Abstract
Levels of certain circulating cytokines and related immune system molecules are consistently altered in schizophrenia and related disorders. In addition to absolute analyte levels, we sought analytes in correlation networks that could be prognostic. We analyzed baseline blood plasma samples with a Luminex platform from 72 subjects meeting criteria for a psychosis clinical high-risk syndrome; 32 subjects converted to a diagnosis of psychotic disorder within two years while 40 other subjects did not. Another comparison group included 35 unaffected subjects. Assays of 141 analytes passed early quality control. We then used an unweighted co-expression network analysis to identify highly correlated modules in each group. Overall, there was a striking loss of network complexity going from unaffected subjects to nonconverters and thence to converters (applying standard, graph-theoretic metrics). Graph differences were largely driven by proteins regulating tissue remodeling (e.g. blood-brain barrier). In more detail, certain sets of antithetical proteins were highly correlated in unaffected subjects (e.g. SERPINE1 vs MMP9), as expected in homeostasis. However, for particular protein pairs this trend was reversed in converters (e.g. SERPINE1 vs TIMP1, being synthetical inhibitors of remodeling of extracellular matrix and vasculature). Thus, some correlation signals strongly predict impending conversion to a psychotic disorder and directly suggest pharmaceutical targets.
Introduction
Circulating levels of immune system proteins and related signaling agents are consistently altered in schizophrenia. This observation includes unmedicated first episode psychosis patients1,2 and persons at clinical high-risk who subsequently convert to psychosis3–5. Consistent findings include proteins in the immune system acute phase response and in the plasminogen activating system1. Many of the proteins influence brain function directly, crossing blood–brain barrier (BBB) and signaling glia or other perivascular cells. These immune signaling molecules also regulate brain function by influencing BBB endothelial cell function and general integrity. Such findings support the hypothesis that psychosis involves brain dysregulation by an altered peripheral immune system and aberrant signaling at BBB.
Persons meeting clinical high-risk criteria have about a 20% risk of developing a psychotic disorder within two years, and that is 100-fold higher than the 0.2% general population risk6. Baseline factors differentiating clinical high-risk subjects that convert to psychosis vs do not convert may be of etiologic significance. Previous psychosis risk prediction studies compared levels of immune signaling molecules, individually or in a linear combination3–5,7. Since responses of the peripheral immune system are highly coordinated, investigation of the correlation patterns of immune signaling molecules might also be informative. In this analysis we sought networks of highly correlated immune molecules in persons at clinical high-risk who developed psychosis, compared to those who did not develop psychosis over the two-year follow-up period. We also analyzed data from unaffected comparison subjects. In some respects, the correlation networks were strikingly different in converters. Some distinguishing proteins were modulators of extracellular matrix (ECM) components and BBB.
Schizophrenia pervasively impacts brain functions, typically causing in adolescence or early adulthood disability that is chronic and relapsing. Improved clinical outcomes are often associated identification and treatment of the disorder early in its course8, implying the desirability of seeking reliable predictors based upon readily accessible biomarkers. Moreover, early indicators might be close to the ultimate causes of schizophrenia.
Thus, researchers (e.g., Domenici et al.9 and Dickerson et al.10) have investigated in particular proteins and other blood plasma analytes that distinguish unaffected comparison subjects from patients with schizophrenia or subsets of such patients11,12. Included among the analytes have been concentrations of circulating cytokines and other immune system signaling molecules. These can be altered in schizophrenia across all stages of the disorder including the prodromal stage.
One key concept of this paper is information from networks. As Fredrickson et al.13 stated, “…accumulation of many individually noisy indicator variables can yield highly stable estimates of the underlying factors they share in common.” Thus, we sought networks of highly correlated signals among each of three groups (converters, nonconverters, and unaffected comparison subjects) from our North American Prodrome Longitudinal Study (NAPLS) project14. The emphasis was analysis of data collected at the prodrome state (see Supplement Figure S1). To place the present work in context, NAPLS is a multi-site program that has accumulated, cleaned, stored, analyzed, and reported many types of clinical and laboratory assays, leading to proposals of various predictors and mechanisms for the development of psychosis15.
Thus, the present emphasis differs from some earlier works in that it is longitudinal and it pertains entirely to networks. The three networks from the three groups are formed by proteins that are highly correlated over subjects in each group, far more highly correlated than could be reasonably explained by chance. All of the reported correlations are positive because there we observed no negative correlations of the same, very high magnitude.
Many of the distinguishing analytes we found turned out to be prominent in the immune system3 and its interaction with trophic factors and ECM components. Thus, the proper arena of this paper became neuroimmunology. Particularly in the last decade, many important reports have developed this view of mental illnesses (e.g., Khandaker et al.16).
A second key concept is the pleiotropic roles of proteins customarily considered in the context of hemostasis vs hemorrhage. Specifically, as Nave and Ehrenreich demonstrated17, “It is becoming apparent that coagulation factors do much more than simply act in the blood-coagulation cascade.” For example, fibrinogen associates with schizophrenia18, Alzheimer disease19, and multiple sclerosis (MS)20.
A third key concept is that the peripheral immune system impacts physiological and pathological brain function21–23. We have hypothesized that peripheral immune system dysregulation may contribute to development of psychosis. Furthermore, the construction of the above classifier3 survived permutation testing very well, implying that certain peripheral blood plasma proteins and conversion of patients to schizophrenia are associated. Finally, dysregulation of BBB permeability, transendothelial cell migration, or remodeling of brain ECM or vasculature—all impacted by the immune system—could obviously be important in the events leading to frank psychotic mood disorders including schizophrenia.
Materials and methods
Subjects
The aims and methods of North American Prodrome Longitudinal Study (NAPLS2) were described in detail previously24. Briefly, NAPLS2 is an eight-site observational study of predictors and mechanisms of conversion to psychosis. The NAPLS2 cohort includes 765 subjects at clinical high-risk for psychosis, based on the Criteria of Prodromal States, determined by the Structured Interview for Prodromal Syndromes, and rated with the Scale of Prodromal Symptoms25 (see Supplement). In addition, the cohort includes 280 demographically similar unaffected comparison subjects. Subjects were between ages 12 and 35 at baseline. Psychiatric diagnoses were determined by the Structured Clinical Interview for DSM IV26. Clinical assessments were performed every six months, and subjects were followed for up to two years. The study was approved by the Institutional Review Board at each site, and each subject provided written informed consent or assent, with a parent or guardian also consenting for minor subjects. Demographics for subjects in the present study are provided in Table 1.
Table 1.
Demographic and clinical characteristics of study subjects taken at baseline of longitudinal study
| Unaffected comparison (UC) N = 35 | Clinical high-risk, nonconverters (CHR-NC) N = 40 | Clinical high-risk, Converters (CHR-C) N = 32 | |
|---|---|---|---|
| Age, average (SD) | 20 (4.5) | 19.5 (4.6) | 19.2 (3.7) |
| Ancestry | |||
| %Caucasian | 60%, | 65% | 55% |
| %African | 31% | 17.5% | 21% |
| %Asian | 9% | 17.5% | 24% |
| Sex, % female | 34% | 37.5% | 30.3% |
| SES, average (SD) | 4.8 (1.8) | 4.5 (2.3) | 4.5 (1.8) |
| Time blood draw, average (SD) | 12.:12 pm (1.85 h) | 12:39 pm (2.0 h) | 11:59 am (1.79 h) |
| Prescription medication | |||
| Antipsychotica | 0% | 25% | 13% |
| Antidepressantb | 1% | 30% | 25% |
| Stimulant | 0% | 8% | 6% |
| Mood stabilizer | 0% | 5% | 3% |
| Benzodiazepinec | 0% | 5% | 13% |
| NSAID | 0% | 0% | 0% |
| Antibiotic | 0% | 0% | 0% |
| Substance Use | |||
| Tobacco used | 9% | 30% | 44% |
| Alcohol use | 46% | 48% | 38% |
| Marijuana usee | 9% | 25% | 31% |
| Current co-morbid DSM IV Diagnosis | |||
| Depressionf | 0% | 45% | 50% |
| Anxiety Disordersg,* | 3% | 60% | 56% |
aCHR-C vs UC FET p-value = 0.047, CHR-NC vs UC Fisher Exact Test (FET) p-value = 0.001
bCHR-C vs UC FET p-value = 0.011, CHR-NC vs UC FET p-value = 0.002
cCHR-C vs UC FET p-value = 0.047
dCHR-C vs UC FET p-value = 0.001, CHR-NC vs UC FET p-value = 0.02
eCHR-C vs UC FET p-value = 0.020, CHR-NC vs UC FET p-value = 0.056
fCHR-C vs UC FET p-value < 0.0001, CHR-NC vs UC FET p-value < 0.0001
gCHR-C vs UC FET p-value < 0.0001, CHR-NC vs UC FET p-value < 0.0001
*Depression disorders include Major Depression, Depressive Disorder Not Otherwise Specified, and Dysthymic Disorder. Anxiety Disorders include Obsessive Compulsive Disorder, Post-Traumatic Stress Disorder, Panic Disorder, Agoraphobia, Social Phobia, Specific Phobia, Generalized Anxiety Disorder
Plasma analytes
During a baseline visit, blood samples were drawn using Becton Dickenson P100 blood collection tubes containing EDTA (as anticoagulant), proprietary protein stabilizers, and a mechanical separator. Mean processing time to −80 °C storage was 28 min (SD = 2 min). Plasma samples were subsequently sent on dry ice to Myriad RBM (Austin TX), a laboratory that has maintained CLIA Accreditation since 2006. Samples were analyzed with the Human DiscoveryMAP v. 1.0 assays of 185 analytes associated with immune system function, hormonal responses, oxidative stress, and metabolism. In total 141 analytes passed preliminary quality control and were used in our analyses. We standardized to z-scores the results for each analyte using the average and SD values of the unaffected comparison subjects. Quality control, normalization methods, and tests with duplicated samples were performed, as previously described3.
Data analyses
We used an unweighted co-expression network analysis to identify highly correlated networks of analytes in each of the three groups. Pearson correlations were calculated using macros and built-in functions in Excel. Limited by the smallest group size (converters, n = 32), we performed random re-sampling with replacement 10,000 times by drawing subgroups of 28 subjects from each of the three groups. In other words, the 9870 pairs of analytes were compared in 28-dimensional space 10,000 times to calculate Pearson correlations. We compared those correlation values to a common threshold and then recorded the number of times a pair exceeded the threshold (flowcharts in Supplement Figure S2). The correlation threshold selected was 0.7662; if two 28-dimensional vectors were populated by a Gaussian distribution, then the probability of their correlation exceeding this value would be 1E-6. Thus, with 9870 pairs of analytes, we expect only 1 such value among all pairs about once in 100 trials.
Considering all 107 subjects and all 9870 pairs of analytes at once, distribution analysis using EasyFit (MathWave, Dnepropetrovsk, Ukraine) revealed that no normal distribution fit the observations but the Johnson SU distribution27 did. Technically, normal distributions failed to fit the observed distribution of correlations in both Kolmogorov–Smirnov and Anderson–Darling tests for even α = 0.01; by contrast, the Johnson SU distribution achieves α = 0.2 in both tests. The Johnson SU distribution accommodates a one-sided tail of very strong, positive correlations not balanced by even one negative correlation of equal magnitude. Therefore, we focused on only the very strong, positive correlations (Fig. 1).
Fig. 1. A histogram with 20 bins of 9870 correlation values among 141 analytes over all 107 subjects.
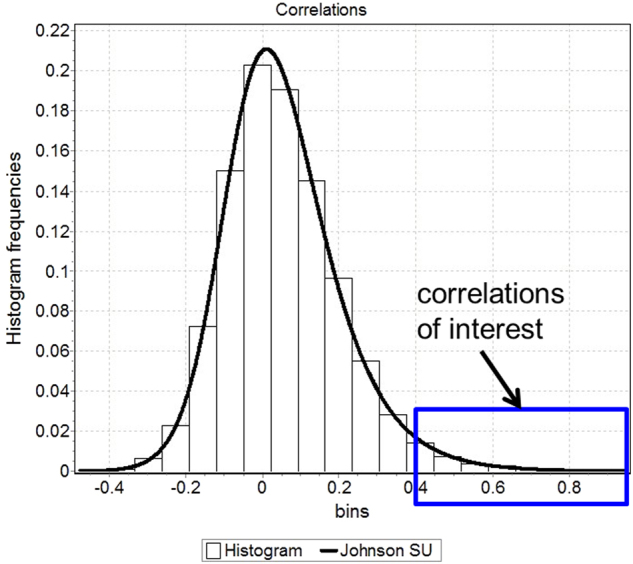
The shown distribution is a Johnson SU fit with four parameters: gamma = −1.2967, delta = 2.2624, lambda = 0.26593, xi = −0.12371. The present study is distinguished from many others by focusing on the tail of very strong, positive correlations (blue box) that are not balanced by any negative correlations of the same magnitude
We validated our approach by first randomly permuting all 107 subjects, then analyzing 28-subject subsets of the pseudo-groups exactly as if they were from the true data. Neither the design nor the implementation of the algorithm conferred any obvious, consistent distinction to edge counts of graphs of very strong correlations in the three pseudo-groups. This result indicates that both the design and implementation of the program correctly achieved unbiased identification of correlation networks.
Measures of network complexity include those of Bonchev and Buck28 (see their formulas 19a,b) in which the normalized edge complexity is the number of (undirected) edges e divided by the maximum possible number of edges using the same number of vertices v, namely, v*(v-1)/2.
Protein network analyses were conducted using Ingenuity Pathway Analysis (IPA) (QIAGEN N.V., Venlo, The Netherlands).
Results
Protein correlation networks distinguish the three groups
There was a striking loss of network complexity going from unaffected to nonconverters and thence to converter subjects. Analyte pairs with Pearson correlations exceeding an a priori threshold in at least 5000 of 10,000 random draws of 28 subjects from each group are shown for unaffected subjects (Fig. 2), nonconverters (Fig. 3), and converters (Fig. 4).
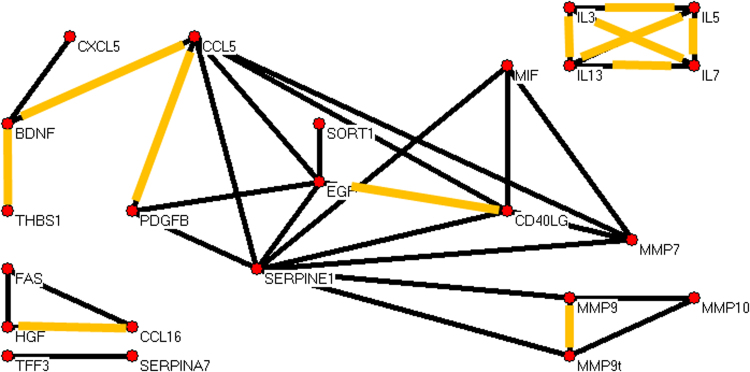
Fig. 2. Unaffected comparison subject data yielded a graph of strongly correlated analytes with 23 analytes (vertices) and 34 robust correlations (edges).
Blood plasma proteins are labeled by their gene common symbols. The correlations in orange appear in all three graphs. We note eight analytes that include SERPINE1, and in particular SERPINE1 correlations include the matrix metalloproteinases MMP7, MMP9, and MMP10. MMP9t denotes an assay for both pro-MMP9 and mature MMP9
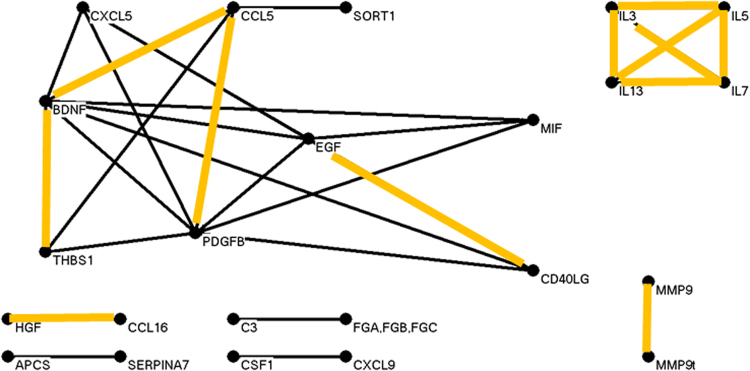
Fig. 3. Nonconverter data yielded a graph of strongly correlated analytes with 23 analytes and 30 robust correlations.
SERPINE1 correlations are completely absent, suggesting a loss of requlation of expression of the gene
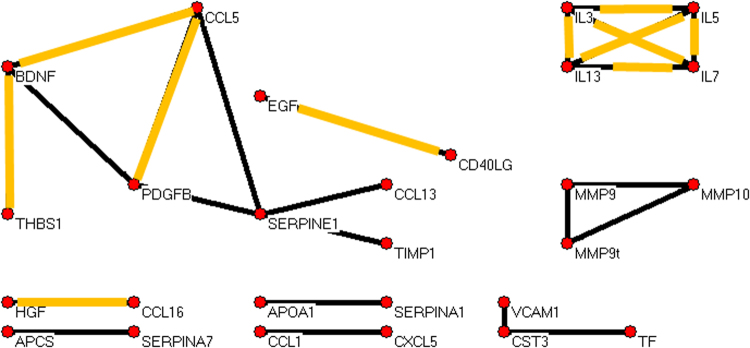
Fig. 4. Converter data yielded a graph of strongly correlated analytes with 27 analytes and 24 robust correlations.
Four SERPINE1 correlations are present, suggesting changes in requlation of the SERPINE1 gene compared to unaffected and nonconverter assays. Remarkable is the gained correlation of SERPINE1 and TIMP1 because both proteins inhibit anticogulation and vascular remodeling in some contexts and both generally promote anti-inflammation. Furthermore, TIMP1 is completely absent in unaffected and nonconverter graphs. Also, the strong SERPINE1 correlations with matrix metalloproteinases (MMPs) in the unaffected graph are absent in this converter graph
For unaffected, nonconverter, and converter groups we calculated a simple metric of graph complexity, namely the ratio of numbers of edges to vertices; respective values were 1.48, 1.30, and 0.89 edges per vertex. Normalized edge complexities were 0.134, 0.119, and 0.062. Moreover, it is visually apparent that the three graphs are quite different in terms of edge densities. Additional graphs and experiments with alternative choices of thresholds led to the same trend and are in the Supplement. This trend toward simplicity going from unaffected to nonconverter to converter for plasma proteins parallels the same for leukocytic microRNAs reported earlier29.
Notably, in unaffected subjects there was a network involving the proteins SERPINE1 (plasminogen activator inhibitor-1), MMP7, MMP9 (activated), MMP9t (total), and MMP10 (matrix metalloproteinases). While SERPINE1 is anti-remodeling, the others are pro-remodeling, and a balance (correlation of some pairs) might be expected in hemostasis vs hemorrhage. In contrast, nonconverters and converters lacked these strong SERPINE1 correlations. Furthermore, while the important inhibitor of remodeling TIMP1 (tissue inhibitor of metalloproteinases) was absent (at the chosen threshold for inclusion) from strong correlations in unaffected and nonconverter graphs, it generally exceeded the threshold correlation value with SERPINE1 in converter subjects. In detail, the SERPINE1 vs TIMP1 correlations exceeded the threshold in the three sets of 10,000 random draws of 28 subjects in totals of <10, <10, and >8300 times, respectively. As sets, the actual SERPINE1 and TIMP1 correlation values over 10,000 draws for converter subjects (mean correlation = 0.79, SD = 0.03) tended to be significantly greater (p-value < 1E-100) than the values in nonconverters (mean = 0.55, SD = 0.06) and unaffected subjects (mean = 0.50, SD = 0.09). The dramatic distinction of SERPINE1 and TIMP1 correlations in converters is further illustrated in the Supplement (Figure S10).
What could explain the extremely high correlations of SERPINE1 and TIMP1 in converters only? We note that another protein, CTGF (connective tissue growth factor), is known to promote mutual expression of SERPINE1 and TIMP1 and so might be part of the explanation (see Discussion).
From a previous study by Domenici el al.9 we evaluated SERPINE1 vs TIMP1 correlations. The subjects contributing to that study were schizophrenia patients and controls. We calculated correlations for 10,000 random subsets of 200 subjects drawn randomly from 267 control subjects and 229 schizophrenia patients. The results (Supplement Figure S11) indicated patients had far stronger SERPINE1 vs TIMP1 correlations than controls.
Subnetworks common among all three groups
Several pairs of analytes were highly correlated in all three groups (highlighted in orange in Figs. 2, 3, and 4). Among them was the complete graph formed by interleukins 3, 5, 7, and 13. We examined the correlation pattern of these interleukins in the Domenici data9 for 267 unaffected subjects. As shown in the Supplement Figure S9, the four interleukins were highly correlated in that cohort as well.
Discussion
Immune correlation networks and psychosis risk
Psychosis conversion in high-risk subjects was characterized by marked simplifications of networks of correlated proteins that regulate tissue remodeling; this might be consistent with the hypothesis of BBB dysregulation in schizophrenia30. Notable were graph changes involving SERPINE1. The serine protease inhibitor SERPINE1 is the major inhibitor of the plasminogen activator PLAT; PLAT activates plasminogen to plasmin (the final substrate of the fibrinolytic system) which in turn degrades fibrin. Thus, a focus infra is SERPINE1 and related proteins31.
Relevant to the present study, schizophrenia patients are subject to increased risk of cardiovascular disease, reduced risk of certain types of cancer, and possibly some aspects of accelerated aging; all these general observations have in turn been associated with SERPINE1 or related proteins32–36.
More particularly, connection of schizophrenia with proteins important in coagulation homeostasis has been amplified by recent studies of Hoirisch-Clapauch, Nardi, and their colleagues37, starting with anecdotal descriptions of possible benefits to five schizophrenia patients of treatment with warfarin (which would seemingly counter the effects of increased SERPINE1 and decreased PLAT activity). They proposed that normalization of levels of PLAT in the psychotic brain might enable long-term remission of psychotic symptoms.
PLAT is secreted by many cell types including blood vessel endothelial cells that are known to express diverse genes differentially even among regions of the same artery38–40. In neurons PLAT occurs in dendrites and synapses; it is stored in pre-synaptic vesicles that cross the synaptic cleft after depolarization, subject to regulation by astrocytes41,42.
Aside from hemostasis, PLAT has related roles in smooth muscle signaling in blood vessel tunica31,43, several types of ECM signaling44, and BBB permeability in the context of cerebral ischemia45. Given the large numbers of schizophrenia patients who are comorbid for cardiovascular diseases, who require treatment with warfarin or functionally related pharmaceuticals, and who are not in remission, the intersection of hemostasis and psychosis cannot be simple. However, Hoirisch-Clapauch et al.34,46. provided additional reasoning and evidence of a connection, finding lower PLAT levels among 70 schizophrenia patients compared with 98 age-matched controls. Since the principal regulator of PLAT levels is SERPINE1, Hoirisch-Clapauch and Nardi46 postulated that inflammatory conditions could increase the risk of schizophrenia through mechanisms involving SERPINE1 levels.
PLAT is highly pleiotropic as, therefore, might be some of its regulators. Two of many reported PLAT substrates directly relevant to psychiatry have functions in epidermal growth factor receptor (EGFR)-mediated neuroprotection47,48 and the dynamics of the glutamate receptor and ion channel protein NMDAR (antagonized by phencyclidine in a model of schizophrenia)49,50. Furthermore, PLAT is expressed in brain endothelial cells, neurons, and microglia. It is strongly and negatively correlated with mRNA for OCLN (occludin)51, a protein important in the stability and permeability of tight junctions. Reactive oxygen species can cause rapid release of PLAT in monocyte and endothelia cocultures52. In a related effect (noting the above correlations in unaffected subjects), MMP9 promotes monocyte migration through brain parenchymal basement membrane52.
Consistent with our findings, there is also an emerging literature implicating the plasminogen pathway in schizophrenia. This literature points towards down-regulation of PLAT, up-regulation of factors including SERPINE1 that inhibit PLAT activation34,37,46,53, and consequences of elevated fibrinogen (fibrin) including incorrect differentiation of progenitors of oligodendrocytes into astrocytes in MS20. This misguided differentiation might relate to reported low levels of oligodendrocytes in layer five of prefrontal cortex in schizophrenia54.
For data from the same subjects presently studied we previously reported that proteins involved in the plasminogen pathway, including MMP7 and Factor 7, predicted psychosis conversion3. In our previous publication we did not find that expression levels of SERPINE1 or TIMP1 were substantially increased going from nonconverters to converters. By contrast, the current study suggests that the extreme changes in correlation networks of SERPINE1 and related proteins, especially TIMP1, may indeed be informative.
Most notable is an interpretation of CTGF in idiopathic pulmonary fibrosis55,56 and other diseases57–59 that might explain the remarkable correlation of SERPINE1 and TIMP1 levels in converters. Unfortunately, in our blood plasma assays CTGF was not detected in 50–70% of the subjects in all three of the groups, precluding its correlation analysis. However, regarding CTGF as a known driver of SERPINE1 and TIMP1 levels, we note that local upregulation of CTGF by a type of alveolar cell, resulting in proliferation of local fibroblasts, has been proposed as a surrogate biomarker of idiopathic pulmonary fibrosis (IPF);55 CTGF is therefore the target of ongoing IPF clinical trials of the fully human monoclonal antibody Pamrevlumab by FibroGen (San Francisco CA) (trial NCT01890265 at ClinicalTrials.gov).
The serine protease inhibitor SERPINE1 is a “suicide protein” in the serpin superfamily and is the major inhibitor of the plasminogen activator PLAT and related protein PLAU (plasminogen activator urokinase). Thus, SERPINE1 is a crucial down regulator of fibrinolysis and ECM degradation31. In wound healing, SERPINE1 contributes to regulation of cell proliferation and tissue remodeling43, as well as other aspects of cell signaling and migration44,45.
Studies of samples from clinical high-risk psychiatric patients in the literature34 and in our data (Supplement Figure S10) can exhibit somewhat elevated levels of SERPINE1. Interestingly, de Fouw et al.60 reported that the glycoprotein Protein S (PROS1) accelerated neutralization of SERPINE1, thereby increasing PLAT activity; this finding suggests possibilities for indirect control of PLAT levels and function. In its free form, PROS1 is a cofactor of protein C (PROC) in the anticoagulation pathway. PROS1 and PROC are vitamin K-dependent plasma proteins61, included among the cofactors in the inactivation of the prothrombinase complex. PROS1 also exists in a complex with complement C4B-binding protein62. Complement inhibitor C4B-binding protein enhances plasminogen activation63. Isotypes of the C4 protein have been implicated in schizophrenia gene association studies64.
SERPINE1 levels are up-regulated by inflammatory cytokines including IL6, TNF, and TGFB1, as reviewed by Brown et al.65. These researchers postulated that inflammatory conditions increased the risk of schizophrenia through a combination of mechanisms involving increased SERPINE1 levels or decreased free PROS1 levels.
PLAT was not measured in our assays, but more should be said about some of its extensive functions66,67. PLAT degrades ECM and in particular cleaves the large glycoprotein RELN, all contributing to cell migration and tissue remodeling, particularly revascularization. PLAT affects neural, endothelial, and glial cells, driving multiple, sometimes opposing effects by activating or otherwise regulating diverse transcription factors and receptors. Regarding the neurotrophin BDNF (brain-derived neurotrophic factor), PLAT promotes the cleavage of neuronal proBDNF to mature BDNF, a function essential for late-phase long-term potentiation68. Pro- and mature BDNF have important and opposing effects on synaptic plasticity, regulation of neurogenesis, and neuronal survival69. Only the mature BDNF was assayed by us; it is prominent in Figs. 2–4.
MMP9 is also an important factor in ECM maintenance and remodeling, assayed herein both as mature MMP9 and as the total of proMMP9 and mature MMP9 (labeled MMP9t in our graphs). It regulates glutamate receptors, modulates physiological and morphological synaptic plasticity, and is regulated by glutamate at excitatory synapses70. MMP9 and other extracellular proteases such as plasmin convert proBDNF to mature BDNF71. PLAT, PLAU, plasmin, and MMP9 all have roles in BBB disruption after stroke72. MMP9 itself is activated in presence of oxidative stress and in turn promotes the receptor for advanced glycation end-product (RAGE) (to be described in a forthcoming paper by D. Dwir et al.), said to induce a self-reinforcing cycle of inflammatory responses and further oxidative stress73,74. In addition, MMP9 is involved in the degradation of the perineuronal net, a type of ECM that wraps fast-spiking parvalbumin interneurons; the perineuronal net is known to be affected in the medial prefrontal brain of schizophrenia patients75,76. In mice, intravenously administered PLAT was detected within the brain parenchyma and cerebrospinal fluid, having crossed the BBB by transcytosis77.
In summary, for converter subjects SERPINE1 was no longer correlated with antithetical MMPs, but instead became highly correlated with the synthetical TIMP1. This observation and the above integration of these proteins and CTGF in multiple disorders suggest the potential importance of CTGF inhibition. Several inhibitors of CTGF have been proposed and studied; for example, insulin and an siRNA have been studied in the context of inhibition of vascular remodeling in diabetic retinopathy78. However, certain advantages attend a monoclonal antibody for CTGF inhibition.
Interleukin networks common in all subjects
We found that IL3, IL5, IL7, and IL13 form a highly correlated module in all groups, and replicated this finding in an external test set of unaffected subjects (Figure S8), suggesting co-regulation and closely related functions of these cytokines. Three genes, IL3, IL5, and IL13 (and also IL4), exist as a cytokine gene cluster on chromosome arm 5q. Unfortunately, IL4 detection was weak (below LLOQ) or missing in more than half our samples, precluding correlation analysis with the rest of that cluster. But IL4 and IL7 are among the six “γ-chain utilizing” interleukins, while IL3, IL4, IL5, and IL13 are the four “IL4-like” interleukins; both sets of proteins are considered tightly packed α-helices in a four-helix bundle motif of short core helices79. There are about 45 human interleukins, so the members of the identified correlation cluster are more similar than would be expected by chance.
The top shared pathway for IL3, IL5, IL7, and IL13 from application of IPA was “hematopoiesis from multipotent stem cells” (p = 1.6E-9). IL3 promotes hematopoietic stem cell proliferation, and IL7 regulates development of the common lymphoid progenitor cells and development of B-cell, T-cell, and NK-cell lineages. In detail, IL3 regulates development of the common myeloid progenitor, and IL5 regulates development of neutrophils and eosinophils80. Less is known regarding IL13, but its receptor, IL12A1, is selectively expressed on CD62L+ cells (common lymphoid progenitors), again suggesting a role in regulation of lymphoid cell differentiation81. Normally, the circulating proportions of neutrophils, lymphocytes, monocytes, and eosinophils are relatively constant, so possibly IL3, IL5, IL7, and IL13 in our graphs contribute to maintenance of homeostatic proportions of those cell types.
Limitations
Foremost among limitations, the sample sizes of the three groups in our study were all small. We plan to add data from more subjects in the near future (NAPLS3). In addition, the Luminex platform is less reproducible for certain proteins than other platforms, including Meso-Scale, ELISA, and microfluidic ELISA. We plan to employ microfluidic ELISA in pending analyses. Another limitation is the two-year limit for the definition of conversion. Although the rate of psychosis conversion is much lower after two years, we anticipate that up to 10% of our nonconverters will eventually convert to psychosis, implying some uncertainty in all our statements about nonconverters vs converters. However, by considering only networks constructed from extremely high correlations and thousands of random subsets of the groups, we consider it unlikely that the findings could be explained entirely by chance alignments. Lastly, many proteins functionally related to those in our assays were not considered due to costs. Therefore, important signals might be missing from our analyses. Despite all the seemingly plausible relationships described supra, our findings need confirmation and expansion in other cohorts. Further work of multiple types, e.g., as that being undertaken by Sorokin82, is required to directly link peripheral immune dysregulation to the etiology of schizophrenia.
Translation to the clinic
The present work suggests that additional longitudinal studies of clinical high-risk patients with logically expanded assays of agents of immune responses could lead to parsimonious lists of proteins implicated in conversion to schizophrenia. Ratios of distinguishing proteins for a new patient could be compared with historical ratios to predict membership among nonconverters or converters.
Furthermore, the above potential connection of SERPINE1 and TIMP1 expression with CTGF regulation might lead to investigation of Pamrevlumab (http://www.fibrogen.com/pamrevlumab-trials/) or related agents of CTGF inhibition. The potential medical value of inhibition of CTGF in various diseases has long been recognized. The recent appearance of Pamrevlumab as a potential treatment for IPF and its repurposing suggested herein for prevention of conversion to psychosis might be especially important. Repurposing is a drug development strategy with huge savings of time and expense.
Electronic supplementary material
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Larry J. Seidman deceased on 7 September 2017.
Electronic supplementary material
Supplementary Information accompanies this paper at (10.1038/s41398-018-0158-y).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sabherwal S, English JA, Focking M, Cagney G, Cotter DR. Blood biomarker discovery in drug-free schizophrenia: The contributionof proteomics and multiplex immunoassays. Expert. Rev. Proteom. 2016;13:1141–1155. doi: 10.1080/14789450.2016.1252262. [DOI] [PubMed] [Google Scholar]
- 2.Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol. Psychiatry. 2011;70:663–671. doi: 10.1016/j.biopsych.2011.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perkins DO, et al. Towards a psychosis risk blood diagnostic for persons experiencing high-risk symptoms: Preliminary results from the NAPLS project. Schizophr. Bull. 2015;41:419–428. doi: 10.1093/schbul/sbu099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan MK, et al. Development of a blood-based molecular biomarker test for identification of schizophrenia before disease onset. Transl. Psychiatry. 2015;5:e601. doi: 10.1038/tp.2015.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Metcalf SA, et al. Serum C-reactive protein in adolescence and risk of schizophrenia in adulthood: a prospective birth cohort study. Brain Behav. Immun. 2017;59:253–259. doi: 10.1016/j.bbi.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fusar-Poli P, et al. At risk or not at risk? A meta-analysis of the prognostic accuracy of psychometric interviews for psychosis prediction. World Psychiatry. 2015;14:322–332. doi: 10.1002/wps.20250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khandaker GM, Pearson RM, Zammit S, Lewis G, Jones PB. Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life: a population-based longitudinal study. JAMA Psychiatry. 2014;71:1121–1128. doi: 10.1001/jamapsychiatry.2014.1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am. J. Psychiatry. 2005;162:1785–1804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- 9.Domenici, E.et al. Plasma protein biomarkers for depression and schizophrenia by multi analyte profiling of case-control collections. PLoS ONE5, (2010).. [DOI] [PMC free article] [PubMed]
- 10.Dickerson F, et al. Multianalyte markers of schizophrenia and bipolar disorder: a preliminary study. Schizophr. Res. 2015;168:450–455. doi: 10.1016/j.schres.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Guest PC, et al. Proteomic profiling in schizophrenia: enabling stratification for more effective treatment. Genome Med. 2013;5:25. doi: 10.1186/gm429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramsey JM, et al. Distinct molecular phenotypes in male and female schizophrenia patients. PLoS ONE. 2013;8:e78729. doi: 10.1371/journal.pone.0078729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fredrickson BL, et al. A functional genomic perspective on human well-being. Proc. Natl Acad. Sci. USA. 2013;110:13684–13689. doi: 10.1073/pnas.1305419110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cannon TD, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch. Gen. Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cannon TD, et al. An individualized risk calculator for research in prodromal psychosis. Am. J. Psychiatry. 2016;173:980–988. doi: 10.1176/appi.ajp.2016.15070890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khandaker GM, et al. Inflammation and immunity in schizophrenia: implications for pathophysiology and treatment. Lancet Psychiatry. 2015;2:258–270. doi: 10.1016/S2215-0366(14)00122-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nave KA, Ehrenreich H. A bloody brake on myelin repair. Nature. 2018;553:31–32. doi: 10.1038/d41586-017-08232-2. [DOI] [PubMed] [Google Scholar]
- 18.Korschenhausen DA, Hampel HJ, Ackenheil M, Penning R, Muller N. Fibrin degradation products in post mortem brain tissue of schizophrenics: a possible marker for underlying inflammatory processes. Schizophr. Res. 1996;19:103–109. doi: 10.1016/0920-9964(95)00073-9. [DOI] [PubMed] [Google Scholar]
- 19.Ryu JK, McLarnon JG. A leaky blood-brain barrier, fibrinogen infiltration and microglial reactivity in inflamed Alzheimer’s disease brain. J. Cell. Mol. Med. 2009;13:2911–2925. doi: 10.1111/j.1582-4934.2008.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petersen MA, et al. Fibrinogen activates BMP signaling in oligodendrocyte progenitor cells and inhibits remyelination after vascular damage. Neuron. 2017;96:1003–1012. doi: 10.1016/j.neuron.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weber MD, Godbout JP, Sheridan JF. Repeated social defeat, neuroinflammation, and behavior: monocytes carry the signal. Neuropsychopharmacology. 2017;42:46–61. doi: 10.1038/npp.2016.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marin IA, Kipnis J. Central nervous system: (Immunological) ivory tower or not? Neuropsychopharmacology. 2017;42:28–35. doi: 10.1038/npp.2016.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Filiano AJ, Gadani SP, Kipnis J. How and why do T cells and their derived cytokines affect the injured and healthy brain? Nat. Rev. Neurosci. 2017;18:375–384. doi: 10.1038/nrn.2017.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Addington JA, et al. North American Prodrome Longitudinal Study (NAPLS 2): overview and recruitment. Schizophr. Res. 2012;142:77–82. doi: 10.1016/j.schres.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller TJ, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am. J. Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- 26.First, M. B., Spitzer R. L., Givvon M., Williams J. B. W. Structured Clinical Interview for DSM-IV TR Axis I Disorders, Non-patient Edition (SCID-I/NP) (Biometrics Research, New York State Psychiatric Institute, New York, 2002).
- 27.Johnson NL. Systems of frequency curves generated by methods of translation. Biometrika. 1949;36:149–176. doi: 10.1093/biomet/36.1-2.149. [DOI] [PubMed] [Google Scholar]
- 28.Bonchev, D. & Buck, G. A. in Complexity in Chemistry, Biology, and Ecology (eds. Bonchev, D. & Rouvray, D. H.) 191–235 (Springer US, 2005).
- 29.Jeffries CD, et al. Insights into psychosis risk from leukocyte microRNA expression. Transl. Psychiatry. 2016;6:e981. doi: 10.1038/tp.2016.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Najjar S, et al. Neurovascular unit dysfunction and blood-brain barrier hyperpermeability contribute to schizophrenia neurobiology: a theoretical integration of clinical and experimental evidence. Front. Psychiatry. 2017;8:83. doi: 10.3389/fpsyt.2017.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rijken DC, Sakharov DV. Basic principles in thrombolysis: regulatory role of plasminogen. Thromb. Res. 2001;103(Suppl 1):S41–S49. doi: 10.1016/S0049-3848(01)00296-1. [DOI] [PubMed] [Google Scholar]
- 32.Hennekens CH. Increasing global burden of cardiovascular disease in general populations and patients with schizophrenia. J. Clin. Psychiatry. 2007;68(Suppl 4):4–7. [PubMed] [Google Scholar]
- 33.Hippisley-Cox J, Vinogradova Y, Coupland C, Parker C. Risk of malignancy in patients with schizophrenia or bipolar disorder: nested case-control study. Arch. Gen. Psychiatry. 2007;64:1368–1376. doi: 10.1001/archpsyc.64.12.1368. [DOI] [PubMed] [Google Scholar]
- 34.Hoirisch-Clapauch S, Amaral OB, Mezzasalma MA, Panizzutti R, Nardi AE. Dysfunction in the coagulation system and schizophrenia. Transl. Psychiatry. 2016;6:e704. doi: 10.1038/tp.2015.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kirkpatrick, B. & Kennedy, B. K. Accelerated aging in schizophrenia and related disorders: Future research. Schizophr. Res. in press, Available online 6 July 2017. [DOI] [PubMed]
- 36.Khan SS, et al. A null mutation in SERPINE1 protects against biological aging in humans. Sci. Adv. 2017;3:eaao1617. doi: 10.1126/sciadv.aao1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoirisch-Clapauch S, Nardi AE. Psychiatric remission with warfarin: should psychosis be addressed as plasminogen activator imbalance? Med. Hypotheses. 2013;80:137–141. doi: 10.1016/j.mehy.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Erdbruegger U, Haubitz M, Woywodt A. Circulating endothelial cells: a novel marker of endothelial damage. Clin. Chim. Acta. 2006;373:17–26. doi: 10.1016/j.cca.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 39.Aird WC. Endothelial cell heterogeneity. Cold Spring Harb. Perspect. Med. 2012;2:a006429. doi: 10.1101/cshperspect.a006429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Augustin HG, Koh GY. Organotypic vasculature: From descriptive heterogeneity to functional pathophysiology. Science. 2017;357:eaal2379. doi: 10.1126/science.aal2379. [DOI] [PubMed] [Google Scholar]
- 41.Shin CY, Kundel M, Wells DG. Rapid, activity-induced increase in tissue plasminogen activator is mediated by metabotropic glutamate receptor-dependent mRNA translation. J. Neurosci. 2004;24:9425–9433. doi: 10.1523/JNEUROSCI.2457-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lochner JE, et al. Activity-dependent release of tissue plasminogen activator from the dendritic spines of hippocampal neurons revealed by live-cell imaging. J. Neurobiol. 2006;66:564–577. doi: 10.1002/neu.20250. [DOI] [PubMed] [Google Scholar]
- 43.Zhu TX, et al. ECM-related gene expression profile in vascular smooth muscle cells from human saphenous vein and internal thoracic artery. J. Cardiothorac. Surg. 2013;8:155. doi: 10.1186/1749-8090-8-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fudge NJ, Mearow KM. Extracellular matrix-associated gene expression in adult sensory neuron populations cultured on a laminin substrate. BMC Neurosci. 2013;14:15. doi: 10.1186/1471-2202-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Suzuki Y, Nagai N, Umemura K. A review of the mechanisms of blood–brain barrier permeability by tissue-type plasminogen activator treatment for cerebral ischemia. Front. Cell. Neurosci. 2016;10:2. doi: 10.3389/fncel.2016.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hoirisch-Clapauch S, Nardi AE. Markers of low activity of tissue plasminogen activator/plasmin are prevalent in schizophrenia patients. Schizophr. Res. 2014;159:118–123. doi: 10.1016/j.schres.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 47.Lemarchand E, et al. Stressed neurons protect themselves by a tissue-type plasminogen activator-mediated EGFR-dependent mechanism. Cell Death Differ. 2016;23:123–131. doi: 10.1038/cdd.2015.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bertrand T, et al. Conformations of tissue plasminogen activator (tPA) orchestrate neuronal survival by a crosstalk between EGFR and NMDAR. Cell Death Dis. 2015;6:e1924. doi: 10.1038/cddis.2015.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deng X, et al. Positive association of phencyclidine-responsive genes, PDE4A and PLAT, with schizophrenia. Am. J. Med. Genet. B. Neuropsychiatr. Genet. 2011;156B:850–858. doi: 10.1002/ajmg.b.31233. [DOI] [PubMed] [Google Scholar]
- 50.Nicole O, et al. The proteolytic activity of tissue-plasminogen activator enhances NMDA receptor-mediated signaling. Nat. Med. 2001;7:59–64. doi: 10.1038/83358. [DOI] [PubMed] [Google Scholar]
- 51.Yang F, et al. Tissue plasminogen activator expression and barrier properties of human brain microvascular endothelial cells. Cell. Physiol. Biochem. 2011;28:631–638. doi: 10.1159/000335785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reijerkerk A, et al. Tissue-type plasminogen activator is a regulator of monocyte diapedesis through the brain endothelial barrier. J. Immunol. 2008;181:3567–3574. doi: 10.4049/jimmunol.181.5.3567. [DOI] [PubMed] [Google Scholar]
- 53.Hoirisch-Clapauch S, Nardi AE. Improvement of psychotic symptoms and the role of tissue plasminogen activator. Int. J. Mol. Sci. 2015;16:27550–27560. doi: 10.3390/ijms161126053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kolomeets, N. S., & Uranova, N. A. Reduced oligodendrocyte density in layer 5 of the prefrontal cortex in schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 1–8, Available online 23 March 2018. [DOI] [PubMed]
- 55.Richeldi L. Targeted treatment of idiopathic pulmonary fibrosis: one step at a time. Eur. Respir. J. 2016;47:1321–1323. doi: 10.1183/13993003.00389-2016. [DOI] [PubMed] [Google Scholar]
- 56.Bonniaud P, et al. Progressive transforming growth factor beta1-induced lung fibrosis is blocked by an orally active ALK5 kinase inhibitor. Am. J. Respir. Crit. Care Med. 2005;171:889–898. doi: 10.1164/rccm.200405-612OC. [DOI] [PubMed] [Google Scholar]
- 57.Tsoutsman T, et al. CCN2 plays a key role in extracellular matrix gene expression in severe hypertrophic cardiomyopathy and heart failure. J. Mol. Cell. Cardiol. 2013;62:164–178. doi: 10.1016/j.yjmcc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 58.Tan JT, et al. Connective tissue growth factor/CCN-2 is upregulated in epididymal and subcutaneous fat depots in a dietary-induced obesity model. Am. J. Physiol. Endocrinol. Metab. 2013;304:E1291–E1302. doi: 10.1152/ajpendo.00654.2012. [DOI] [PubMed] [Google Scholar]
- 59.Wang X, McLennan SV, Allen TJ, Twigg SM. Regulation of pro-inflammatory and pro-fibrotic factors by CCN2/CTGF in H9c2 cardiomyocytes. J. Cell. Commun. Signal. 2010;4:15–23. doi: 10.1007/s12079-009-0083-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Fouw NJ, et al. The cofactor role of protein S in the acceleration of whole blood clot lysis by activated protein C in vitro. Blood. 1986;67:1189–1192. [PubMed] [Google Scholar]
- 61.Long GL, Marshall A, Gardner JC, Naylor SL. Genes for human vitamin K-dependent plasma proteins C and S are located on chromosomes 2 and 3, respectively. Somat. Cell Mol. Genet. 1988;14:93–98. doi: 10.1007/BF01535052. [DOI] [PubMed] [Google Scholar]
- 62.Rezende SM, Simmonds RE, Lane DA. Coagulation, inflammation, and apoptosis: different roles for protein S and the protein S-C4b binding protein complex. Blood. 2004;103:1192–1201. doi: 10.1182/blood-2003-05-1551. [DOI] [PubMed] [Google Scholar]
- 63.Agarwal V, Talens S, Grandits AM, Blom AM. A novel interaction between complement inhibitor C4b-binding protein and plasminogen that enhances plasminogen activation. J. Biol. Chem. 2015;290:18333–18342. doi: 10.1074/jbc.M114.619494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sekar A, et al. Schizophrenia risk from complex variation of complement component 4. Nature. 2016;530:177–183. doi: 10.1038/nature16549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brown NJ. Therapeutic potential of plasminogen activator inhibitor-1 inhibitors. Ther. Adv. Cardiovasc Dis. 2010;4:315–324. doi: 10.1177/1753944710379126. [DOI] [PubMed] [Google Scholar]
- 66.Hebert M, Lesept F, Vivien D, Macrez R. The story of an exceptional serine protease, tissue-type plasminogen activator (tPA) Rev. Neurol. 2016;172:186–197. doi: 10.1016/j.neurol.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 67.Hoirisch-Clapauch S, Nardi AE. Multiple roles of tissue plasminogen activator in schizophrenia pathophysiology. Semin. Thromb. Hemost. 2013;39:950–954. doi: 10.1055/s-0033-1357505. [DOI] [PubMed] [Google Scholar]
- 68.Pang PT, et al. Cleavage of proBDNF by tPA/plasmin is essential for long-term hippocampal plasticity. Science. 2004;306:487–491. doi: 10.1126/science.1100135. [DOI] [PubMed] [Google Scholar]
- 69.Lin PY. Regulation of proteolytic cleavage of brain-derived neurotrophic factor precursor by antidepressants in human neuroblastoma cells. Neuropsychiatr. Dis. Treat. 2015;11:2529–2532. doi: 10.2147/NDT.S87743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lepeta K, Kaczmarek L. Matrix metalloproteinase-9 as a novel player in synaptic plasticity and schizophrenia. Schizophr. Bull. 2015;41:1003–1009. doi: 10.1093/schbul/sbv036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hashimoto K. Sigma-1 receptor chaperone and brain-derived neurotrophic factor: emerging links between cardiovascular disease and depression. Prog. Neurobiol. 2013;100:15–29. doi: 10.1016/j.pneurobio.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 72.Turner RJ, Sharp FR. Implications of MMP9 for blood brain barrier disruption and hemorrhagic transformation following ischemic stroke. Front. Cell. Neurosci. 2016;10:56. doi: 10.3389/fncel.2016.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ramasamy R, et al. Advanced glycation end products and RAGE: a common thread in aging, diabetes, neurodegeneration, and inflammation. Glycobiology. 2005;15:16R–28R. doi: 10.1093/glycob/cwi053. [DOI] [PubMed] [Google Scholar]
- 74.Steullet P, et al. Redox dysregulation, neuroinflammation, and NMDA receptor hypofunction: A “central hub” in schizophrenia pathophysiology? Schizophr. Res. 2016;176:41–51. doi: 10.1016/j.schres.2014.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Berretta S, Pantazopoulos H, Markota M, Brown C, Batzianouli ET. Losing the sugar coating: potential impact of perineuronal net abnormalities on interneurons in schizophrenia. Schizophr. Res. 2015;167:18–27. doi: 10.1016/j.schres.2014.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cabungcal JH, et al. Perineuronal nets protect fast-spiking interneurons against oxidative stress. Proc. Natl Acad. Sci. USA. 2013;110:9130–9135. doi: 10.1073/pnas.1300454110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Benchenane K, et al. Tissue-type plasminogen activator crosses the intact blood-brain barrier by low-density lipoprotein receptor-related protein-mediated transcytosis. Circulation. 2005;111:2241–2249. doi: 10.1161/01.CIR.0000163542.48611.A2. [DOI] [PubMed] [Google Scholar]
- 78.Winkler JL, Kedees MH, Guz Y, Teitelman G. Inhibition of connective tissue growth factor by small interfering ribonucleic acid prevents increase in extracellular matrix molecules in a rodent model of diabetic retinopathy. Mol. Vis. 2012;18:874–886. [PMC free article] [PubMed] [Google Scholar]
- 79.Brocker C, Thompson D, Matsumoto A, Nebert DW, Vasiliou V. Evolutionary divergence and functions of the human interleukin (IL) gene family. Hum. Genom. 2010;5:30–55. doi: 10.1186/1479-7364-5-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Akdis M, et al. Interleukins, from 1 to 37, and interferon-gamma: receptors, functions, and roles in diseases. J. Allergy Clin. Immunol. 2011;127:701–721. doi: 10.1016/j.jaci.2010.11.050. [DOI] [PubMed] [Google Scholar]
- 81.Kohn LA, et al. Lymphoid priming in human bone marrow begins before expression of CD10 with upregulation of L-selectin. Nat. Immunol. 2012;13:963–971. doi: 10.1038/ni.2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sorokin L. The impact of the extracellular matrix on inflammation. Nat. Rev. Immunol. 2010;10:712–723. doi: 10.1038/nri2852. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.