Abstract
We report outcomes of using GraftJacket to repair massive rotator-cuff-tears. Twenty patients with a mean age of 64.6y over 12-month duration were reviewed. Two patients had a single GraftJacket repair (group1), whilst 18 had the GraftJacket sheet doubled (group2). Pre and post oxford shoulder scores (OSS) and patient related outcome measures were evaluated. A statistically significant improvement of OSS was demonstrated in-group 2 from a mean of 22 to 45.5 (p < 0.00148) over a follow up of 18 months. GraftJacket is a safe and effective procedure to use as an interpositional graft and doubling the graft may improve outcomes.
Keywords: Rotator cuff, Massive rotator cuff tear, GraftJacket, Irreparable tears, Oxford shoulder score, Interpositional graft
1. Introduction
The management of massive rotator cuff tears (RCT) is a technical challenge to shoulder surgeons.1,2 Inability to mobilize the residual tendon, muscular degeneration and high re-tear rates up to 94%3,4 with poor clinical outcomes5 are reasons why surgical reattachment is difficult to achieve. In elderly patients reverse shoulder arthroplasty can be performed to relieve pain and restore function6. This form of treatment is not acceptable to younger and higher functionally demanding patients. In our institution we have started to use GraftJacket (Wright Medical Technology, Inc., Arlington, TN) as an interpositional device for repairing rotator cuff tears in such patients. Through our early experience we have decided to aim for tissue-matched thickness as we feel this may improve results and report our experience, and patient related outcome measures (PROMS) with this technique.
2. Materials and methods
Twenty-two patients were operated on between 2015 and 2016. The operation was offered to all patients who were symptomatic with pain, an absence of glenuhumeral joint osteoarthritis and where direct repair of the cuff was not possible. The size of the tear did not influence surgery. The first two patients (group 1) operated on had a single layer GraftJacket interpositional repair. However, their immediate post-operative results were poor and so we decided to double the GraftJacket aiming for tissue-matched thickness in all other cases (group 2).
Case notes, operative records, radiographic imaging were reviewed for mode of diagnosis, presence or otherwise of a preceding injury, the size of the tear, previous ipsilateral primary rotator-cuff-repair, preoperative Oxford shoulder scores (OSS), smoking status and surgical complications. PROMS included: Short form health survey (SF-12) with physical composite (PCS) and mental composite scores (MCS). Also assessed was the length of recovery from the time to return to work, driving and satisfaction of the shoulder post surgery using the following devised scoring system 0 = worse, 1 = no improvement, 2 = partly better, 3 = much better, 4 = normal. Postoperative OSS was collected by a combination of self-assessment at follow up and telephone consultations.
The Wilcoxon signed-rank test was used to calculate if there was any correlation between pre- and postoperative OSS. A p-value of 0.05 denoted statistical significance.
3. Operative technique
All patients were operated on by the senior author (TFS), or under his supervision. Patients consented for the use of cadaveric allograft. The technique as described by Modi et al was used. Patients were positioned in the beach chair position under general anesthetic and a brachial plexus block. Intravenous teicoplanin and gentamicin were given on induction.
A superior lateral approach (modified Nevaiser-Mackenzie) was used. The anterior deltoid was detached from the acromion and a periosteal flap created. The long head of biceps was released only if it was dislocated or degenerate, and generous bursectomy performed if there was evidence of hypertrophy or degeneration. The rotator cuff and defect was identified and attempts at converging the tear were made to reduce the size and achieve good tissue tension. Defect dimensions in anterior, posterior and medial-lateral planes were measured using a sterile ruler.
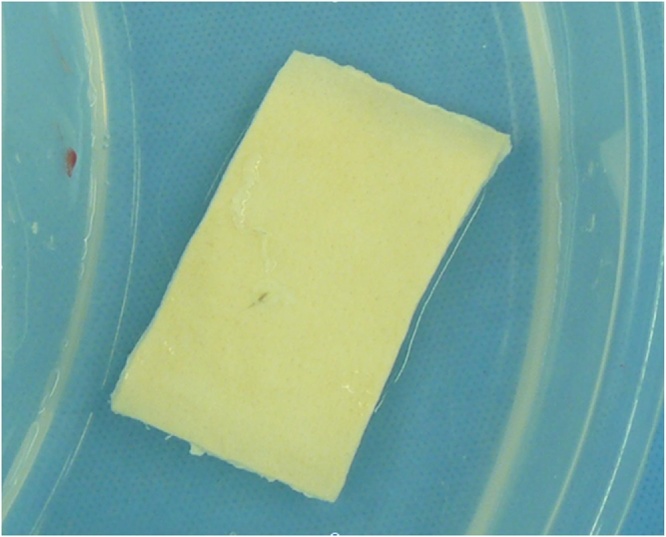
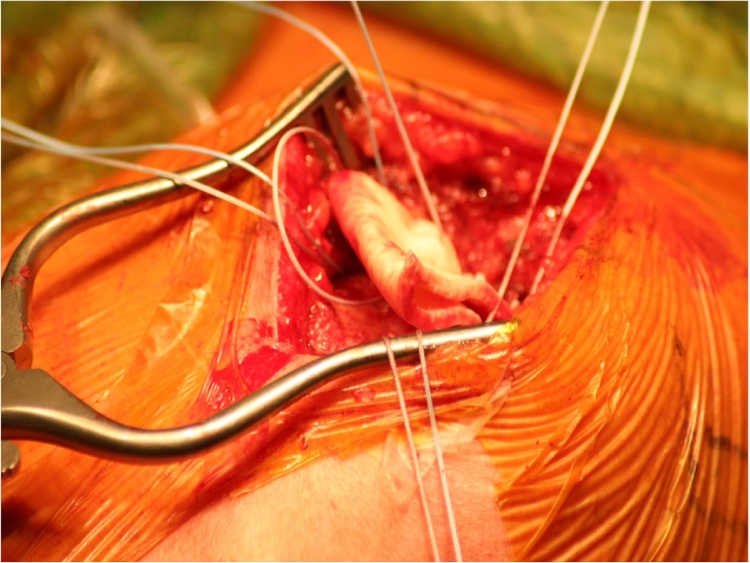
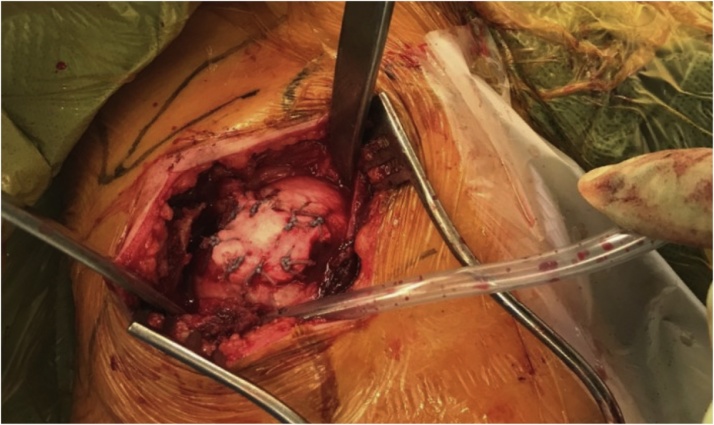
The GraftJacket was prepared by hydrating it in warm sterile saline solution for approximately 15 min (Fig1). After suitable expansion of the GraftJacket, an appropriate size was cut to fill the defect, aiming at tissue-matched thickness (double the graft in majority of cases). We were careful to orientate the GraftJacket appropriately according to manufacturing instructions – smooth side (epidermal basement membrane) facing upwards and dermal side onto the tuberosity. Approximation and fixation of the GraftJacket onto the defect was made using Fibrewire No. 2 sutures, inserted 1 cm apart (Fig2). An anchor was used to secure the GraftJacket with the footprint, after adequate tension had been applied (Fig3). There was no residual defect.
Fig. 1.
GraftJacket hydrated for 15 min.
Fig. 2.
Fixation of GraftJacket with No.2 Fibrewire.
Fig. 3.
GraftJacket secured to the footprint with adequate tension.
The deltoid muscle was repaired anatomically, with transosseous sutures through the acromion. Patients were discharged in a collar and cuff the same day. Postoperative rehabilitation for the first 3 weeks was pendulum exercises and passive movement, for 3–6 weeks gentle stretching and active assisted movements, and after 6 weeks full ROM was permitted together with proprioceptive stretching.
4. Results
Twenty-two patients were operated on between 2015–2016 with two being lost to follow up. There were 16 male and 4 female patients, with a mean age of 64.6 years (39-87y). In twelve patients there was a definite history of trauma. Eighteen patients had pre-operative imaging to diagnose a rotator cuff tear (USS in 16, MRI in 2). Sixteen patients were right hand dominant and an operation on the ipsilateral side. Mean size of tear was 31.5 mm (20–50 mm, size does not include the footprint). Post-operative SF-12 questionnaire scores were performed in 20 patients with a PCS mean of 47.4 (32.8 to 57.7, SD +- 9.19) and MCS of 56.6 (48.6 to 62.9, SD +- 5.48). Both score range from 0 to 100, with 0 being lowest level of health and 100 being the highest level.
In-group 1 there are 2 patients with a mean, age of 53y, tear size of 22.5 mm (20 mm, 25 mm) and follow up of 24.5 months who were treated with a single interpositional GraftJacket repair. Their postoperative OSS was 19 and 26 (mean 12.5).
In-group 2 there are eighteen patients with a mean, age of 65.9y, tear size of 32.5 mm and follow up of 18 months that were treated by interpositional repair of a doubled GraftJacket. Due to insufficient documentation preoperative OSS was found in only thirteen patients. Of these, OSS improved from a mean of 22 (13 to 29, SD +-4.5) to a mean of 45.5 (42 to 48 SD +-2.5), at mean follow up of 17 months, p < 0.00148 Wilcoxon signed-rank test. The mean post-operative OSS of group 2 as a whole was 44.7 (36 to 48, SD +-3.8).
Operative recovery to maximum function was 5 months, 85.7% returned to work in 16 weeks, 93.8% returned to driving in 8 weeks, 90% of patients were overall satisfied with their operation and post-operative results, and 95% would recommend this operation to a family member or friend.
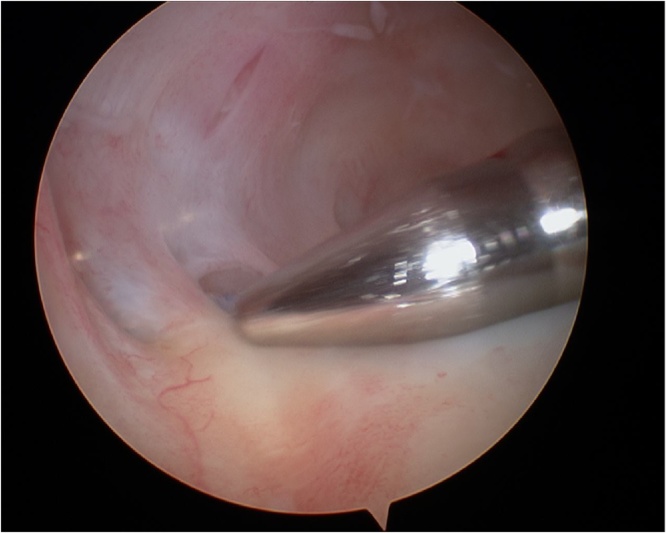
One patient suffered a post-operative adhesive capsulitis, which recovered with two months of physiotherapy and another (group 1) who developed persistent pain after surgery and underwent two arthroscopies, both of which did not demonstrate infection or rejection (Fig. 4) and biopsies demonstrate integration of the GraftJacket within the host tissue. This patient underwent a reverse shoulder replacement and is currently under follow up.
Fig. 4.
Arthroscopy demonstrating host cell integration.
5. Discussion
Our study demonstrates an improvement of mean OSS from 22 to 45.5 (p = 0.00148) during a 17 month follow up, when using tissue-matched thickness GraftJacket as an interpositional allograft in repairing rotator cuff tears.
Similar outcomes have been reported by Modi et al7 who performed a prospective study, which included sixty-one patients treated with open interpositional reconstruction using GraftJacket. They report a significant improvement in OSS from 26.4 to 44.6, p < 0.01 with a mean follow up of 3.6 years (1 to 6 years). Furthermore they noted their patients had significant improvement in pain, range of motion and strength.
Venouziou et al8 operated on fourteen patients with irreparable RCT using GraftJacket as an interpositional graft. Nine patients had previous primary rotator cuff repairs, the mean age was 54.6 years (33–64 years) and follow up was 30.2 months. Improvement was seen in scores of pain pre-op 7.4 to postop 1.7 (p < 0.001), ASES pre-op 23.8 to postop 72.3 (p < 0.001) and range of abduction pre-op 67.5° to 117.9° post-op (p < 0.002) and external rotation pre-op 7.9° to post-op 43.2° (p < 0.001). Of fourteen patients, eleven were satisfied or very satisfied with their operation and three were not. Their study demonstrated improvement in range of motion, pain and muscle strength. Although we did not compare pre- and postoperative range of motion (ROM) and pain scores, eighteen patients (90%) were satisfied and nineteen (95%) would recommend this operation.
Gupta et al9 treated twenty-four patients with open rotator cuff repair using GraftJacket as an interpositional graft. In this study all patients were satisfied with their outcome with no reported graft rejections or infections. ASES Score improved from 66.6 to 88.7 (p < 0.0003). Postoperative USS demonstrated a fully intact rotator cuff in 74% and partially intact in 26% of patients.
Barber et al10 performed a randomized prospective study of massive rotator cuff repair with and without GraftJacket augmentation. All tears involved two tendons greater than 3 cm in size, repaired arthroscopically. Mean age was 56 years (34–72 years) with a follow-up of 24 months (12–38 months). They demonstrated intact rotator cuffs in 85% of augmented and 40% of non-augmented groups (p < 0.01). Furthermore a more significant increase in pre- and postoperative scores of ASES (p < 0.035), Constant (p < 0.008) and University of California Los Angeles (UCLA) (p < 0.43) was demonstrated in the augmentation group.
Wong et al11 repaired 45 rotator cuff tears arthroscopically. There was an increase of the modified UCLA score from 18.4 to 27.5 (p < 0.001) after a mean follow-up of 2 years (24–68 months). These studies have shown good outcomes of using GraftJacket as interpositional or augmentation with open and arthroscopic techniques.
According to Longo et al12 the ideal biological scaffold should induce host-tissue ingrowth and tendon regeneration. Within our study, sufficient integration of the GraftJacket with native rotator cuff tissue was demonstrated during diagnostic arthroscopy 6 weeks post-repair in one patient. Smith et al13 compared various biological scaffolds and found the GraftJacket showed increase cell proliferation on day 13 compared to others. Interestingly Protzman et al14 compared the histology of rotator cuff repair with and without GraftJacket after 8 weeks in a patient. Results showed dense collagen and elastin four times as thick as native cuff repair. Studies have also shown GraftJacket to have stronger biomechanical properties than primary repair. Omae et al15 evaluated the biomechanical properties of GraftJacket augmentation in a cadaveric study, showing repair with GraftJacket withstand higher biomechanical loads (560.2 N), compared to those treated with only primary end-to-end repair (345.7 N).
In this study we did not classify the size of the rotator cuff because there is large variability within the literature. At our institution interpositional GraftJacket repair was offered to patients based on clinical symptoms of rotator cuff tear, on-going pain and failure of conservative measures with physiotherapy to treat. We felt that these patients would benefit from surgery; and GraftJacket was used where primary repair was not possible or had failed.
In our institution initial results were poor. We then doubled the graft thickness. Although we have very small numbers making it difficult to compare both groups, we strongly feel that in most cases doubling the GraftJacket may improve results of the operation, giving the interpositional construct additional strength and scaffold in which host cells can integrate.
Limitations of our study include a small sample size, with only thirteen patients (65%) having had their pre-operative scores documented for analysis. Post-operative imaging to evaluate the rotator cuff was not deemed necessary, and so was not performed. We did not compare ROM before and after surgery, and there was no control group. However, despite these limitations, a statistically significant improvement was seen following surgery.
The short-term results of our study suggest that GraftJacket can be used safely to repair rotator cuff tears as an interpositional graft, and that it improves symptoms and function. Feedback from patients included recommendations to comply with post-operative physiotherapy, and continue isometric exercises as long as possible to speed up rehabilitation.
6. Conclusion
Short-term results of rotator cuff repair using GraftJacket, as an interpositional allograft is a safe and effective procedure with good PROMS demonstrated, and we would suggest aiming for tissue-matched thickness. Compliance to post-operative physiotherapy will improve rehabilitation and outcomes of surgery. Further studies need to be done to ascertain the long-term follow-up of these patients and we would recommend further research in the form of a randomized controlled trial to evaluate its efficacy.
Contribution of the paper
This study demonstrates rotator cuff repair using a "doubled GraftJacket", as an interpositional allograft aiming for tissue-matched thickness is safe and effective and may demonstrate improved outcomes in PROMS and OSS.
Ethical approval
Observational study. No ethical approval was required.
Disclaimer
There are no financial benefits or otherwise conflicts of interests
Funding
No funding was received and there are no financial incentives with this product.
Conflicts of interests
There are no conflicts of interest involving any of the authors.
References
- 1.Favard L., Berhouet J., Colmar M. Massive rotator cuff tears in patients younger than 65 years. What treatment options are available? Orthop Traumatol Surg Res. 2009;95S:S19–S26. doi: 10.1016/j.otsr.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Bond J., Dopirak R., Higgins J. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJacket allograft: technique and preliminary results. J Arthroscopic Relat Surg. 2008;24(4):403–409. doi: 10.1016/j.arthro.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 3.Nho S.J., Delos D., Yadav H. Biomechanical and biologic augmentation for the treatment of massive rotator cuff tears. Am J Sports Med. 2010;38:619–629. doi: 10.1177/0363546509343199. [DOI] [PubMed] [Google Scholar]
- 4.Galatz L.M., Ball C.M., Teefey S.A. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Jt Surg Am. 2004;86-A(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Gerber C., Fuchs B., Hodler J. The results of repair of massive tears of the rotator cuff. JBJS. 2000;82(4(April)):505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Harreld K.L., Puskas B.L., Frankle M.A. Massive rotator cuff tears without arthropathy: when to consider reverse shoulder arthroplasty. Instr Course Lect. 2012;61:143–156. [PubMed] [Google Scholar]
- 7.Modi A., Singh H., Pandey R. Management of irreparable rotator cuff tears with the GraftJacket allograft as an interpositional graft. Shoulder Elb. 2013;5(3):1–7. [Google Scholar]
- 8.Venouziou A., Kokkalis Z.T., Sotereanos D.G. Human dermal allograft interposition for the reconstruction of massive irreparable rotator cuff tears. Am J Orthop. 2013;42(2):63–70. [PubMed] [Google Scholar]
- 9.Gupta A.K., Hug K., Berkoff D.J. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med. 2012;40(1):141–147. doi: 10.1177/0363546511422795. [DOI] [PubMed] [Google Scholar]
- 10.Barber F., Burns J., Deutsch A. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. J Arthrosc Relat Surg. 2012;28(1):8–15. doi: 10.1016/j.arthro.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 11.Wong I., Burns J., Snyder S. Arthroscopuc GraftJacket repair of rotator cuff tears. J Shoulder Elb Surg. 2010;19(2):104–109. doi: 10.1016/j.jse.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 12.Longo U.G., Lamberti A., Rizzello G. Synthetic augmentation in massive rotator cuff tears. Med Sport Sci. 2012;57:168–177. doi: 10.1159/000328891. [DOI] [PubMed] [Google Scholar]
- 13.Smith R.D., Carr A., Dakin S. The response of tenocytes to commercial scaffolds used for rotator cuff repair. Eur Cell Mater. 2016;31:107–118. doi: 10.22203/ecm.v031a08. [DOI] [PubMed] [Google Scholar]
- 14.Protzman N., Stopyra G., Hoffman J. Biologically enhanced healing of the human rotator cuff: 8-month postoperative histological evaluation. Orthopedics. 2013;36(1(January)):38–41. doi: 10.3928/01477447-20121217-06. [DOI] [PubMed] [Google Scholar]
- 15.Omae H., Steinmann S., Zhao C. Biomechanical effect of rotator cuff augmentation with an acellular dermal matrix graft: a cadaver study. Clin Biomech. 2012;27:779–789. doi: 10.1016/j.clinbiomech.2012.05.001. [DOI] [PubMed] [Google Scholar]