A 60-year-old woman presented for evaluation of recurrent pancreatitis. Her workup, including EUS, revealed only biliary sludge as the cause of recurrent pancreatitis. ERCP with biliary sphincterotomy and sludge extraction was planned. When the endoscope was advanced to the second portion of the duodenum for ERCP, a periampullary diverticulum was seen. The papillary orifice was not visualized for biliary cannulation.
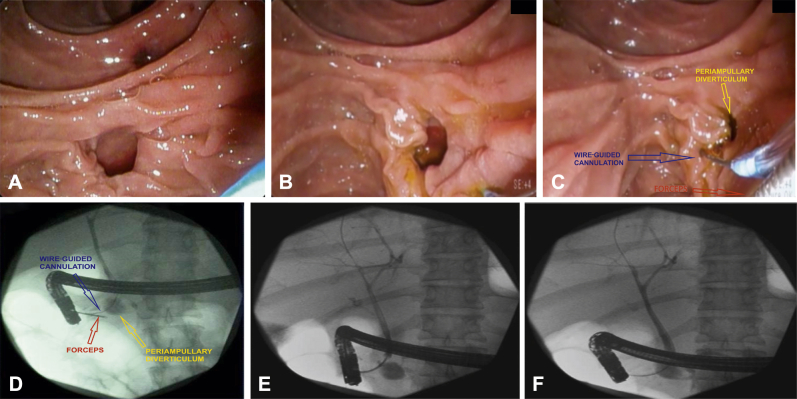
Periampullary diverticulum occurs in up to one third of patients undergoing ERCP. In general, 2 types of periampullary diverticulum have been described. Type 1, peridiverticular papilla, is diagnosed when the papilla is at the rim or within 2 cm of the edge of the diverticulum. Type 2, intradiverticular papilla, is diagnosed when the papilla is deep within the diverticulum or between 2 diverticula. Success rates of 60% to 95% have been reported with the use of a variety of techniques. Some reported techniques include endoscopic clipping of the diverticular rim to expose the papillary orifice; this technique is the most commonly reported. Other techniques include the use of 2 devices in 1 channel method, balloon dilation of the diverticular rim, and saline solution injection to lift the papilla. In this particular case, the anatomy of the diverticulum was suboptimal for placement of endoscopic clipping. Thus, we opted to perform the 2 devices in 1 channel method (Video 1, available online at www.VideoGIE.org). This technique requires a therapeutic duodenoscope, which has a channel size of at least 4.2 millimeters. In addition, other tools include a sphincterotome, generally ranging from 3.9F to 4.4F, and a pediatric biopsy forceps or small grasping forceps, which generally measures less than 2 millimeters in diameter. A sphincterotome was advanced through the channel of the endoscope along with a pediatric biopsy forceps. The biopsy forceps was used to grasp the lip of the periampullary diverticulum and evert it to expose the papillary orifice. The sphincterotome was then repositioned while the position of the biopsy forceps was maintained, and wire-guided cannulation of the bile duct was accomplished. Fluoroscopy imaging shows deep cannulation of the bile duct during simultaneous eversion of the lip of the diverticulum with the biopsy forceps (Fig. 1). This technique is optimal when the papillary orifice is located at the lip of the diverticulum, as in type 1 or periampullary diverticulum. This technique may be more challenging with a type 2 intradiverticular papilla or if the ampulla is very floppy. For difficult biliary cannulation in the setting of a periampullary diverticulum, the simultaneous use of pediatric biopsy forceps and wire-guided cannulation can be a valuable technique for biliary access when conventional methods fail.
Figure 1.
A, Duodenal diverticulum with papilla not visible. B, Duodenal diverticulum with type 1 (periampullary) papilla. C, Endoscopic image showing biliary cannulation during simultaneous grasping of the lip of the diverticulum with biopsy forceps. D, Fluoroscopy image showing biliary cannulation during simultaneous grasping of the lip of the diverticulum with biopsy forceps. E, Fluoroscopy image showing balloon sweep with clearance of duct. F, Occlusion cholangiogram showing no sludge or filling defects.
Disclosure
Dr Sejpal is a consultant for Boston Scientific. All other authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Biliary cannulation in the setting of periampullary diverticulum with the simultaneous use of biopsy forceps and wire-guided cannulation.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Biliary cannulation in the setting of periampullary diverticulum with the simultaneous use of biopsy forceps and wire-guided cannulation.