Abstract
The long-term use of adefovir and tenofovir–antiviral medications commonly used to treat chronic hepatitis B–can be associated with proximal renal tubular dysfunction resulting in significant hypophosphatemic osteomalacia. However, there have been few reports about pathological fractures requiring surgical stabilization in cases of antiviral drug-induced hypophosphatemic osteomalacia. We present the case of a 51-year-old man who sustained bilateral pathological hip fractures associated with antiviral drug-induced hypophosphatemic osteomalacia. To treat a lamivudine-resistant hepatitis-B viral infection, the patient received adefovir for 7 years followed by tenofovir for the subsequent 3 years. He had suffered from polyarthralgia and generalized weakness for 2 years prior to presentation at our clinic. Misdiagnosis and inadequate management of his condition accelerated weakness of the bone matrix and ultimately induced pathological fractures. The patient was managed via cementless total hip arthroplasty on the left hip and internal fixation on the right hip. This case highlights that orthopaedic surgeons should consider the possibility of hypophosphatemic osteomalacia if patients receiving antiviral drugs complain of polyarthralgia and generalized weakness.
Keywords: Antiviral agents, Hypophosphatemic osteomalacia, Pathological fracture
Hypophosphatemic osteomalacia is associated with Fanconi's syndrome, a disease of the proximal renal tubules in which glucose, uric acid, phosphate, and bicarbonate are passed into the urine, instead of being reabsorbed1). Adefovir and tenofovir–antivirals that prevent viral proliferation by inhibiting nucleotide reverse transcriptase–are widely used antiviral drugs in the treatment of chronic hepatitis B virus (HBV) and human immunodeficiency virus (HIV) infections2,3). They are frequently prescribed not only for their efficacy, but also for their decreased side-effect profile compared with other antiviral drugs2,3,4,5,6,7,8). Despite their relatively favorable safety profile, they may induce dose-dependent nephrotoxicity leading to proximal tubular dysfunction and phosphate wasting9). Severe hypophosphatemia due to excessive phosphate wasting can cause inadequate mineralization of the bone matrix and subsequent osteomalacia. Several cases of hypophosphatemic osteomalacia induced by antiviral drugs have been reported2,3,4,5,6,7,8). However, there are few reports of pathological fractures requiring surgical stabilization in cases of antiviral drug-induced hypophosphatemic osteomalacia3,8).
We report an uncommon case of bilateral pathological hip fractures associated with hypophosphatemic osteomalacia induced by the long-term use of antiviral drugs. Adult-onset hypophosphatemic osteomalacia is rarely encountered in orthopedic practice, and adverse effects related to long-term use of antiviral drugs have not been fully recognized by orthopedic surgeons. Furthermore, hypophosphatemic osteomalacia can be overlooked or confused with other musculoskeletal disorders because of the wide variety of associated clinical, laboratory, and radiographic findings10). This case highlights that if patients treated with antiviral drugs complain of bone pain and weakness, a high index of suspicion for underlying hypophosphatemic osteomalacia is crucial to prevent potential serious complications.
CASE REPORT
The patient and his family were informed that this case would be submitted for publication. A 51-year-old male had experienced generalized weakness and arthralgia involving both the knee and ankle joints 2 years prior to presentation in our clinic. He visited several local orthopedic clinics and was prescribed analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and methylprednisolone therapy for arthralgia of unknown etiology. However, the pain gradually increased and he started to experience hip joint pain as well. During the 5 months prior to presentation, he could walk only with the assistance of a cane because of increased joint pain and generalized weakness. On the day of admission, he experienced an abrupt onset of severe pain in the left hip joint while walking with a cane and he presented to our emergency department. He denied any known antecedent trauma. He had a history of chronic HBV infection and liver cirrhosis, and had received lamivudine from 1998 to 2004. However, in 2004, lamivudine was replaced by adefovir (10 mg/day) owing to lamivudine resistance, and the medication was continued until 2011. During that time, the hepatitis had progressed to liver cirrhosis and hepatocellular carcinoma. In 2011, the patient underwent liver lobectomy to remove a solitary mass diagnosed as hepatocellular carcinoma, and adefovir was replaced by tenofovir (300 mg/day). During that period, he had not experienced any pain in the ankle, knee, and hip joints. He had no other medical history and was not previously taking any medication known to result in nephrotoxicity.
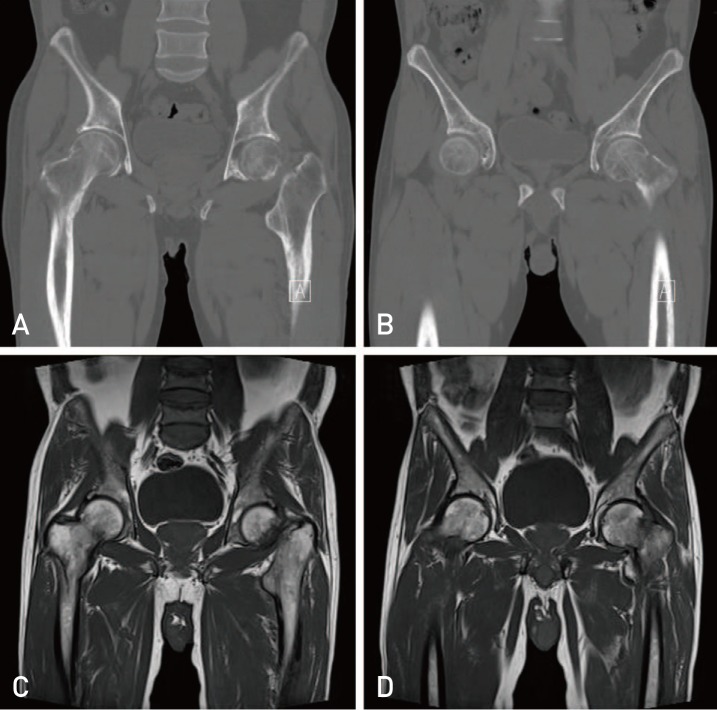
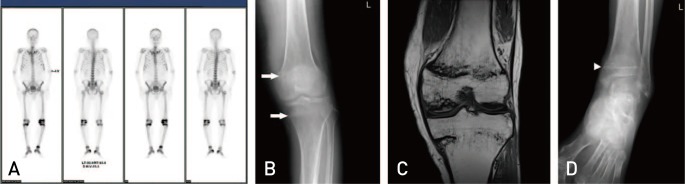
On physical examination, tenderness and increased pain during range of motion of the left hip were observed. Radiographs showed diffuse osteopenia and a fracture line across the femoral neck with a partially displaced femoral head in the left hip11). In addition, a vertical, nondisplaced linear crack across the intertrochanteric area was observed in the right hip (Fig. 1). Further evaluation, including computed tomography and magnetic resonance imaging (MRI) showed a complete fracture with surrounding bone edema in the left hip and a vertical crack extending to the femoral neck as well as a subtrochanteric lesion in the right hip (Fig. 2). Dualenergy X-ray absorptiometry showed decreased lumbar spine bone mineral density of 0.695 g/cm2 (T score, −2.7) and total hip bone mineral density of 0.570 g/cm2 (T score, −2.7).
Fig. 1. Anteroposterior plain radiograph of both hip joints shows a displaced femoral neck fracture on the left side (arrow head) and a vertical crack across the intertrochanteric area (white arrow) on the right side.
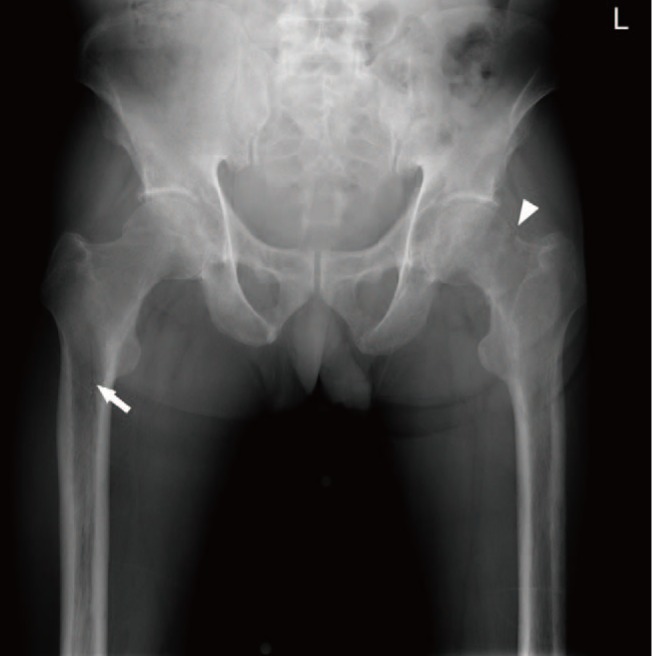
Fig. 2. Coronal views of (A, B) computed tomography and (C, D) T1-weighted magnetic resonance images demonstrate a vertical crack in the right hip joint extending to the femoral neck and the subtrochanteric area.
Laboratory data revealed hypophosphatemia (0.8 mg/dL; normal range, 2.6–4.6 mg/dL), hypouricemia (<2.0 mg/dL; normal range, 2.5–8.0 mg/dL), and an increased level of alkaline phosphatase (ALP, 1,197 IU/L; normal range, 95–280 IU/L). Serum aspartate aminotransferase, alanine aminotransferase, sodium, calcium, potassium, intact parathyroid hormone, and 25-hydroxyvitamin D levels were normal. Urinalysis showed positive albumin and glucose in the absence of hyperglycemia or a history of diabetes mellitus, and 24-hour urinalysis showed increased urinary excretion of phosphate (1,004 mg/day; normal range, 70–220 mg/day) and calcium (471.0 mg/day; normal range, 100–300 mg/day). We considered that impaired phosphate reabsorption could have been caused by proximal renal tubule dysfunction rather than by vitamin D deficiency as the patient's 25-hydroxyvitamin D level was normal.
On the basis of these findings, we made a diagnosis of hypophosphatemic osteomalacia and pathological fractures due to Fanconi's syndrome secondary to antiviral therapy. We performed cementless total hip arthroplasty (Zimmer, Warsaw, IN, USA) on the left hip and internal fixation using the proximal femoral nail antirotation (DePuySynthes, Zuchwil, Switzerland) on the right hip after a 2-week interval (Fig. 3). The patient began ambulation with crutches on postoperative day 7, with progressive weight bearing as tolerated. However, he complained of persistent pain in bilateral knee and ankle joints. Additional radiological evaluation with bone scintigraphy using technetium-99 m-labeled 3,3-diphosphono-1,2-propanodicarboxylicacid (DPD) revealed multiple foci of increased radiotracer uptake in multiple ribs, both knees, and both ankle joints. Plain radiographs and MRI of the affected joints showed incomplete fracture lines involving the distal femur and proximal and distal tibias (Fig. 4). Weight bearing was delayed until the symptoms in multiple joints had resolved. His antiviral drug was replaced by entecavir hydrate (1 mg/day), and phosphorus, calcium carbonate, and alendronate sodium hydrate were administered. Four weeks postoperatively, the clinical symptoms were slightly improved and crutch ambulation was therefore permitted. Three months postoperatively, the patient's symptoms of polyarthralgia and weakness had dramatically improved, and he was able to walk without a cane. At 1 year after surgery, the patient was no longer suffering from joint pain and his hip function recovered to normal. He did not show any new pathological fractures at the last follow-up.
Fig. 3. Postoperative anteroposterior radiograph of both hip joints shows total hip arthroplasty on the left side and internal fixation with an intramedullary device on the right side.

Fig. 4. (A) Whole-body bone scintigraphy demonstrates multiple foci of increased radiotracer uptake in multiple ribs, bilateral distal femurs, bilateral proximal and distal tibias, and right calcaneus. (B) Plain radiograph of both knee joints shows radiopaque transverse lines (white arrows) involving the left proximal femur and distal tibia suggestive of an insufficiency fracture. (C) Coronal T1-weighted magnetic resonance image of the left knee reveals incomplete fracture lines involving both distal femurs and the proximal tibial metaphysis. (D) Plain radiograph of the left ankle joint shows radiopaque transverse lines (arrow head) involving the left distal tibial metaphysis.
DISCUSSION
As the life expectancy of individuals with HBV and HIV infections has increased, long-term adverse effects of antiviral therapies have become more common1). Antiviral agent induced dose-dependent nephrotoxicity can cause renal phosphate wasting by impairing reabsorption in the renal proximal tubule8). Subsequently, chronic loss of phosphate may lead to insufficient bone mineralization. Recently, several cases of hypophosphatemic osteomalacia have been reported in patients treated with antiviral drugs1,2,3,4,5,6,7). Despite recent reports, hypophosphatemic osteomalacia can be easily overlooked or confused with other musculoskeletal disorders because of the lack of a single screening or diagnostic tool and wide variation in clinical manifestations9). Serious complications, such as pathological fractures, may develop if adequate management is delayed. In our case, the patient had complained of polyarthralgia and generalized weakness 2 years before visiting our clinic and visited other outpatient orthopedic clinics several times. However, the orthopedic surgeons whom he visited did not consider the possibility of hypophosphatemic osteomalacia and rather diagnosed the patient as having fibromyalgia, rheumatic disease, and polyarthralgia of unknown etiology, and prescribed analgesics, NSAIDs, and corticosteroids. Despite these drugs, the clinical symptoms became worse and the patient could not walk without a cane. If early diagnosis was made and appropriate management was undertaken (e.g., changing antiviral drugs, adding phosphate supplementation), he may not have suffered from polyarthralgia and generalized weakness for such a long time, and bilateral pathological fractures may have been prevented. Therefore, it is important to consider the possibility of drug-induced hypophosphatemic osteomalacia if patients with a history of long-term antiviral drug use complain of polyarthralgia and generalized weakness.
Antiviral drugs induce dose-dependent nephrotoxicity related to renal tubular dysfunction, causing impaired reabsorption of amino acids, uric acid, bicarbonate, and phosphate and increased excretion of these solutes into the urine8). Chronic loss of phosphate may cause inadequate mineralization of the bone matrix and subsequent osteomalacia1,2,3,4,5,6,7). Considering this pathophysiology, the most definitive laboratory findings for hypophosphatemic osteomalacia are decreased phosphate and increased ALP in hematologic examination and excessive excretion of phosphate in 24-hours urinalysis. Our patient had a history of prolonged use of antiviral drugs for the treatment of HBV and laboratory findings consistent with the above-mentioned criteria. Furthermore, clinical symptoms improved dramatically following discontinuation of antiviral drugs and phosphate supplementation. These findings suggest that antiviral drugs had caused hypophosphatemic osteomalacia in our patient.
The unique feature of our case was that the fracture configuration differed between both hip joints. In the left hip joint, a transcervical femoral neck fracture was noted. Radiologically, osteomalacia presents with generalized osteopenia and multiple, often symmetrical, transverse cortical lucencies that are perpendicular to the long axis of the bone. They are referred to as ‘looser zone’ or ‘pseudofractures’, and they represent cortical stress fractures filled with poorly mineralized callus and fibrous tissue11,12). Pseudofractures of the femoral neck are an unusual complication of osteomalacia. If osteomalacia is diagnosed early and the fractures are not displaced, they often heal with supplementation of deficient ingredients (e.g., calcium, vitamin D, and phosphate)13). However, if they progress to displaced fractures, presumably as a result of torsional, tensile, or shearing stress on the weakened area of the bone, they may require surgical intervention. In our case, it was not certain whether the displaced femoral neck fracture initially originated from the pseudofracture in the medial cortex. However, it was not crucial to our therapeutic decision-making process. Considering the fracture configuration and the age and activity level of the patient, surgical intervention was inevitable. Therefore, we surgically stabilized the left hip using total hip arthroplasty because the exact time of fracture was unknown, bone union could not be expected, and bone quality was poor. In the right hip joint, the vertical crack across the intertrochanteric area was seen on radiographs. If the vertical crack was regarded as a type of pseudofracture, surgical intervention would not have been required and the fracture could have healed with conservative management because it was not displaced. However, the fracture configuration was quite dissimilar to that of a typical pseudofracture in terms of the direction of the fracture line. Pseudofractures commonly develop at right angles to the involved cortex, but in our case, the crack ran vertically across the trochanteric area11,12). Therefore, it was more reasonable to consider that the fracture was not a pseudofracture, but an incomplete fracture that resulted from minor trauma. Patients with osteomalacia are more prone to develop complete fractures compared with the normal population because of the inherent weakness of the bony architecture. Thus, after total hip arthroplasty of the left hip joint, we were concerned about the propagation of the crack to a complete fracture during rehabilitation. With respect to early rehabilitation and prevention of complications, prophylactic fixation of the fracture site was a more viable option than conservative management; thus, we surgically stabilized the fracture using an intramedullary device.
Treatment consensus for antiviral drug-induced hypophosphatemic osteomalacia has not yet been established. Considering the potential risk of breakthrough phenomena after switching to other antiviral agents or exacerbation of liver dysfunction after discontinuation of antiviral drugs, discontinuation or switching of antiviral drugs is not favored in clinical practice. Maintenance or reduction of the dose of antiviral drugs with phosphate supplementation can thus be considered a treatment option4,5) and may partially improve the clinical symptoms. However, without determining the etiology, a phosphate regimen alone cannot serve as the fundamental management solution. Recent reports have demonstrated good clinical outcomes after switching patients to entecavir, which shows a more favorable safety profile and a lower incidence of nephrotoxicity than other antiviral drugs6,14). However, the sample size was too small due to the lack of cases. Therefore, further consensus is needed regarding the management of antiviral drug-induced osteomalacia.
In conclusion, orthopedic surgeons should consider the possibility of hypophosphatemic osteomalacia if patients receiving antiviral drugs complain of polyarthralgia and generalized weakness. Delayed diagnosis of these complications can lead to weakness of the bony architecture resulting from prolonged inhibition of bone matrix mineralization and resultant pathological fractures. Therefore, early diagnosis through regular monitoring of serum ALP and phosphate levels and confirmation of the presence of arthralgia and weakness is crucial to prevent additional serious complications.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Koenig KF, Kalbermatter S, Menter T, Graber P, Kiss D. Recurrent bone fractures due to tenofovir-induced renal phosphate wasting. Scand J Infect Dis. 2014;46:221–224. doi: 10.3109/00365548.2013.840921. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka M, Setoguchi T, Ishidou Y, et al. Pathological femoral fractures due to osteomalacia associated with adefovir dipivoxil treatment for hepatitis B: a case report. Diagn Pathol. 2012;7:108. doi: 10.1186/1746-1596-7-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung YK, Yeon JE, Choi JH, et al. Fanconi's syndrome associated with prolonged adefovir dipivoxil therapy in a hepatitis B virus patient. Gut Liver. 2010;4:389–393. doi: 10.5009/gnl.2010.4.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim du H, Sung DH, Min YK. Hypophosphatemic osteomalacia induced by low-dose adefovir therapy: focus on manifestations in the skeletal system and literature review. J Bone Miner Metab. 2013;31:240–246. doi: 10.1007/s00774-012-0384-y. [DOI] [PubMed] [Google Scholar]
- 5.Terasaka T, Ueta E, Ebara H, et al. Long-term observation of osteomalacia caused by adefovir-induced Fanconi's syndrome. Acta Med Okayama. 2014;68:53–56. doi: 10.18926/AMO/52145. [DOI] [PubMed] [Google Scholar]
- 6.Jeong HJ, Lee JM, Lee TH, et al. Two cases of hypophosphatemic osteomalacia after long-term low dose adefovir therapy in chronic hepatitis B and literature review. J Bone Metab. 2014;21:76–83. doi: 10.11005/jbm.2014.21.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sit YK, Lui TH. Corrective osteotomy in femoral non-union in drug-induced hypophosphataemic osteomalacia. BMJ Case Rep. 2014;2014:bcr2013201269. doi: 10.1136/bcr-2013-201269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tanji N, Tanji K, Kambham N, Markowitz GS, Bell A, D'agati VD. Adefovir nephrotoxicity: possible role of mitochondrial DNA depletion. Hum Pathol. 2001;32:734–740. doi: 10.1053/hupa.2001.25586. [DOI] [PubMed] [Google Scholar]
- 9.Reginato AJ, Coquia JA. Musculoskeletal manifestations of osteomalacia and rickets. Best Pract Res Clin Rheumatol. 2003;17:1063–1080. doi: 10.1016/j.berh.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Garden RS. Stability and union in subcapital fractures of the femur. J Bone Joint Surg Br. 1964;46:630–647. [PubMed] [Google Scholar]
- 11.Le May, Blunt JW., Jr A factor determining the location of pseudofractures in osteomalacia. J Clin Invest. 1949;28:521–525. doi: 10.1172/JCI102099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinbach HL, Kolb FO, Gilfillan R. A mechanism of the production of pseudofractures in osteomalacia (Milkman's syndrome) Radiology. 1954;62:388–395. doi: 10.1148/62.3.388. [DOI] [PubMed] [Google Scholar]
- 13.Lee C, Lashari S. Pseudofracture of the neck of femur secondary to osteomalacia. J Bone Joint Surg Br. 2007;89:956–958. doi: 10.1302/0301-620X.89B7.18425. [DOI] [PubMed] [Google Scholar]
- 14.Palermo A, Strollo R, Papalia R, et al. Severe hypophosphatemic osteomalacia secondary to Fanconi syndrome due to adefovir: a case report. Endocr Pract. 2014;20:e246–e249. doi: 10.4158/EP14251.CR. [DOI] [PubMed] [Google Scholar]