Abstract
Background
As demand for total shoulder arthroplasty (TSA) rises, containing costs will become increasingly important. We hypothesize that performing ambulatory TSA procedures results in significant cost savings.
Methods
A model was created to evaluate cost savings. Hospital stay length and cost, pain control method and cost, and number of annual outpatient TSA procedures were estimated based on literature.
Results
Estimated cost savings per patient were $747 to $15,507 (base case $5594), total annual savings of $4.1M to $349M (base case $82M), and ten-year savings of $51M to $5.4B (base case $1.1B).
Conclusion
Ambulatory TSA procedures result in significant cost savings.
Keywords: Cost, Shoulder, Arthroplasty, Ambulatory, Outpatient
1. Introduction
The annual demand for total shoulder arthroplasty (TSA) in the U.S. is significant, and is expected to increase substantially in the future. Recent estimates suggest that a total of 39,000 TSAs are performed annually, with a growth rate of approximately 5%–9% per year.[1], [2], [3] In addition, total shoulder arthroplasty is associated with significant costs, with mean total cost estimates of $14,000-$52,000 per patient,[3], [4], [5] resulting in total estimated societal costs of $490M-$1.8B per year. As demand for TSA continues to grow, hospital administrators and policy makers will seek to identify means to reduce costs associated with these operations. Inpatient hospital fees are a major contributor to these costs and are sure to be a focus of efforts to optimize care.
Reducing length of stay is one such way to manage rising costs. Attempts at instituting accelerated pathways with quicker discharge have been successful in the total joints literature, cutting costs significantly and improving patient satisfaction while not increasing complication or readmission rates.[6], [7], [8], [9], [10], [11], [12] Costs associated with inpatient admission can be eliminated altogether by performing the procedure in an outpatient setting; a strategy that has been successful in other joints literature. Several studies have reported data on outpatient total knee arthroplasty (TKA), with significant reduction in total costs, similar outcomes, high satisfaction rates, and a relatively low rate of complications and readmissions.8,[13], [14], [15] Ambulatory total hip arthroplasty (THA) has also been studied and shown success in select groups of patients,16,17 although one study suggested that additional personnel costs required to affect this change may make the outpatient system more expensive to implement, however a cost analysis was not done in this case.18 Attempts have been made at performing TSA in the ambulatory setting, although the majority of reports come from the media, as there is little data in the literature reporting on outpatient TSA management.[19], [20], [21] Postoperative pain has been one major obstacle to same-day discharge for TSA, though successful ambulatory management with at-home perineural interscalene infusion22 and continuous brachial plexus blockade23 has been reported. Other studies have reported successful outpatient pain management of major shoulder surgeries (of which TSA was a part) with continuous interscalene brachial plexus blockade,[24], [25], [26], [27] and it has been suggested that such a pathway may be a route to cost savings.28 An improved understanding of the trade-offs between inpatient and outpatient TSA could aid patients, physicians, researchers, and policy makers in (a) determining if outpatient TSA is more cost-effective than inpatient TSA and (b) in estimating the amount of cost-savings associated with the outpatient procedure over time.
The primary objective of this study was to establish a model to perform a cost-identification analysis of performing total shoulder arthroplasty in the outpatient compared to the inpatient setting. Cost-identification analysis considers the costs associated with the interventions in question, with the purpose of identifying the less expensive option given equal outcomes between the two.29 Other total joints procedures performed in the outpatient setting8,[13], [14], [15], [16], [17] and successful reports in the media[19], [20], [21] have shown equal outcomes for inpatient and outpatient operations in a select group of patients. Recent studies in shoulder arthroplasty have similarly shown no significant difference in the adverse event and readmission rates between outpatient and inpatient TSA.30,31 We aimed to estimate cost savings per patient as well as evaluate societal savings annually and over a period of 10 years. As a part of the model, we hoped to characterize the reduction in costs that would accompany this change. Our hypothesis was that performing ambulatory TSA procedures in appropriate cases would result in considerable cost savings to society.
2. Methods
2.1. Study and model design
A model was created to evaluate the cost savings associated with outpatient TSA procedures compared with those performed in the inpatient setting. Our reference case was a hypothetical cohort of patients who were candidates for total shoulder arthroplasty, including both male and female patients with all underlying etiologies. The subgroup of patients who would be candidates for outpatient management was estimated based on the literature. Two studies were identified which studied outpatient TSA, with the first defining patients as candidates for same-day discharge if they 1) had a numerical rating scale pain score ≤ 4, 2) required < 5 mg IV morphine, 3) ambulated without assistance or light-headedness, 4) tolerated oral liquids, 5) had normal vital signs, 6) had estimated blood loss < weight (kg) x 10 mL, and 7) had no medical issues requiring admission, as well as lived within 2 h of the hospital and had a caretaker for the duration of the local anesthetic infusion.22 In the second study, eligibility criteria for outpatient TSA were: 1) American Society of Anesthesiologists (ASA) Grade 1 or 2, 2) no major medical reason for postoperative monitoring, 3) residency in the same region as the hospital, and 4) availability of a caretaker during the first 24 h after surgery.23
Costs were calculated from both an individual patient and societal perspective, with an annual and ten-year time horizon. Outcomes were expressed as cost differences in 2015 US dollars, which takes into account an annual discount rate of 3%. A model was generated with inputs (assumptions on inpatient hospitalization, pain control, and prevalence of outpatient TSA), which provided cost difference outcomes associated with inpatient and outpatient management of TSA. Sensitivity analyses were performed on key model parameters to evaluate their effects on base case conclusions.
2.2. Inpatient hospitalization
One of the primary inputs into the model is length of stay associated with inpatient TSA. Our assumptions were based on the previous literature, which has shown that length of stay associated with these procedures ranges from one to four or more days of hospitalization.4,23,32 At our institution, the current average length of stay for patients undergoing TSA is 2.2 days. In our reference case, we estimated the length of stay based on the experience at our institution as well as that reported by Virani et al and Dunn et al4,32
One of the primary differences in cost outcomes of inpatient and outpatient TSA is related to the cost of inpatient hospitalization. This cost, which was included in the calculation of inpatient TSA costs but not in outpatient TSA costs, was estimated based on the previous literature, which varies greatly with reports of inpatient admission costing from $1,500/day to $12,500/day.[9], [10], [11], [12],33 In our reference case, we estimated the cost of inpatient admission to be $3300 per inpatient day based on the work of Raphael et al and Scranton.11,12
2.3. Pain control
Previous work has suggested that oral pain medication or nurse-administered analgesia is insufficient to provide pain relief following TSA.23,34 For this reason, the pain control options considered in our study included patient-controlled analgesia (PCA) with opiates and peripheral nerve blockade (PNB). Cost estimates for PCA were based on the prior literature, which shows a range from $64 to $347 per patient per day.[35], [36], [37] We estimated PCA cost of $224, based on work by Palmer et al35 corrected for average length of stay. Similarly, PNB cost estimates were based on the previous literature, with ranges from $1752 to $5550 in total cost per patient. In our reference case, we estimated the cost of PNB $3556 based on similar reports by Cheng et al38, Horn et al39, and Williams et al40
The proportion of those undergoing inpatient TSA managed with each of these pain regimens was also estimated. We could not identify prior studies in the literature upon which to draw when generating estimates about pain control.
2.4. Prevalence of outpatient TSA
Reports from previous literature were used to estimate the total number of TSA procedures performed annually.[1], [2], [3] The annual growth rate was estimated from the work of Kim et al2 and Day et al1 (7.2%, the average of 4.9%, annual growth rate of Kim et al prior to introduction of reverse TSA, and 9.4%, annual growth rate reported by Day et al), and our reference case for the total number of TSAs performed in 2015 derived from these studies, as well as by Ponce et al3 (39,104 cases in 2015, calculated using above growth rate, applied to the total prevalence reported by Ponce et al). The subset of patients undergoing TSA who were candidates for outpatient management was also estimated based on previous literature23, with our base case being 36% of those undergoing TSA being candidates for outpatient management, a figure which corresponds well to both of these references.
2.5. Sensitivity analysis
Sensitivity analysis was performed to evaluate the uncertainties in key parameter values. A multi-way sensitivity analysis was performed to evaluate the combined uncertainties of average length of inpatient stay, cost of inpatient hospitalization, cost of both methods of pain control, annual prevalence of total TSAs, annual growth rate in the number of TSA procedures, and the proportion of TSAs performed that could be done in the outpatient setting.
3. Results
3.1. Reference case
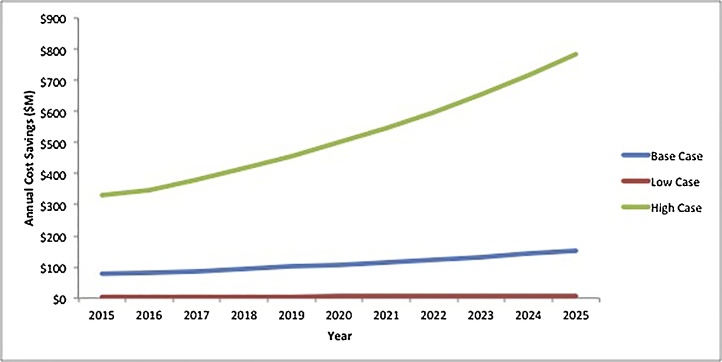
The results of the model output are presented in Table 2. When compared to inpatient management of total shoulder arthroplasty, performing the procedure in the ambulatory setting was associated with cost savings of $5594 per patient. Assuming 15,000 total outpatient TSAs performed in 2016 in the US, total cost savings in that year was estimated to be $82M (Fig. 1). In the base case scenario, 10-year cost savings from 2016 to 2025 was estimated to be $1.1B.
Table 2.
Presents model outputs, including cost savings per patient, total annual cost savings, and 10-year cost savings that would result from outpatient management of TSA.
| Value |
|||
|---|---|---|---|
| Description | Base Case | Low | High |
| Cost Savings Per Patient ($) | 5594 | 747 | 15,507 |
| Overall Cost Savings ($), 2016 | 81,960,089 | 4,091,597 | 349,291,430 |
| Overall Cost Savings ($), 2016-2025 | 1,143,151,269 | 51,224,092 | 5,409,142,626 |
Fig. 1.
Annual cost savings over time (2015-2025). Annual US cost savings in 2016 was $82M ($4.1M to $349M), while ten-year cost savings (2016-2025) was $1.1B ($51M to $5.4B).
3.2. Sensitivity analysis
In the multi-way sensitivity analyses, in which parameters were varied according to the ranges specified in Table 1, outpatient TSA was associated with substantial cost savings in every scenario, even when all of the low case assumptions were used in the model. Using the multi-way sensitivity analyses, cost savings per patient varied from a nadir of $747 to a peak of $15,507 per patient. Overall cost savings in 2016 ranged from $4.1M to $349M (Fig. 1). Ten-year cost savings from 2016 to 2025 varied from $51M to $5.4B.
Table 1.
Presents the model inputs, including assumptions on inpatient hospitalization, pain control, and prevalence of outpatient TSA procedures.
| Value |
||||
|---|---|---|---|---|
| Description | Base Case | Low | High | References |
| Inpatient hospitalization | ||||
| Average length of stay: inpatient TSA (days) | 2.2 | 1 | 4 | Gallay et al, Virani et al, Dunn et al |
| Average length of stay: outpatient TSA (days) | 0 | 0 | 0 | |
| Cost of hospital inpatient stay ($/day) | 3300 | 1,591 | 4,397 | Raphael et al, Hunt et al, Healy et al, Scranton, International Federation of Health Plans 2012 Consumer Price Report |
| Pain Control | ||||
| Cost of pain control: PCA ($) | 224 | 64 | 1,388 | Palmer et al, Choi et al, Chang et al |
| Cost of pain control: PNB ($) | 3556 | 1752 | 5550 | Cheng et al, Horn et al, Williams et al |
| Proportion of inpatients receiving PCA (%) | 50% | 50% | 50% | Expert opinion |
| Proportion of inpatients receiving PNB (%) | 50% | 50% | 50% | Expert opinion |
| Proportion of outpatients receiving PCA (%) | 0% | 0% | 0% | Expert opinion |
| Proportion of outpatients receiving PNB (%) | 100% | 100% | 100% | Expert opinion |
| Prevalence of Outpatient TSA | ||||
| Total TSAs in 2015 (no.) | 39,104 | 35,854 | 42,414 | Kim et al, Ponce et al, Day et al |
| Annual growth rate (%) | 7.2% | 4.9% | 9.4% | Kim et al, Day et al |
| Proportion performed as outpatient (%) | 36% | 15% | 50% | Gallay et al |
TSA = Total shoulder arthroplasty; PCA = patient-controlled analgesia; PNB = peripheral nerve block.
4. Discussion
Total shoulder arthroplasty is an increasingly common procedure that is associated with substantial costs. A considerable portion of these costs arises from postoperative inpatient admission, highlighting the possibility of substantial cost savings if TSA were performed in the ambulatory setting. Given the increasing focus on cost containment, we studied the costs associated with inpatient and outpatient TSA, as well as the subset of patients who would be candidates for this procedure, and estimated the amount of cost savings that could be realized by this shift in treatment paradigm.
This study indicates that, on an individual patient level, transitioning TSA from the inpatient to the outpatient setting could result in cost savings of $750 to $15,500 per patient, with substantial cost savings to society of $51M to $5.4B over a period of 10 years. For patients who are candidates for the ambulatory procedure, they would avoid the costs associated with an average of 2.2 days of inpatient hospital admission. We estimated that 36% of total TSA procedures could be performed on an outpatient basis.
Despite many studies reporting on outpatient management of select patients undergoing TKA and THA, we could not identify any existing studies providing a cost analysis of outpatient TSA, although prior work has suggested that outpatient TSA would result in considerable cost savings.23,28 The results reported in the study are in line with prior cost analyses performed in the total joints literature. Lovald et al, for example, studied outpatient TKA and found that costs in the outpatient group were reduced by $8527 compared to the group with a standard 3–4 day inpatient stay, although this cost savings was observed at 2 years post-operatively.8 In a retrospective study of outpatient and inpatient TKA, Ilfield and colleagues reported a cost savings of $2685 in the outpatient cohort.41 Finally, in a study of unicompartmental knee arthroplasty (UKA), Repicci and Eberle reported cost savings of $9000 associated with same day discharge, compared to the standard 3–4 day hospital stay.42
In this study, the outpatient TSA strategy was cost saving in all scenarios for several reasons. First, the majority of modifiable costs (i.e. not surgeon’s fees, OR time, PACU costs) are derived from inpatient stay, so eliminating this cost results in substantial cost savings across all scenarios. There is increased cost associated with peripheral nerve block compared with patient-controlled analgesia, although this cost difference was never sufficient to overcome the overwhelming cost-savings that resulted from avoiding inpatient admission. Apart from pain control, outpatient TSA is expected to produce no increased cost (i.e. complication and readmission rates). This assumption is based on the limited data on outpatient TSA in few patients, in which pain was well-controlled, patient satisfaction was high, and there were no reported complications or readmissions,22,23 as well as several studies reporting data on outpatient TKA and THA.[6], [7], [8], [9], [10], [11], [12]
We estimated that 36% of patients would be candidates for outpatient TSA, with sensitivity analysis of 15%–50%. This proportion is based on the work of Gallay et al, who reported that 36% (8 of 22) of patients in their study were eligible for same day discharge. This estimate is similar to that reported in Kolisek et al, who found that 43% (64/150) of TKA patients were eligible for outpatient management14, and with the study of Berger et al, who reported that 28% (150/535) of primary THA patients could be discharged the same day of surgery.18 We believe our estimate and sensitivity analyses are conservative as, compared to patients undergoing TKA and THA, those having TSA are not having surgery on the lower extremity and would therefore feel more comfortable ambulating and be more amenable to discharge.
Our study has several limitations. Due to the lack of available data on outpatient TSA outcomes, many assumptions were required, using proxy data from other total joints literature when necessary. However, to limit the shortcomings of this scarcity of data, sensitivity analyses were employed and resulted in substantial cost savings even in the worst-case scenario, which lends support to our conclusions. Our model assumed no difference in complication or readmission rates, base on work by Leroux et al using the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database, which found no significant difference in the 30-day adverse event and readmission rates between outpatient and inpatient TSA.30 Similarly, a study by Brolin et al comparing 30 patients with outpatient TSA to an age- and comorbidities-matched cohort with traditional inpatient TSA found no significant difference in rates of complications and no hospital admissions from the outpatient cohort.31 And while only reflecting the experience of a small number of patients, the studies by Gallay et al and Ilfield et al report no complications or readmissions among patients who underwent outpatient TSA.
Furthermore, an additional limitation of our study is the lack of a specified target population who would be candidates for outpatient TSA, which is difficult to define given the current lack of data. Gallay and colleagues, from which we estimated the proportion of patients who would be eligible for ambulatory management, used the following criteria: ASA grade 1 or 2, no medical reason for postoperative monitoring, residency near to the hospital, and caretaker availability for 24 h after surgery.23 Finally, apart from the costs associated with the PNB, we did not consider any additional costs (e.g. any additional resources or staff required) associated with discharging patients on the day of surgery. We did not believe that these patients would require any additional resources at discharge compared to their inpatient counterparts.
In conclusion, this analysis shows that, for a subgroup of patients undergoing TSA, outpatient management can represent a cost-effective strategy for reducing the significant costs associated with this procedure. Although there is little data on outpatient TSA, these results are based on high-quality published literature on outpatient TKA and THA as well as studies reporting on the feasibility of performing ambulatory TSA from a pain management standpoint, and are robust with consistent conclusions when tested with broad sensitivity analyses. With a significant reduction in costs associated with inpatient hospitalization and without increased complication or readmission rates, there is likely a role for ambulatory TSA in a considerable portion of patients. Future research should focus on defining the specific characteristics, which would make patients candidates for outpatient TSA, as well as on outcomes associated with outpatient management.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors have no conflicts of interest to declare.
All authors contributed equally toward drafting, revising, supervision, and analysis of data
References
- 1.Day J.S., Lau E., Ong K.L., Williams G.R., Ramsey M.L., Kurtz S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder elbow Surg / Am Shoulder Elbow Surgeons [Et Al] 2010;19:1115–1120. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Kim S.H., Wise B.L., Zhang Y., Szabo R.M. Increasing incidence of shoulder arthroplasty in the United States. J Bone Jt Surg Am Vol. 2011;93:2249–2254. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 3.Ponce B.A., Oladeji L.O., Rogers M.E., Menendez M.E. Comparative analysis of anatomic and reverse total shoulder arthroplasty: in-hospital outcomes and costs. J Shoulder elbow Surg / Am Shoulder Elbow Surgeons [Et Al] 2015;24:460–467. doi: 10.1016/j.jse.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 4.Virani N.A., Williams C.D., Clark R., Polikandriotis J., Downes K.L., Frankle M.A. Preparing for the bundled-payment initiative: the cost and clinical outcomes of total shoulder arthroplasty for the surgical treatment of glenohumeral arthritis at an average 4-year follow-up. J Shoulder Elbow Surg / Am Shoulder Elbow Surgeons [Et Al] 2013;22:1601–1611. doi: 10.1016/j.jse.2012.12.028. [DOI] [PubMed] [Google Scholar]
- 5.Davis D.E., Paxton E.S., Maltenfort M., Abboud J. Factors affecting hospital charges after total shoulder arthroplasty: an evaluation of the National Inpatient Sample database. J Shoulder Elbow Surg / Am Shoulder Elbow Surgeons [Et Al] 2014;23:1860–1866. doi: 10.1016/j.jse.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Larsen K., Hansen T.B., Thomsen P.B., Christiansen T., Soballe K. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Jt Surg Am Vol. 2009;91:761–772. doi: 10.2106/JBJS.G.01472. [DOI] [PubMed] [Google Scholar]
- 7.Vorhies J.S., Wang Y., Herndon J., Maloney W.J., Huddleston J.I. Readmission and length of stay after total hip arthroplasty in a national medicare sample. J Arthroplasty. 2011;26:119–123. doi: 10.1016/j.arth.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 8.Lovald S.T., Ong K.L., Malkani A.L. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. 2014;29:510–515. doi: 10.1016/j.arth.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 9.Hunt G.R., Crealey G., Murthy B.V. The consequences of early discharge after hip arthroplasty for patient outcomes and health care costs: comparison of three centres with differing durations of stay. Clin Rehabilit. 2009;23:1067–1077. doi: 10.1177/0269215509339000. [DOI] [PubMed] [Google Scholar]
- 10.Healy W.L., Iorio R., Ko J., Appleby D., Lemos D.W. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Jt Surg Am Vol. 2002;84-a:348–353. doi: 10.2106/00004623-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Scranton P.E., Jr. The cost effectiveness of streamlined care pathways and product standardization in total knee arthroplasty. J Arthroplasty. 1999;14:182–186. doi: 10.1016/s0883-5403(99)90123-7. [DOI] [PubMed] [Google Scholar]
- 12.Raphael D.R., Cannesson M., Schwarzkopf R. Total joint perioperative surgical home: an observational financial review. Perioperative Med (Lond, Engl) 2014;3:6. doi: 10.1186/2047-0525-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berger R.A., Kusuma S.K., Sanders S.A., Thill E.S., Sporer S.M. The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res. 2009;467:1443–1449. doi: 10.1007/s11999-009-0736-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolisek F.R., McGrath M.S., Jessup N.M., Monesmith E.A., Mont M.A. Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res. 2009;467:1438–1442. doi: 10.1007/s11999-009-0730-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berger R.A., Sanders S., D’Ambrogio E. Minimally invasive quadriceps-sparing TKA: results of a comprehensive pathway for outpatient TKA. J Knee Surg. 2006;19:145–148. doi: 10.1055/s-0030-1248097. [DOI] [PubMed] [Google Scholar]
- 16.Dorr L.D., Thomas D.J., Zhu J., Dastane M., Chao L., Long W.T. Outpatient total hip arthroplasty. J Arthroplasty. 2010;25:501–506. doi: 10.1016/j.arth.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Berger R.A. A comprehensive approach to outpatient total hip arthroplasty. Am J Orthopedics (Belle Mead, NJ) 2007;36:4–5. [PubMed] [Google Scholar]
- 18.Berger R.A., Sanders S.A., Thill E.S., Sporer S.M., Della Valle C. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. Clin Orthop Relat Res. 2009;467:1424–1430. doi: 10.1007/s11999-009-0741-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.2013. C Y. OhiohHealth surgeon performs area’s first outpatient total shoulder replacement. [Google Scholar]
- 20.2011. Medicine CHS. First outpatient shoulder replacement. [Google Scholar]
- 21.FloridaMD; 2013. C G. outpatient total shoulder replacement surgery procedure provides multiple benefits to patients, surgeons. [Google Scholar]
- 22.Ilfeld B.M., Wright T.W., Enneking F.K. Total shoulder arthroplasty as an outpatient procedure using ambulatory perineural local anesthetic infusion: a pilot feasibility study. Anesth Analg. 2005;101:1319–1322. doi: 10.1213/01.ANE.0000180199.52383.CE. [DOI] [PubMed] [Google Scholar]
- 23.Gallay S.H., Lobo J.J., Baker J., Smith K., Patel K. Development of a regional model of care for ambulatory total shoulder arthroplasty: a pilot study. Clin Orthop Relat Res. 2008;466:563–572. doi: 10.1007/s11999-007-0083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russon K., Sardesai A.M., Ridgway S. Postoperative shoulder surgery initiative (POSSI): an interim report of major shoulder surgery as a day case procedure. Br J Anaesth. 2006;97:869–873. doi: 10.1093/bja/ael281. [DOI] [PubMed] [Google Scholar]
- 25.Fredrickson M.J., Ball C.M., Dalgleish A.J. Successful continuous interscalene analgesia for ambulatory shoulder surgery in a private practice setting. Reg Anesth Pain Med. 2008;33:122–128. doi: 10.1016/j.rapm.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Kean J., Wigderowitz C.A., Coventry D.M. Continuous interscalene infusion and single injection using levobupivacaine for analgesia after surgery of the shoulder. A double-blind, randomised controlled trial. J Bone Jt Surg Br Vol. 2006;88:1173–1177. doi: 10.1302/0301-620X.88B9.17412. [DOI] [PubMed] [Google Scholar]
- 27.Mariano E.R., Afra R., Loland V.J. Continuous interscalene brachial plexus block via an ultrasound-guided posterior approach: a randomized, triple-masked, placebo-controlled study. Anesth Analg. 2009;108:1688–1694. doi: 10.1213/ane.0b013e318199dc86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sulaiman L., Macfarlane R.J., Waseem M. Current concepts in anaesthesia for shoulder surgery. Open Orthopaedics J. 2013;7:323–328. doi: 10.2174/1874325001307010323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nwachukwu B.U., Schairer W.W., Bernstein J.L., Dodwell E.R., Marx R.G., Allen A.A. Cost-effectiveness analyses in orthopaedic sports medicine: a systematic review. Am J Sports Med. 2014 doi: 10.1177/0363546514544684. [DOI] [PubMed] [Google Scholar]
- 30.Leroux T.S., Basques B.A., Frank R.M., Griffin J.W., Nicholson G.P., Cole B.J., Romeo A.A., Verma N.N. Outpatient total shoulder arthroplasty: a population-based study comparing adverse event and readmission rates to inpatient total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:1780–1786. doi: 10.1016/j.jse.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 31.Brolin T.J., Mulligan R.P., Azar F.M., Throckmorton T.W. Outpatient total shoulder arthroplasty in an ambulatory surgery center is a safe alternative to inpatient total shoulder arthroplasty in a hospital: a matched cohort study. J Shoulder Elbow Surg. 2017;26:204–208. doi: 10.1016/j.jse.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 32.Dunn J.C., Lanzi J., Kusnezov N., Bader J., Waterman B.R., Belmont P.J., Jr. Predictors of length of stay after elective total shoulder arthroplasty in the United States. J Shoulder Elbow Surg / Am Shoulder Elbow Surgeons [Et Al] 2015 doi: 10.1016/j.jse.2014.11.042. [DOI] [PubMed] [Google Scholar]
- 33.International Federation of Health Plans; 2012. Plans IFoH. 2012 Comparative price report.http://www.ifhp.com [Google Scholar]
- 34.Hutchison R.W. Challenges in acute post-operative pain management. Am J Health-System Pharm. 2007;64:S2–S5. doi: 10.2146/ajhp060679. [DOI] [PubMed] [Google Scholar]
- 35.Palmer P., Ji X., Stephens J. Cost of opioid intravenous patient-controlled analgesia: results from a hospital database analysis and literature assessment. ClinicoEcon. Outcomes Res : CEOR. 2014;6:311–318. doi: 10.2147/CEOR.S64077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi Y.Y., Park J.S., Park S.Y. Can intravenous patient-controlled analgesia be omitted in patients undergoing laparoscopic surgery for colorectal cancer? Ann Surg Treat Res. 2015;88:86–91. doi: 10.4174/astr.2015.88.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chang A.M., Ip W.Y., Cheung T.H. Patient-controlled analgesia versus conventional intramuscular injection: a cost effectiveness analysis. J Adv Nurs. 2004;46:531–541. doi: 10.1111/j.1365-2648.2004.03027.x. [DOI] [PubMed] [Google Scholar]
- 38.Cheng G.S., Choy L.P., Ilfeld B.M. Regional anesthesia at home. Curr Opin Anaesthesiol. 2008;21:488–493. doi: 10.1097/ACO.0b013e328303bfb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horn J.L., Swide C., Gaebel B.A., Cross R.L., Jr. Comparison of efficiency, recovery profile and perioperative costs of regional anaesthesia vs. general anaesthesia for outpatient upper extremity surgery. Eur J Anaesthesiol. 2007;24:557–559. doi: 10.1017/s0265021506002195. [DOI] [PubMed] [Google Scholar]
- 40.Williams B.A., Kentor M.L., Vogt M.T. Economics of nerve block pain management after anterior cruciate ligament reconstruction: potential hospital cost savings via associated postanesthesia care unit bypass and same-day discharge. Anesthesiology. 2004;100:697–706. doi: 10.1097/00000542-200403000-00034. [DOI] [PubMed] [Google Scholar]
- 41.Ilfeld B.M., Mariano E.R., Williams B.A., Woodard J.N., Macario A. Hospitalization costs of total knee arthroplasty with a continuous femoral nerve block provided only in the hospital versus on an ambulatory basis: a retrospective, case-control, cost-minimization analysis. Reg Anesth Pain Med. 2007;32:46–54. doi: 10.1016/j.rapm.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Repicci J.A., Eberle R.W. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999;8:20–27. discussion 7. [PubMed] [Google Scholar]