Abstract
Retrospective review of the National Inpatient Sample was performed. LOS and IHM were assessed among TJA patients and assessed by comorbidity status.
LOS among TJA patients decreased from 4.31 to 5.87 days to 2.83–4.49 days. Relative risk for prolonged LOS among high comorbidity patients ranged from 3.01–5.62. IHM per 1,000 was 5.1 for revision THA, 1.8 for revision TKA, 1.1 for primary THA, and 0.4 for primary TKA. Relative risk for IHM in high comorbidity patients ranged from 443.9–780.9 (p < 0.0001). LOS and IHM decreased significantly across all TJA procedures. LOS and IHM among the highest comorbidity groups are unacceptably high.
Keywords: Total joint arthroplasty, Length of stay, Index hospitalization mortality, Comorbidity, Epidemiology
1. Introduction
Total joint arthroplasty (TJA) procedures have increased in volume continuously over the past several decades.1, 2, 3, 4, 5, 6 Previous studies have projected future volume of primary and revision TJA procedures.7,8 However, there has been little discussion of the marked recent changes in length of stay (LOS), index hospitalization mortality and comorbidity prevalence among the primary and revision TJA population since 2000.
Over the past 20 years, the literature has reported on clinical interventions to reduce LOS following TJA, which include improved perioperative pain management using multi-modal therapies,9, 10, 11, 12 and dedicated clinical pathways focused specifically on the post-operative arthroplasty patient.13, 14, 15, 16 Recent changes in TJA reimbursement strategies to contain costs, such as bundled payments, demonstrate that pre-discharge costs comprise the majority of expense of care within 30 days of the index procedure.17 Furthermore, previous studies have demonstrated that reimbursements that financially incentivize shorter LOS will lead to rapid decreases in LOS.18 Therefore, we expect these recent changes in reimbursement to lead to a decrease in LOS from 2000 to 2014.
Additionally, this study aims to quantify recent changes to safety related to TJA procedures. One study looked at index hospitalization mortality following primary TJA, which has demonstrated declines in recent decades.19 An earlier study assessed improvement in index hospitalization mortality following implementation of new anesthesia care techniques.20 Cardiac and pulmonary disease history has been associated with 30-day mortality following primary TJA.21 We expect to see similar trends with improved index hospitalization mortality following both primary and revision TJA procedures from 2000 to 2014, in light of modern improvements in anesthesia care and pre-operative screening methods.
Finally, this study aims to address overall changes in the health characteristics of the TJA population. Previous studies have noted increasing prevalence of comorbidity among TJA patients.22 Others have identified that comorbidities, such as obesity and diabetes, portend increased risk of post-operative infection rates and other perioperative complications.23 We expect to identify increasing prevalence of comorbidity among the TJA population from 2000 to 2014, in line with recent trends.
2. Methods
A retrospective review using discharge data from the National Inpatient Sample and the Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality from 2000 to 2014 was performed.24 This study was given exempt status by the local Institutional Review Board. This database contains 116 million patient records and is a representative sample of discharges among hospitals in the United States. Procedures were identified by International Classification of Diseases, Ninth Revision (ICD-9) codes corresponding to primary total hip arthroplasty (THA; 81.51), primary total knee arthroplasty (TKA; 81.54), revision THA (81.53, 00.70, 00.71, 00.72, 00.73), and revision TKA (81.55, 00.80, 00.81, 00.82, 00.83, 00.84). Procedure volume during the study period was evaluated using the appropriate weighting characteristics. Patient population characteristics were evaluated according to discharge variables included in the NIS database corresponding to LOS, index hospitalization mortality, and a comorbidity index score. Comorbidity index was divided into four categories as defined by the 3M All Patient Refined Diagnosis Related Group (APR-DRG) Risk of Mortality subgroups.25 These groups are classified as minor, moderate, major, and extreme likelihood of dying and based on a proprietary algorithm using ICD-9 diagnosis codes. Data for APR-DRGs is available for most patients starting in 2002, and for all patients starting in 2006.
Mean continuous variables were compared between 2000 and 2014 using t-test, and proportions were compared by Chi-square test. Linear regression was performed to assess trends in LOS, mortality, and comorbidity prevalence over time. Z-score and relative risk for LOS and mortality by comorbidity subgroup were performed with comparison to “Minor Comorbidity” set as baseline risk. Stata Statistical Software (College Station, TX) was used for all statistical analyses.26
3. Results
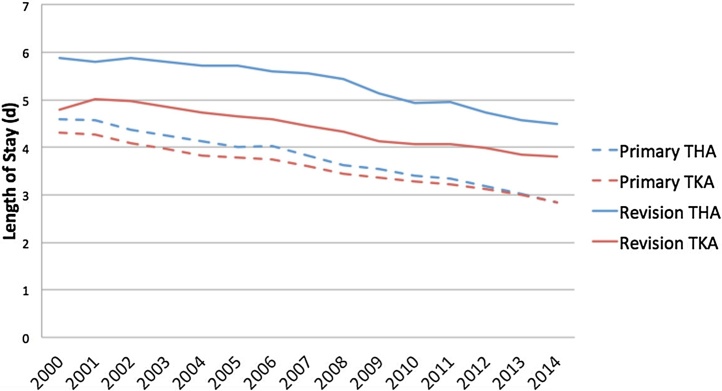
3.1. Procedural volume
From 2000 to 2014, TJA procedure volume increased among all categories. Primary THA increased from 160,282 to 371,605 procedures per year. Primary TKA increased from 274,467 to 680,886 procedures per year. Revision THA increased from 34,493 to 50,425 procedures per year. Revision TKA increased from 24,763 to 63,205 procedures per year. During this same time period, TJA population patient characteristics changed markedly. LOS decreased significantly from 2000 to 2014 across all TJA procedures (Fig. 1).
Fig. 1.
Length of stay (LOS) following primary and revision TJA procedures in the United States, 2000–2014.
3.2. Length of stay
Primary THA procedure LOS decreased from 4.59 d to 2.83 d (38% decrease, p < 0.01), primary TKA LOS decreased from 4.31 d to 2.84 d (34% decrease, p < 0.01), revision THA LOS decreased from 5.87 d to 4.49 d (24% decrease, p < 0.01), and revision TKA LOS decreased from 4.79 d to 3.80 d (21% decrease, p < 0.01). Regression models for all TJA procedure demonstrated a trend of 0.12 d to 0.80 d per year decreases in LOS (p < 0.01, R-square >0.90).
3.3. Index hospitalization mortality
Index hospitalization mortality among all TJA procedures demonstrated a statistically significant 60–70% decrease from 2000 to 2014. Primary THA index hospitalization mortality per 1,000 decreased from 3.5 in 2000 to 1.1 in 2014 (−69%, p < 0.01). Primary TKA index hospitalization mortality decreased from 1.7 in 2000 to 0.43 in 2014 (−75%, p < 0.01). Revision THA index hospitalization mortality decreased from 8.8 in 2000 to 5.1 in 2014 (−42%, p < 0.01). Revision TKA index hospitalization mortality decreased from 2.3 in 2000 to 1.8 in 2014 (−22%, p < 0.01).
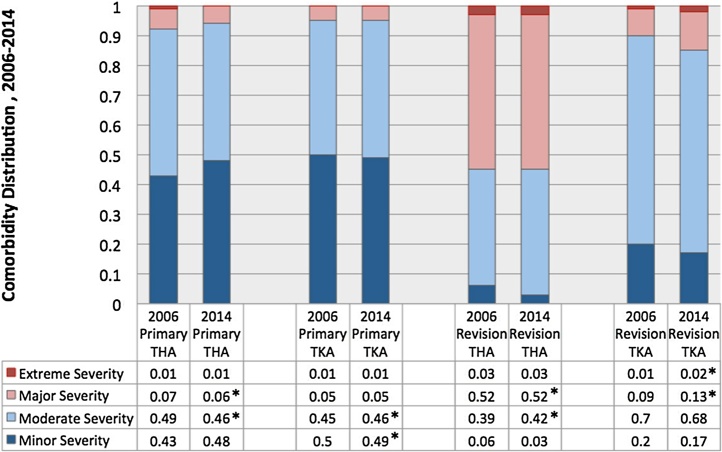
3.4. Comorbidity subgroup
Primary and revision TJA procedures differ significantly by comorbidity index (p < 0.01). As of 2014, revision THA patients demonstrate the highest proportion of major comorbidity (52%), followed by revision total knee (13%), primary THA (6%), and primary TKA (5%). The THA population demonstrated higher levels of comorbidity compared with the TKA population. Changes in comorbidity subgroup proportions are demonstrated in Fig. 2.
Fig. 2.
Comorbidity distribution among primary and revision TJA patients in the United States, 2006–2014.
*Indicates linear regression p-trend <0.05.
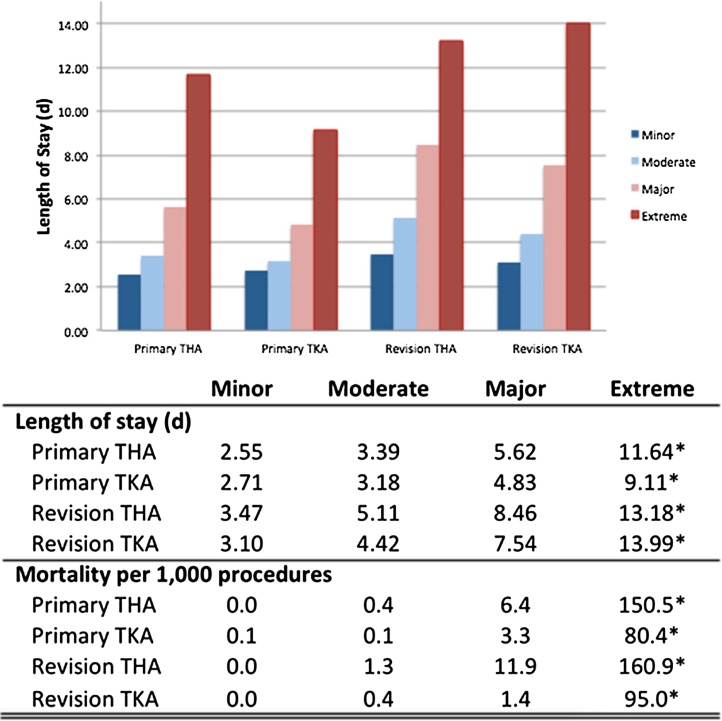
3.5. Comorbidity-stratified length of stay and index hospitalization mortality
LOS and index hospitalization mortality were stratified by comorbidity subgroup. (Fig. 3) LOS increased across comorbidity subgroups in all years. By 2014, LOS ranged 2.55 d to 3.47 d among TJA patients in the minor comorbidity subgroup. Among patients in the extreme comorbidity subgroup, LOS ranged 9.11 d–13.99 d. Revision procedures demonstrated longer LOS compared with primary procedures, and THA procedures demonstrated longer LOS compared with TKA procedures.
Fig. 3.
Length of stay and index hospitalization mortality stratified by comorbidity subgroup among primary and revision TJA patients in the United States, 2006–2014.
*Denotes t-test p-value <0.05 comparing extreme comorbidity subgroup compared with all other subgroups. All p-values recorded <0.01.
Relative risk of prolonged LOS (≥5 days) for extreme comorbidity in comparison to minor comorbidity subgroups ranged from 3.01 to 5.62 (95% CI 2.96–5.70, p < 0.0001) for primary and revision TJA procedures. (Table 1) The relative risk of extremely prolonged LOS (≥10 days) for the extreme comorbidity subgroup ranged from 6.36 to 8.61 (95% CI 6.12–9.02, p < 0.0001).
Table 1.
Relative risk for prolonged length of stay, extremely prolonged length of stay, and index hospitalization mortality stratified by comorbidity subgroup among primary and revision TJA patients in the United States, 2006–2014.
| Prolonged LOS (≥5 days) |
Extremely Prolonged LOS (≥10 days) |
Index Hospitalization Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| RR | P Value | RR | P Value | RR | P Value | ||||
| Primary Hip | |||||||||
| Minor | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| Moderate | 1.98 | (1.96–2.00) | <0.0001 | 1.36 | (1.34–1.39) | <0.0001 | 8.79 | (6.88–11.23) | <0.0001 |
| Major | 3.78 | (3.74–3.83) | <0.0001 | 3.09 | (3.01–3.19) | <0.0001 | 93.13 | (74.65–116.19) | <0.0001 |
| Extreme | 5.40 | (5.33–5.48) | <0.0001 | 7.25 | (7.02–7.49) | <0.0001 | 780.85 | (634.05–961.63) | <0.0001 |
| Primary Knee | |||||||||
| Minor | 1.00 | – | – | 1.00 | – | –j | 1.00 | – | – |
| Moderate | 1.72 | (1.71–1.74) | <0.0001 | 1.10 | (1.08–1.12) | <0.0001 | 3.86 | (3.15–4.75) | <0.0001 |
| Major | 3.67 | (3.63–3.72) | <0.0001 | 2.19 | (2.12–2.26) | <0.0001 | 37.78 | (31.38–45.49) | <0.0001 |
| Extreme | 5.62 | (5.55–5.70) | <0.0001 | 6.62 | (6.42–6.83) | <0.0001 | 494.87 | (425.80–575.15) | <0.0001 |
| Revision Hip | |||||||||
| Minor | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| Moderate | 1.79 | (1.76–1.82) | <0.0001 | 1.78 | (1.72–1.84) | <0.0001 | 9.26 | (6.02–14.25) | <0.0001 |
| Major | 2.63 | (2.59–2.67) | <0.0001 | 3.73 | (3.60–3.87) | <0.0001 | 62.01 | (41.43–92.79) | <0.0001 |
| Extreme | 3.01 | (2.96–3.06) | <0.0001 | 6.36 | (6.12–6.61) | <0.0001 | 443.85 | (301.26–653.92) | <0.0001 |
| Revision Knee | |||||||||
| Minor | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| Moderate | 1.94 | (1.90–1.98) | <0.0001 | 1.70 | (1.63–1.78) | <0.0001 | 6.44 | (3.52–11.75) | <0.0001 |
| Major | 3.36 | (3.29–3.43) | <0.0001 | 4.05 | (3.86–4.25) | <0.0001 | 46.54 | (26.82–80.76) | <0.0001 |
| Extreme | 4.32 | (4.23–4.40) | <0.0001 | 8.61 | (8.21–9.02) | <0.0001 | 517.76 | (314.67–851.92) | <0.0001 |
The values are given as relative risk with 95% CI in parentheses.
Mortality per 1,000 procedures increased across comorbidity subgroups in all years (p < 0.01). (Fig. 3) By 2014, index hospitalization mortality per 1,000 procedures was near 0 for all primary and revision TJA procedures among patients with minor comorbidity. With increasing comorbidity subgroup, index hospitalization mortality per 1,000 procedures increased. Revision THA demonstrated the highest mortality rate in all subgroups. THA procedures demonstrated higher mortality than TKA procedures, and revision procedures demonstrated higher mortality than primary procedures. Index hospitalization mortality for revision THA among patients in the extreme comorbidity subgroup was 160.9 per 1,000 procedures in 2014.
Relative risk of index hospitalization mortality for extreme comorbidity compared with minor comorbidity subgroup ranged from 443.85 to 780.85 (95% CI 301.26–961.63, p < 0.0001) among TJA procedures. (Table 1) Relative risk for moderate and major comorbidity subgroups was also significantly elevated in comparison to the minor comorbidity subgroup.
4. Discussion
As anticipated, LOS has continued to decrease significantly across all TJA procedures. This has likely been prompted by recent changes in post-operative care and reimbursement models. Medicare provides payment for the majority of TJA patients. The Medicare repayment structure is based on historic averages of LOS, which has steadily decreased over recent years, as noted in this study and others. Medicare incentivizes early discharge by decreasing reimbursement for each hospital day.27
For 2014, the hospital reimbursements from Medicare in one health system database were $7406 for Day 1 (to incorporate cost of implant), $3703 for Day 2, and $370 for Day 327 For most hospitals, this equates to a net loss of funds for any patient staying 3 days or longer. Coordination between pre-operative evaluation, anesthesia, pain protocols, physical therapy, and multidisciplinary discharge pathways has facilitated this continued advance toward shorter LOS.
Kirksey et al. noted decreased mortality among primary TJA patients from 1998–200819 While LOS has decreased, index hospitalization mortality has concurrently dropped significantly for all TJA procedures. However, the revision THA population has four times greater rates of comorbidity and nearly three times greater incidence of index hospitalization mortality than revision TKA, 4.5 times greater risk than primary THA, and 13 times greater risk than primary TKA.
Patients with more severe comorbidities require significantly longer LOS than the average TJA patient. Based on the reimbursement schedule above, the average patient in the Major or Extreme comorbidity subgroups for primary and revision TJA procedures will exceed the point at which admissions are financially advantageous by several days. Even revision TJA patients in the Moderate comorbidity subgroup exceed the average reimbursed LOS.
Most remarkable is the extent to which risk for extremely prolonged LOS and index hospitalization mortality is increased with comorbidity subgroup, even among primary TJA procedures. Given the unacceptably high rate of mortality demonstrated in extreme and major comorbidity subgroups, surgeons should take caution when operating on patients in these groups and provide adequate informed consent pre-operatively. Future research may focus on specific modifiable risk factors that could optimize the patient to move them to lower comorbidity category with a more acceptable risk profile.
Our model is based on data derived from the HCUP NIS databases and the United States Census Bureau population projections. These databases have been previously used by others2,4,5,8,19,28 to estimate TJA procedure volume. The HCUP NIS is the largest resource available for estimating annual national surgical procedure volumes. The main limitation is due to the shortcomings inherent with using a large administrative database extracted from discharge data. Namely, the accuracy of the data is dependent upon the codes entered into the billing claims data in the discharge record. Certain diagnoses may be overlooked, particularly if they are without value for reimbursement, and individual records are unable to be reviewed to confirm accuracy. Further, specific variables, such as body mass index, estimated blood loss during procedures, ASA classification, or other variables that may assist with current and future analyses are unavailable. However, for the purpose of this study, the HCUP NIS is the best available database for evaluating national trends in surgical procedure volumes.
Future research may evaluate clinical postoperative outcomes aside from mortality, such as patient satisfaction and function scores. These outcomes are not available in our current database.
Conflict of interest
No conflict of interest pertaining to this unfunded research study.
References
- 1.Kim S. Changes in surgical loads and economic burden of hip and knee replacements in the US: 1997–2004. Arthritis Rheum. 2008;59(April (4)):481–488. doi: 10.1002/art.23525. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S., Mowat F., Ong K., Chan N., Lau E., Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(July (7)):1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz S.M., Ong K.L., Schmier J., Zhao K., Mowat F., Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009;24(February (2)):195–203. doi: 10.1016/j.arth.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz S.M., Ong K.L., Lau E., Bozic K.J. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96(April (8)):624–630. doi: 10.2106/JBJS.M.00285. [DOI] [PubMed] [Google Scholar]
- 5.Losina E., Thornhill T.S., Rome B.N., Wright J., Katz J.N. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(February (3)):201–207. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh J.A., Vessely M.B., Harmsen W.S. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969–2008. Mayo Clin Proc. 2010;85(10):898–904. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurtz S.M., Ong K.L., Schmier J. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;(October (89 Suppl. 3)):144–151. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 8.Kurtz S.M., Lau E., Ong K., Zhao K., Kelly M., Bozic K.J. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(October (10)):2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duellman T.J., Gaffigan C., Milbrandt J.C., Allan D.G. Multi-modal, pre-emptive analgesia decreases the length of hospital stay following total joint arthroplasty. Orthopedics. 2009;32(March (3)):167. [PubMed] [Google Scholar]
- 10.Peters C.L., Shirley B., Erickson J. The effect of a new multimodal perioperative anesthetic regimen on post-operative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplasty. 2006;21(September (6 Suppl. 2)):132–138. doi: 10.1016/j.arth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Salinas F.V., Liu S.S., Mulroy M.F. The effect of single-injection femoral nerve block versus continuous femoral nerve block after total knee arthroplasty on hospital length of stay and long-term functional recovery within an established clinical pathway. Anesth Analg. 2006;102(April (4)):1234–1239. doi: 10.1213/01.ane.0000198675.20279.81. [DOI] [PubMed] [Google Scholar]
- 12.Wang H., Boctor B., Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med. 2002;27(April (2)):139–144. doi: 10.1053/rapm.2002.29253. [DOI] [PubMed] [Google Scholar]
- 13.Forrest G., Fuchs M., Gutierrez A., Girardy J. Factors affecting length of stay and need for rehabilitation after hip and knee arthroplasty. J Arthroplasty. 1998;13(February (2)):186–190. doi: 10.1016/s0883-5403(98)90097-3. [DOI] [PubMed] [Google Scholar]
- 14.Forrest G.P., Roque J.M., Dawodu S.T. Decreasing length of stay after total joint arthroplasty: effect on referrals to rehabilitation units. Arch Phys Med Rehabil. 1999;80(February (2)):192–194. doi: 10.1016/s0003-9993(99)90120-x. [DOI] [PubMed] [Google Scholar]
- 15.Husted H., Holm G., Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79(April (2)):168–173. doi: 10.1080/17453670710014941. [DOI] [PubMed] [Google Scholar]
- 16.Husted H., Hansen H.C., Holm G. What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg. 2010;130(February (2)):263–268. doi: 10.1007/s00402-009-0940-7. [DOI] [PubMed] [Google Scholar]
- 17.Bozic K.J., Ward L., Vail T.P., Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res. 2014;472(January (1)):188–193. doi: 10.1007/s11999-013-3034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan L., Koepsell T.D., Deyo R.A. The effect of Medicare’s payment system for rehabilitation hospitals on length of stay, charges, and total payments. N Engl J Med. 1997;337(October (14)):978–985. doi: 10.1056/NEJM199710023371406. [DOI] [PubMed] [Google Scholar]
- 19.Kirksey M., Chiu Y.L., Ma Y. Trends in in-hospital major morbidity and mortality after total joint arthroplasty: United States 1998–2008. Anesth Analg. 2012;115(August (2)):321–327. doi: 10.1213/ANE.0b013e31825b6824. [DOI] [PubMed] [Google Scholar]
- 20.Sharrock N.E., Cazan M.G., Hargett M.J., Williams-Russo P., Wilson P.D. Changes in mortality after total hip and knee arthroplasty over a ten-year period. Anesth Analg. 1995;80(February (2)):242–248. doi: 10.1097/00000539-199502000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Parvizi J., Sullivan T.A., Trousdale R.T., Lewallen D.G. Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg Am. 2001;83-A(August (8)):1157–1161. doi: 10.2106/00004623-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Memtsoudis S.G., Della Valle A.G., Besculides M.C., Gaber L., Laskin R. Trends in demographics, comorbidity profiles, in-hospital complications and mortality associated with primary knee arthroplasty. J Arthroplasty. 2009;24(June (4)):518–527. doi: 10.1016/j.arth.2008.01.307. [DOI] [PubMed] [Google Scholar]
- 23.Namba R.S., Paxton L., Fithian D.C., Stone M.L. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20(October (7 Suppl. 3)):46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 24.HCUP Nationwide and National Inpatient Sample (NIS) Agency for Healthcare Research and Quality; Rockville, MD: 2000. Healthcare cost and utilization project (HCUP) 2000–2014. [Google Scholar]
- 25.Averill R., Goldfield N., Steinbeck B. Vol. 1997. 2017. (Development of all patient refined DRGs (APR-DRGs)). September (23) [Google Scholar]
- 26.Statacorp . 2015. Stata statistical software: release 14. [Google Scholar]
- 27.Accelero Health Partners . 2014. Length of stay is critical for total hip and knee replacement cost of care. 2017 (23 September) [Google Scholar]
- 28.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(April (4)):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]