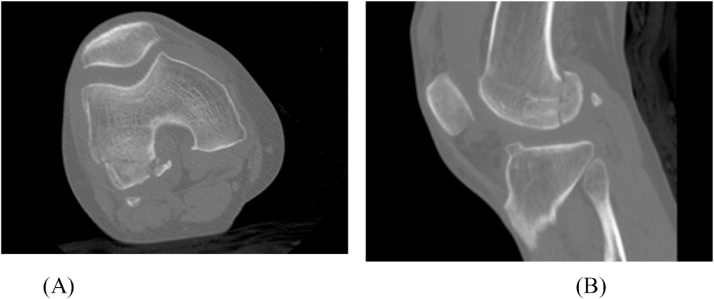
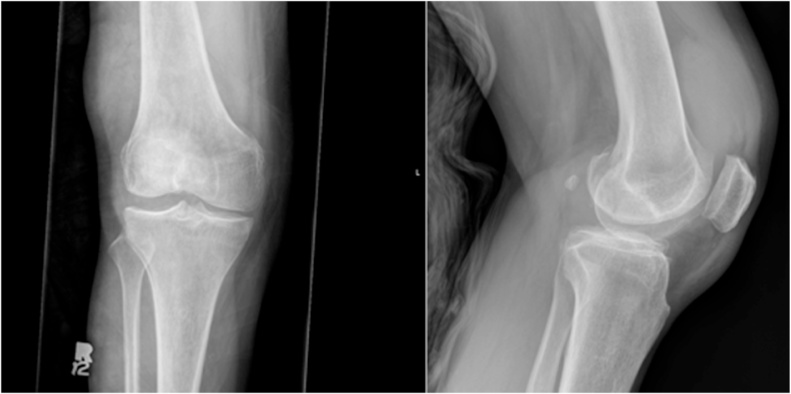
Assessment of injuries associated with motor vehicle collisions often fails to diagnose Hoffa fractures. One study of 95 Hoffa cases indicates that only 69% of them were identified on radiographs, while 10 of them (without use of CT scan) were identified intra-operatively.8 About 25% of Hoffa fracture are undiagnosed on initial exam with plain radiographs.8 It is important to have a high index of suspicion in order to diagnose the fracture. Of the six patients evaluated by Dhillon et al, only one was diagnosed without the use of CT scan, and one patient required x-ray, CT, and MRI for diagnosis.5 Fig. 2, Fig. 3 illustrate the presence of Hoffa fractures on CT imaging as well as AP and lateral radiographs. In one instance, an AP radiograph obtained to assess the cause of knee pain and tenderness looked normal until the lateral view revealed a coronal fracture.14 A report by Thakar identified a trauma patient that was evaluated by routine radiographs and surgically treated for forearm and humerus fractures. However, the consistent pain and effusion observed in the patient’s knee lead to the discovery of a Hoffa fracture in the left knee two day postoperatively.12 Patients with a Hoffa fracture should also be diagnosed for trauma to the pelvis, hip, patella, tibial plateau, femur shaft, popliteal vessels, and ligament tears of the knee.2,3,12
Fig. 2.
A computed topography image of the Hoffa fracture with (A) coronal and (B) sagittal planes depicting the lateral fragments.
Fig. 3.
AP and lateral radiographs showing Hoffa fragments.
3. Management and treatment
The location and nature of the Hoffa fracture often complicated management decisions when considering non-surgical treatment or surgical approaches. One of the first steps of management is the need to assess injury to other organ systems with general surgery colleagues before proceeding with management of distal femur fractures.15 Due to its intraarticular nature, open reduction and internal fixation is required for successful treatment of the Hoffa fracture. Most published case studies indicate that non-surgical treatment of the fragment leads to poor results. For example, one study where non-surgical approach was used for 5% of the 154 Hoffa fracture patients resulted in poor outcomes and displacement of fragment resulting from the treatment.11 Nonunion may result if the nondisplaced fragment is treated conservatively.5,10 However, one study reported on a medial condylar fracture treated with knee bracing and protective weight bearing which yielded a good result.16
4. Surgical techniques
Some of the general principles indicated for surgical treatment of distal femoral fractures highlight the importance of assessing whether the fracture involves intra-articular surface. If the fracture does involve a joint, the initial priority should be to reconstruct and repair the articular site. Furthermore, the rotation and length should be properly controlled while treating the condylar region in the sagittal or coronal plane.17 Open reduction and internal fixation is the dominant treatment strategy for Hoffa fractures and has yielded satisfactory results in appropriate time periods. A variety of techniques and equipment have been discussed in the literature, most of which refer to treatment of distal femur fractures. The surgical approach relies on the location of the injury and presence or absence of a posterior comminution.
Some of the approaches used and reported frequently include a medial or lateral parapatellar arthrotomy, subvastus approach, arthroscopic approach and a Gerdy’s tubercle osteotomy. A summary of some of the cases described and additional cases of unicondylar Hoffa fractures is presented in Table 1.
Table 1.
Summary of studies reporting unicondylar and bicondylar Hoffa fractures.
| Authors | Cases | Surgical Approach | Fixation Method | Postoperative Treatment | Outcomes | Complications |
|---|---|---|---|---|---|---|
| Holmes et al13 | 5: 2 lateral, 3 medial | MPPA or LPPA | 3.5mm AP parallel screws | Limited WB initially, full WB at 10 weeks. Unrestricted ROM exercise regiment | Mean Knee Society Score: 173 (160-180). | None |
| Manfredini et al7 | 19 distal femur fractures: 6 Hoffa injuries | Medial or lateral incision | – | Articulated splint for mean 25 days. CPM after 96 hours post-op. WB at 70 days. | – | – |
| Miyamoto et al22 | 1 medial + ipsilateral femoral shaft fracture | – | 2 3.5mm cortical screws applied AP | ROM exercises from day 1 post-op. Non-WB till 6 weeks | Percutaneous case: ROM 0º to 100º. Revised open case: 0º to 110º. | Revision for open case due to fracture displacement |
| Lewis et al10 | 7 lateral | Direct lateral between ITB and B. Femoris or MPPA | 2 non-paralle PTCS. Small + large fragment screws | 2 week extended cylinder cast | Non-operative: 1-Fair. Operative: 2 good, 3 fair. | None |
| Sahu et al28 | 22: 6 bilateral unicondylar, 7 bicondylar, 8 supracondylar | Medial or lateral incision | Reduction and Fixation using K wires and screws | Touch-down WB started 2nd day post-op. | – | 1 case each of malunion, delayed union, knee stiffness, arthritis, ligament laxity |
| Kone et al26 | 1: Bilateral medial condylar | Nonoperative: Immobilization of knees for 4 weeks. Physiotheraphy at 6weeks | – | – | Excellent with normal flexion. Absence of laxity or pain | – |
| Agarwal et al19 | 1: Bicondylar | Lateral incision | Revisional reconstruction with small fragment screws and LISS-DF device | Unrestricted active or passive movements+touch WB encouraged | ROM from 10º to 100º | – |
WB: Weight Bearing.
MPPA/LPPA: Medial/Lateral parapatellar approach.
LISS-DF: Less Invasive Stabilisation System–—Distal Femur; Synthes.
ITB: Iliotibial Band.
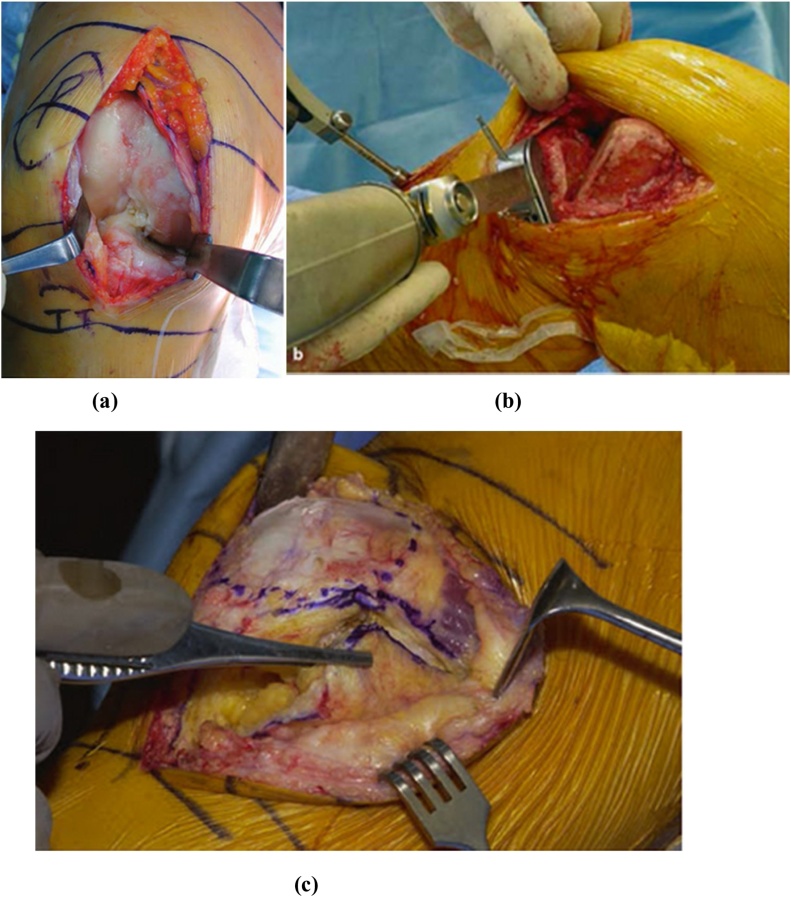
Many studies have utilized a general lateral or a medial parapatellar incision to access the anterior femur 10,13 (Fig. 4). A medial parapatellar approach seems to be the most frequently reported approach.11,13 Although this approach allows visualization of the anterior surface without compromising future arthroplasty surgery, it inhibits the view of the posterior femur thereby preventing treatment.3 A multicenter study of 154 patients with condylar fractures contained 18 patients with the B3 Hoffa injury. 78% of the 18 patients were treated using antero-medial or antero-lateral approach while 22% with postero-lateral or postero-medial approach. The fixation majorly relied on insertion of screws either anteriorly or posteriorly.11 Dhillon et al presented six Hoffa cases, four of which were treated with a medial parapatellar arthrotomy, and other two with a lateral parapatellar arthrotomy. The instruments used for fixation varied from 7.0 mm partially threaded cancellous screws to a lateral femoral locking plate. These methods allowed for a proper reduction and fixation to be achieved.5 Another study reported by Gavaskar et al used a medial parapatellar incision regardless of the location of the Hoffa fragment. 4.0 mm screws were used in the AP approach whereas 2.4 mm headless screws were used in the PA direction while avoiding damage to the fat pad and meniscal attachments.18
Fig. 4.
(a) Medial and (b) lateral parapatellar incisions 29,30 and (c) illustrating the subvastus approach frequently used to prevent damage to quadriceps tendon 30.
Agarwal et al reported a revision surgical intervention using a lateral parapatellar approach of poorly treated double Hoffa fracture which was then treated with a small fragment screw and a LISS-DF (Less Invasive Stabilisation System–Distal Femur; Synthes) plate to regain a post-operative range of motion from 10 to 100 degrees. The revision surgery revealed both Hoffa fractures along with inter-articular fragments. 3.5 mm screws were used to reconstruct the fragment antero-posteriorly while the distal articular fragment was reduced using 3.5 mm screws latero-medially. The fracture was then stabilized using the LISS-DF device.19
A unique case-report of a 14-year-old patient who presented with a severe horizontal rotation of the patella combined with a lateral femoral condylar fracture. On presentation, the patient had a locked knee in the flexed position and was unable to perform straight leg raise or any movements concerning the knee joint. Initially, the patella was freed from the intercondylar notch to achieve normal joint function. Then, the Hoffa fracture was approached using a lateral parapatellar approach and 0.065 mm K wires in order to achieve reduction. Two bio-compression screws and a cannulated screw were used to achieve satisfactory fixation. An allograft bone was also used to treat the articular damage.1
A subvastus approach was used by Bali et al to treat a medial unicondylar Hoffa injury. The subvastus approach allows for clear visualization of the distal femur and knee joint region while preserving the vasculature and extensor mechanism. This approach is associated with lower post-operative pain and stronger extensor mechanism. A deep midline incision allows access to the deeper portion of joint under the vastus medialis muscle.20 The posterior fragment was accessed and manipulated using a K (Kirschner) wire in order to achieve reduction. Two, large fragment, cannulated screws were used antero-posteriorly to achieve fixation.9
Viskontas et al 4 described a subvastus approach to access injuries associated with the Hoffa fracture. The infrapatellar branch of the saphenous nerve and the medial genicular vascular bundle are some of the structures at risk when using this approach. Proper visualization of the fracture site can be achieved using this approach and allow for reduction and fixation as visualized in Fig. 4. In case of a displaced fracture, the intraosseous blood supply is likely to be disrupted making it critical to preserve the extraosseous blood supply, which is mainly derived from the superior popliteal artery.
Garofalo et al described a Gerdy tubercle osteotomy in order to access the posterolateral portion of the knee. A 10 mm wide osteotomy parallel to the long tibial axis allows detachment of a 20 mm long and 7–10 mm thick bone flap from Gerdy’s tubercle. Further reflection of the iliotibial tract allows proper access to the posterolateral region to treat a fracture of the lateral femoral condyle. The proximial tibial metaphysis can serve as a source of autologous bone grafts, which could be used to fill bone defects and address depressed articular fragment.21
An arthroscopic approach, although not frequently reported for treatment of Hoffa fractures, is one of the least invasive approaches and allows for minimal soft tissue damage, blood loss, infection rate, and operative time.14 Lal et al reported a unique case of bicondylar Hoffa fractures discovered during an arthroscopically assisted internal fixation of a Type II lateral condylar injury. Guide wires were used to achieve reduction and 4.5 mm cancellous screws were inserted AP to achieve fixation. The knee was then casted to achieve immobilization for 2 weeks. The treatment did not result in any occurrence of avascular necrosis or osteoarthritis.14 A report on a medical condylar fracture associated with a femoral shaft fracture described the use of a shorter femoral nail in order to prevent displacement of the medial condyle. Reduction and fixation was achieved using AP screw placement.22
Minimally invasive approaches such as arthroscopically assisted management of intra-articular fractures have been described.14,23,24 Wallenbock and Ledinski reported on 24 intra-articular knee fractures of which 2 were Hoffa injuries. This approach to reduce and internally fix the fractures arthroscopically proved challenging; however, there were good early results. McCarthy and Parker treated a sagittal plane fracture of the lateral femoral condyle. They were unable to achieve complete satisfactory reduction but noted the reduced soft tissue dissection, blood loss, and operative time, and a faster recovery time. Arthroscopy has been cited useful in the assessment of neglected Hoffa fractures as well as accompanying ligamentous and intra-articular injuries which could be missed during preoperative clinic exam or magnetic resonance imaging.25
5. Postoperative results and management
As summarized in Table I, the outcomes for the various fractures, surgical techniques, and post-op management varied greatly depending on individual treatment strategies. This variation makes it challenging to pinpoint a particular management strategy that will achieve excellent results. Early mobilization seems to be encouraged by most studies to stimulate bone healing and avoid joint stiffness. Some reports allowed weight bearing two days post-operatively, however most preferred a more slowly progressive approach. Complications that occurred post-operatively seem to be more common in bicondylar fixation than unicondylar.
The few studies that used a non-operative approach reported both successful and unsuccessful results.8,26 The multicenter study conducted by Nork et al, attempted non-operative treatment for 5% (n=163) of the cases. Non-operative treatment is recommended for patients with lateral unicondylar fractures with limited functional needs and presence of osteoarthritis.8
6. Future recommendations
The prevalence of Hoffa fractures in high-energy injuries should be watched for with the evaluating surgeon maintaining a high index of suspicion. CT images should be obtained in order to properly diagnose the presence of this injury. Non-operative treatment should be sparingly utilized depending on a case-by-case basis. Open reduction and internal fixation produces satisfactory results for these intraarticular fractures and is the present standard of care. Lateral condylar fractures can be approached using a lateral parapatellar approach,10 swashbuckler approach,27 or Gerdy’s tubercle osteotomy.21 Medical condylar fractures can be approached via a medial parapatellar approach or a subvastus approach.4 Bicondylar fractures can be approached with a combination of the approaches described above. Small fragment screws, lag screws, and staples or pins can be utilized to address fixation.8 The variation among the different aspects of this fracture makes it difficult to outline a specific set of protocols to address the fracture. A large systematic review or a multicenter study may allow for a better understanding of the Hoffa fracture and its treatment.
Disclosure statement/conflict of interest
None of the authors have a financial or proprietary interest in the subject matter or materials discussed, including, but not limited to, employment, consultancies, stock ownership, honoraria, and paid expert testimony.
References
- 1.Potini V.C., Gehrmann R.M. Intra-articular dislocation of the Patella with associated Hoffa fracture in a skeletally immature patient. Am J Orthop (Belle Mead NJ) 2015;44(6):E195–E198. [PubMed] [Google Scholar]
- 2.Baker B., Escobedo E., Nork S. Hoffa fracture: a common association with high-energy supracondylar fractures of the distal femur. AJR Am J Roentgenol. 2002;178(4):994. doi: 10.2214/ajr.178.4.1780994. [DOI] [PubMed] [Google Scholar]
- 3.Arastu M., Kokke M., Duffy P. Coronal plane partial articular fractures of the distal femoral condyle: current concepts in management. Bone Jt J. 2013;95-B(9):1165–1171. doi: 10.1302/0301-620X.95B9.30656. [DOI] [PubMed] [Google Scholar]
- 4.Viskontas D., Nork S., Barei D. Technique of reduction and fixation of unicondylar medial Hoffa fracture. Am J Orthop (Belle Mead NJ) 2010;39(9):424–428. [PubMed] [Google Scholar]
- 5.Dhillon M., Mootha A., Bali K. Coronal fractures of the medial femoral condyle: a series of 6 cases and review of literature. Musculoskelet Surg. 2012;96(1):49–54. doi: 10.1007/s12306-011-0165-0. [DOI] [PubMed] [Google Scholar]
- 6.Bartonicek J., Rammelt S. History of femoral head fracture and coronal fracture of the femoral condyles. Int Orthop. 2015;39(6):1245–1250. doi: 10.1007/s00264-015-2730-x. [DOI] [PubMed] [Google Scholar]
- 7.Manfredini M., Gildone A., Ferrante K. Unicondylar femoral fractures: therapeutic strategy and long-term results. A review of 23 patients. Acta Orthop Belg. 2001;67(2):132–138. [PubMed] [Google Scholar]
- 8.Nork S., Segina D., Aflatoon K. The association between supracondylar-intercondylar distal femoral fractures and coronal plane fractures. J Bone Jt Surg Am. 2005;87(3):564–569. doi: 10.2106/JBJS.D.01751. [DOI] [PubMed] [Google Scholar]
- 9.Bali K., Mootha A., Prabhakar S. Isolated Hoffa fracture of the medial femoral condyle in a skeletally immature patient. Bull NYU Hosp Jt Dis. 2011;69(4):335–338. [PubMed] [Google Scholar]
- 10.Lewis S.L., Pozo J.L., Muirhead-Allwood W.F. Coronal fractures of the lateral femoral condyle. J Bone Jt Surg Br. 1989;71(1):118–120. doi: 10.1302/0301-620X.71B1.2914979. [DOI] [PubMed] [Google Scholar]
- 11.Bel J., Court C., Cogan A. Unicondylar fractures of the distal femur. Orthop Traumatol Surg Res. 2014;100(8):873–877. doi: 10.1016/j.otsr.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Thakar C. The Hoffa fracture--a fracture not to miss. Emerg Med J. 2010;27(5):391–392. doi: 10.1136/emj.2009.087213. [DOI] [PubMed] [Google Scholar]
- 13.Holmes S.M., Bomback D., Baumgaertner M.R. Coronal fractures of the femoral condyle: a brief report of five cases. J Orthop Trauma. 2004;18(5):316–319. doi: 10.1097/00005131-200405000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Lal H., Bansal P., Khare R., Mittal D. Conjoint bicondylar Hoffa fracture in a child: a rare variant treated by minimally invasive approach. J Orthop Traumatol. 2011;12(2):111–114. doi: 10.1007/s10195-011-0133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barei D.P., Schildhauer T.A., Nork S.E. Noncontiguous fractures of the femoral neck, femoral shaft, and distal femur. J Trauma. 2003;55(1):80–86. doi: 10.1097/01.TA.0000046259.43886.25. [DOI] [PubMed] [Google Scholar]
- 16.Mak W., J H., Escobedo E. Hoffa fracture of the femoral condyle. Radiol Case Rep. 2008;3(231) doi: 10.2484/rcr.v3i4.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ehlinger M., Ducrot G., Adam P., Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res. 2013;99(3):353–360. doi: 10.1016/j.otsr.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 18.Gavaskar A.S., Tummala N.C., Krishnamurthy M. Operative management of Hoffa fractures--a prospective review of 18 patients. Injury. 2011;42(12):1495–1498. doi: 10.1016/j.injury.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal S., Giannoudis P.V., Smith R.M. Cruciate fracture of the distal femur: the double Hoffa fracture. Injury. 2004;35(8):828–830. doi: 10.1016/S0020-1383(02)00168-7. [DOI] [PubMed] [Google Scholar]
- 20.Hofmann A.A., Plaster R.L., Murdock L.E. Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;269:70–77. [PubMed] [Google Scholar]
- 21.Garofalo R., Wettstein M., Fanelli G., Mouhsine E. Gerdy tubercle osteotomy in surgical approach of posterolateral corner of the knee. Knee Surg Sports Traumatol Arthrosc. 2007;15(1):31–35. doi: 10.1007/s00167-006-0121-y. [DOI] [PubMed] [Google Scholar]
- 22.Miyamoto R., Fornari E., Tejwani N.C. Hoffa fragment associated with a femoral shaft fracture. A case report. J Bone Jt Surg Am. 2006;88(10):2270–2274. doi: 10.2106/JBJS.E.01003. [DOI] [PubMed] [Google Scholar]
- 23.Wallenbock E., C L. Indications and limits of arthroscopic management of intra-articular fracture of knee joint. Aktuelle Traumatol. 1996;23(97):101. [PubMed] [Google Scholar]
- 24.McCarthy J.J., Parker R.D. Arthroscopic reduction and internal fixation of a displaced intraarticular lateral femoral condyle fracture of the knee. Arthroscopy. 1996;12(2):224–227. doi: 10.1016/s0749-8063(96)90016-x. [DOI] [PubMed] [Google Scholar]
- 25.Ercin E., Bilgili M., Basaran S. Arthroscopic treatment of medial femoral condylar coronal fractures and nonunions. Arthrosc Tech. 2013;2(4):e413–e415. doi: 10.1016/j.eats.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kone S. Hoffa fracture of medial unicondylar and bilateral in a man: a rare case. Pan Afr Med J. 2015;20:382. doi: 10.11604/pamj.2015.20.382.6092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Starr A., Jones A., Reinert C. The "swashbuckler": a modified anterior approach for fractures of the distal femur. J Orthop Trauma. 1999;13(2):138–140. doi: 10.1097/00005131-199902000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Sahu R.L., Gupta P. Operative management of Hoffa fracture of the femoral condyle. Acta Med Iran. 2014;52(6):443–447. [PubMed] [Google Scholar]
- 29.Stiehl James B., Konerman Werner H., Haaker Rolf G., DiGioia Anthony M., III . Springer; Berlin Heidelberg: 2007. Navigation and MIS in orthopedic surgery; pp. 229–244. Retrieved from http://link.springer.com/book. [Google Scholar]
- 30.Scuderi Giles R., Tria Alfred J. Springer; New York: 2010. Minimally invasive surgery in orthopedics; pp. 281–289. [Google Scholar]