Abstract
Background
We investigated the clinical progress and bacteriological characteristics of infectious adverse events (AEs) following acupuncture and compared patient characteristics between serious and non-serious outcome groups.
Methods
A retrospective observational study was conducted in 1,174 patients with infectious complications associated with acupuncture at the emergency department (ED) in a tertiary hospital in Korea between 2010 and 2014. Serious outcome was defined as development of septic shock, admission to intensive care unit (ICU) or attaining permanent morbidity.
Results
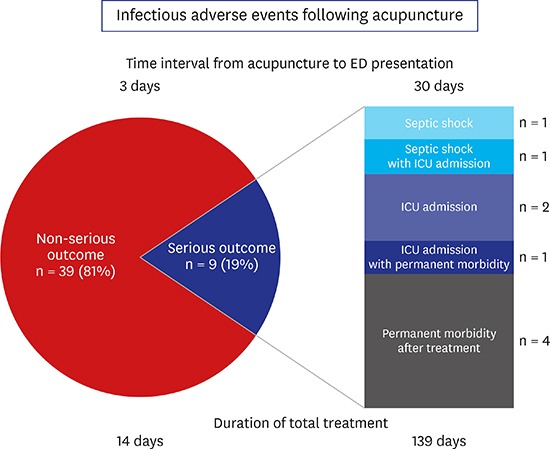
Forty-eight patients had certain causality and cellulitis, necrotizing fasciitis and osteomyelitis were common in order. Among them, 9 patients (18.8%) were categorized into serious outcome group, and they showed devastating outcomes such as septic shock (n = 2), ICU admission (n = 4), and permanent sequelae (n = 5). The serious group had delayed admission to the ED after acupuncture (30.0 [4.0–55.0] vs. 3.0 [1.0–10.0] days, P = 0.023). Methicillin-sensitive Staphylococcus aureus was the most frequently identified microorganism. The patients in the serious group required longer treatment duration (139.0 [49.0–183.5] vs. 14.0 [7.0–34.0] days, P < 0.001) as well as more operation with local (44.4% vs. 10.3%, P = 0.031) or general anaesthesia (33.3% vs. 2.6%, P = 0.017).
Conclusion
The infectious AEs after acupuncture may cause serious outcomes. Patients and primary physicians should be aware of the risk of infectious complications and make efforts to prevent them.
Keywords: Acupuncture, Complications, Infection
Graphical Abstract
INTRODUCTION
Acupuncture is becoming popular as an effective treatment method in complementary and alternative medicine.1,2 Acupuncture is a relatively safe procedure in the hands of qualified practitioners and rarely results in serious complications. Most of the adverse events (AEs) reported were pain, bleeding, bruising, and hematoma at the needle site.3,4,5,6 Nevertheless, a growing number of studies on serious AEs after acupuncture have been reported, which indicates that physicians and patients should be aware of the varied presentations and level of severity of these AEs.7,8,9,10 However, infectious AEs after acupuncture have not been studied well after the use of disposable needles was introduced and the popularization of heath knowledge. Moreover, some previous reports of infectious AE have focused on the incidence and diagnosis,1,4,11 and only few studies have provided insight into the clinical progress and bacteriological characteristics after the diagnosis of infectious AEs.
In view of this unclear situation, we aimed to investigate the clinical and bacteriological characteristics of infectious AEs following acupuncture and to determine the patient characteristics that cause serious outcomes in comparison with a non-serious outcome group. The results of this study could be important because unrecognition and ignorance of AEs could be associated with delay of appropriate treatment and worse outcomes.
METHODS
Study design and population
A retrospective observational study was conducted at the emergency department (ED) of a university-affiliated teaching hospital in Seoul, Korea, with an annual census of approximately 100,000 visits, between 1 January 2010 and 31 December 2014. We identified patients who were receiving acupuncture treatment by using a de-identified clinical database in our institute. We retrieved electronic medical records prepared by physicians and nurses that included terms such as “acupuncture” (“침”[chim] in Korean) and “oriental medical clinic” (“한의원” [Haneuiwon] in Korean).
In this study, 1,174 consecutive adult patients (≥ 18 years old) who were admitted to our ED after receiving acupuncture were eligible to enrol. Two emergency physicians reviewed all the cases independently for inclusion based on the causality between acupuncture and ED presentation and infection. The World Health Organization (WHO)-Uppsala Monitoring Centre causality scale was applied to assess the causality (certain, probable/likely, possible, unlikely, or unclassified/unclassifiable).12 Any disagreement was resolved through discussion. Serious outcome was defined as development of septic shock, admission to intensive care unit (ICU) or attaining permanent morbidity after treatment.
Data collection
Patient clinical and demographic characteristics were collected from the de-identified clinical database, which included age, sex, history, clinical characteristics, diagnosis, treatment, and outcome. Specifically, we extracted data on the following: symptom for acupuncture treatment; underlying disease; medication; symptom onset after acupuncture; ED admission after acupuncture; punctured site; complication type; culture study; therapeutic methods; and duration required for recovery.
Statistical analysis
Continuous variables were expressed as means with standard deviations or medians with interquartile range if the assumption of a normal distribution was violated. All the variables were tested for normal distribution by using the Kolmogorov-Smirnov test. Categorical variables were expressed as numbers and percentages. The Student's t-test was used to compare the mean values of normally distributed continuous variables, whereas the Mann-Whitney U test was used to compare non-normally distributed continuous variables. The χ2 or Fisher's exact test was applied for categorical variables. A two-sided P value of < 0.05 was considered to be statistically significant. All statistical analyses were performed by using SPSS version 21.0 for Windows (SPSS Inc., Chicago, IL, USA).
Ethics statement
The Institutional Review Board of Asan Medical Center approved our study (approval number: 2015-0381) and waived the requirement for informed consent because of its retrospective design.
RESULTS
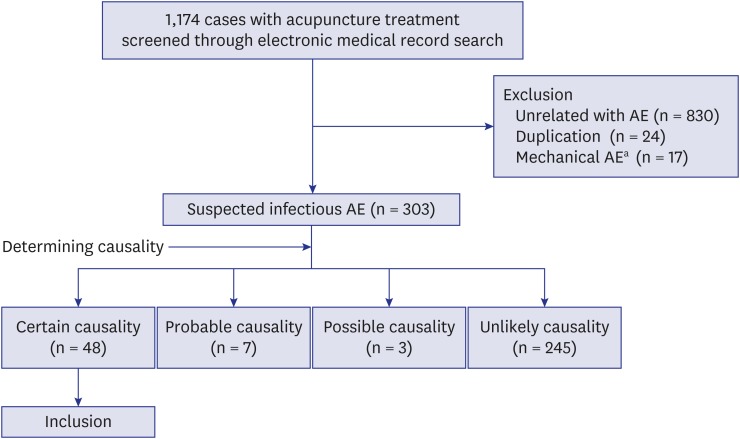
Between January 1, 2010, and December 31, 2014, 1,174 cases who admitted to our ED after acupuncture treatment were identified through electronic medical record search (Fig. 1). Of these cases, 871 were excluded from the study because of no relation with complications (n = 830), duplication (n = 24) and mechanical complications (n = 17). Mechanical complications consisted of 10 cases of pneumothorax (1 combined with pneumomediastinum), 5 cases of bleeding and bruise, and 2 cases of pneumoperitoneum.9 A total of 303 were evaluated for causality, and 48 cases with certain causality were finally included in the study.
Fig. 1. Patient selection flow diagram.
AE = adverse event.
aThere were 17 cases of mechanical AEs: 10 cases of pneumothorax (1 combined with pneumomediastinum), 5 cases of bleeding and bruise, and 2 cases of pneumoperitoneum.
The demographic and clinical findings of the patients with infectious complications after acupuncture are demonstrated in Table 1. The mean patient age was 62.4 ± 14.2 years, and the male-to-female ratio was 2:3. Nine patients (18.8%) were categorized into the serious outcome group. Most (95.8%) of the patients, including all the patients in the serious outcome group received acupuncture treatment for musculoskeletal pain. The median time interval from acupuncture to onset of adverse symptom in the serious outcome group was longer compared with that in the non-serious outcome group without statistical significance (median, 5.0 [0.5–38.5] vs. 1.0 [0.0–4.0] days, P = 0.120). The time interval from acupuncture to ED presentation was longer in the serious outcome group than in the non-serious outcome group (median, 30.0 [4.0–55.0] vs. 3.0 [1.0–10.0] days, P = 0.023). One third of them (n = 14, 29.2%) received multiple sessions of acupuncture, and the patients in the serious outcome group did more frequently (66.7% vs. 20.5%, P = 0.012). In the serious outcome group, joint (n = 4, 44.4%) and back (n = 4, 44.4%) were the most frequently punctured sites. By contrast, the joint (n = 17, 43.6%) and other extremities (n = 17, 43.6%) were the most common punctured site in the non-serious outcome group, followed by back (n = 4, 10.3%), and chest/abdomen (n = 1, 2.6%).
Table 1. Demographic and clinical data of the study patients.
| Variables | Total patients (n = 48) | Serious outcome group (n = 9) | Non-serious outcome group (n = 39) | P value | |
|---|---|---|---|---|---|
| Age, yr | 62.4 ± 14.2 | 69.3 ± 11.6 | 60.9 ± 14.4 | 0.107 | |
| Male | 21 (43.8) | 6 (66.7) | 15 (38.5) | 0.153 | |
| Symptom for acupuncture | > 0.990 | ||||
| Musculoskeletal pain | 46 (95.8) | 9 (100.0) | 37 (94.9) | ||
| Others | 2 (4.2) | 0 (0) | 2 (5.1) | ||
| Underlying disease | |||||
| Hypertension | 20 (41.7) | 5 (55.6) | 15 (38.5) | 0.460 | |
| Diabetes mellitus | 12 (25.0) | 2 (22.2) | 10 (25.6) | > 0.990 | |
| Cardiovascular disease | 6 (12.5) | 2 (22.2) | 4 (10.3) | 0.312 | |
| Chronic liver disease | 4 (8.3) | 1 (11.1) | 3 (7.7) | > 0.990 | |
| Anticoagulant medication | 10 (20.8) | 3 (33.3) | 7 (17.9) | 0.370 | |
| Adverse symptom onset after acupuncture, day | 1.0 (0.0–7.0) | 5.0 (0.5–38.5) | 1.0 (0.0–4.0) | 0.120 | |
| ED presentation after acupuncture, day | 4.5 (2.0–13.5) | 30.0 (4.0–55.0) | 3.0 (1.0–10.0) | 0.023 | |
| No. of acupuncture treatments | 0.012 | ||||
| Single | 34 (70.8) | 3 (33.3) | 31 (79.5) | ||
| Multiple | 14 (29.2) | 6 (66.7) | 8 (20.5) | ||
| Punctured site | 0.060 | ||||
| Joint | 21 (43.8) | 4 (44.4) | 17 (43.6) | ||
| Other extremities | 18 (37.5) | 1 (11.1) | 17 (43.6) | ||
| Back | 8 (16.7) | 4 (44.4) | 4 (10.3) | ||
| Chest/abdomen | 1 (2.1) | 0 (0) | 1 (2.6) | ||
Values are expressed as mean ± standard deviation, median (interquartile range), or as number (%).
ED = emergency department.
Table 2 summarizes the type and severity of the infectious complication that required treatments. The patients in the serious outcome group were compromised with necrotizing fasciitis (n = 5, 55.6%) and osteomyelitis (n = 4, 44.4%). Two patients (22.2%) in the serious outcome group were admitted our ED in a septic shock state. More than a half of the patients in the non-serious group showed cellulitis (n = 23, 58.9%). According to the patients' conditions, culture examinations using blood, pus, and tissue samples were performed and microorganisms were more frequently identified in the serious outcome group (77.8% vs. 32.1%). While most of the patients in the non-serious outcome group (n = 34, 87.2%) did not require invasive interventions, those in the serious group underwent operation with local anaesthesia such as debridement and incision and drainage (44.4% vs. 10.3%, P = 0.031) or with general anaesthesia (33.3% vs. 2.6%, P = 0.017).
Table 2. Type of infection and outcomes of the study patients.
| Variables | Total patients (n = 48) | Serious outcome group (n = 9) | Non-serious outcome group (n = 39) | P value | |
|---|---|---|---|---|---|
| Type of infection | 0.004 | ||||
| Cellulitis without abscess | 21 (43.8) | 0 (0) | 21 (53.8) | ||
| Cellulitis with abscess | 2 (4.2) | 0 (0) | 2 (5.1) | ||
| Necrotizing fasciitis | 11 (22.9) | 5 (55.6) | 6 (15.4) | ||
| Septic arthritis | 5 (10.4) | 0 (0) | 5 (12.8) | ||
| Osteomyelitis | 9 (18.8) | 4 (44.4) | 5 (12.8) | ||
| Septic shock | 2 (4.2) | 2 (22.2) | 0 (0) | 0.032 | |
| Culture examinationa | 37 | 9 | 28 | 0.024 | |
| Positive | 16 (43.2) | 7 (77.8) | 9 (32.1) | ||
| Negative | 21 (56.8) | 2 (22.2) | 19 (67.9) | ||
| Required therapeutic treatments | |||||
| Oral antibiotics | 34 (70.8) | 7 (77.8) | 27 (69.2) | > 0.990 | |
| Intravenous antibiotics | 36 (75.0) | 9 (100.0) | 27 (69.2) | 0.088 | |
| Operation with local anaesthesiab | 8 (16.7) | 4 (44.4) | 4 (10.3) | 0.031 | |
| Operation with general anaesthesia | 4 (8.3) | 3 (33.3) | 1 (2.6) | 0.017 | |
| Hospitalization to the general ward | 36 (75.0) | 9 (100.0) | 27 (69.2) | 0.088 | |
| Admitted at the ICU | 4 (8.3) | 4 (44.4) | 0 (0) | 0.001 | |
| Duration of hospitalizationc, day | 11.0 (0.0–47.5) | 78.0 (47.5–110.0) | 6.5 (0.0–28.3) | < 0.001 | |
| Duration of total treatmentc, day | 29.0 (8.0–79.0) | 139.0 (49.0–183.5) | 14.0 (7.0–34.0) | < 0.001 | |
Values are expressed as median (interquartile range) or as number (%).
ICU = intensive care unit.
aCulture examination such as blood, pus and tissue was not performed for 11 patients in the non-serious outcome group; bOperation with local anaesthesia represents debridement and/or incision and drainage; cThree patients in the non-serious outcome group were excluded because of transfer to another hospital.
Three-fourths of our study patients were admitted the hospital for treatment (100.0%, serious outcome group vs. 69.2%, non-serious outcome group, P = 0.088), and 4 patients (8.3%) were treated in the ICU. The median hospitalization duration of our study patients was 11.0 days, which was longer in the serious outcome group than in the non-serious group (78.0 [47.5–110.0] vs. 6.5 [0.0–28.3] days, P < 0.001). The median total treatment duration in all the patients was 29.0 days, but the patients in the serious group required much longer treatment duration (139.0 [49.0–183.5] vs. 14.0 [7.0–34.0] days, P < 0.001). Five patients in the serious outcome group had permanent morbidity after treatment, skin defects (n = 2), joint immobility (n = 1), toe amputation (n = 1), and chronic kidney disease (n = 1). Table 3 presents the identified microorganisms in our patients, such as Staphylococcus (n = 8), Streptococcus (n = 3), Mycobacterium (n = 2), and other gram-negative bacteria (n = 5).
Table 3. Identified microorganisms in the study patients.
| Microorganisms | Total patients (n = 48) | Serious outcome group (n = 9) | Non-serious outcome group (n = 38) | Blood culture | Pus culture | Tissue culture |
|---|---|---|---|---|---|---|
| Methicillin-sensitive Staphylococcus aureusa | 5 | 2 | 3 | 3 | 3 | 0 |
| Methicillin-resistant S. aureus | 3 | 2 | 1 | 2 | 2 | 0 |
| Streptococcus agalactiaea | 2 | 1 | 1 | 1 | 1 | 0 |
| Streptococcus viridans | 1 | 0 | 1 | 0 | 1 | 0 |
| Klebsiella pneumoniae | 2 | 1 | 1 | 2 | 0 | 0 |
| Escherichia coli | 2 | 1 | 1 | 1 | 1 | 1 |
| Fusobacterium varium | 1 | 0 | 1 | 1 | 0 | 0 |
| Mycobacterium tuberculosisa | 1 | 0 | 1 | 0 | 1 | 0 |
| NTM, unspecified | 1 | 1 | 0 | 0 | 0 | 1 |
| Total | 16 | 7 | 9 | 10 | 6 | 2 |
NTM = nontuberculous mycobacteria.
aMethicillin-sensitive S. aureus and S. agalactiae were identified in the same patient, and methicillin-sensitive S. aureus and M. tuberculosis were identified in another same patient.
DISCUSSION
In this study, we identified 48 patients with infectious AEs which occurred after acupuncture. The event ranged from focal soft tissue infection to septic shock. In particular, a substantial number of patients showed devastating outcomes such as septic shock (n = 2), ICU admission (n = 4), and permanent sequelae (n = 5), and they required long-term hospitalization (median, 78 days).
Although many acupuncture safety practice guidelines emphasize the proper sterile techniques for acupuncture procedures,3,13 a large gap still exists between these guidelines and actual clinical practice. Recent studies about AEs of acupuncture performed by regulated and qualified acupuncturists revealed the low incidence of serious AEs that could be fully recovered with adequate treatment.6,14,15 By contrast to the results of these studies, 9 (18.8%) of 48 patients in our study presented with serious AEs including development of septic shock, admission to ICU admission and suffering permanent sequelae, and consequently they required long-term hospitalization, including ICU care. This difference may reflect the real-world situation. Lack of adherence to sterile techniques, and infection control might have been the cause of the infectious AE. Another factor likely contributing to severity of infection was the delay between onset of symptoms and presentation at ED. With the increasing incidence of diabetes or immunocompromised patients, the qualifying training of acupuncturists should be systemized and the clinical procedure should be standardized to prevent the occurrence of infectious complications after acupuncture. In addition, acupuncturists should monitor and evaluate the possibility of AEs after acupuncture.
The identified microorganisms in our study were Staphylococcus (n = 8), Streptococcus (n = 3), Mycobacterium (n = 2), and other gram-negative bacteria (n = 5), which were consistent with those identified in previous reports about infections that occur after acupuncture.11 Gram-positive cocci are known as the most common pathogens of the skin and soft tissue infection. However, Mycobacterium played an important role as a pathogen for those infections after acupuncture, usually reported as an outbreak associated with improper sterilization of equipment.8,16,17,18 The patients with Mycobacterium in our study also delayed presentation to our ED, with a relatively long incubation period. In addition, gram-negative bacilli, including Klebsiella pneumoniae (n = 2), Escherichia coli (n = 2), and Fusobacterium varium (n = 1), caused skin and soft tissue infections in our study. The incidence of skin and soft tissue infections caused by gram-negative bacilli is lower than that caused by gram-positive cocci.19 Previous reports about gram-negative bacilli infections that occur after acupuncture did not state the possible cause of infections, but the mechanism of bacterial inoculation might be the translocation of organisms from other organs caused by the acupuncture needle overlying other structures.20
Most patients seemed to visit the ED without any delay, but some patients in the serious group delayed their hospital visit, resulting in worse outcomes. This delayed seeking for medical advice might be attributed to the patient's and acupuncturist's unrecognition of the possibility of AEs after acupuncture and the relatively indolent symptom caused by the pathogen.16,21 Additionally, the acupuncture site such as back might be another contributing factor for delayed presentation, which the patient could not notice the lesion. Patients should be aware of these infectious AEs because most of them may be prevented by early appropriate treatment.
The main limitation of our present study is its retrospective design with the potential biases inherent to this type of study such as selective and recall biases. The patients sometimes did not mention their previous acupuncture treatment before the doctor's specific question about it, which made doctors fail to associate the acupuncture procedure with the infection.20 Moreover, attending physicians would rather concentrate more on patients with severe infections, which resulted in our cohort being composed of severe cases rather than mild ones. In addition, the relative small number of patients (n = 48) might have contributed to the lack of statistical power of some results. Finally, our cohort consisted of patients from a single tertiary medical centre and limited the generalization.
In conclusion, although using sterile injection techniques and infection control practices could contribute to reduce the infections associated with acupuncture, sterile techniques will not prevent all AEs. As a further step toward the modernization of acupuncture, patients and acupuncturists should be aware of the possibility of serious infectious complications, and physicians should provide early appropriate treatment based on commonly identified microorganisms.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions: Conceptualization: Kim WY. Data curation: Lee HJ. Formal analysis: Kim YJ. Methodology: Kim YJ Writing - original draft: Kim YJ, Kim WY. Writing - review & editing: Kim SH, Kim WY.
References
- 1.Park SM, Kim WJ, Mun JH, Kim HS, Ko HC, Kim BS, et al. Adverse events associated with acupuncture: a clinicopathologic review. Int J Dermatol. 2016;55(7):757–763. doi: 10.1111/ijd.12914. [DOI] [PubMed] [Google Scholar]
- 2.Woo PC, Lau SK, Wong SS, Yuen KY. Staphylococcus aureus subcutaneous abscess complicating acupuncture: need for implementation of proper infection control guidelines. New Microbiol. 2003;26(2):169–174. [PubMed] [Google Scholar]
- 3.Clean Needle Technique Manual: Best Practices for Acupuncture Needle Safety and Related Procedures. 7th ed. Baltimore, MD: Council of Colleges of Acupuncture and Oriental Medicine; 2015. [Google Scholar]
- 4.Ernst G, Strzyz H, Hagmeister H. Incidence of adverse effects during acupuncture therapy-a multicentre survey. Complement Ther Med. 2003;11(2):93–97. doi: 10.1016/s0965-2299(03)00004-9. [DOI] [PubMed] [Google Scholar]
- 5.Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9(1):72–83. [PubMed] [Google Scholar]
- 6.Witt CM, Pach D, Brinkhaus B, Wruck K, Tag B, Mank S, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplement Med. 2009;16(2):91–97. doi: 10.1159/000209315. [DOI] [PubMed] [Google Scholar]
- 7.Ernst E. Deaths after acupuncture: a systematic review. Int J Risk Saf Med. 2010;22(3):131–136. [Google Scholar]
- 8.Tang P, Walsh S, Murray C, Alterman C, Varia M, Broukhanski G, et al. Outbreak of acupuncture-associated cutaneous Mycobacterium abscessus infections. J Cutan Med Surg. 2006;10(4):166–169. doi: 10.2310/7750.2006.00041. [DOI] [PubMed] [Google Scholar]
- 9.Lee HJ, Kim YJ, Kim WY. Safety concerns with thoracoabdominal acupuncture: experience at a tertiary-care emergency department. Pain Med. 2017;18(12):2504–2508. doi: 10.1093/pm/pnx068. [DOI] [PubMed] [Google Scholar]
- 10.Kee SJ, Suh SP. Increasing burden of nontuberculous mycobacteria in Korea. J Korean Med Sci. 2017;32(8):1215–1216. doi: 10.3346/jkms.2017.32.8.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu S, Wang L, Cooper E, Zhang M, Manheimer E, Berman B, et al. Adverse events of acupuncture: a systematic review of case reports. Evid Based Complement Alternat Med. 2013;2013:581203. doi: 10.1155/2013/581203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uppsala Monitoring Centre. The use of the WHO-UMC system for standardized case causality assessment. [Accessed September 1, 2016]. http://www.who.int/medicines/areas/quality_safety/safety_efficacy/WHOcausality_assessment.pdf.
- 13.World Health Organization. Guidelines on Basic Training and Safety in Acupuncture. Geneva, Switzerland: World Health Organization; 1999. [Google Scholar]
- 14.Kim MR, Shin JS, Lee J, Lee YJ, Ahn YJ, Park KB, et al. Safety of acupuncture and pharmacopuncture in 80,523 musculoskeletal disorder patients: a retrospective review of internal safety inspection and electronic medical records. Medicine (Baltimore) 2016;95(18):e3635. doi: 10.1097/MD.0000000000003635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture: prospective survey of 32,000 consultations with doctors and physiotherapists. BMJ. 2001;323(7311):485–486. doi: 10.1136/bmj.323.7311.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woo PC, Leung KW, Wong SS, Chong KT, Cheung EY, Yuen KY. Relatively alcohol-resistant mycobacteria are emerging pathogens in patients receiving acupuncture treatment. J Clin Microbiol. 2002;40(4):1219–1224. doi: 10.1128/JCM.40.4.1219-1224.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song JY, Sohn JW, Jeong HW, Cheong HJ, Kim WJ, Kim MJ. An outbreak of post-acupuncture cutaneous infection due to Mycobacterium abscessus. BMC Infect Dis. 2006;6(1):6. doi: 10.1186/1471-2334-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koh SJ, Song T, Kang YA, Choi JW, Chang KJ, Chu CS, et al. An outbreak of skin and soft tissue infection caused by Mycobacterium abscessus following acupuncture. Clin Microbiol Infect. 2010;16(7):895–901. doi: 10.1111/j.1469-0691.2009.03026.x. [DOI] [PubMed] [Google Scholar]
- 19.Ruef C. Complicated skin and soft-tissue infections--consider gram-negative pathogens. Infection. 2008;36(4):295. doi: 10.1007/s15010-008-3408-8. [DOI] [PubMed] [Google Scholar]
- 20.Bang MS, Lim SH. Paraplegia caused by spinal infection after acupuncture. Spinal Cord. 2006;44(4):258–259. doi: 10.1038/sj.sc.3101819. [DOI] [PubMed] [Google Scholar]
- 21.Woo PC, Li JH, Tang W, Yuen K. Acupuncture mycobacteriosis. N Engl J Med. 2001;345(11):842–843. doi: 10.1056/NEJM200109133451119. [DOI] [PubMed] [Google Scholar]