Toxoplasmosis, a protozoal infection caused by Toxoplasma gondii, is a common opportunistic infection in patients with acquired immunodeficiency syndrome (AIDS) occurring in advanced stages with a fall in the CD4 counts <100 cells/μL. The most common clinical presentation of toxoplasmosis in AIDS is cerebral toxoplasmosis, while other forms include pneumonitis, chorioretinitis, and very rarely involves the heart, bone marrow, bladder, liver, lymph nodes, spine, and skin.[1] In humans, infection occurs through ingestion of infectious oocyst from the soil, cat litter, or uncooked meat of infected animal which disseminate through the blood, lying dormant in immunocompetent people, but in AIDS with low CD4 count, the infection gets reactivated most commonly as cerebral toxoplasmosis.
We report a rare presentation of toxoplasmosis in AIDS presenting for the first time with pyrexia of unknown origin, an erythematous macular rash with left-sided hemiplegia and high levels of toxoplasma IgG antibodies.
A 62-year-old male, daily laborer by occupation, presented with a history of low-grade fever for 1 month and acute onset of pruritic erythematous rash of the upper limbs and anterior chest wall. He had a history of recurrent attacks of the skin rash in the past 1 year for which he was treated symptomatically. There was no history of diarrhea, weight loss, headache, or orogenital ulceration. History of unprotected sex with multiple partners was present. He was a nondiabetic, nonhypertensive, and there was no history of tuberculosis or any major febrile illness in the past. There was no history of intravenous drug abuse. On examination, the patient was febrile with a pulse rate of 106 beats/min, blood pressure of 110/70 mmHg, and respiratory rate of 16/min. There was no clubbing or lymphadenopathy. There were multiple erythematous macules involving front of the neck, anterior chest wall, and upper abdomen [Figure 1]. On the 3rd day of admission, he developed a generalized tonic–clonic convulsion with a drop in Glasgow coma scale (GCS) to 10/15, and detailed neurological examination revealed left-sided upper motor neuron type hemiplegia. Other systems yielded no clinical abnormalities. The patient was evaluated for pyrexia of unknown origin with rash, with a left-sided hemiplegia. The hematological profile was normal. Except for mild liver dysfunction, rest of the biochemistry results were normal [Table 1]. His viral marker for human immunodeficiency virus-1 (HIV-1) by enzyme immunoassay test was positive which was later confirmed by Western blot test, but serology for hepatitis B, hepatitis C, and Venereal Disease Research Laboratory (VDRL) were negative. Blood culture (three samples taken within 12 h of hospitalization), as well as urine and sputum culture were sterile. His chest X-ray and sonography of abdomen were normal. Mantoux test was negative. An urgent contrast tomography brain was done which showed hypodense areas involving bilateral cerebellum, right temporal, caudate nucleus, basal ganglia, and thalamic area with a ring-like lesion on the left parietal area. A contrast magnetic resonance imaging brain was carried out with imaging suggestive of multiple ring-enhancing lesions with perilesional edema in the right thalamus, left cerebellar, and bilateral cerebral hemisphere [Figure 2]. The most common central nervous system (CNS) lesions with such picture in HIV-infected patients with CD4 counts <100/cumm includes toxoplasmosis and primary CNS lymphomas.[2] The primary CNS lymphoma lesions are usually solitary and multiple mass lesions with degree of enhancement that is irregular and patchy though ring-enhancing lesions has also been reported.[3] It is the location and size that helps differentiate cerebral toxoplasmosis from primary CNS lymphomas. Primary CNS lymphomas lesions involve the corpus callosum or the periventricular or periependymal areas where as posterior fossa lesions, lesions in parietal or frontal lobes, thalamus, basal ganglia, or corticomedullary junction are more likely due to toxoplasmosis infection. Lesions that are larger than 4 cm in size are more likely to be lymphoma.[4,5]
Figure 1.

Multiple erythematous macules involving front of the neck, anterior chest wall, and upper abdomen
Table 1.
Laboratory findings in the patient with cerebral toxoplasmosis with fever and erythematous macular rash - an initial presentation in an advanced HIV infection
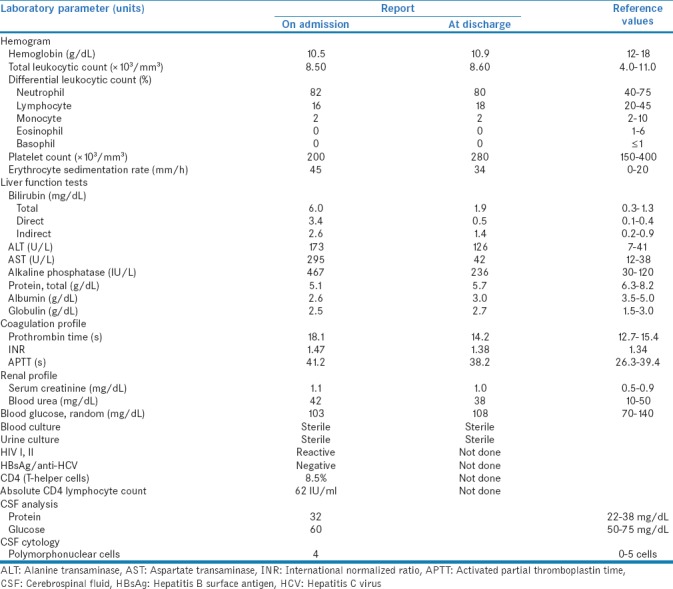
Figure 2.
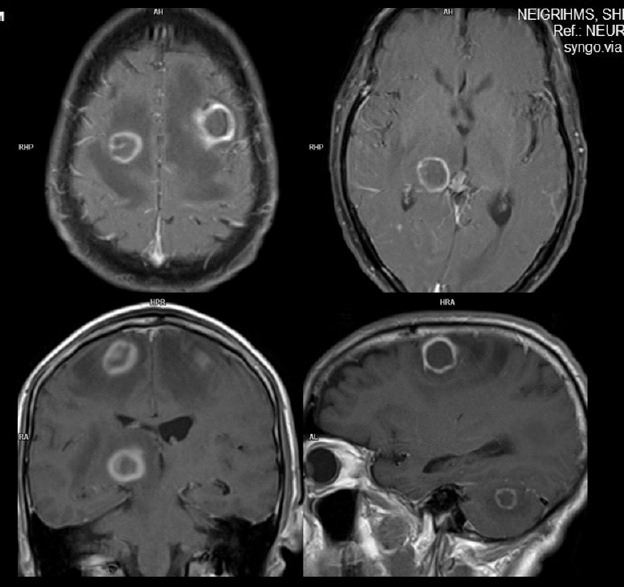
Contrast magnetic resonance imaging brain suggestive of multiple ring-enhancing lesions with perilesional edema in the right thalamus, left cerebellar, and bilateral cerebral hemisphere
His toxoplasma IgG antibodies were found to be very high >200 IU/ml. His CD4 count was 8.5% with absolute CD4 lymphocyte count 62 IU/ml. Fundoscope examination was normal. Cerebrospinal fluid analysis was done and revealed normal study including VDRL. In view of the above findings supporting toxoplasmosis, the patient was started on sulfadiazine and pyremethamine plus clindamycin along with anti epileptic therapy and intravenous dexamethasone and broad spectrum antibiotic. Once patient was improved, highly active antiretroviral therapy (HAART) was also initiated. After 5 days of hospitalization, his GCS improved and the patient was discharged. On reviewing the patient after 2 weeks, he was found to have recovered from the focal neurological deficits. Further, repeat brain-imaging showed resolution of the mass lesions and cerebral edema (Figure 3]. The patient was advised to continue the therapy for another 2 weeks.
Figure 3.
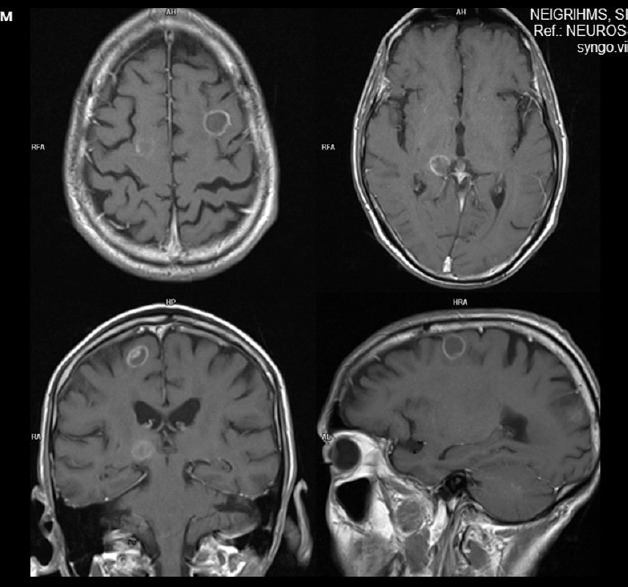
Follow-up contrast magnetic resonance imaging suggestive of persistent ring-enhancing lesion with decrease in perilesional edema
The leading differential diagnosis in AIDS with abnormal neurological finding includes toxoplasmosis, primary CNS lymphoma, progressive multifocal leukoencephalopathy, HIV encephalopathy, and CMV encephalitis. Our patient presented to us for the first time with an opportunistic infection in the CNS unaware of his HIV status. In the present era of early detection and treatment with HAART and antitoxoplasmosis prophylaxis, a significant reduction of toxoplasmosis has been observed.[6,7] Cerebral toxoplasmosis lesions are multiple, or localized lesions in parietal or frontal lobes, in the thalamus, basal ganglia, or corticomedullary junction with ring enhancement seen in 90% of the cases.[5] Definitive diagnosis is made by the clinical syndrome, presence of one or more mass lesion on brain imaging and detection of the organism in biopsy. However due to morbidity and mortality associated with brain biopsy, a presumptive diagnosis is made in an HIV positive patient with clinical syndrome, presence of toxoplasma antibodies, advanced immunosuppression with CD4 cell counts less than 100 cells per cubic millimeter. Studies have also shown that macular rashes may be present in a small percentage of patients with opportunistic toxoplasma infection.[8] Whether the recurrent urticarial rash in the patient is a part of the opportunistic toxoplasma infection is still confusing. Pruritic papular eruption is also a common cutaneous marker in HIV-infected patients for which the cause is not known. Studies showed that >80% of the HIV-infected patients with pruritic rashes have an advanced immunosuppression.[9]
Toxoplasmosis in AIDS presents mostly as a CNS infection in patients who have not received appropriate prophylaxis. In our case, the patient present for the first time with pyrexia of unknown origin, along with a macular rash which on evaluation was found to be in an advanced immunocompromised stage of HIV infection, with a CNS lesion very much suggestive of toxoplasmosis. Thus, it is important that toxoplasmosis infection in an immunocompromised patient should be one of the differential diagnoses in cases of pyrexia of unknown origin with pruritic urticarial rash and CNS involvement.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rabaud C, May T, Amiel C, Katlama C, Leport C, Ambroise-Thomas P, et al. Extracerebral toxoplasmosis in patients infected with HIV. A French National Survey. Medicine (Baltimore) 1994;73:306–14. doi: 10.1097/00005792-199411000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Modi M, Mochan A, Modi G. Management of HIV-associated focal brain lesions in developing countries. QJM. 2004;97:413–21. doi: 10.1093/qjmed/hch080. [DOI] [PubMed] [Google Scholar]
- 3.Ciacci JD, Tellez C, VonRoenn J, Levy RM. Lymphoma of the central nervous system in AIDS. Semin Neurol. 1999;19:213–21. doi: 10.1055/s-2008-1040839. [DOI] [PubMed] [Google Scholar]
- 4.Antinori A, Ammassari A, De Luca A, Cingolani A, Murri R, Scoppettuolo G, et al. Diagnosis of AIDS-related focal brain lesions: A decision-making analysis based on clinical and neuroradiologic characteristics combined with polymerase chain reaction assays in CSF. Neurology. 1997;48:687–94. doi: 10.1212/wnl.48.3.687. [DOI] [PubMed] [Google Scholar]
- 5.Miller RF, Hall-Craggs MA, Costa DC, Brink NS, Scaravilli F, Lucas SB, et al. Magnetic resonance imaging, thallium-201 SPET scanning, and laboratory analyses for discrimination of cerebral lymphoma and toxoplasmosis in AIDS. Sex Transm Infect. 1998;74:258–64. doi: 10.1136/sti.74.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy JA. Human immunodeficiency viruses and the pathogenesis of AIDS. JAMA. 1989;261:2997–3006. [PubMed] [Google Scholar]
- 7.Ciricillo SF, Rosenblum ML. Use of CT and MR imaging to distinguish intracranial lesions and to define the need for biopsy in AIDS patients. J Neurosurg. 1990;73:720–4. doi: 10.3171/jns.1990.73.5.0720. [DOI] [PubMed] [Google Scholar]
- 8.Pinkerton H, Hendason RG. Adult toxoplasmosis previously unrecognized disease entity simulating the typhus spotted fever groups. JAMA. 1941;116:807–14. [Google Scholar]
- 9.Boonchai W, Laohasrisakul R, Manonukul J, Kulthanan K. Pruritic papular eruption in HIV seropositive patients: A cutaneous marker for immunosuppression. Int J Dermatol. 1999;38:348–50. doi: 10.1046/j.1365-4362.1999.00694.x. [DOI] [PubMed] [Google Scholar]


