Abstract
The rate of acetabular cup revision arthroplasty is gradually rising along with an increased risk of osteolysis and prosthesis loosening over time and an increase in life expectancy. The goals of revision total hip arthroplasty are: i) implant stability through reconstruction of large bone defects, ii) restoration of range of motion and biomechanics of the hip joint, and iii) normalization of uneven limb lengths. In acetabular cup revision arthroplasty, stable fixation of acetabular components is difficult in the presence of severe bone loss (e.g., evidence suggests that it is challenging to achieve satisfactory results in cases of Paprosky type 3 or higher bone defects using conventional techniques). The author of this study performed acetabular revision to manage patients with large areas of defective bones by filling in with morselized impaction allografts. These allografts were irradiated frozen-stored femoral heads acquired from a tissue bank, and were applied to areas of an acetabular bone defect followed by insertion of a cementless cup. When this procedure was insufficient to obtain primary fixation, a tri-cortical or structural allograft using a femoral head was carried out. Structural stability and bone incorporation were confirmed via long-term follow-up. This study aims to review conventional surgical techniques and verify the utility of surgical procedures by analyzing the author's surgical methods and discussing case reports.
Keywords: Hip arthroplasty, Acetabulum, Allograft, Revision
INTRODUCTION
The rate of acetabular cup revision arthroplasty is gradually rising along with increases in: i) the use of total hip arthroplasty (THA), ii) the risk of osteolysis and prosthesis loosening over time, and iii) life expectancy1). The goals of revision THA are: i) implant stability through reconstruction large bone defects, ii) restoration of the range of motion and biomechanics of the hip joint, and iii) normalization of uneven limb lengths. In acetabular cup revision arthroplasty, stable fixation of acetabular components is difficult when severe bone loss is present. To restore bone loss and achieve initial stability of the acetabular component, multiple surgical techniques have been presented (e.g., high hip center technique, bipolar cup with chip bone graft, structural allograft, morselized bone graft with acetabular reinforcement ring, morselized allograft with cemented acetabular cup fixation, morselized allograft with cementless acetabular cup fixation, revision with trabecular metal augmentation, and cup-in-cage)2,3,4,5,6). Despite the use of these surgical methods, it is not easy to achieve satisfactory results in cases of Paprosky type 3 or higher bone defects. The author of this study intends to address the theoretical background, surgical procedures and outcomes of acetabular revision arthroplasty with morselized impaction allograft and cementless cup.
CLASSIFICATION OF ACETABULAR DEFICIENCIES
The accurate classification of bone stock conditions and acetabular defects is important when deciding an adequate surgical technique for acetabular reconstruction; these assessments are made based on the anteroposterior, lateral and Judet views of simple radiography and computed tomography (CT) scans of the hip. The most commonly used classification systems are the D'Antonio classification7) adopted by the American Association of Orthopaedic Surgeons (AAOS) and the Paprosky classification8) (Table 1, 2). The AAOS system is based on intraoperative assessments of acetabular defects, while the Paprosky system is based on preoperative simple radiographs of the pelvis. The CT scans can improve the accuracy of preoperative classification (Paprosky's classification) done using simple radiography. In addition to the AAOS and Paprosky systems, other classification schemes have been proposed by Saleh et al.9), Gustilo and Pasternak10), Gross et al.11), and Parry et al12). The author of this study mainly used the Paprosky classification to plan surgery procedure using simple radiography and CT scan.
Table 1. The American Association of Orthopaedic Surgeons (AAOS) Classification System for Acetabular Deficiencies.
| Type | Defect |
|---|---|
| Type I | Segmental deficiencies |
| IA Peripheral: superior, anterior, posterior | |
| IB Central (medial wall absent) | |
| Type II | Cavitary deficiencies |
| IIA Peripheral: superior, anterior, posterior | |
| IIB Central (medial wall absent) | |
| Type III | Combined segmental and cavitary deficiencies |
| Type IV | Pelvic discontinuity |
| Type V | Arthrodesis |
Table 2. The Paprosky's Classification System for Acetabular Deficiencies.
| Type | Superior migration* | Ischial lysis† | Med migration‡ | Teardrop lysis§ |
|---|---|---|---|---|
| 1 | Insignificant | None | None | None |
| 2A | Insignificant | Mild | Grade I | Mild |
| 2B | Insignificant to significant | Mild | Grade II | Mild |
| 2C | Insignificant | Mild | Grade III | Moderate to severe |
| 3A | Significant | Moderate | Grade II or III | Moderate to severe |
| 3B | Significant | Severe | Grade III | Moderate to severe |
* Insignificant: <3 cm above superior transverse obturator line, Significant: >3 cm above superior transverse obturator line.
† Mild: 0 to 7 mm below superior transverse obturator line, Moderate: 7 to 14 mm below superior transverse obturator line, Severe: 15-mm lysis.
‡ Grade I: lateral to Kohler's line, Grade II: migration to Kohler's line, Grade II+: medial expansion of Kohler's line into pelvis, Grade III: migration into pelvis with violation of Kohler's line, Grade III+: marked migration into pelvis.
§ Mild: minimal loss of the lateral border, Moderate: complete loss of lateral border, Severe: loss of lateral and medial borders.
BONE GRAFT
There are several different types of bone grafts (e.g., autograft, allograft, and bone substitute). Autografts are known to achieve better clinical outcomes and incorporation compared to allograft with the benefits of facilitated bone formation and no immune response13). Importantly, however, autografts have a number of limitations as well (e.g., insufficient amount of grafts, poor bone quality in elderly patients, and the requirement for additional incisions). When the degree of bone loss is severe, the use of allograft is unavoidable because large bone defects cannot be restored using just an autograft.
The types of allografts used in revision hip arthroplasty are typically divided into structural or morselized allografts. Structural allografts are used for reconstruction of structural or uncontained bone defects, while morselized allografts are usually used to manage non-structural or cavitary bone defects. The benefits of using allograft include: i) excellent applicability and ii) no residual sequelae in the area where bone grafts are harvested (as occur when autografts are used). However, the potential adverse events associated allografts (the absence of osteoblasts and bone inducing factors, the risk of disease transmission, bone graft fractures)14) should be carefully considered prior to their use. In revision surgery, allografts frozen and stored under −80℃ are typically used after collection and radiation sterilization at a dose of 25 kGy. Furthermore, the type of allografts should be chosen depending on the: i) size and area of bone defect, ii) condition of recipient site for bone graft, and iii) type of bone defects (i.e., contained or segmental).
Regarding the histological fate of bone graft materials, whether autografts or allografts, incorporation is important and mediated through a series of processes closely related with the host bone. The host bone supplies blood and living osteoblasts–which are critical factors in incorporation and regeneration of the dead bone graft. Bone grafts stimulate the cellular activity of the host bone, leading to new bone formation within and around graft materials, and serve as a scaffold structure for bone regeneration. Important factors for bone incorporation include: i) firm fixation of bone grafts into the host bone, ii) the surface area between graft and host bone, iii) vascularity of the host bone, iv) weight-bearing condition within grafts, and v) the size and structure of grafts15).
Primary structural bone graft fixation is easy to achieve, however, the graft surface has higher density making ingrowth of blood vessels challenging. Furthermore, stress fractures or bone resorption may occur because bone incorporation occurs with blood vessel ingrowth into the graft surface only while the internal sections of the grafted bone remain mostly dead until later.
Although initial fixation is difficult to achieve with the morselized impaction allografting approach primarily used in this study, complete incorporation can be obtained as morselized allografts have homogeneous surface without gaps compared to the rough surface of the host bone. New bone deposition can be facilitated with dead bone trabeculae without the loss of mechanical intensity through minimized immune response by removing fatty marrow with sufficient cleansing and easy ingrowth of new blood vessels onto the graft16).
METHODS OF ACETABULAR REVISION ARTHROPLASTY IN BONE DEFECTS
1. High Hip Center Technique
This technique is primarily used to manage huge acetabular bone defects in the posterior column, and a cementless acetabular cup is inserted into the upper part of the acetabulum with severe bone loss. The placement of the acetabular component was defined as the presence of hip center above a teardrop line connecting the superior aspect of the acetabulum greater than 35 mm17). When using this technique, the primary stability of the acetabular component and greater than 70% host bone contact with the cup should be obtained. The superior migration of the hip center causes no definitive problems with hip biomechanics, but the superolateral migration of the hip center needs to be avoided due to its adverse effects on hip biomechanics18). Since the superior migration of hip center may result in leg length shortening and abductor weakness leading to dislocation of the hip joint, the use of a long neck-head, a calcar replacement stem and a high offset stem is recommended. Excessive reaming into the posterior column should be avoided and all possible causes of impingement should be eliminated19,20). This surgical technique is limitedly recommended and should be avoided if possible.
2. Bipolar Cup with Chip Bone Graft
This surgical technique is used in progressive acetabular reconstruction in the presence of huge defects in acetabular bone stock. In this procedure, acetabular reconstruction is not completed via a single operation; instead, a bipolar cup is fixed at secondary surgery after restoration of bone stock and the incorporation of the bone graft into the host bone.
The surgical method can be used in AAOS type I, II, and III and Paprosky type 1, 2, and 3 bone defects, but is not desirable in AAOS type IV bone defects. A porous-coated cementless cup is typically used after chip bone grafting when the cup surface is in contact with more than 50% of the host acetabular bone and solid fixation of the acetabular cup can be attained with screws and alternatively, the use of a bipolar cup can be considered when firm fixation of the acetabular cup cannot be attained21,22,23). The primary concern with this surgical method is ensuring stable placement of the bipolar cup into the relatively healthy host bone through over-reaming of the acetabular rim. When bone loss is severe in the superomedial acetabular wall, it is important to prevent the postoperative medial displacement of the bipolar cup by using sufficient amounts of allograft.
A study of McFarland et al.24) showed that although clinical improvement was shown in 83% of cases, radiological outcomes at an average of 1.3 years of follow up revealed osteolysis around the acetabular component in most cases. Takatori et al.25) also note that the use of a bipolar cup should be limited since medial displacement of the cup of greater than 10 mm occurred in 40% of cases during an average follow-up of 7 years. This surgical technique has been rarely used in the clinical settings.
3. Structural Allograft
Structural allografts are often used in patients with AAOS type III and IV defects in the acetabular bone. This procedure fixes the structural bone at the site of acetabular bone defect and then the defect can be filled with autografts between the graft and host bones. Cemented and cementless cups and acetabular reinforcement ring are also used. Total acetabulum, distal femur, proximal tibia and femoral head allografts are commonly used as structural allograft materials. Usually, failure rates are high when structural grafts support more than 50% of the acetabular component26). Relatively good short-term results have been attained, but mid- and long-term failure rates range between 4% and 47%27). The major cause of failure is bone resorption during reformation of the grafted bone which leads to structural instability. When performing this procedure, the high long-term failure rates when structural grafts are attempting to support large areas of the acetabular component should be considered.
4. Morselized Allograft with Acetabular Reinforcement Ring
This surgical technique is commonly used for elderly patients with Paprosky type 2 and 3 structural defects in which greater than 50% host bone contact with the cup cannot be attained. The defects are filled with impacted moralized allografts and fixed with the acetabular reinforcement ring using screws, and a polyethylene liner 2 to 3 mm smaller than the acetabular reinforcement ring is fixed with cement. There are two types of Müller acetabular reinforcement rings: i) one that is fixed to the ilium alone with screws and ii) other reinforced types (e.g., Ganz and Octopus rings that are fixed to the ilium using screws and thus providing stability by a hook attached to cotyloid notch in the inferior aspect). Another ring type is Burch-Schneider antiprotrusio cage that is fixed to both the ilium and ischium28). The rate of short-term acetabular cup loosening is about 24%29), and the revision rates at mid- and long-term follow up are 20% and 44%, respectively30). Despite the use of a solid metal ring, Berry and Müller29) addressed problems encountered between the more flexible pelvic bone and a hard implant and stress shielding of the graft bone. The posterior column is fixed with a pelvic reconstruction plate in cases with pelvic incontinuity and the acetabular reinforcement ring is used for fixation. This technique is a commonly used surgical option, but should be carefully applied with accuracy. For this reason, the author of this study rarely uses this method.
5. Morselized Allograft with Cemented Acetabular Cup Fixation
In 1984, Slooff et al.31) used a modified morselized impaction allografting technique. In summary, the contained acetabular defect is impacted with an allograft (average size of 1 cm) and the segmental defect is covered with a metal mesh or a thin cancellous bone layer. Subsequently, cement is used directly onto the bone bed for fixation without using the acetabular reinforcement ring to allograft bone fragments. The key principles of this technique are: i) reconstruction of hip biomechanics by placing the cup on the anatomic teardrop, ii) impaction of the segmental defect with a metal wire mesh to achieve containment, iii) impaction of the cavitary defect with a morselized allograft to replace bone loss around implants, and iv) impaction of bone chips using bone cement to increase stability. The benefits of this surgical technique include: i) minimized polyethylene wear, ii) restoration of bone stock with satisfactory graft incorporation, and iii) stable interdigitation of cement with morselized grafts32).
This surgical method can be used in AAOS type I, II, and III and Paprosky type 1, 2, and 3 bone defects, but is not desirable in AAOS type IV defects. When performing this technique, the following cautions should be carefully considered: i) massive segmental defects should be converted to cavitary defects using metal meshes, ii) small-sized chip bone grafts are impacted into the site of the cavitary defect, and iii) the polyethylene acetabular cup is cemented onto the graft.
A wide variety of radiological and clinical outcomes relating to this technique have been reported. Previous studies that introduced this surgical technique have reported favorable results. Studies on aseptic loosening of the acetabular component by Trumm et al.33), Highcock et al.34), and Sloof et al.35) demonstrated a low re-revision rate of 4% to 6%. Buttaro et al.36) documented a success rate of 90% in 23 hips at 3-year follow-up. Comba et al.37) obtained favorable results in 96% of 142 hips at 4-year follow-up. Schreurs et al.38) note that cemented acetabular cup fixation is considered a good surgical option because of a survival rate of 85% at an average follow-up of 12 years. On the contrary, Jasty and Harris39) reported a failure rate of 75% at 6-year follow-up, and Pellicci et al.40) and Kavanagh et al.41) also obtained unsatisfactory results with a re-revision rate of 22%, complication rate for sepsis at 2.5%, recurrent dislocation at 4%, aseptic loosening at 16% and others. Nevertheless, this technique is considered fairly safe.
6. Cementless Cup with Bone Graft
This is a widely used surgical technique that restores the anatomic hip center and facilitates incorporation of the bone graft. To use a cementless cup, ensuring as much contact as possible with healthy host bone is critical. Although the extent of viable host bone contact with a cementless cup remains controversial, it is generally considered that the cup surface should make contact with at least 50% of healthy host bone in cavitary defects. In addition, it is desirable to fix the cup by inserting extra-long screws from different directions. Greater than 70% host bone contact with a cementless cup is commonly recommended in segmental defects42,43).
This surgical method can be used in AAOS type I, II, and III and Paprosky type 1, 2, and 3 bone defects, but is not allowed in AAOS type IV defects and patients with Paget's disease, metabolic bone disease (e.g., acetabular necrosis and bone tumor)42). The success of this surgery is considerably affected by the preservation of the posterior column. Moreover, solid impaction of morselized bone chips is important and initial stability needs to be attained by placement of the cup with the acetabular rim and acetabular floor on the remaining host bone.
Multiple mid- and long-term studies report relatively good clinical results in fixation with a cementless vs. cement cup. Silverton et al.44) documented a radiological failure rate of 7% in a study with a median follow-up period of 8.3 years. In a study by Sun et al.45), radiological findings revealed osteolysis in 24.6% of patients at an average follow-up of 8.2 years, but the survival rate of implants was 92.1%. Leopold et al.46) noted a survival rate of 98% and a noninfectious acetabular loosening rate of 1.8% at a median follow-up of 10.5 years. Rosenberg47) reported a survival rate of 84% and no revisions due to loosening at an average follow-up of 11 years after revision in 138 hips. The author of this study prefers the surgical method using morselized impaction allograft and a cementless cup and intends to more clearly delineate this procedure in the future.
7. Revision with Trabecular Metal Augmentation
Trabecular metal augmentation has been introduced to improve biological fixation rather than mechanical fixation and is used in revision when there is clearly a smaller contact surface between the implant and host bone due to osteolysis. This technique facilitates bone ingrowth by using tantalum to fill the bone defect and trabecular metal material can be an alternative to structural allograft. Since tantalum has properties of high volumetric porosity and low modulus of elasticity and exhibits high coefficient of friction, this metal can ensure primary implant stability48). Furthermore, this technique is a simple and quick procedure, and can achieve biological fixation with bone ingrowth without the risk of bone resorption after grafting.
This surgical method can be used in Paprosky type 3 defects, type 3A with severe bone loss in the superior aspect of the acetabulum and less than 50% host bone contact and type 3B associated with 3A defects or pelvic discontinuity.
Siegmeth et al.49) performed acetabular revisions using trabecular metal augments and trabecular metal cups in 34 cases, and stable fixation was achieved in 32 requiring no additional surgery; re-revision was required in only two cases with more than 2 years of follow-up. Other authors obtained comparable results and suggest that this technique is a surgical option for bone ingrowth around the cup when contact surface between the cup and host bone is small and firm screw fixation is impossible50,51). Boscainos et al.52) report more than 32-month follow-up results of 14 patients who underwent revision using the trabecular metal cup-cage construct, and all patients gained stable implant fixation; only two patients underwent re-revision due to dislocation.
However, since the clinical outcomes of trabecular metal augments are insufficient due to short-term follow-up, further long-term investigations are warranted to improve long-term clinical results (e.g., stability, wear debris between the cup and metal augments, fatigue failure, the amount of the host bone required in revision, and difficult recovery).
8. Cup-cage Reconstruction
A cage-in-cup technique is a recent surgical option for acetabular fixation using the cup-cage construct. In this method, a second-generation porous-coated cup is used for pelvic fixation. When implant stability is weak, an acetabular cage can be placed into the superior portion of the cup and fixed to the ilium and ischium by screws. Acetabular revision arthroplasty using a cup-cage construct is a useful technique when managing Paprosky type 3A and 3B defects and pelvic discontinuity. In a case report by Bellester Alfaro and Sueiro Fernádez53), no failures were observed among 5 patients who underwent revision using cup-cage constructs and trabecular metal augments (an average follow-up of 26 months). Further studies are warranted to investigate this rarely used technique and only explored with short-term follow-up in Korea.
9. Author's Surgical Technique
The author of this study prefers a transgluteal approach, but concomitantly uses trans-trochanteric osteotomy, if necessary. After exposure of the surgical site, a loose acetabular component, osteolytic soft tissues and all bone cements are completely removed. After observation of the defect area, reaming is continued using progressively larger-diameter reamers. Reaming is carefully carried out to ensure maximum stability without damaging structures within the periacetabular region. Sufficient medialization of the acetabular component is obtained by conserving as much contact with the original bone bed as possible. In particular, the contact area between the cup and host bone should be maximized by progressively increasing reamer diameters as tolerable to optimize contact pressure in the anterior, inferior and posterior areas. Allografts used in implantation are harvested from the femoral head, frozen and stored under −80℃ for more than 6 months in a tissue bank after being collected from a patient with femoral neck fracture. Bacterial cultures are done before allografts are frozen and stored, and screening tests are performed on each donor. Cartilage and cortical bone are removed from the allograft, and separated cancellous bone is cut into about 1 cm using bone scissors. To minimize immune response, allografts are repeatedly washed with saline solution using pulsatile lavage to eliminate as much fat and blood as possible and then dried with a skin towel. Dried morselized impaction allografts are mixed with the patient's blood. Morselized bone grafts are impacted into the defect using impactors with reverse reaming (Fig. 1). Proper reaming allows satisfactory results using morselized impaction allograft despite major bone loss affecting more than 60% of the acetabulum. A hemispherical jumbo cup larger than a reamer by 2 mm is press-fit and firmly fixed to the superior portion using 4 to 7 cancellous screws to ensure bony ingrowth (Fig. 2). When severe bone loss is managed with morselized impaction allograft alone, a jumbo cup with a diameter of 66 to 74 mm is commonly used.
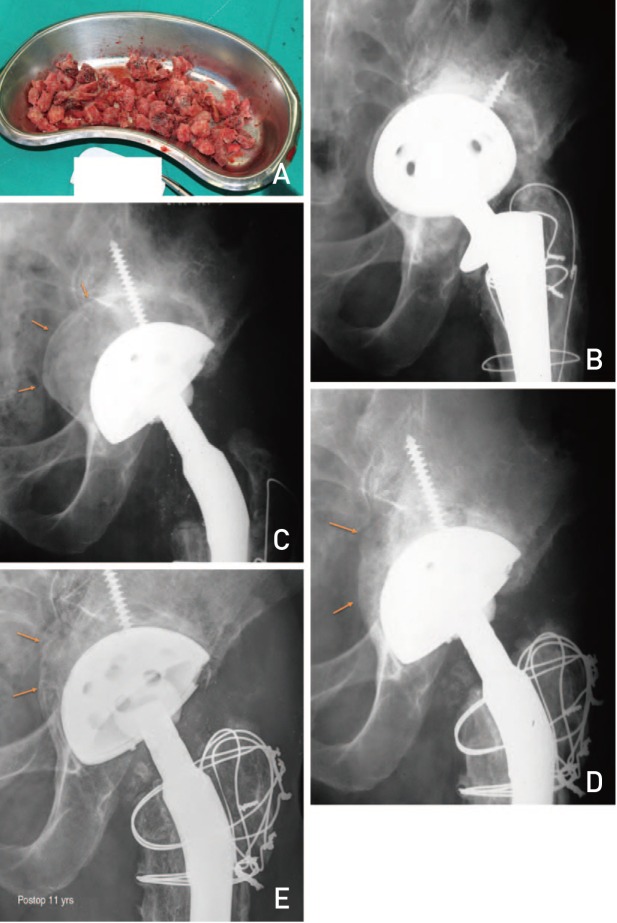
Fig. 1. (A) Morselized allografts are made by removing roughly 1 cm from the head of a femur with bone scissors following by cleansing (using pulsatile lavage) and drying. Dried morselized impaction allografts are next mixed with a patient's blood. (B) Preoperative anteroposterior view of a 58-year-old male patient with a bony defect (Paprosky type 2C) and aseptic loosening after total hip arthroplasty (THA). (C) Immediate postoperative anteroposterior view showing revision THA with a morselized impacted allograft. (D) Two years after operation, we performed greater trochanter reattachment and checked bone remodeling through medial bone absorption. (E) Eleven years after operation, acetabular components were well fixed and bony remodeling of the allograft was observed through changes in sclerotic lesions.
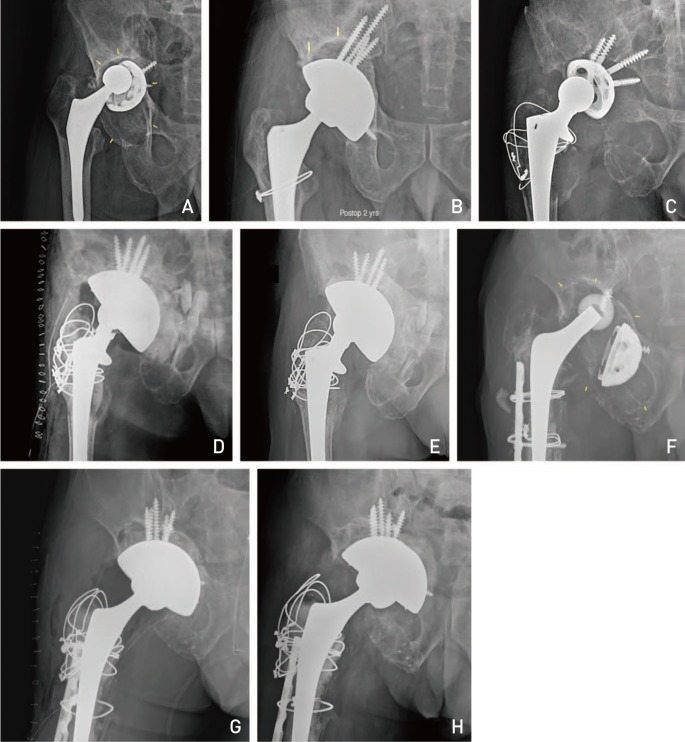
Fig. 2. (A) Preoperative anteroposterior view of a 63-year-old male patient with a bony defect and aseptic loosening requiring total hip arthroplasty (THA). (B) Revision THA with morselized impaction allograft was performed. Implants were well fixed after 2 years postoperatively. (C) Preoperative anteroposterior view of a 60-year-old male patient with bony defect and aseptic loosening requiring THA. (D) Immediate postoperative anteroposterior view showing revision THA with a morselized impacted allograft. (E) Implants were fixed after 3 years postoperatively. (F) Preoperative anteroposterior view of a 60-year-old male patient with a bony defect and aseptic loosening requiring THA. (G) Immediate postoperative anteroposterior view showing revision THA with a morselized impacted allograft. (H) Radiograph taken 2 years after revision showing bone resorption remodeling and allograft incorporation.
The author prefers allograft in mild bone defects unless a bone graft is required. Adequate fixation can be achieved in some cases when morselized impaction allograft is applied to a Paprosky type 3B defect with more than 60% of bone loss. However, when sufficient fixation cannot be attained due to severe segmental defect in the medial wall and bone stock first, one of the two techniques used for early fixation is used. The first tricortical bone graft which is harvested from the iliac tuberosity the most abundant source of cancellous bone via an incision of 5 to 7 cm, and then fixed to the superior acetabular margin using 2 to 3 screws. This technique is similar to slotted acetabular augmentation described by Staheli54). In addition, the remaining bone defect is packed with morselized allograft and cancellous autograft reaming is applied to help impact the graft (Fig. 3). Secondly, initial fixation may be obtained via adequate reaming with structural allograft from the femoral head, and the remaining defect is well designed with femoral head allograft. Femoral head structural graft is fixed with 2 to 3 cancellous screws. A minimum compressive load to the graft bone needs to be generated, and as much of the load as possible should be in contact with the remaining acetabular rim. Congruency of the acetabulum is ensured by packing morselized allograft around the structural allograft (Fig. 4). Despite more than 60% of bone loss between the boundary of Paprosky type 3A and 3B defects, the author's revision technique can be performed if pelvic discontinuity is not severe, the posterior column and acetabular dome remain after maximum reaming, or a jumbo cup can be placed on the acetabular margin, despite a discontinuity of the acetabular rim (Fig. 2). Reaming the exact amount of the diameter of the acetabular component should be ensured to obtain satisfactory fixation.
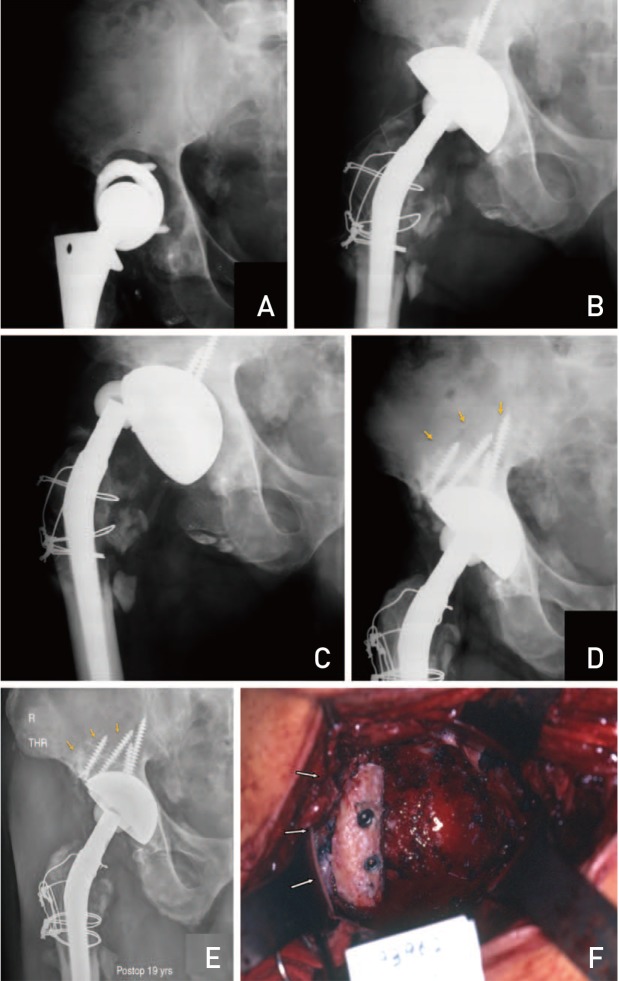
Fig. 3. (A) Preoperative anteroposterior view of a 58-year-old male patient with aseptic loosening requiring total hip arthroplasty (THA). (B) Immediate postoperative anteroposterior view showing revision THA with a morselized impacted allograft. (C) Following a traffic accident 6 weeks after surgery, fixation was lost. (D, F) Re-revision THA with morselized impaction allograft and tricortical iliac autograft was performed. Autograft was fixed with 2 screws. (E) Implants remained well fixed 19 years postoperatively. Bony union and remodeling were observed.
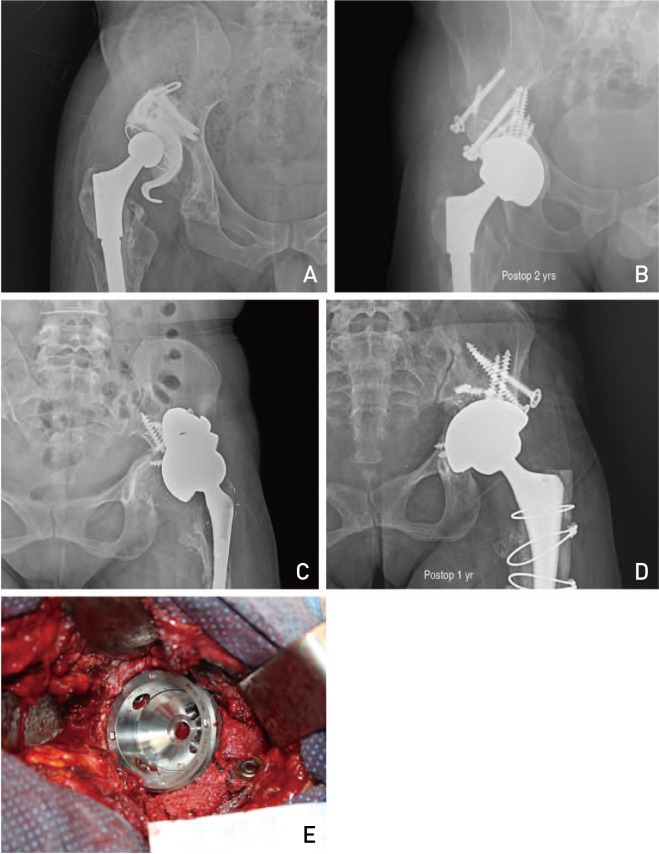
Fig. 4. (A) Preoperative anteroposterior view of a 40-year-old male patient with a severe bony defect and requiring aseptic total hip arthroplasty (THA). Immediate postoperative anteroposterior view showing revision THA with a morselized impaction allograft and 2 femoral head structural allografts was performed. (B) Radiograph taken 2 years after revision showing bone resorption remodeling and allograft incorporation. (C) Preoperative anteroposterior view of a 40-year-old female patient with a severe bony defect and requiring aseptic THA. (D) Implants were well fixed after 1 year postoperatively. (E) Immediate postoperative anteroposterior view showing revision THA with morselized impaction allograft and femoral head structural allograft.
Passive hip joint and knee joint exercises are allowed from the second to third postoperative day, and partial weight bearing ambulation is normally begun from 3–4 days to 6 weeks after surgery depending on rigidity of fixation. Partial weight bearing gait with heavier weight load is recommended at the sixth postoperative week and full weight bearing gait is allowed three months after surgery. However, non-weight bearing ambulation can be performed in cases with excessive allograft implantation by considering patient's age and systemic status.
With respect to ossification when using a cementless acetabular cup and morselized impaction allograft, first, bony ingrowth in the contact surface with autograft encourages fixation with autograft. Second, host bone-derived new blood vessels and osteoblasts flow into a dead space in the contact area with morselized impaction allograft, and progressive ossification enables fixation with allograft as a scaffold structure. Sloof et al.31) proved bony ingrowth from a cementless acetabular cup in contact with allograft based on the results of laboratory animal tests. Although elucidated in a study of Lee et al.15,55,56,57), bone ingrowth appears to occur indirectly without a radiolucent line as shown in the author's long-term follow-up.
The advantages of the author's technique are the ability to achieve greater early fixation and incorporation using press-fit technique and morselized impaction bone compared to previous techniques. Avoiding direct weight load to the structural allograft minimizes the risk of collapse and this facilitates bony ingrowth, leading to restoration of the segmental defect.
The procedure, as stated by Lee et al.15), has been used since the early 1990s. Instead of fixation loss, bony union and graft bone changes in hip joints at a minimum follow-up period of 10 years (range, 10–20 years 2 months) after morselized impacted allograft into acetabular bone defect were reported in 2012. This previous study reviewed 98 hips (93 patients) followed up for at least 10 years (range, 10–20 years 2 months) to examine: i) new bone formation, ii) changes in the radiolucent zone between allograft and cup size, iii) changes in the allograft margin, and iv) formation of trabecular bone by comparing enlarged anteroposterior and lateral views on radiographs taken immediately after surgery and at final follow-up. Since determining incorporation between the host bone and graft bone is challenging, incorporation is defined as the finding of newly formed trabecular bone and radiographic disappearance of borders between the host bone and graft bone on follow-up anteroposterior views.
According to the radiographic results at final follow-up, a radiolucent zone between the host bone and graft bone was observed in 3 cases and periacetabular component in 12 cases, but the width of all radiolucent zones was less than 2 mm. When comparing radiographs taken on regular follow-ups, radiolucency of the graft bone was increased in 38 cases and decreased in 58 cases on follow-up radiographs taken between 3rd and 6th postoperative months. Newly formed trabecular bone and incorporation between the host bone and graft bone were confirmed in all cases, excluding 15 hips. There were no complications associated with injury to the nerves including the sciatic nerve, and no revision surgery due to deep infection. Although postoperative dislocation occurred in 1 hip, this was managed with an abduction brace after closed reduction. Reformation of the graft bone seems to be affected by patterns in stress change. Therefore, the author's technique with structural autograft and a cementless cup is suggested as a good surgical option for acetabular revision arthroplasty assuming accurate surgical procedures are applied.
In 2004, Lee et al.15) reported outcomes of morselized allograft in revision for management of acetabular bone defect and reviewed 77 cases (81 hips) with acetabular revision using morselized allograft bone by reviewing the anteroposterior and lateral views on radiographs taken at final follow-up (range, 6–12 years and 10 months). Fixation was well maintained in 30 out of 31 cases. Compared to immediately after surgery, radiodensity increased in 32 cases and decreased in 48 cases. A radiolucent zone between the host bone and graft bone was observed in 2 cases and around the acetabular component in 9 cases; all radiolucent zones had a width of less than 2 mm. Moreover, reformation of the medial graft bone was observed with acetabular bone resorption.
In a study published in 2011, Lee et al.56) reported radiographic and clinical results in 62 of 71 hips that underwent surgery using morselized impaction allograft and a cementless cup based on radiographic images and Harris hip scores at a minimum of 10 years (range, 10–14 years and 8 months) from 1992 to 2000. The mean Harris hip score was 92 at final follow-up and re-revision was done in 3 cases. There were no injuries to the blood vessels and nerves including sciatic nerve palsy, and two patients with recurrent dislocation within the first postoperative week were managed with an abduction brace. The 12-year survival rate was 95.8%. These outcomes demonstrate that satisfactory long-term results can be obtained using the author's surgical technique.
CONCLUSION
For reconstruction of severe acetabular bone loss, restoration of acetabular bone defect using morselized impaction allograft and a cementless jumbo cup is a useful surgical option to achieve stable short-term fixation and satisfactory long-term surgical outcomes.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 2.Issack PS, Nousiainen M, Beksac B, Helfet DL, Sculco TP, Buly RL. Acetabular component revision in total hip arthroplasty. Part I: cementless shells. Am J Orthop (Belle Mead NJ) 2009;38:509–514. [PubMed] [Google Scholar]
- 3.Issack PS, Nousiainen M, Beksac B, Helfet DL, Sculco TP, Buly RL. Acetabular component revision in total hip arthroplasty. Part II: management of major bone loss and pelvic discontinuity. Am J Orthop (Belle Mead NJ) 2009;38:550–556. [PubMed] [Google Scholar]
- 4.Pulido L, Rachala SR, Cabanela ME. Cementless acetabular revision: past, present, and future. Revision total hip arthroplasty: the acetabular side using cementless implants. Int Orthop. 2011;35:289–298. doi: 10.1007/s00264-010-1198-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blumenfeld TJ. Implant choices, technique, and results in revision acetabular surgery: a review. Hip Int. 2012;22:235–247. doi: 10.5301/HIP.2012.9281. [DOI] [PubMed] [Google Scholar]
- 6.Jiranek WA. Acetabular liner fixation by cement. Clin Orthop Relat Res. 2003;(417):217–223. doi: 10.1097/01.blo.0000096805.78689.8b. [DOI] [PubMed] [Google Scholar]
- 7.D'Antonio JA, Capello WN, Borden LS, et al. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;(243):126–137. [PubMed] [Google Scholar]
- 8.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 9.Saleh KJ, Holtzman J, Gafni A, et al. Development, test reliability and validation of a classification for revision hip arthroplasty. J Orthop Res. 2001;19:50–56. doi: 10.1016/S0736-0266(00)00021-8. [DOI] [PubMed] [Google Scholar]
- 10.Gustilo RB, Pasternak HS. Revision total hip arthroplasty with titanium ingrowth prosthesis and bone grafting for failed cemented femoral component loosening. Clin Orthop Relat Res. 1988;(235):111–119. [PubMed] [Google Scholar]
- 11.Gross AE, Allan DG, Catre M, Garbuz DS, Stockley I. Bone grafts in hip replacement surgery. The pelvic side. Orthop Clin North Am. 1993;24:679–695. [PubMed] [Google Scholar]
- 12.Parry MC, Whitehouse MR, Mehendale SA, et al. A comparison of the validity and reliability of established bone stock loss classification systems and the proposal of a novel classification system. Hip Int. 2010;20:50–55. doi: 10.1177/112070001002000108. [DOI] [PubMed] [Google Scholar]
- 13.Aaron AD, Wiedel JD. Allograft use in orthopedic surgery. Orthopedics. 1994;17:41–48. doi: 10.3928/0147-7447-19940101-08. [DOI] [PubMed] [Google Scholar]
- 14.Strong DM, Friedlaender GE, Tomford WW, et al. Immunologic responses in human recipients of osseous and osteochondral allografts. Clin Orthop Relat Res. 1996;(326):107–114. doi: 10.1097/00003086-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Lee JM, Roh JY, Lee JH, Wang WJ, Kim HM. Fate of morselized impaction allograft used for the defect of acetabulum in revision total hip arthroplasty. J Korean Musculoskelet Transplant Soc. 2004;4:104–111. [Google Scholar]
- 16.Goldberg VM, Stevenson S, Schaffer JW. Bone and cartilage allografts. In: Friedlaender GE, Goldberg VM, editors. American Academy of Orthopaedic Surgeons Symposium. vol. 1. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1991. pp. 3–12. [Google Scholar]
- 17.Dearborn JT, Harris WH. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty. Results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Doehring TC, Rubash HE, Shelley FJ, Schwendeman LJ, Donaldson TK, Navalgund YA. Effect of superior and superolateral relocations of the hip center on hip joint forces. An experimental and analytical analysis. J Arthroplasty. 1996;11:693–703. doi: 10.1016/s0883-5403(96)80008-8. [DOI] [PubMed] [Google Scholar]
- 19.Murayama T, Ohnishi H, Okabe S, et al. 15-year comparison of cementless total hip arthroplasty with anatomical or high cup placement for Crowe I to III hip dysplasia. Orthopedics. 2012;35:e313–e318. doi: 10.3928/01477447-20120222-28. [DOI] [PubMed] [Google Scholar]
- 20.Hendricks KJ, Harris WH. High placement of noncemented acetabular components in revision total hip arthroplasty. A concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am. 2006;88:2231–2236. doi: 10.2106/JBJS.E.00247. [DOI] [PubMed] [Google Scholar]
- 21.Namba R, Scott RD. Acetabular revision with the bipolar prosthesis and particulate bone grafting. Semin Arthroplasty. 1993;4:87–91. [PubMed] [Google Scholar]
- 22.Oakeshott RD, Morgan DA, Zukor DJ, Rudan JF, Brooks PJ, Gross AE. Revision total hip arthroplasty with osseous allograft reconstruction. A clinical and roentgenographic analysis. Clin Orthop Relat Res. 1987;(225):37–61. [PubMed] [Google Scholar]
- 23.Papagelopoulos PJ, Lewallen DG, Cabanela ME, McFarland EG, Wallrichs SL. Acetabular reconstruction using bipolar endoprosthesis and bone grafting in patients with severe bone deficiency. Clin Orthop Relat Res. 1995;(314):170–184. [PubMed] [Google Scholar]
- 24.McFarland EG, Lewallen DG, Cabanela ME. Use of bipolar endoprosthesis and bone grafting for acetabular reconstruction. Clin Orthop Relat Res. 1991;(268):128–139. [PubMed] [Google Scholar]
- 25.Takatori Y, Ninomiya S, Umeyama T, Yamamoto M, Moro T, Nakamura K. Bipolar revision arthroplasty for failed threaded acetabular components: radiographic evaluation of cup migration. J Orthop Sci. 2002;7:467–471. doi: 10.1007/s007760200081. [DOI] [PubMed] [Google Scholar]
- 26.Leopold SS, Jacobs JJ, Rosenberg AG. Cancellous allograft in revision total hip arthroplasty. A clinical review. Clin Orthop Relat Res. 2000;(371):86–97. doi: 10.1097/00003086-200002000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Paprosky WG, Magnus RE. Principles of bone grafting in revision total hip arthroplasty. Acetabular technique. Clin Orthop Relat Res. 1994;(298):147–155. [PubMed] [Google Scholar]
- 28.Yoo MC. [Revision total hip arthroplasty using acetabular reinforcement ring] J Korean Hip Soc. 2004;16:183–190. Korean. [Google Scholar]
- 29.Berry DJ, Müller ME. Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg Br. 1992;74:711–715. doi: 10.1302/0301-620X.74B5.1527119. [DOI] [PubMed] [Google Scholar]
- 30.Zehntner MK, Ganz R. Midterm results (5.5–10 years) of acetabular allograft reconstruction with the acetabular reinforcement ring during total hip revision. J Arthroplasty. 1994;9:469–479. doi: 10.1016/0883-5403(94)90092-2. [DOI] [PubMed] [Google Scholar]
- 31.Slooff TJ, Huiskes R, van Horn J, Lemmens AJ. Bone grafting in total hip replacement for acetabular protrusion. Acta Orthop Scand. 1984;55:593–596. doi: 10.3109/17453678408992402. [DOI] [PubMed] [Google Scholar]
- 32.Hwang KT, Kim YH. Revision total hip arthroplasty of an acetabular cup with acetabular bone defects. J Korean Hip Soc. 2011;23:237–247. [Google Scholar]
- 33.Trumm BN, Callaghan JJ, George CA, Liu SS, Goetz DD, Johnston RC. Minimum 20-year follow-up results of revision total hip arthroplasty with improved cementing technique. J Arthroplasty. 2014;29:236–241. doi: 10.1016/j.arth.2013.04.040. [DOI] [PubMed] [Google Scholar]
- 34.Highcock A, Siney P, Wroblewski BM, Wynne Jones H, Raut VV. Severe femoral osteolysis treated with a cemented Charnley revision arthroplasty. Clinical and radiological follow-up to 27 years. Orth Proc. 2015;97-B:51. [Google Scholar]
- 35.Slooff TJ, Buma P, Schreurs BW, Schimmel JW, Huiskes R, Gardeniers J. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop Relat Res. 1996;(324):108–115. doi: 10.1097/00003086-199603000-00013. [DOI] [PubMed] [Google Scholar]
- 36.Buttaro MA, Comba F, Pusso R, Piccaluga F. Acetabular revision with metal mesh, impaction bone grafting, and a cemented cup. Clin Orthop Relat Res. 2008;466:2482–2490. doi: 10.1007/s11999-008-0442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Comba F, Buttaro M, Pusso R, Piccaluga F. Acetabular revision surgery with impacted bone allografts and cemented cups in patients younger than 55 years. Int Orthop. 2009;33:611–616. doi: 10.1007/s00264-007-0503-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schreurs BW, Luttjeboer J, Thien TM, et al. Acetabular revision with impacted morselized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis. A concise follow-up, at eight to nineteen years, of a previous report. J Bone Joint Surg Am. 2009;91:646–651. doi: 10.2106/JBJS.G.01701. [DOI] [PubMed] [Google Scholar]
- 39.Jasty M, Harris WH. Total hip reconstruction using frozen femoral head allografts in patients with acetabular bone loss. Orthop Clin North Am. 1987;18:291–299. [PubMed] [Google Scholar]
- 40.Pellicci PM, Wilson PD, Jr, Sledge CB, et al. Long-term results of revision total hip replacement. A follow-up report. J Bone Joint Surg Am. 1985;67:513–516. [PubMed] [Google Scholar]
- 41.Kavanagh BF, Ilstrup DM, Fitzgerald RH., Jr Revision total hip arthroplasty. J Bone Joint Surg Am. 1985;67:517–526. [PubMed] [Google Scholar]
- 42.Bal BS, Maurer T, Harris WH. Revision of the acetabular component without cement after a previous acetabular reconstruction with use of a bulk femoral head graft in patients who had congenital dislocation or dysplasia. A follow-up note. J Bone Joint Surg Am. 1999;81:1703–1706. doi: 10.2106/00004623-199912000-00007. [DOI] [PubMed] [Google Scholar]
- 43.Gross AE. Revision arthroplasty of the acetabulum with restoration of bone stock. Clin Orthop Relat Res. 1999;(369):198–207. doi: 10.1097/00003086-199912000-00021. [DOI] [PubMed] [Google Scholar]
- 44.Silverton CD, Rosenberg AG, Sheinkop MB, Kull LR, Galante JO. Revision total hip arthroplasty using a cementless acetabular component. Technique and results. Clin Orthop Relat Res. 1995;(319):201–208. [PubMed] [Google Scholar]
- 45.Sun C, Lian YY, Jin YH, Zhao CB, Pan SQ, Liu XF. Clinical and radiographic assessment of cementless acetabular revision with morsellised allografts. Int Orthop. 2009;33:1525–1530. doi: 10.1007/s00264-009-0722-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leopold SS, Rosenberg AG, Bhatt RD, Sheinkop MB, Quigley LR, Galante JO. Cementless acetabular revision. Evaluation at an average of 10.5 years. Clin Orthop Relat Res. 1999;(369):179–186. [PubMed] [Google Scholar]
- 47.Rosenberg AG. Cementless acetabular components: the gold standard for socket revision. J Arthroplasty. 2003;18(3) Suppl 1:118–120. doi: 10.1054/arth.2003.50108. [DOI] [PubMed] [Google Scholar]
- 48.Levine B, Della Valle CJ, Jacobs JJ. Applications of porous tantalum in total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:646–655. doi: 10.5435/00124635-200611000-00008. [DOI] [PubMed] [Google Scholar]
- 49.Siegmeth A, Duncan CP, Masri BA, Kim WY, Garbuz DS. Modular tantalum augments for acetabular defects in revision hip arthroplasty. Clin Orthop Relat Res. 2009;467:199–205. doi: 10.1007/s11999-008-0549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22(6) Suppl 2:151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 51.Nehme A, Lewallen DG, Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res. 2004;(429):201–208. doi: 10.1097/01.blo.0000150133.88271.80. [DOI] [PubMed] [Google Scholar]
- 52.Boscainos PJ, Kellett CF, Maury AC, Backstein D, Gross AE. Management of periacetabular bone loss in revision hip arthroplasty. Clin Orthop Relat Res. 2007;465:159–165. doi: 10.1097/BLO.0b013e3181560c6c. [DOI] [PubMed] [Google Scholar]
- 53.Ballester Alfaro JJ, Sueiro Fernández J. Trabecular Metal buttress augment and the Trabecular Metal cup-cage construct in revision hip arthroplasty for severe acetabular bone loss and pelvic discontinuity. Hip Int. 2010;20(Suppl 7):S119–S127. doi: 10.1177/11207000100200s720. [DOI] [PubMed] [Google Scholar]
- 54.Staheli LT. Slotted acetabular augmentation. J Pediatr Orthop. 1981;1:321–327. doi: 10.1097/01241398-198111000-00014. [DOI] [PubMed] [Google Scholar]
- 55.Lee JM, Cho KH, Cha YS. A morselized impaction allograft used for the defect of acetabulum in revision total hip arthroplasty: minimum 10-year follow-up. J Korean Musculoskelet Transplant Soc. 2012;12:76–84. [Google Scholar]
- 56.Lee JM, Nam HT. Acetabular revision total hip arthroplasty using an impacted morselized allograft and a cementless cup: minimum 10-year follow-up. J Arthroplasty. 2011;26:1057–1060. doi: 10.1016/j.arth.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 57.Lee JM, Sun MY, Jeon JB. Acetabular revision total hip arthroplasty using morselized impaction allograft for acetabular bone defect above Paprosky type III. J Korean Musculoskelet Transplant Soc. 2013;13:58–64. [Google Scholar]