Abstract
Background:
The role of arthroscopic partial meniscectomy (APM) for painful degenerative meniscal tears (PDMT) is currently controversial.
To define the rate of early (1 to 5 years) conversion to total knee replacement (TKR) and their predictors after APM for PDMT in patients with knee osteoarthritis and more than 50 years of age.
Methods:
Retrospective cohort study of patients more than 50 years of age with the diagnosis of PDMT, treated by means of APM. Patients were classified in two groups: Patients that required an early (between 1 and 5 years after APM) TKR (TKR group) after its failure and patients that did not require a TKR (non-TKR group). Patient demographics, general characteristics, Kellgren & Lawrence (KL) classification, Outerbridge classification, and other characteristics were analyzed. Postoperative variables were also analyzed: pain, use of walking aids and use of intra-articular injections (hyaluronic acid or corticosteroids) at 3, 6, and 12 months of follow-up.
Results:
A total of 356 patients (356 APMs) were included. Forty-nine patients (13.7%) required an early (1.8 years on average) TKR and 307 did not. The main predictor of early TKR was the grade of the KL classification. After APM, the presence of pain and the need of walking aids also were predictors of an early TKR.
Conclusion:
In patients older than 50 years with PDMT, APM should be cautiously indicated in case of KL grade of 1 or more. Postoperative pain and prolonged need of walking aids were also predictors of an early (mean 1.8 years) TKR.
Keywords: arthroscopic partial meniscectomy, degenerative meniscal tear, failure, knee, total knee replacement
Introduction
Painful degenerative meniscal tear (PDMT) is a very common problem. In patients that do not respond to conservative treatment, arthroscopic partial meniscectomy (APM) may alleviate pain in the short-term. However, APM does not guarantee success, mainly if PDMT is associated with knee osteoarthritis (OA) (1-3). Mechanical symptoms in these patients have been claimed as the clue to indicate meniscectomy with expected efficacy, but these may be difficult to interpret and eventually the presence of a tear associated with pain may prompt surgical indication (4).
In 2014, Skedros et al reported that conventional criteria are poor in predicting which patients with PDMT should avoid APM and go straight to total knee replacement (TKR) (5). In 2015, Thorlund et al reported a systematic review and meta-analysis of benefits and harms of arthroscopic surgery for degenerative knee (6). Their findings did not support the practice of arthroscopic surgery for middle aged or older patients with knee pain with or without signs of OA.
However, this same year, Bollen et al criticized Thorlund´s report stating that: “The evidence that arthroscopic intervention for knee pain is of no benefit would seem to be thin at best, and Thorlund et al have made some sweeping conclusions that do not seem to be justified by the evidence presented (6, 7). An amalgamation of conclusions that are not based on hard science does not equate to a new evidence based conclusion”. Bailey et al stated that APM was beneficial regardless of patient body mass index (BMI), duration of symptoms, history of injury, or in the presence of early OA (8).
The main conclusions of a recently published “ESSKA Meniscus Consensus” were the following (9): 1) Surgery should not be proposed as a first line of treatment of degenerative meniscus lesions (grade A-high scientific level); 2) No arthroscopic surgery should be proposed for a degenerative meniscus lesion with advanced OA on weight bearing radiographs (grade A-high scientific level); 3) After three months with non-operative treatment and persistent pain/mechanical symptoms, APM must be proposed; 4) Surgery can be proposed earlier for patients presenting considerable mechanical symptoms (grade D-expert opinion) with normal X-rays/abnormal MRI (grade III meniscus lesion), APM may be proposed (grade B-scientific presumption); Exceptions should be discussed for young patients with considerable symptoms.
In a systematic review of the evidence for operative management of meniscal tears recently published, Monk et al found no difference between arthroscopic meniscal debridement compared with nonoperative management as a first-line treatment strategy for patients with knee pain and a degenerative meniscal tear (10). Some evidence was found to indicate that patients with resistant mechanical symptoms who initially fail nonoperative management may benefit from meniscal debridement. One study compared exercise therapy and arthroscopic partial meniscectomy for knee function in middle aged patients with degenerative meniscal tears (11). The results of this study should encourage clinicians and middle aged patients with degenerative meniscal tear and no definitive radiographic evidence of OA to consider supervised exercise therapy as a treatment option.
Therefore, the role of APM for PDMT is currentlty controversial. The purpose of this study was to define the timing and the rate of early (between 1 and 5 years after the failure of APM) conversion to TKR, as well as the predictors of conversion to TKR after APM for PDMT in the degenerative knee, in patients with more than 50 years of age.
Materials and Methods
We performed a retrospective cohort study of 356 patients more than 50 years of age with diagnosis of PDMT treated from January 2010 to December 2014 (5-year period) in a single tertiary University Hospital by means of APM. The cohort was a consecutive series. In all our patients magnetic resonance imaging (MRI) demonstrated a preoperative PDMT. The study was approved by the Ethics Committee of our Institution (number of protocol PI-2421).
Surgical indication was severe knee pain (more than 7 in a Visual Analog Scale from 0-no pain to 10-maximum pain), without a previous low-energy traumatic event, associated with a PDMT on MRI in patients that did not respond to a 3-month period of conservative treatment. This included pain-killers, NSAIDs, walking with one cane and a sedentary way life style. High-energy injuries were not included. Patients were classified in two groups: those that needed an early total knee replacement (TKR) (TKR group) after APM failure, and those that did not (non-TKR group). The indication for a TKR was pain after APM of more than 7 in the visual analog scale (VAS, no pain 0, maximum pain 10), implicating the normal realization of the activities of daily living.
The general characteristics of our patients are summarized in Table 1. The variables that were considered included patient demographics and general characteristics (age, gender, and comorbidities), Kellgren and Lawrence (KL) classification of knee OA based on radiographs, Outerbridge classification based on arthroscopy and characteristics of the PDMT treatment (12, 13). Among the outcome variables, we collected postoperative pain, postoperative use of walking aids and the need of intra-articular knee injections of hyaluronic acid or corticosteroids (if required) at 3, 6, and 12 months of follow up. Table 2 shows the main treatment characteristics.
Table 1.
General characteristics of this series (TKR = total knee replacement; n = number; w/o = without; sd = standard deviation; NA = not available)
| Variables | TKR n=49 | Non-TKR n=307 | P Value |
|---|---|---|---|
| mean±sd n(%) | mean±sd n(%) | ||
| Age | 62.8±7.1 | 61.0±7.2 | 0.082* |
| Female sex | 36(73.5%) | 188(61.2%) | 0.067** |
| Right side | 25(51.0%) | 139(45.3%) | 0.537** |
| Preoperative diagnosis | |||
| Meniscus w/o cartilage | 1(2.0%) | 17(5.6%) | 0.487** |
| Gonarthrosis or chondral degeneration | 48(98.0%) | 290(94.4%) | |
| Kellgren & Lawrence classification (grades) | 2.0±0.8 | 1.21±1.0 | 0.000† |
| 0 | 1(2.0%) | 77(25.1%) | 0.000** |
| 1 | 11(22.5%) | 86(28.0%) | |
| 2 | 19(38.8%) | 76(24.8%) | |
| 3 | 11(22.5%) | 18(5.9%) | |
| 4 | 2(4.0%) | 7(2.2%) | |
| NA | 5(10.2%) | 43(14.0%) | |
| Meniscus affected by MRI diagnosis | |||
| Medial | 33(67.4%) | 222(72.3%) | 0.903** |
| Lateral | 7(14.3%) | 40(13.0%) | |
| Both | 6(12.2%) | 40(13.0%) | |
| NA | 3(6.1%) | 5(1.7%) | |
| Cartilage diagnosis by MRI | |||
| Thinning | 4(8.2%) | 41(13.4%) | 0.068** |
| Degeneration | 9(18.3%) | 56(18.2%) | |
| Disappeared cartilage | 14(28.6%) | 34(11.1%) | |
| Advanced Degeneration + Osteophytosis | 13(26.6%) | 58(18.9%) | |
| NA | 9(18.3%) | 118(38.5%) | |
| Meniscal tear preoperative | |||
| Medial | 37(75.5%) | 202(65.8%) | 0.317** |
| Lateral | 8(16.3%) | 38(12.4%) | |
| Both | 4(8.2%) | 47(15.3%) | |
| NA | 0 | 20(6.5%) | |
| Chondral lesion | |||
| Medial | 9(18.4%) | 53(17.3%) | 0.170** |
| Lateral | 0 | 5(1.6%) | |
| Femorotibial (FT) lateral/medial | 2(4.1%) | 10(3.3%) | |
| Femoropatellar (FP) isolated | 1(2.0%) | 36(11.7%) | |
| FT+FP | 34(69.4%) | 171(55.7%) | |
| NA | 3(6.1%) | 32(10.4%) | |
Mann-Whitney test
Fisher’s exact test
t-test
P value estimated without missing values for categorical variables.
Table 2.
Treatment characteristics of degenerative meniscal tears (TKR = total knee replacement; n = number; w/o = without; debridem = debridement; NA = not available)
| Variables | TKR n=49 | Non-TKR n=307 | P Value |
|---|---|---|---|
| mean±sd n(%) | mean±sd n(%) | ||
| Medial compartment, Outerbridge grade: | 2.9±1.5 | 2.4±1.5 | 0.014* |
| 0 | 8(16.3%) | 71(23.1%) | 0.010** |
| I | 2(4.1%) | 6(1.9%) | |
| II | 5(10.2%) | 47(15.3%) | |
| III | 6(12.3%) | 82(26.7%) | |
| IV | 27(55.1%) | 96(31.3%) | |
| NA | 1(2.0%) | 5(1.7%) | |
| Lateral compartment, Outerbridge grade: | 1.2±1.6 | 0.8±1.4 | 0.090* |
| 0 | 29(59.2%) | 217(70.7%) | 0.270** |
| I | 0 | 5(1.6%) | |
| II | 6(12.2%) | 23(7.5%) | |
| III | 5(10.2%) | 31(10.1%) | |
| IV | 8(16.4%) | 27(8.8%) | |
| NA | 1(2.0%) | 4(1.3%) | |
| Femoropatellar compartment, Outerbridge grade: | 2.4±1.6 | 2.1±1.6 | 0.211* |
| 0 | 12(24.5%) | 94(30.6%) | 0.561** |
| I | 0 | 8(2.6%) | |
| II | 10(20.4%) | 54(17.6%) | |
| III | 9(18.4%) | 70(22.8%) | |
| IV | 17(34.7%) | 76(24.8%) | |
| NA | 1(2.0%) | 4(1.3%) | |
| Other techniques in cartilage | |||
| None | 46(93.9%) | 276(89.9%) | 0.624** |
| Perforation / microfractures | 1(2.0%) | 12(3.9%) | |
| Free body extraction | 1(2.0%) | 3(1.0%) | |
| Regularization + Perforation + Debridem. | 1(2.0%) | 16(5.2%) | |
| Other techniques in soft tissue | |||
| None | 45(91.9%) | 275(89.6%) | 0.760** |
| Meniscal cyst | 0 | 2(0.7%) | |
| Synovectomy | 2(4.1%) | 21(6.8%) | |
| Debridement with lateral release | 1(2.0%) | 5(1.6%) | |
| Suture | 1(2.0%) | 4(1.3%) | |
Mann-Whitnet test
Fisher’s exact test
P value estimated without missing values for categorical variables.
The statistical methods analysis included parametric and non-parametric statistics (Fisher test, t-test, Mann-Whitney test) to compare the variables with a confidence level of 95%. A logistic regression was modelled to identify the risk factors for TKR. The independent variables included severity (KL classification), postoperative pain at the established intervals of the follow-up (yes/no), use of walking aids in the follow-up (yes/no), intra-articular injections in the FU, sex, and age. The statistical analysis was made using STATA software (StataCorp.2009 College Station, TX: StataCorp LP).
Results
A total of 356 patients were included in this retrospective study; of these, 49 (13.7%) required TKR and 307 did not require TKR in the follow-up period (24 to 60 months). The mean time of follow up of the TKR group was of 3.6±1.5 years while for the not-TKR group it was of 2.5±1.6 years (P<0.01). The mean time from index surgery (APM) to TKR was 1.8±1.3 years.
A significantly higher percentage of patients with higher grades in the KL classification was found in the TKR group [Table 1] that also showed 24% more of Outerbridge grade in the medial compartment than the not-TKR group [Table 2]. The rest of general population characteristics and PDMT treatment characteristics showed no statistical differences. Both groups were considered comparable [Table 1].
Outcome variables were significantly different between the TRK group and the non-TKR group [Table 3]. In the TKR group, we identified significantly more pain at 3 months of follow-up (94% vs. 60%, P=0.000); more pain at 6 months follow-up (92% vs. 53%, P=0.000) and more frequent need of walking aids (26% vs. 6%, P=0.000); at 12 months of follow-up, we found more pain (92% vs. 40%, P=0.000) and more frequent need of walking aids (16% vs. 2%, P=0.000). There were more indications of knee intra-articular injections of any type (hyaluronic acid or corticosteroids) in the TKR group, with 44.9% vs. 18.9% (P=0.000) at 6 months follow-up, and 34.6% vs. 14.3% (P=0.002) at 12 months follow-up. Also, at 6 and 12 months follow-up, significantly more patients required other forms of treatment including analgesics and physiotherapy, as seen in Table 3.
Table 3.
Outcome variables and follow-up characteristics (TKR = total knee replacement). NA = not available
| Variables | TKR n=49 | Non-TKR n=307 | P Value |
|---|---|---|---|
| n(%) | n(%) | ||
| 3 months postoperative | |||
| Pain (Yes) | 46(93.9%) | 184(60%) | 0.000** |
| 6 months postoperative | |||
| Pain (Yes) | 45(91.8%) | 163(53.1%) | 0.000** |
| Walking aids (Yes) | 13(26.5%) | 19(6.2%) | 0.000** |
| Intra-articular injection | 0.000** | ||
| None | 27(55.1%) | 249(81.1%) | 0.001** |
| Hyaluronic acid | 13(26.5%) | 30(9.8%) | |
| Corticosteroids | 9(18.4%) | 28(9.1%) | |
| Other treatments (Yes) | 41(61.6%) | 189(61.6%) | |
| 12 months postoperative. | |||
| Pain (Yes) | 45(91.8%) | 122(39.7%) | 0.000** |
| Crutches or walking aids (Yes) | 8(16.3%) | 6(2%) | 0.000** |
| Intra-articular injections | |||
| None | 32(65.3%) | 263(85.7%) | 0.002** |
| Hyaluronic acid | 11(22.4%) | 30(9.7%) | |
| Corticosteroids | 6(12.2%) | 14(4.6%) | |
| Other treatments | |||
| No | 27(55.1%) | 206(67.1%) | 0.026** |
| Rehabilitation | 7(14.3%) | 56(18.3%) | |
| Analgesics intake | 7(14.3%) | 32(10.4%) | |
| Rehabilitation + Analgesics | 7(14.3%) | 12(3.9%) | |
| NA | 1(2.0%) | 1(0.3%) | |
Fisher’s exact test
Table 4 shows the significant logistic regression models of the variables at 6 and 12 months that were associated with undergoing TKR surgery. Higher grades of radiographic KL index and also the persistence of pain and walking aids at 6 and 12 months of follow-up increased the risk of receiving TKR. Figure 1 displays the probabilities of TKR with the presence of pain and walking aids at 6 and 12 months of follow-up for a given KL index.
Table 4.
Variables associated with total knee replacement (TKR). FU = follow-up; CI = confidence interval
| Variable | 3 months FU | 6 months FU | 12 months FU | |||
|---|---|---|---|---|---|---|
| TKR Odd Ratio | CI, 95% | TKR Odd Ratio | CI, 95% | TKR Odd Ratio | CI, 95% | |
| Age | 1.0ns | 0.9-1.1 | 1.0ns | 0.9-1.0 | 1.0ns | 0.9-1.0 |
| Female sex | 1.3ns | 0.6-2.7 | 1.2ns | 0.6-2.5 | 1.3ns | 0.6-2.8 |
| Kellgren & Lawrence classification | ||||||
| 0 | 1 | 1 | 1 | |||
| 1 | 8.1* | 1.0-65.4 | 8.3* | 1.0-68.7 | 11.2* | 1.2-102.9 |
| 2 | 17.2** | 2.2-134.8 | 15.3* | 1.9-122.1 | 20.7** | 2.3-186.7 |
| 3+ | 14.5* | 1.8-113.9 | 13.6* | 1.6-109.3 | 20.9** | 2.3-190.2 |
| Pain (Yes) | 9.5*** | 2.8-31.8 | 6.2** | 20.3-18.8 | 13.8*** | 4.6-41.6 |
| Walking aids (Yes) | - | - | 3.1* | 1.3-7.5 | 8.6** | 2.1-34.6 |
| Intra-articular injection | - | - | ||||
| None | 1 | 1 | ||||
| Hyaluronic acid | 1.4ns | 0.6-3.3 | 0.6ns | 0.2-1.5 | ||
| Corticosteroids | 1.4ns | 0.5-3.6 | 0.9ns | 0.3-3.1 | ||
| Model adjust(ps.R2) | 0.169*** | 0.206*** | 0.275*** | |||
p<0.05;
p<0.01;
p<0.001;ns: Not significant
Figure 1.
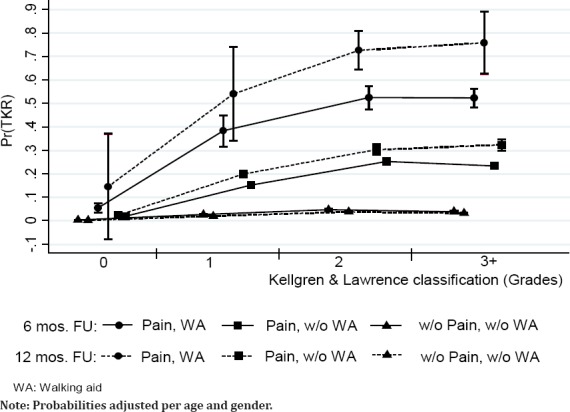
Pain, walking aid (WA) and severity as predictors (Pr) of total knee replacement (TKR) at 3, 6 and 12 months of follow-up (FU). W/o = without; mos = months.
Discussion
Taking into account the current controversy on the role of APM for PDMT of the knee, we tried to define the rate of early conversion to TKR and its predictors after APM for PDMT in the presence of knee OA in patients with more than 50 years of age. We performed a retrospective cohort study of patients with more than 50 years of age with the diagnosis of PDMT (confirmed on MRI) treated from 2010 to 2014 by means of APM and compared the baseline and the outcome variables in patients that were classified in two groups: those that required a TKR (TKR group) and those that did not (non-TKR group). Our results confirm that higher degrees of KL index in preoperative radiographs increase the risk of early TKR (less than 2 years after arthroscopic partial meniscectomy), and that postoperative persistent pain and walking aids requirements also lead to early TKR.
Our results are clinically relevant as the experience of a large tertiary teaching hospital, where 49 out of 356 patients over 50 years of age undergoing arthroscopic partial meniscectomy did not experience clinical benefit but on the contrary, required further surgical treatment 2 years after, namely TKR (13.7%). This fact further reinforces the questioning of patient selection and patient benefit of this technique in case of MRI diagnosed partial degenerative meniscal tears in symptomatic patients not responding to conservative treatment.
Our study has a number of limitations. First of all, this is a retrospective study and not a prospective one. Furthermore, patient selection was performed based on the age, the diagnosis and the performed technique. The allocation of mechanical symptoms as a precise indication for APM is unclear. A recent report found that satisfaction after arthroscopy was significantly lower among those with preoperative mechanical symptoms (14). Therefore, we did not use mechanical symptoms, frequently present, as a criteria for patient selection. Although selection bias is not fully cleared due to population attending the Hospital, time from symptoms to surgery, or other aspects related to the Hospital setting, we incorporated all patients in our Unit that truly represents population over 50 in our area. Another limitation is the comparison of both groups, selected upon the outcome (early TKR after APM) but with different mean follow-up (3.6±1.5 years in the TKR group, and 2.5±1.6 in the not-TKR group) that was judged as not clinically relevant. Both groups were found basically comparable except that a higher percentage of patients with higher grades of OA (particularly grades 2 and 3 in the KL grading) was found in the TKR group. However, these patients were offered APM due to preserved function at the time of treatment, and the poor outcome poor enables us to conclude on the risk factors and the recommendation of cautious APM indication.
Several randomized controlled trials (RCT) of arthroscopy on middle aged patients with knee pain with or without OA have reported no beneficial effect of surgery over placebo surgery or physiotherapy, although very seldom the final TKR requirements are studied in RCTs due to insufficient follow-up (15-19). This is a major benefit of a retrospective study such as the current one.
In 2012 Englund et al stated that PDMT must be initially treated conservatively before deciding an APM, and also that patients with mechanical symptoms (painful catching or locking) may need surgical treatment (20). In a subgroup of patients, APM may alleviate pain and other symptoms potentially caused by the meniscal tear.
In a report of level I of evidence published in 2013, Herrlin et al found that exercise therapy plus APM was not superior to exercise therapy alone (21). However, one third of patients of the exercise group did not improve. Such patients improved after APM at the same level as the rest.
A systematic review and meta-analysis published in 2014 by Khan et al found a moderate degree of evidence suggesting that there is no benefit from APM for PDMT in comparison with non-operative or sham treatments in middle-aged patients with mild or no concomitant OA (22). An intent of non-operative management should be the first line treatment for such patients.
In 2014, Skedros et al reported a 12% rate of conversion to TKR in patients younger than 65 years, compared to 36% in patients older than 65 years (5). The overall rate of conversion to TKR was 26%. In our series of patients older than 50 years the rate of early (1.8 years on average) conversion to TKR has been 13.7% (49/356) at 2 years, in the same range as reported.
The systematic review and meta-analysis of benefits and harms of APM for PDMT reported in 2015 by Thorlund et al did not support the practice of arthroscopic surgery for middle aged or older patients with knee pain with or without signs of OA (6).
However, this same year, Bollen stated that “the evidence that arthroscopic intervention for knee pain is of no benefit would seem to be thin at best, and Thorlund et al have made some sweeping conclusions that do not seem to be justified by the evidence presented” (5, 7).
Another systematic review published in 2015 by Petersen et al demonstrated that for most PDMT surgical and non-surgical treatment seem to have the same value (23). Of six assays, only one showed less pain after APM. However, in the rest of assays it was evident that APM failed in some patients. Petersen et al stated that such patients could benefit from APM.
In a randomized, patient- and outcome assessor-blinded, sham surgery-controlled, multicenter trial published in 2016 by Sihvonen et al, APM did not add benefit over sham surgery to relieve knee catching or occasional locking (24). Sihvonen et al questioned whether mechanical symptoms were caused by a PDM. In fact, they prompted caution in using patients’ self-report of these symptoms as an indication for APM, which lead us to avoid this symptom among the selection criteria.
In a cohort study or case series (level IV of evidence) reported in 2016 by Demange et al, 71 patients with “fatigue meniscal tear” were analyzed (25). Inclusion criteria were spontaneous abrupt onset knee pain, minor or no trauma, no radiographic or MRI OA, no bone edema, preoperative MRI image of medial meniscus tear, and arthroscopic evaluation demonstrating radial or vertical flap tear in the body to posterior horn junction of the medial meniscus. The mean follow-up was 4.2 years. There were 59 (83.1 %) good and excellent results, and 12 (16.9 %) poor results. These 12 patients demanded further treatment because of persistent pain, with three of the patients developing subchondral bone fracture. All patient complaints and poor outcomes were identified in the initial six months after surgery. The findings of Demange et al indicated that patients with “fatigue meniscal tear” benefited from APM, with only 16.9 % reporting unfavorable results (24).
In an observational study reported in 2016, Sihvonen et al tried to determine the value of using patients’ preoperative self-reports of mechanical symptoms as a justification surgery in patients with degenerative meniscus tear (18). Their data contradicted the idea of using patients’ self-report of mechanical symptoms as a justification for performing APM on patients with PDMT.
It has been recently reported by Roemer et al that partial meniscectomy for degenerative meniscal tear is strongly associated with incident OA within 1 year and with increased risk of worsening cartilage damage (25).
In our study, 13.7% of patients required an early TKR (TKR group) in the follow-up period (1.8 years on average) and 86.3% did not require a TRK (non-TKR group). Both groups were basically comparable. However, a higher percentage of patients with higher grades of OA (KL classification) was found in the non-TKR group, The mean time of follow-up in the TKR group was of 3.6±1.5 while for the non-TKR group it was of 2.5±1.6. The rest of general characteristics and meniscal tear treatment characteristics showed no statistical differences.
In a systematic review of the evidence for operative management of meniscal tears recently published, Monk et al found no difference between arthroscopic meniscal debridement compared with nonoperative management as a first-line treatment strategy for patients with knee pain and a degenerative meniscal tear (10). Some evidence was found to indicate that patients with resistant mechanical symptoms who initially fail nonoperative management may benefit from meniscal debridement, but studies are lacking in the comparison of meniscal repair with meniscectomy or nonoperative management (10).
In conclusion, in our study the rate of early conversion (1.8 years on average) to TKR after APM for PDMT in patients with more than 50 years and OA was 13.7%. Factors associated with the need of an early TKR after APM for DSMT were the following: The severity of preoperative OA (KL classification), that increased the risk of TKR from 8 times (KL grade 1) to 14.5 times (KL more than grade 3) compared to those with grade cero before APM. The associations get stronger at 12 months, with an odd ratio from 11 for grade 1 to 21 for more than grade 3. The presence of postoperative pain was strongly associated to TKR with an odd ratio of 9.5, 6.2, and 13.8 at 3, 6 and 12 months, respectively. The need of walking aids was also strongly associated with TKR, triplicating the risk at 6 months and multiplying the risk by eight at 12 months follow-up. Postoperative knee intra-articular injections (hyaluronic acid or corticosteroids) seemed not to be a risk factor for TKR.
References
- 1.Alipour M, Tabari M. Effect of dexmedetomidine on postoperative pain in knee arthroscopic surgery;a randomized controlled clinical trial. Arch Bone Jt Surg. 2014;2(1):e52. [PMC free article] [PubMed] [Google Scholar]
- 2.Nahravani M, Tekye SM, Alipour M, Makhmalbaf H, Aghaee MA. Analgesia following arthroscopy–a comparison of intra-articular bupivacaine and/or midazolam and or fentanyl. Arch Bone Jt Surg. 2017;5(1):e28. [PMC free article] [PubMed] [Google Scholar]
- 3.Howell R, Kumar NS, Patel N, Tom J. Degenerative meniscus:pathogenesis, diagnosis, and treatment options. World J Orthop. 2014;5(5):597–602. doi: 10.5312/wjo.v5.i5.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675–84. doi: 10.1056/NEJMoa1301408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skedros JG, Knight AN, Thomas SC, Paluso AM, Bertin KC. Dilemma of high rate of conversion from knee arthroscopy to total knee arthroplasty. Am J Orthop (Belle Mead NJ) 2014;43(7):E153–8. [PubMed] [Google Scholar]
- 6.Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee:systematic review and meta-analysis of benefits and harms. Br J Sports Med. 2015;49(19):1229–35. doi: 10.1136/bjsports-2015-h2747rep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bollen SR. Is arthroscopy of the knee completely useless?Meta-analysis--a reviewer's nightmare. Bone Joint J. 2015;97-B(12):1591–2. doi: 10.1302/0301-620X.97B12.37456. [DOI] [PubMed] [Google Scholar]
- 8.Bailey O, Gronkowski K, Leach WJ. Effect of body mass index and osteoarthritis on outcomes following arthroscopic meniscectomy:a prospective nationwide study. Knee. 2015;22(2):95–9. doi: 10.1016/j.knee.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Meniscus consensus. ESSKA. 2017 Available at:URL: www.esska/org/education/projects .
- 10.Monk P, Garfjeld Roberts P, Palmer AJ, Bayliss L, Mafi R, Beard D, et al. The urgent need for evidence in arthroscopic meniscal surgery. Am J Sports Med. 2016;45(4):965–73. doi: 10.1177/0363546516650180. [DOI] [PubMed] [Google Scholar]
- 11.Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients:randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740. doi: 10.1136/bmj.i3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–7. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 14.Sihvonen R, Englund M, Turkiewicz A, Järvinen TL. Mechanical symptoms as an indication for knee arthroscopy in patients with degenerative meniscus tear:a prospective cohort study. Osteoarthritis Cartilage. 2016;24(8):1367–75. doi: 10.1016/j.joca.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Moseley JB, O'Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347(2):81–8. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 16.Herrlin S, Hållander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears:a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):393–401. doi: 10.1007/s00167-006-0243-2. [DOI] [PubMed] [Google Scholar]
- 17.Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359(11):1097–107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
- 18.Sihvonen R, Englund M, Turkiewicz A, Järvinen TL Finnish Degenerative Meniscal Lesion Study Group. Mechanical symptoms and arthroscopic partial meniscectomy in patients with degenerative meniscus tear:a secondary analysis of a randomized trial. Ann Intern Med. 2016;164(7):449–55. doi: 10.7326/M15-0899. [DOI] [PubMed] [Google Scholar]
- 19.Yim JH, Seon JK, Song EK, Choi JI, Kim MC, Lee KB, et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41(7):1565–70. doi: 10.1177/0363546513488518. [DOI] [PubMed] [Google Scholar]
- 20.Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A. Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol. 2012;8(7):412–9. doi: 10.1038/nrrheum.2012.69. [DOI] [PubMed] [Google Scholar]
- 21.Herrlin SV, Wange PO, Lapidus G, Hållander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non traumatic, degenerative medial meniscal tears?A five year follow-up. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):358–64. doi: 10.1007/s00167-012-1960-3. [DOI] [PubMed] [Google Scholar]
- 22.Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M. Arthroscopic surgery for degenerative tears of the meniscus:a systematic review and meta-analysis. CMAJ. 2014;186(14):1057–64. doi: 10.1503/cmaj.140433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petersen W, Achtnich A, Lattermann C, Kopf S. The treatment of non-traumatic meniscus lesions. Dtsch Arztebl Int. 2015;112(42):705–13. doi: 10.3238/arztebl.2015.0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Demange MK, Gobbi RG, Camanho GL. “Fatigue meniscal tears”:a description of the lesion and the results of arthroscopic partial meniscectomy. Int Orthop. 2016;40(2):399–405. doi: 10.1007/s00264-015-3010-5. [DOI] [PubMed] [Google Scholar]
- 25.Roemer FW, Kwoh CK, Hannon MJ, Hunter DJ, Eckstein F, Grago J, et al. Partial meniscectomy is associated with increased risk of incident radiographic osteoarthritis and worsening cartilage damage in the following year. Eur Radiol. 2017;27(1):404–13. doi: 10.1007/s00330-016-4361-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


