Abstract
The non-recurrent inferior laryngeal nerve (NRLN) represents a risk factor for nerve injury during thyroid surgery. The aim of this study is to investigate the traveling patterns of NRLNs and its relationships to inferior thyroid arteries (ITAs). We had 11 patients showing NRLNs on the right side who underwent thyroidectomies. The NRLNs were classified into four different types, according to the traveling patterns. We evaluated the anatomical position of the ITA as follows: (1) three types according to the joint location with the thyroid gland; and (2) three types according to the level of the retro-esophageal subclavian artery (RSA). The traveling patterns of NRLN could be classified into four types, descending, vertical, ascending, and V-shaped. ITA was joined variably with the thyroid gland on the superior, middle, and inferior positions. The levels of the RSA were also located at different positions, the first thoracic vertebra, the second vertebra, and the third vertebra. During thyroid surgery, the surgeon must be aware of the existence of anatomical variations of NRLNs and ITAs. The anatomy of the NRLN and the ITA are frequently irregular, and there is no correlation between the traveling pattern of NRLN and the level of the RSA.
Keywords: Non-recurrent laryngeal nerve, Inferior thyroid artery
Introduction
It is very important to understand the relationship between the inferior thyroid arteries (ITA) around the thyroid gland and the recurrent laryngeal nerve (RLN) during neck surgery, especially thyroid surgery. A paralysis of the RLN is one of the major complications of thyroid surgery and results in voice and swallowing problems. To decrease these complications, meticulous surgical technique is necessary and the ITA and RLN should always be identified during a thyroidectomy [1–3]. Nonetheless, vocal fold paralysis occurs unintentionally because of their anatomical variation. A major variation is a non-recurrent laryngeal nerve (NRLN). The right RLN branches off from the vagus nerve at the right subclavian artery and rises up along the tracheoesophageal groove. The right subclavian artery infrequently arises directly from the aortic arch and the inferior laryngeal nerve enters into the larynx directly, not recurrently. Dysphagia and foreign body sensations during swallowing may be noticed in patients with NRLN. However, patients do not display symptoms in most cases.
The ITA supplies the thyroid gland and typically arises from the thyrocervical trunk. Occasionally, ITA can arise from the aortic arch and subclavian arteries. The thyrocervical trunk arises from the upper border of the subclavian artery and divides into three branches: the inferior thyroid, suprascapular, and transverse cervical arteries. The ITA passes upward in front of the longus colli muscle, then turns medially behind the carotid sheath and vagus nerve. Afterward, it was divided into two branches, which supply the pharynx, esophagus, trachea, and thyroid glands. The ITA has various relationships with the RLN. The RLN passes anterior to the ITA on the right side and posterior to the ITA on the left side, in most cases. Occasionally, the RLN lies in between the branches of the ITA [4, 5].
The NRLN has various traveling patterns. Two types of NRLN, which are based on the inferior thyroid artery (ITA), have been described by Cagnol et al. [6] and Hong et al. [7]. and are classified into four different types, according to their traveling patterns. (1) Descending type: the nerve is descending from the vagus nerve trunk. (2) Vertical type: the nerve runs vertically to the cricothyroid joint. (3) Ascending type: the nerve runs upward to the cricothyroid joint. (4) V-shaped type: the nerve is made downward and runs upward to the cricothyroid joint.
In our study, we evaluated the relationship between the traveling pattern of NRLN and ITA courses. We report 11 cases of NRLNs and discuss the traveling patterns of NRLNs and their relationships to ITAs.
Materials and Methods
A retrospective review of 16 NRLN cases in thyroidectomized patients was performed over a 16-year period from January 1997 to August 2014. The NRLNs were classified into four different types according to the traveling patterns observed. (Fig. 1) Among 11 cases of 16 patients, we have investigated the traveling patterns of the NRLN and its relationship to ITA and retro-esophageal right subclavian arteries (RSAs). RSAs were identified in preoperation CT results. The course of ITAs was identified using the operative photos or drawings.
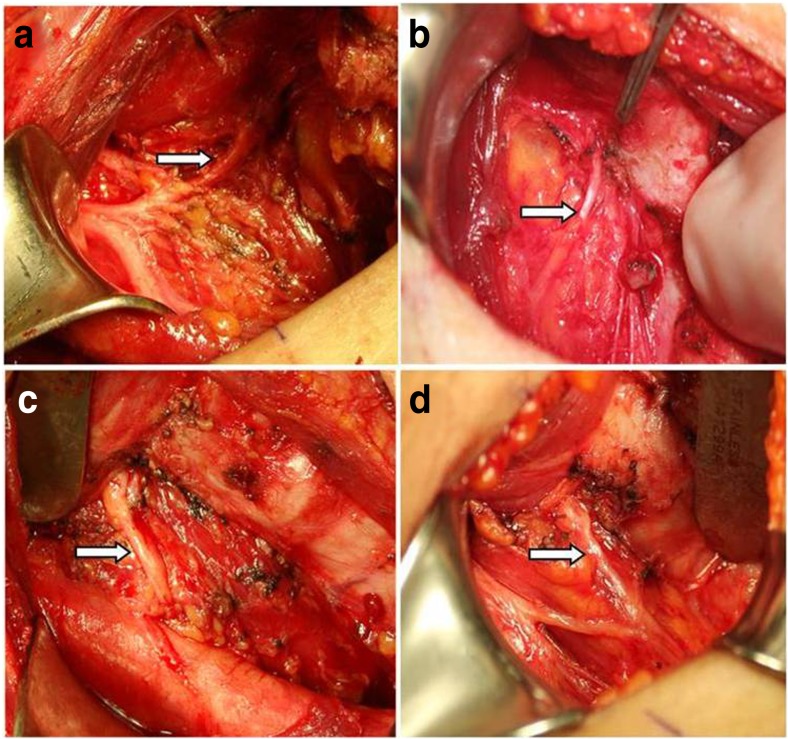
Fig. 1.
Four patterns of non-recurrent laryngeal nerves (arrows) arising directly from the vagus nerve and entering the larynx; descending (a), vertical (b), ascending (c), and V-shaped (d) patterns
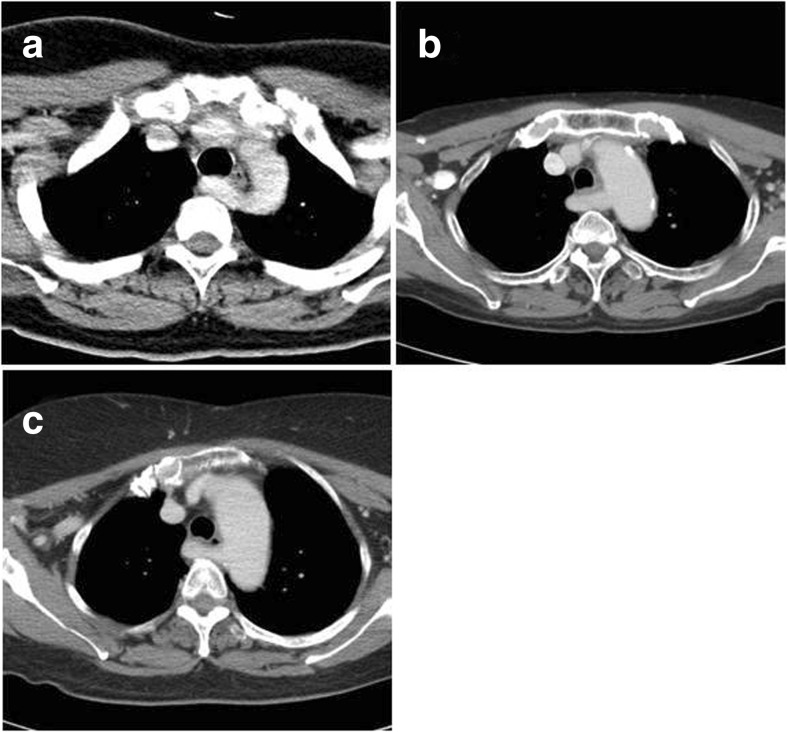
We have evaluated the anatomical position of the ITA. Firstly, ITAs were classified into three types, according to their location in the tracheoesophageal groove. Three types are those in the superior 1/3, middle 1/3, or the inferior 1/3 of the thyroid gland (Fig. 2). Secondly, from preoperative CT results, the levels of RSA were classified as levels of the first, second, or third thoracic vertebral body (Fig. 3) because the level of RSA may affect the level of ITAs.
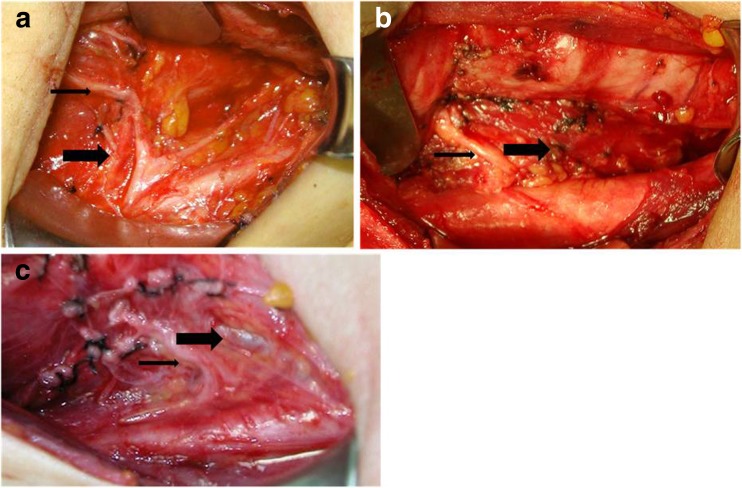
Fig. 2.
Three patterns of inferior thyroid arteries according to a joint location with the thyroid gland (thick arrows); superior (a), middle (b), and inferior (c). Non-recurrent laryngeal nerves RLNs are all ascending types (thin arrow)
Fig. 3.
Axial preoperation CT images. Thoracic vertebral level according to the level of the retro-esophageal right subclavian artery; first (a), second (b), third (c)
Results
Among the patients who underwent total thyroidectomy or right hemithyroidectomy over a 16-year period, we identified 16 cases of NRLNs. They are all right-side cases. There were 14 women and 2 men, with a mean age of 52.4 years (range, 34–76 years). Nine patients received a total thyroidectomy with central neck dissection, and seven patients received a right hemithyroidectomy. Histologically, 13 cases were papillary carcinoma and three cases goiter and follicular adenoma (Table 1). Upon retrospective chart review, four patients (25%) complained of mild dysphagia, but there were no other clinical symptoms observed, such as dysphonia. NRLNs were identified and classified as descending, vertical, ascending, and descending-ascending (V-shaped) types (Fig.1). We have identified ITA using operation pictures or drawings. RRSA was identified upon preoperation CT findings in all cases.
Table 1.
Summary of patients with non-recurrent laryngeal nerves
| Age/sex Op. name | Pathology | Types | TG level of ITA | Vertebral level of SA |
|---|---|---|---|---|
| 1. 51/F Rt. lobectomy | Goiter | Ascending | Upper | T2 |
| 2. 53/F TT + CND | PTC | Descending | Middle | T3 |
| 3. 40/M Rt. lobectomy | PTC | Vertical | Middle | T1 |
| 4. 57/F TT + CND | PTC | Descending | Upper | T1 |
| 5. 70/F TT + CND | PTC | V-shaped | Lower | T2 |
| 6. 53/F TT + CND | PTC | Vertical | Middle | T3 |
| 7. 64/F Rt. lobectomy | Adenoma | Ascending | Middle | T1 |
| 8. 76/F Rt. lobectomy | PTC | Ascending | Upper | T2 |
| 9. 52/F TT + CND | PTC | V-shaped | Middle | T2 |
| 10. 47/F TT + CND | PTC | Vertical | Upper | T1 |
| 11. 48/F Rt. lobectomy | PTC | Ascending | Lower | T3 |
In terms of the course of ITAs, they were joined with the thyroid gland in the superior one third in four cases (36%), middle one third in five cases (45%), and the inferior one third in two cases (18%). There was no consistency between the traveling pattern of the NRLN and the level at which the ITA joined with the thyroid gland. The level of RRSA, which is represented by the level of the ITA, was the first thoracic vertebra in four cases (36%), the second vertebra in four cases (36%), and third vertebra in three cases (27%). There was also no correlation observed between the traveling pattern of the NRLN and the level of the RRSA.
Discussion
Embryologically, both RLNs supply the sixth brachial arches. These nerves pass beneath the sixth aortic arch and ascend to the larynx with the descent of the heart. On the right side, the distal portion of the sixth aortic arch and the fifth aortic arch disappears, and the RLN moves up to lie beneath the fourth arch. However, the right fourth aortic arch and proximal right dorsal aorta are occasionally obliterated, and the origin of the subclavian artery becomes anomalous. This subclavian artery reaches the right side by crossing the midline behind the esophagus and locates between the esophagus and the trachea [1, 2, 8]. This anomalous subclavian artery allows the inferior laryngeal nerve to form in a non-recurrent pattern. As such, we can say that the NRLN originates from abnormal embryological development.
An NRLN was first described by Stedman [9] in 1823, who noted a right inferior laryngeal nerve in a non-recurrent situation accompanying the right subclavian artery arising from the aortic arch to the left of the left subclavian artery. The overall reported incidence of NRLN is around 0.6 to 0.8% on the right side, and 0.04% on the left side [1, 8, 10]. The incidence of surgically identified NRLNs in this study is 0.86%, similar to that of other studies. All 16 cases of NRLN were right sided. NRLN increases the risk of injury during thyroid surgery and patients acquired persistent vocal cord palsy after surgery in 12.9% of all thyroidectomized patients with NRLN, high compared to the 0.2–2% incidence rate observed with normal recurrent nerve anatomy [9, 11, 12]. NRLN is not only at risk of being damaged during thyroidectomy but also other surgical procedures, such as neck dissection, parathyroidectomy, and carotid endarterectomy [11]. Postoperative vocal paralysis is increased more than tenfold if NRLN evaluation is not adequately performed.
If a surgeon identifies NRLN preoperation, the surgeon can approach NRLN with the appropriate method. Preoperation neck CT is a very effective tool for identifying RSA associated with such NRLN. A neck CT can be performed as part of the preoperative evaluation in patients with thyroid surgery and parathyroid surgery for identifying the extent of disease and the state of the surrounding structures. Sometimes, radiology reports can miss vascular anomalies because of overlooking mediastinum evaluation [13]. Therefore, surgeons should be particularly thorough with their evaluation of the mediastinum in preoperation neck CTs. The NRLN has various traveling patterns. Two types of NRLN, which are based on the inferior thyroid artery (ITA), have been described by Cagnol et al. [6] as follows. The high type of NRLNs (type I) arises perpendicularly from the vagal nerve trunk to join the laryngotracheal junction transversally via a short route, and the low type of NRLNs (type II) originates from the vagal nerve trunk and follows a supero-external concavity before accompanying the ITA. However, Hong et al. [7] reported four types of NRLN because the anatomy of the NRLN and the ITA are frequently irregular. The four types include the descending, vertical, ascending, and V-shaped types.
Normally, RLN originates from the vagus nerve and, on the right, surrounds the right subclavian artery, and on the left, surrounds the aortic arch. Before reaching its point of penetration in the larynx, the RLN ascends in the neck in the tracheoesophageal groove in most cases. During this ascending passage, the RLN will cross the ITA. The ITA supplies blood to the thyroid gland and is located near the recurrent nerve, which controls the larynx. The inferior laryngeal nerve is highly susceptible to damage, especially during thyroid or spine surgery around the ITA. On the right side, in most cases, the recurrent laryngeal nerve (RLN) is found between the branches of the ITA, followed by, in decreasing order of frequency, positions anterior and posterior to the artery. On the left, the RLN was also placed more frequently between the branches of the ITA, followed by, in decreasing order of frequency, positions posterior and anterior to the ITA [14]. Injury to the RLN is one of the most frequent and important causes of morbidity in thyroidectomies. The knowledge of its passage and of its anatomical relationships is therefore essential to best avoid such injury.
In this study, we have evaluated the relationship between the traveling pattern of the NRLN and ITA courses. As shown above, ITA is not useful for landmark for the accurate identification of the NRLN due to its various anatomical positions. Therefore, classification of NRLN, which is based on the ITA, is not of assistance during surgery.
In conclusion, prior to surgery, surgeons should investigate the existence of NRLNs by CT scan. During surgery, surgeons must be aware of the existence of anatomical variations of NRLNs and ITAs. Meticulous dissection of the thyroid gland and thorough identification of the NRLN should always be made to prevent vocal paralysis.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Watanabe A, Kawabori S, Osanai H, Taniguchi M, Hosokawa M. Preoperative computed tomography diagnosis of on-recurrent inferior laryngeal nerve. Laryngoscope. 2001;111:1756–1759. doi: 10.1097/00005537-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Defechereux T, Albert V, Alexandre J, Bonnet P, Hamoir E, Meurisse M. The inferior nonrecurrent laryngeal nerve: a major surgical risk during throidectomy. Acta Chir Belg. 2000;100:62–67. [PubMed] [Google Scholar]
- 3.Riddell VH. Injury to recurrent laryngeal nerves during thyroidectomy; a comparison between the results of identification and non-identification in 1022 nerves exposed to risk. Lancet. 1956;2:638–641. doi: 10.1016/S0140-6736(56)92333-9. [DOI] [PubMed] [Google Scholar]
- 4.Chadrakala SP, Mamatha Y, Thejaswini KO. Variations in the origin of inferior thyroid artery and relation of the artery with recurrent laryngeal nerves. Nat J Clin Anatomy. 2013;2:11–15. [Google Scholar]
- 5.Campos BA, Henriques PRF. Relation between the recurrent laryngeal nerve and the inferior thyroid artery: a study in corpses. Rev Hosp Clin Fac Med. 2000;55:195–200. doi: 10.1590/S0041-87812000000600001. [DOI] [PubMed] [Google Scholar]
- 6.Cagnol G, Santini J. Demard anatomy of the recurrent nerve. Descriptive anatomy, trajectory and relationships, variations. Acta Otolaryngol Belg. 1987;41:821–827. [PubMed] [Google Scholar]
- 7.Hong KH, Park HT, Yang YS. Characteristic travelling patterns of non-recurrent laryngeal nerves. J Laryngol Otol. 2014;128:534–539. doi: 10.1017/S0022215114000978. [DOI] [PubMed] [Google Scholar]
- 8.Toniato A, Mazzarotto R, Piotto A, Bernante P, Pagetta C, Pelizzo MR. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Sugr. 2004;28:659–661. doi: 10.1007/s00268-004-7197-7. [DOI] [PubMed] [Google Scholar]
- 9.Stedman GW. A singular distribution of some of the nerves and arteries of the neck and the thorax. Edin Med Sugr J. 1823;19:564–565. [PMC free article] [PubMed] [Google Scholar]
- 10.De Luca L, Bergman JJ, Tytgat GN, Fockens PE. EUS imaging of the arteria lusoria: case series and review. Gastrointest Endosc. 2000;52:670–673. doi: 10.1067/mge.2000.109808. [DOI] [PubMed] [Google Scholar]
- 11.Abbound B, Aouad R. Non-recurrent inferior laryngeal nerve in thyroid surgery: report of three cases and review of the literature. J Laryngol Otol. 2004;118(2):139–142. doi: 10.1258/002221504772784603. [DOI] [PubMed] [Google Scholar]
- 12.Henry JF, Audiffret J, Denizot A, Plan M. The nonrecurrent inferior laryngeal nerve: review o f33 cases, including two on the left side. Surgery. 1988;104:977–984. [PubMed] [Google Scholar]
- 13.Hermans R, Dewandel P, Debruyne F, Delaere PR. Arteria lusoria identified on preoperative CT and nonrecurrent inferior laryngeal nerve during thyroidectomy: a retrospective study. Head Neck. 2003;25:113–117. doi: 10.1002/hed.10180. [DOI] [PubMed] [Google Scholar]
- 14.Weiand G, Mangold G. Variations in the course of the inferior laryngeal nerve. Surgical anatomy, classification, diagnosis. Chirug. 2004;75(2):187–195. doi: 10.1007/s00104-003-0776-6. [DOI] [PubMed] [Google Scholar]