Abstract
Introduction
There are numerous configurations of double row fixation for rotator cuff tears however, there remains to be a consensus on the best method. In this study, we evaluated three different double-row configurations, including a new method. Our primary question is whether the new anchor and technique compares in biomechanical strength to standard double row techniques.
Methods
Eighteen prepared fresh frozen bovine infraspinatus tendons were randomized to one of three groups including the New Double Row Equivalent, Arthrex Speedbridge and a transosseous equivalent using standard Stabilynx anchors. Biomechanical testing was performed on humeri sawbones and ultimate load, strain, yield strength, contact area, contact pressure, and a survival plots were evaluated.
Results
The new double row equivalent method demonstrated increased survival as well as ultimate strength at 415N compared to the remainder testing groups as well as equivalent contact area and pressure to standard double row techniques.
Conclusions
This new anchor system and technique demonstrated higher survival rates and loads to failure than standard double row techniques. This data provides us with a new method of rotator cuff fixation which should be further evaluated in the clinical setting.
Level of Evidence
Basic science biomechanical study.
Keywords: Arthroscopy, Shoulder, Rotator cuff repairs, Double row, Biomechanical, Anchors
1. Introduction
The rotator cuff is essential to the shoulder’s biomechanical functionality, making its anatomic reconstruction a necessary step to maximize shoulder mobility.1, 2 The goal of rotator cuff repair is to recreate the anatomic footprint of the shoulder thereby maximizing healing potential and ultimately preserving its function. Various double-row, transosseous-equivalent, and footprint-type repairs have been evaluated in an attempt to maximize the contact area and pressure at the tendon-bone interface. Prior biomechanical studies have shown the superior strength of the double row and transosseous techniques in vitro compared to single row techniques.3, 4, 5, 6, 7 Additionally, studies have demonstrated improved clinical function and improved histologic healing in patients who underwent the double-row technique.8, 9, 10, 11 Although double row and transosseous-equivalent fixation have greater biomechanical strength, they also come at a higher cost due to increased anchor use.
A number of different suture configurations including simple, mattress, and Mason Allen have been evaluated to determine the strongest technique.11 Burkart et al.12, 13 showed that a diamondback (transosseous) repair had the most strength. Additionally, numerous studies have demonstrated the importance of the medial row linkage for overall construct strength.14, 15 This new system creates an efficient method of forming the medial linkage while eliminating medial knots, thus allowing for a smooth interface at the tendon-suture junction. Despite constant innovation in rotator cuff repair technique, the question remains: which method provides the best footprint restoration, contact pressure, contact area, and strength?
While double row and transosseous systems require two medial and two lateral anchors with a minimum of four suture passes, the new double row equivalent system creates the same number of suture passes using only two anchors total. This is accomplished by creating two interconnected suture anchors via loops in the suture where neighboring suture can be shuttled. The new double row equivalent system delivers an efficient method of providing a medial and lateral row with even tensioning throughout, lending the ability to maximize compression at the tendon-bone footprint.
The aim of the current study was to compare the biomechanical performance of a new double row equivalent system to that of two other linked and unlinked transosseous configurations. Our null hypothesis was that there would be no difference between the various fixation methods.
2. Materials and methods
Sixteen frozen bovine infraspinatus tendons were obtained and thawed. Bovine infraspinatus tendons have been used in a number of other rotator cuff biomechanical studies.15, 16, 17, 18 The tendons were prepared by removing all soft tissues, including muscle. The tendons were then bisected to create 32 specimens. The specimens were evaluated for homogeneity of structure and size and 18 of the most uniform tendon specimens were chosen for testing. At the anticipated suture site, thickness was measured and recorded for each tendon. Tendons were randomly assigned to Group A, Group B or Group C and these were subsequently divided into testing groups. Tendons from the same specimen were assigned to different test groups in an endeavor to control for differences in the size of the tendons. In addition, the surgeon was blinded to the selection of tendons for each group. No statistically significant difference in tendon thickness was observed between groups (Table 1).
Table 1.
Testing groups. Significance set at P < 0.05. mm = millimeters.
| Group | Fixation method | Number of Specimens | Average Tendon Thickness (mm) | p-value for tendon thickness (compared to Group C) |
|---|---|---|---|---|
| A | Trans-Osseous Equivalent #1 | 6 | 3.5 | 0.35 |
| B | Trans-Osseous Equivalent #2 | 6 | 3.8 | 0.33 |
| C | Double Row Equivalent | 6 | 4.5 | N/A |
Sawbones were used as surrogate humeri. The most distal 75% of the surrogate humerui were encased in epoxy resin in order to achieve greater purchase with test fixturing. Each specimen was fixed in the testing apparatus at a 30° angle from the horizontal.
A TekScan 4205 pressure sensor (TekScan, South Boston, MA) was used to measure contact pressure, which has been shown to be highly accurate in determining pressure and force under an object.19 A 10 mm × 42 mm sensor was placed under the repairs. The sensor was pinned at one end of the humerus and taped on the other to prevent motion during testing.
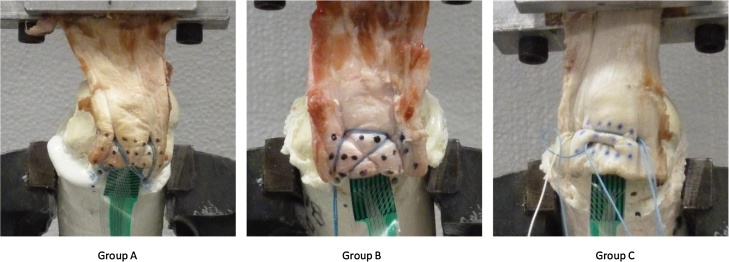
The tendons were divided into one of three groups: the Trans-osseous Equivalent #1 (Arthrex SpeedBridge) in Group A, the Trans-osseous Equivalent #2 in Group B, or the new double row equivalent (Stabilynx) in Group C (Table 1, Fig. 1). Group A and Group B were knotless, whereas Group C used knots to secure fixation in the lateral row. Stabilynx medial row anchors were used in Group B in a knotless, linked configuration.
Fig. 1.
Lab images of Group A–C Repair Contructs. Images are complete in-lab constructs prior to biomechanical testing. A –Trans-osseous Equivalent #1. B –Trans-osseous Equivalent #2. C –Double Row Equivalent.
Eight points were marked along the repair site to measure gap formation, footprint strain, and musculotendinous strain during testing.
Video was taken for each group throughout cycling and testing.
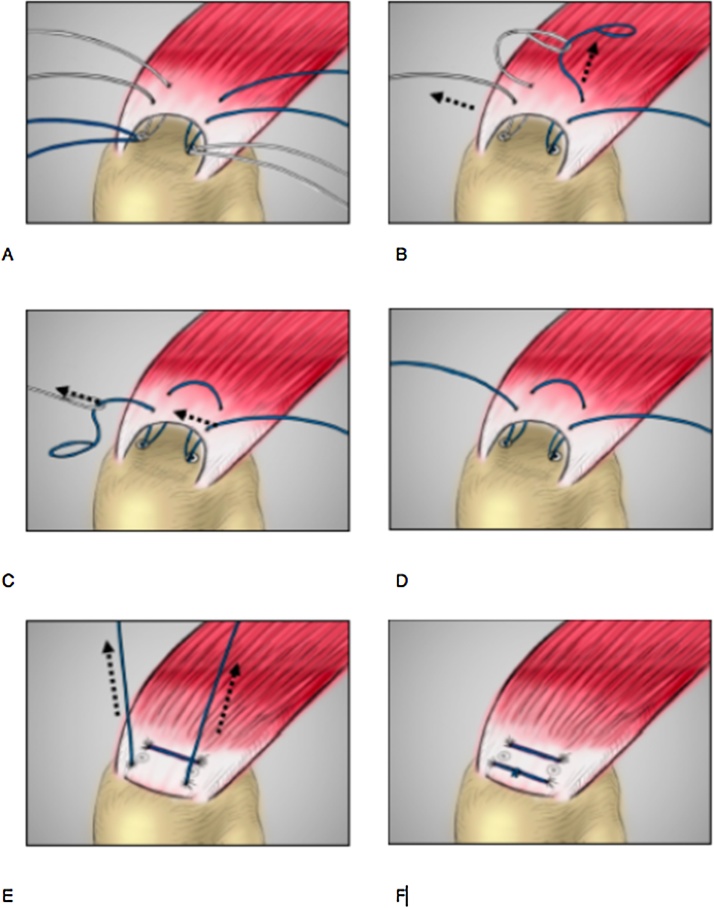
3. Surgical technique
The new double row equivalent anchor system (Fig. 2) utilizes two anchors which are first placed at the same level in the anatomic rotator cuff footprint. Each anchor is double loaded with non-absorbable No. 2 braided polyester suture. A pass is made with one suture from either anchor approximately 5 mm medially into the rotator cuff. One of these sutures has a loop where the suture from the other anchor can be shuttled through. The suture with the loop is pulled, and the contralateral suture is shuttled through the path of that suture pass, then through the suture anchor thereby creating a knotless medial bridge. Next, the suture ends that remain are now each passed approximately 5 mm lateral to the anchors. The lateral suture ends are tied thereby creating a lateral knotted bridge in a double row configuration. The end result is a knotless medial bridge with a lateral knotted bridge over the rotator cuff tendon.
Fig. 2.
Technique Guide for new Double Row Equivalent. A –Seat two double armed, looped suture anchors and pass suture through tendon in desired position (each bite should be 8–10 mm apart. B –Pass a suture tail from one anchor through the tail loop of the contralateral anchor. C –Next, the anchors are linked by pulling the contralateral suture limb –this will pull the suture through the second anchor. D –knotless medial bridge is created. E –Pull suture tails to compress tendon against bone. F –Join free ends of the suture with a lateral knot after appropriate tensioning of the construct.
The lateral knot acts as the final tensioner. In this system, both the medial and lateral bridges are created using a single suture via the shuttling mentioned above in the technique. Given this, the two rows can be tensioned evenly whereas in the current systems, the medial and lateral rows are NOT interconnected and tensioned independently from another. This potentially leads to different contact forces over the footprint rather than a uniform, even tension.
The trans-osseous equivalent #1 was used with standard technique in Group A which includes two double armed medial anchors that are crossed and pulled down laterally with a knotless anchor. For trans-osseous equivalent #2 in Group B, the technique mirrored Group A with the exception of different medial anchors and an inclusion of a medial bridge. Two double armed medial anchors were placed, a knotless medial bridge was formed, then one arm from each anchor was crossed and all sutures were brought down to the greater tuberosity via knotless suture anchors. No medial bridge was created in Group A. There was a knotless medial bridge created in Group B. The new double row equivalent was performed in Group C to provide fixation and imitate the anatomic footprint (Fig. 2, see Surgical technique above).
All surgeries were performed by a single Board Certified Orthopedic Surgeon in Sports Medicine who has significant experience with all systems in the arthroscopic and open setting. The manufacturer recommendations and surgical technique guides were followed for each anchor system.
4. Biomechanical testing
Dynamic cyclic fatigue followed by static load to failure testing was performed on each specimen. The humerus was fixed to the table using a vice and positioned at a 30° angle above the horizontal. The tendon was then clamped to the actuator of the test frame. A load-displacement plot was generated from each test.
Pressure data were collected via a Tekscan pressure sensor immediately after implantation of fixation and rotator cuff footprint characteristics (area and pressure) were extracted.
During cyclic loading, each specimen was pre-loaded to 10 N for 60 s followed by cycling from 10 N to 180 N at a rate of 100 N/s for 30 cycles. Hysteresis and stiffness were calculated from the load-displacement curve. Hysteresis was defined as the area inside of one loop (one cycle) of the plot. Stiffness was defined as the slope of a line drawn from the points of minimum and maximum load on one loop (one cycle) of the plot. Initial hysteresis and stiffness were recorded after the third cycle for each tendon that survived three cycles. Final hysteresis and stiffness were calculated for the 30th cycle in those tendons that survived that many cycles, or for the final cycle with a sinusoidal waveform prior to tendon failure. In addition, initial and final strain and gap formation were collected at the same cycles that hysteresis and stiffness measurements were.
For load to failure, each specimen was preloaded with 10 N for 60 s to remove the slack then loaded at a rate of 1 mm/s until construct failure. Ultimate load, yield load, and displacement at yield were calculated from the load-displacement curve. Energy absorbed was defined as the area under the load-displacement curve from the initiation of the test to the ultimate load endured by any given tendon.
Force and displacement of the actuator were recorded during the duration of both modes of testing. Images were taken at the beginning, throughout, and at the end of both testing modules.
Finally, a survival analysis was performed to analyze the percentage of specimens within a group that survived a given number of cycles.
Significance was analyzed using paired t-test where p < 0.05 was deemed significant.
5. Results
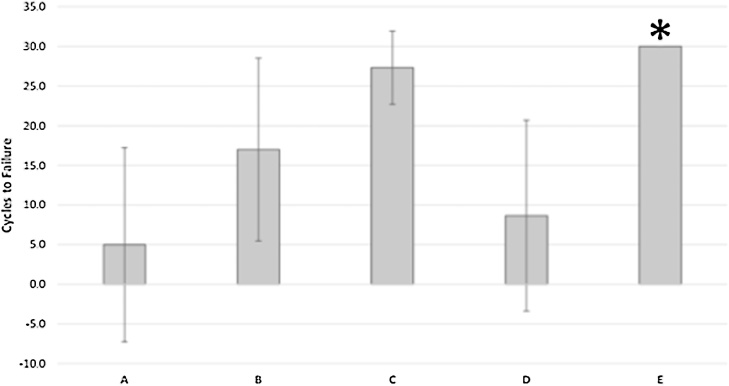
Group C demonstrated significantly higher ultimate loads (415 N) compared with the other groups (A, p = 0.01; B, p = 0.006) (Table 2). It took approximately 2.5–3 times more force for Group C anchor configuration to fail, compared with the other groups. In addition to having significantly higher ultimate load, Group C was also superior in the survival analysis surviveing all 30 cycles of testing (Fig. 3).
Table 2.
Construct Ultimate Strength compared to Group C. Strength measured in Newtons with standard deviation in parentheses. Significance set at P < 0.05. A–Trans-Osseous Equivalent #1. B–Trans-Osseous Equivalent #2. C–Double Row Equivalent.
| Group | Number of Specimens | Ultimate Strength, N | p-value |
|---|---|---|---|
| A | 6 | 158 (167) | 0.01 |
| B | 6 | 142 (60) | 0.006 |
| C (Comparison Group) | 6 | 415 (233) | N/A |
Fig. 3.
Survival Analysis Plot. The survival analysis plot shows what percent of each group survived a given number of cycles. Cycles to failure averaged for each group with data presented as mean +/1 standard deviation. The asterisk demonstrates the group that had each specimen complete all 30 cycles of testing. A – Trans-osseous Equivalent #1. B –Trans-osseous Equivalent #1. C –New Double Row Equivalent.
No statistical difference in hysteresis or stiffness was observed between the groups (Table 3).
Table 3.
Hysteresis and Stiffness Compared to Group C. N = Newton. mm = millimeter. Standard Deviation in parentheses. Significance set at p < 0.05. A–Trans-Osseous Equivalent #1. B–Trans-Osseous Equivalent #2. C–Double Row Equivalent.
| Group | Number of Specimens | Initial Hysteresis, N*mm | Final Hysteresis, N*mm | Initial Stiffness, N/mm | Final Stiffness, N/mm | p-value |
|---|---|---|---|---|---|---|
| A | 1 | 52 (0) | 44 (0) | 61 (0) | 54 (0) | 0.92 |
| B | 3 | 136 (50) | 84 (25) | 54 (19) | 62 (4) | 0.32 |
| C (Comparison Group) | 6 | 110 (27) | 63 (15) | 62 (7) | 61 (7) | NA |
There was no statistical difference in total contact area or contact pressure amongst the groups. However, there was a trend toward Group C having the highest contact pressure amongst all tendons (0.19 Mpa) (Table 4).
Table 4.
Contact Area and Pressure Compared to Group C. mm^2 = area in squared millimeters. Mpa = megapascal. Standard deviation in parentheses. Significance set at p < 0.05. A–Trans-Osseous Equivalent #1. B–Trans-Osseous Equivalent #2. C–Double Row Equivalent.
| Group | Number of Specimens | Contact Area, mm^2 | p-value | Contact Pressure, Mpa | p-value |
|---|---|---|---|---|---|
| A | 3 | 13 (7) | 0.7 | 0.15 (0.03) | 0.7 |
| B | 3 | 30 (7) | 0.12 | 0.13 (0.02) | 0.32 |
| C (Comparison Group) | 3 | 15 (3) | NA | 0.19 (0.02) | NA |
In terms of how the constructs failed, Group A and B failed due to tendon failure. In Group C, two tendons failed due to suture failure, while the remaining four were due to tendon failure. In Group C, the two constructs that failed at the suture required more than two times the amount of force compared to the tendon failure constructs.
Table 5 demonstrates the load at yield and energy absorbed.
Table 5.
Load at Yield and Displacement at Yield. Standard deviations are presented in parentheses. Groups A and B each only had one specimen complete the predesignated number of cycles to be counted in the calculation. N = Newtons. mm = millimeters. A–Trans-Osseous Equivalent #1. B–Trans-Osseous Equivalent #2. C–Double Row Equivalent.
| Group | Number of Specimens | Load at Yield (N) | Displacement at Yield (mm) | Energy Absorbed (N*mm) |
|---|---|---|---|---|
| A | 1 | 315 (0) | 5.0 (0.0) | 8133 (0) |
| B | 1 | 229 (0) | 4.1 (0.0) | 1462 (0) |
| C | 6 | 223 (21) | 3.8 (1.0) | 2696 (2935) |
6. Discussion
The goal of our study was to compare a new double-row configuration to standard linked and unlinked transosseous-equivalent rotator cuff configurations. The theory behind the new double row equivalent system is that an even tensioning and distribution of force over the tendon can be accomplished with two anchors. This is accomplished by linking the sutures on the medial row to avoid the inherent toggle created by knots that can potentially cause attritional wear of the tendon. The knotted lateral row allows for the even distribution of tension throughout the entire system with an additional suture bridge over the tendon. This system allows for increased tendon passes and increased areas of direct pressure to the anatomic footprint, while limiting the number of total anchors used.
It has been hypothesized that contact pressure is a key variable in rotator cuff tendon healing.17, 18 Burkhart et al.13 showed a significantly higher pressurized contact area in the diamondback repair versus other configurations, while Park et al.18, 20 demonstrated increased pressurized contact area of the transosseous equivalent method compared with a double row. These studies also demonstrated the transosseous-equivalent design to have increased ultimate load. The transosseous-equivalent relies on increased suture crossover rather than additional suture passes or any reliance on the lateral row for direct fixation. Park et al. reported the importance of bridging the medial row anchors to increase the pressurized contact area; however, this did not increase ultimate load in their study.21 Other studies showed the medial row increases the pressurized contact area and also strengthened the overall construct,22 further demonstrating the importance of the medial row.23
Our results for Group C (new double row equivalent), which used increased tendon passes while bridging the medial and lateral rows, showed significantly increased ultimate load-to-failure compared with all other constructs. While the contact pressure was not significantly different, Group C had a strong trend toward increased pressure versus all other groups, which as noted above, is a potential component in tendon healing. Previous studies have shown that knotted double row transosseous equivalent configurations have the strongest biomechanical strength.13, 14, 15, 22, 23, 24 The worst performers in terms of ultimate strength were the knotless groups, A and B. We hypothesize that this is largely due to the inability to tension knotless systems appropriately. Last, while compression at the bone-tendon interface is theoretically important for healing, Cho et al. showed a possibility of secondary tendon necrosis and re-tear at the medial row sutures.25
The survival curve for each construct should be noted. Group C was the only group that survived all 30 cycles. The knotless systems (Group A and B) demonstrated decreased survival in comparison. In addition, Load at Yield (Table 5) was calculated in samples that survived complete cycling. This again demonstrates the resilience and strength of the new double row equivalent system.
In our study, the new double row equivalent construct proved to have equivocal contact pressure, contact area, and stiffness as standard techniques, while having significantly improved survival and load-to-failure. This may be explained by its ability to have four tendon passes with only two suture bridges overlying the tendon, one medial and one lateral. Standard double row configurations use two tendon passes via medial anchors, which are then secured down to lateral anchors, with or without suture bridges. In transosseous configurations, the pressure is conferred by simple overlying crossed sutures without any added force generated from the lateral anchor sutures. Ultimately, the new double row equivalent system allows for an efficient method of forming a knotless medial bridge, which is advantageous for strength of the construct. In addition, it eliminates the medial knot allowing for even tensioning through the eyelets of the anchors.
There are a number of limitations in this study. First, it is a biomechanical study, which does not account for typical post-operative motion as well as biological healing nor does it account for multidirectional movements of rotator cuff in the real world. Second, we used bovine infraspinatus tendons rather than fresh frozen human cadaveric tendons; however, bovine shoulder has been shown to be a useful and consistent model for experimentation.26 Third, increasing the sample size in each group may have resulted in more significant differences. Fourth, we used humerus saw bones rather than fresh cadaveric bone which may not be as generalizable to the real world. However, sawbones provide controlled density in this setting for biomechanical testing, where cadaveric bones are more heterogeneous in their cancellous makeup. Fifth, there is the possibility of inherent bias given the new double row equivalent system was created by one of the authors, however we avoided bias where we were able in the study plan.
In summary, this study demonstrates a new suture technique with superior survival and ultimate load, while maintaining equivocal contact pressure, contact area and stiffness compared to transosseous equivalent configurations. Further studies in the clinical setting are warranted to ensure the clinical outcomes are as promising as the biomechanical data.
Conflict of interest
None.
Disclosure statement
We have a single disclosure and that is Joseph Donahue, MD is the founder, patent holder and stock holder of Stabilynx – the new technique studied in this manuscript.
Contributor Information
Sean Robinson, Email: spcrobinson1@gmail.com.
Henry Krigbaum, Email: HenryKrigbaum@gmail.com.
Jon Kramer, Email: JonDKramer@gmail.com.
Connor Purviance, Email: cpurviance@taylorcollaboration.org.
Robin Parrish, Email: rparrish@taylorcollaboration.org.
Joseph Donahue, Email: donahue@stanfordalumni.org.
References
- 1.Hansen M.L., Otis J.C., Johnson J.S. Biomechanics of massive rotator cuff tears: implications for treatment. J Bone Joint Surg Am. 2008;90(2):316–325. doi: 10.2106/JBJS.F.00880. [DOI] [PubMed] [Google Scholar]
- 2.Curtis A.S., Burbank K.M., Tierney J.J. The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy. 2006;22(6):609e1. doi: 10.1016/j.arthro.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Grimberg J., Diop A., Kalra K. In vitro biomechanical comparison of three different types of single- and double-row arthroscopic rotator cuff repairs: analysis of continuous bone-tendon contact pressure and surface during different simulated joint positions. J Shoulder Elbow Surg. 2010;19(2):236–243. doi: 10.1016/j.jse.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Smith C.D., Alexander S., Hill A.M. A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2006;88(11):2425–2431. doi: 10.2106/JBJS.E.00697. [PubMed. Web] [DOI] [PubMed] [Google Scholar]
- 5.Dines J.S., Bedi A., ElAttrache N.S. Single-row versus double-row rotator cuff repair: techniques and outcomes. J Am Acad Orthopaedic Surg. 2010;18(2):83–93. doi: 10.5435/00124635-201002000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Quigley R.J., Gupta A., Oh J.H. Biomechanical comparison of single-row, double-row, and transosseous-equivalent repair techniques after healing in an animal rotator cuff tear model. J Orthop Res. 2013;31(8):1254–1260. doi: 10.1002/jor.22363. [DOI] [PubMed] [Google Scholar]
- 7.Demirhan M., Atalar A.C., Kilicoglu O. Primary fixation strength of rotator cuff repair techniques: a comparative study. Arthroscopy. 2003;19(6):572–576. doi: 10.1016/s0749-8063(03)00126-9. [Print] [DOI] [PubMed] [Google Scholar]
- 8.Christoforetti J.J., Krupp R.J., Singleton S.B. Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Shoulder Elbow Surg. 2012;21(4):523–530. doi: 10.1016/j.jse.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Charousset C., Grimberg J., Duranthon L.D. Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair?: a prospective, nonrandomized, comparative study of double-Row and single-Row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med. 2007;35(8):1247–1253. doi: 10.1177/0363546507301661. [DOI] [PubMed] [Google Scholar]
- 10.Ma H.L., Chiang E.R., Wu H.T. Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: a prospective randomized trial. Arthroscopy. 2012;28(1):16–24. doi: 10.1016/j.arthro.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Ozbaydar M., Elhassan B., Esenyel C. A comparison of single-versus double-row suture anchor techniques in a simulated repair of the rotator cuff: an experimental study in rabbits. J Bone Joint Surg British. 2008;90(10):1386–1391. doi: 10.1302/0301-620X.90B10.20862. [DOI] [PubMed] [Google Scholar]
- 12.Liem D., Dedy N.J., Hauschild G. In vivo blood flow after rotator cuff reconstruction in a sheep model: comparison of single versus double row. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):470–477. doi: 10.1007/s00167-013-2429-8. [DOI] [PubMed] [Google Scholar]
- 13.Burkhart S.S., Denard P.J., Obopilwe E. Optimizing pressurized contact area in rotator cuff repair: the diamondback repair. Arthroscopy. 2012;28(2):188–195. doi: 10.1016/j.arthro.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 14.Arrigoni P., Brady P., Burkhart S.S. The DoublePulley technique for DoubleRow rotator cuff repair. Arthroscopy. 2007;675:e1–e4. doi: 10.1016/j.arthro.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Kim K.C., Kwang J.R., Hyun D.S. Arthroscopic DoublePulley suture-bridge technique for rotator cuff repair. Arch Orthop Trauma Surg. 2008;128(11):1335–1338. doi: 10.1007/s00402-007-0527-0. [DOI] [PubMed] [Google Scholar]
- 16.Koganti A.K., Adamson G.J., Gregersen C.S. Biomechanical comparison of traditional and locked suture configurations for arthroscopic repairs of the rotator cuff. Am J Sports Med. 2006;34(11):1832–1838. doi: 10.1177/0363546506289701. [DOI] [PubMed] [Google Scholar]
- 17.Milano G., Grasso A., Zarelli D. Comparison between single-row and double-row rotator cuff repair: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2008;16(1):75–80. doi: 10.1007/s00167-007-0382-0. [DOI] [PubMed] [Google Scholar]
- 18.Park M.C., Cadet E.R., Levine W.N. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33(8):1154–1159. doi: 10.1177/0363546504273053. [DOI] [PubMed] [Google Scholar]
- 19.Bachus K.N., DeMarco A.L., Judd K.T. Measuring contact area, force, and pressure for bioengineering applications: using Fuji film and TekScan systems. Med Eng Phys. 2006;28(5):483–488. doi: 10.1016/j.medengphy.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 20.Park M.C., ElAttrache N.S., Tibone J.E. Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16(4):461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Park J.S., McGarry M.H., Campbell S.T. The optimum tension for bridging sutures in transosseous-equivalent rotator cuff repair: a cadaveric biomechanical study. Am J Sports Med. 2015;43(9):2118–2125. doi: 10.1177/0363546515590596. [DOI] [PubMed] [Google Scholar]
- 22.Pauly S., Fiebig D., Kieser B. Biomechanical comparison of four double-row speed-bridging rotator cuff repair techniques with or without medial or lateral row enhancement. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2090–2097. doi: 10.1007/s00167-011-1517-x. [DOI] [PubMed] [Google Scholar]
- 23.Busfield B.T., Glousman R.E., McGarry M.H. A biomechanical comparison of 2 technical variations of double-row rotator cuff fixation: the importance of medial row knots. Am J Sports Med. 2008;36(5):901–906. doi: 10.1177/0363546507312640. [DOI] [PubMed] [Google Scholar]
- 24.Barber A.F., Hapa O., Bynum J.A. Comparative testing by cyclic loading of rotator cuff suture anchors containing multiple high-strength sutures. Arthroscopy. 2010;26(9 Suppl):S134–S141. doi: 10.1016/j.arthro.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Cho N.S., Yi J.W., Lee B.G., Rhee Y.G. Retear patterns after arthroscopic rotator cuff repair: single row versus suture bridge technique. Am J Sports Med. 2010;38(April (4)):664–671. doi: 10.1177/0363546509350081. [DOI] [PubMed] [Google Scholar]
- 26.Petit C.J., Boswell R., Mahar A. Biomechanical evaluation of a new technique for rotator cuff repair. Am J Sports Med. 2003;31(November–December (6)):849–853. doi: 10.1177/03635465030310062001. [DOI] [PubMed] [Google Scholar]