Abstract
Objective:
This study quantified differences in indirect costs due to decreased work productivity between current and former smokers. Former smokers were further categorized by number of years since quitting to assess corresponding differences.
Methods:
Data on employed individuals were obtained from the 2013 US National Health and Wellness Survey (NHWS; N = 75,000). Indirect costs were calculated for current smokers and former smokers from weekly wages based on age and sex.
Results:
The annual total indirect costs for current smokers were $1327.53, $1560.18, and $1839.87 higher than for those who quit 0 to 4 years, 5 to 10 years, and more than or equal to 11 years prior, respectively. There were no significant differences in mean total indirect costs between the former smoker groups.
Conclusions:
Current smokers showed significantly higher total annual indirect costs compared with former smokers, independently of the number of years since quitting smoking.
Keywords: current smokers, former smokers, indirect costs, smoking cessation
Learning Objectives
Discuss previous knowledge on the direct and indirect costs of smoking, including the economic benefits of quitting smoking.
Summarize the new findings on the difference in indirect costs, including absenteeism and presenteeism, for smokers versus former smokers.
Identify the cost impact, if any, of differences in time since quitting smoking and the implications for workplace smoking cessation programs.
Tobacco use is a global epidemic and a leading cause of illness and death worldwide.1 In 2015, the World Health Organization (WHO) reported that over 1.1 billion people smoked tobacco globally.2 While the prevalence of tobacco smoking has declined in the United States (US), with the percentage of adults (aged 18 years or older) who smoke cigarettes dropping from 20.9% in 2005 to 15.1% in 2015, differences in tobacco smoking persist across sex, age, race/ethnicity, and socioeconomic status.3 For example, in 2015, smoking prevalence was higher among adults aged 25 to 44 years (17.7%) than those aged 65 years or older (8.4%); higher among males (16.7%) than females (13.6%); highest among American Indian/Alaskan Natives (21.9%) and lowest among non-Hispanic Asians (7.0%); highest among people with a General Education Development certificate (GED) (34.1%) and lowest among people with a graduate degree (3.6%).3
Smoking imposes a burden on individuals as well as society. Current smokers exhibit worse health-related quality of life (HRQoL), physical inactivity, sleep impairment, pain, and inadequate consumption of fruits and vegetables compared with non-smokers.4 Smoking is the leading cause of preventable disease and death in the United States.5 One in every five deaths, or more than 480,000 deaths, occur annually due to cigarette smoking in the United States.6 Both active and passive smoking are attributed to over 87% of lung cancer deaths, 61% of pulmonary disease deaths, and 32% of coronary heart disease deaths.7 In recent years, smoking was associated with nearly 2 years of quality-adjusted life expectancy (QALE) loss for US adults throughout their lifetime starting at 18 years of age.8
The annual costs due to smoking in the United States from 2009 to 2012 were between $289 and $332.5 billion, including $132.5 to $175.9 billion for direct medical expenditures for adults, around $151 billion for productivity lost due to premature deaths for the years 2005 to 2009, and about $5.6 billion (in 2006) for productivity lost due to exposure to second-hand smoke.7
Indirect costs of smoking are the costs to employers associated with lost work productivity due to absenteeism and presenteeism.9 A systematic review and meta-analysis of 29 longitudinal and cohort studies in working adults reported that the increase in risk of absenteeism in current smokers was 33% higher compared with non-smokers and 19% higher compared with former smokers. Current smokers were absent from work an average of between 2 and 3 days more per year than non-smokers.10–12 Another study reported that US smokers were absent from work around 6.5 days more per year than non-smokers, and that they and their dependents make more visits per year to health care centers than do non-smokers.13
Evidence indicates that quitting smoking yields short- and long-term benefits to smokers. Shorter-term effects of smoking cessation include improvement in lung function.14 About 12 months of non-smoking is linked to a reduction in the risk of heart disease, cancer, and respiratory diseases.14,15 Within 5 years of quitting, reductions in overall mortality as well as cardiovascular- and cancer-related mortality are realized, sometimes equal to the levels of non-smokers.16 Improved HRQoL has been reported after only a 3-month smoking cessation program, irrespective of quit status.17 The US federal workforce could also benefit from smoking reduction. A five percentage-point reduction in smoking prevalence within the US federal workforce could reduce medical costs by $59 million, absenteeism costs by $332 million, and productivity costs due to premature mortality by $117 over a 5-year period.18
Quitting smoking also reduces both direct and indirect costs, benefitting employees, employers, and society as a whole.19 Smoking prevention programs in the US may be effective at reducing lifetime medical care expenditures by $1.2 billion and increasing lifetime quality-adjusted life-years (QALYs) by 98,590.20 After implementation of legislation that prohibited smoking in all enclosed public places, one study found that the number of hospital admissions for acute coronary syndrome was reduced by 14% among smokers, 19% among former smokers, and 21% among non-smokers whose exposure to second-hand smoke was decreased.21
Several barriers to smoking cessation have been identified. Stress22,23 and urge to smoke or withdrawal symptoms were reported as barriers to quitting smoking among young adults.24 Smokers undergoing the initial phase of quitting reported increased pain sensitivity and blunted stress responses compared with non-smokers, and their reported symptoms of withdrawal were associated with greater pain.25 Benefits of quitting smoking may be realized quickly, however, even considering these initial ill health effects.
Additional barriers may hamper a smoker's attempt at medication-assisted smoking cessation in particular. These include inadequate patient–physician interactions,26,27 less effective cessation methods,28 use of electronic cigarettes,29 unfavorable reimbursement and access,28,30 low awareness of health risks,31,32 and hesitation or unwillingness to quit.33 Other factors that may delay or prevent smokers from medication-assisted attempts to quit may include unawareness of available treatments30,34 and sociodemographic factors.
There is a paucity of studies examining costs associated with smoking-related productivity loss in the United States. While there are a few such studies representative of the US population,9,35–37 there are fewer studies quantifying productivity loss in terms of average dollars per person.9,37 In addition, there is a lack of research exploring the relationship between the length of time since smokers have quit and productivity loss. The current study sought to understand how quickly those who quit smoking may experience beneficial outcomes (eg, increased work productivity), building on a previous related study by examining monetary losses in particular.10 The objective of this study was to quantify the difference in indirect costs associated with work productivity between current smokers and former smokers categorized by years since quitting smoking.
METHODS
Data
Data were analyzed from the 2013 US National Health and Wellness Survey (NHWS; N = 75,000). The current study sample includes respondents who were between the ages of 18 and 64 years old, currently employed, and identified as either current or former smokers (N = 15,181).
The US NHWS is a self-administered, Internet-based survey questionnaire of a large sample of adults aged 18 years or older residing in the United States. A random sample stratified by sex, age, and race/ethnicity was implemented to ensure that the demographic composition of the sample mirrored that of the corresponding adult population, based on data from the US Census. Several peer-reviewed publications have previously compared the NHWS with other governmental sources.38
Measures
Background Characteristics
Sociodemographic measures included age (in years), sex (female vs male), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, or other race/ethnicity), and university education (4-year degree or greater vs less than 4-year degree).
Health Characteristics
Health characteristics included obesity based on body mass index (BMI), which was calculated in kilograms per meter squared (kg/m2) from self-reported height and weight (underweight [less than 18.5], normal [18.5 to less than 25], overweight [25 to less than 30], obese [more than or equal to 30], or decline to answer), and comorbid burden, which was measured by applying the Charlson comorbidity index (CCI) weighted scoring to respondents’ self-reported diagnosis with corresponding conditions (myocardial infarct, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, connective tissue disease, ulcer disease, mild liver disease, diabetes, hemiplegia, moderate or severe renal disease, diabetes with end organ damage, any tumor, leukemia, lymphoma, moderate or severe liver disease, metastatic solid tumor, and AIDS); greater CCI scores indicate greater comorbid burden on the respondent.39
Independent Variable
Years Since Quitting Smoking
Years since quitting smoking were used as the independent variable. Respondents were first asked if they had ever smoked cigarettes. If they selected yes, respondents were then asked for their current smoking status (ie, former smoker, trying to quit but not smoking, trying to quit but still smoking, and current smoker). Respondents who were former smokers or not currently smoking cigarettes were then asked in what year they quit smoking; this result was then subtracted from the year of the survey (2013) to calculate years elapsed since quitting. As in the prior study on which the current analysis is based, depending on the number of years since quitting smoking, respondents were divided into the following four categories: currently smoke (ie, current smokers, including those trying to quit but still smoking), quit smoking between 0 and 4 years prior, quit smoking between 5 and 10 years prior, and quit smoking 11 or more years prior.10
Dependent Variables
Annual Indirect Costs
Work productivity was assessed using the Work Productivity and Activity Impairment-General Health (WPAI-GH) questionnaire, a six-item validated instrument that provides the following four metrics calculated from hours missed and worked in the past 7 days, as well as rated percentage impairment in the past 7 days during work or daily activities: absenteeism (percentage of work time missed because of one's health), presenteeism (how much one's productivity while at work [quality and quantity of work accomplished] was affected by health problems), overall work productivity loss (an overall impairment estimate combining absenteeism and presenteeism), and activity impairment (percentage impairment in daily activities because of one's health).40 Only absenteeism, presenteeism, and overall work productivity scores were analyzed as dependent measures in this study, given that only those scores could be used to derive indirect costs reliably.
Indirect costs were calculated based on weekly wages (by age and sex) obtained from the US Bureau of Labor Statistics (BLS, 2014). Hourly-based wages were estimated by dividing weekly wages by 40. Based on the age and sex of each respondent, the hours missed due to absenteeism and presenteeism were multiplied by corresponding hourly-based wages. These figures were multiplied by 50 work weeks per year to calculate annual indirect costs. The absenteeism- and presenteeism-related indirect costs per year were reported separately and used as dependent variables; these estimates were also combined to calculate total annual indirect costs.
Statistical Analyses
Two-part models were performed using STATA, version 14 (StataCorp LLC, College Station, TX) to assess indirect costs associated with years since quitting smoking.41 Because of the high zero-skewed distribution of indirect cost data where most people have no loss in work productivity and absenteeism, single-distribution generalized linear models often cannot adequately model this type of data.42,43 Two-part models have been commonly used to better model indirect costs and to more accurately predict mean costs.42–45
In the first part of the two-part model, a logit model was used to predict the probability of having a positive cost. Due to the discrete and over-dispersed nature of the dependent measures, a negative binomial distribution with a log-link function was used for the second part of the model, to estimate mean costs conditional on the sample with positive costs. Estimated means (M), delta-method standard errors (SEs), and P-values for joint significance of parameter estimates from both parts of the model are reported for years since quitting smoking. Covariates in multivariable models included age, sex, race/ethnicity, university education, obesity, and CCI.10 Two-sided P-values <0.05 were considered statistically significant. No missing value imputations or multiplicity adjustments were performed. Adjusted mean annual costs for former smokers (ie, those generated by the two-part models) were combined using a weighted average (accounting for sample size per subgroup) for the purpose of an additional, aggregated comparison against the costs for current smokers.
RESULTS
The average age of respondents was 42 years (SD = 12), and most of the respondents identified as male (54.1%), not obese (70.3%), non-Hispanic White (71.6%), and earned less than a 4-year university degree (62.5%). The mean comorbidity burden of the sample was 0.36 (SD = 1.00), as measured by CCI (Table 1).39 All variables were significantly different by years since quitting smoking (all P < 0.05; Table 1). Multivariable two-part models, controlling for covariates, were used to determine absenteeism costs, presenteeism costs, and total indirect costs by years since quitting smoking.
TABLE 1.
Sociodemographic and Health Characteristics by Years Since Quitting Smoking
| Years Since Quitting Smoking | ||||||
| Currently Smoke | 0–4 yrs | 11+ yrs | 5–10 yrs | Total | ||
| N= | 6529 | 2901 | 3842 | 1909 | 15,181 | P Value |
| Age in years (mean ± SD) | 41.81 ± 11.66 | 37.15 ± 12.27 | 49.68 ± 9.72 | 40.87 ± 11.39 | 42.79 ± 12.10 | <0.001 |
| Gender | <0.001 | |||||
| Male (%) | 3,693 (56.6%) | 1,411 (48.6%) | 2,149 (55.9%) | 954 (50.0%) | 8,207 (54.1%) | |
| Female (%) | 2,836 (43.4%) | 1,490 (51.4%) | 1,693 (44.1%) | 955 (50.0%) | 6,974 (45.9%) | |
| Race/Ethnicity | <0.001 | |||||
| Non-Hispanic White (%) | 4,613 (70.7%) | 2,052 (70.7%) | 2,852 (74.2%) | 1,353 (70.9%) | 10,870 (71.6%) | |
| Non-Hispanic Black (%) | 684 (10.5%) | 266 (9.2%) | 355 (9.2%) | 169 (8.9%) | 1,474 (9.7%) | |
| Hispanic (%) | 687 (10.5%) | 324 (11.2%) | 337 (8.8%) | 200 (10.5%) | 1,548 (10.2%) | |
| Other (%) | 545 (8.3%) | 259 (8.9%) | 298 (7.8%) | 187 (9.8%) | 1,289 (8.5%) | |
| University education | <0.001 | |||||
| Less than 4-year degree (%) | 4,570 (70.0%) | 1,787 (61.6%) | 2,064 (53.7%) | 1,062 (55.6%) | 9,483 (62.5%) | |
| 4-year degree or more (%) | 1,959 (30.0%) | 1,114 (38.4%) | 1,778 (46.3%) | 847 (44.4%) | 5,698 (37.5%) | |
| BMI obese | <0.001 | |||||
| Not Obese (%) | 4,871 (74.6%) | 2,068 (71.3%) | 2,465 (64.2%) | 1,266 (66.3%) | 10,670 (70.3%) | |
| Obese (%) | 1,658 (25.4%) | 833 (28.7%) | 1,377 (35.8%) | 643 (33.7%) | 4,511 (29.7%) | |
| CCI (1987) (mean ± SD) | 0.40 ± 1.16 | 0.28 ± 0.78 | 0.35 ± 0.86 | 0.34 ± 0.95 | 0.36 ± 1.00 | <0.001 |
P-values represent the omnibus comparisons noting significant differences across quitting years and are derived from one-way ANOVAs (for continuous measures) or chi-squared tests (for categorical measures) and are two-sided.
CCI, Charlson comorbidity index; SD, standard deviation.
Based on years since quitting smoking, current smokers had significantly greater absenteeism costs, presenteeism costs, and total indirect costs than those who quit smoking 0 to 4 years prior, 5 to 10 years prior, and 11 years or more prior (see Fig. 1 and Table 2). For example, estimated annual total indirect costs for current smokers were $1327.53 higher than for those who quit 0 to 4 years prior, $1560.18 higher than for those who quit between 5 and 10 years prior, and $1839.87 higher than for those who quit more than or equal to 11 years prior. Compared with weighted average annual costs for all former smokers, annual costs for current smokers were estimated to be $512.29 higher for absenteeism, $1247.47 higher for presenteeism, and $1606.37 higher for total indirect costs.
FIGURE 1.
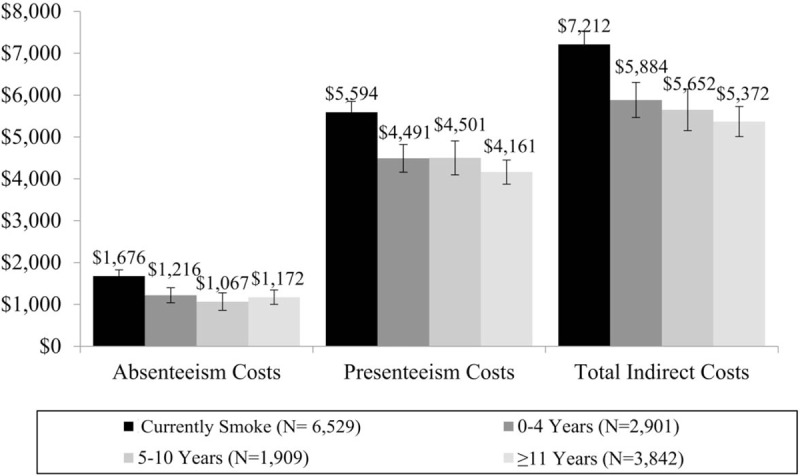
Indirect costs of annual productivity loss as a function of years since quitting smoking. Note: Presented are mean indirect costs as a function of years since quitting smoking, adjusting for covariates in two-part models, with corresponding 95% confidence intervals.
TABLE 2.
Indirect Costs of Annual Productivity Loss by Years Since Quitting Smoking
| Currently Smoke (A) (N = 6,529) | P-Value | 0 to 4 Years (B) (N = 2,901) | P-Value | 5 to 10 Years (C) (N = 1,909) | P-Value | ≥11 Years (D) (N = 3,842) | ||||||||
| Indirect Costs ($/yr) | M | SE | A vs B | A vs C | A vs D | M | SE | B vs C | B vs D | M | SE | C vs D | M | SE |
| Absenteeism cost | 1,676.04 | 77.03 | <0.001 | <0.001 | <0.001 | 1,216.00 | 91.75 | 0.278 | 0.807 | 1,067.21 | 106.75 | 0.190 | 1,172.27 | 87.92 |
| Presenteeism cost | 5,594.29 | 130.36 | <0.001 | <0.001 | <0.001 | 4,491.21 | 169.68 | 0.930 | 0.352 | 4,500.91 | 207.72 | 0.376 | 4,161.23 | 145.85 |
| Total indirect cost | 7,211.78 | 163.28 | <0.001 | <0.001 | <0.001 | 5,884.25 | 214.15 | 0.779 | 0.190 | 5,651.60 | 253.13 | 0.633 | 5,371.91 | 181.98 |
Presented are comparisons of mean indirect costs by years since quitting smoking, adjusting for covariates including age, Charlson comorbidity index, sex, ethnicity, education, and obesity in two-part models. M, mean indirect costs; SE, Delta-method standard error.
There were no statistically significant differences in mean absenteeism costs, presenteeism costs, and total indirect costs between those who quit less than or equal to 4 years, 5 to 10 years, or more than or equal to 11 years prior to their survey participation. Table 3 presents the distribution of relatively short-term cessation among respondents who quit smoking within the previous 0 to 4 years: 48% quit less than or equal to 1-year prior, 37% quit between 2 and 3 years prior, and 15% quit 4 years prior.
TABLE 3.
Years Since Quitting Smoking for Respondents Who Quit 4 Years Prior or Less
| Years Quit | Frequency (n) | Percent (%) |
| 0 | 473 | 16.30 |
| 1 | 919 | 31.68 |
| 2 | 492 | 16.96 |
| 3 | 586 | 20.20 |
| 4 | 431 | 14.86 |
DISCUSSION
This study provides evidence of the economic burden of smoking from lost productivity for employers and the near-term benefits associated with quitting smoking. Current smokers had significantly greater absenteeism, presenteeism, and total indirect costs compared with the former smoker groups, independent of time since they quit. Notably, indirect costs did not differ based on years since quitting, among former smokers. Even those who quit within 4 years of their study participation did not differ significantly from those who quit 11 years or more prior, in terms of indirect costs inclusive of absenteeism and presenteeism.
Results of the current study are consistent with previous studies that established greater work productivity loss for current smokers than non-smokers.9,10,46–48 This productivity loss is attributed to both absenteeism and presenteeism due to smoking and smoking-related illnesses. The current study showed that across each of the four cessation groups, presenteeism costs constituted more than 75% of total productivity losses compared with those due to absenteeism. This substantial share of lost productivity by reduced performance, not work absence, is consistent with results of a previous study conducted by the American Productivity Audit, which found that 71% of total productivity loss was due to presenteeism.37 Higher productivity losses were reflected in higher costs for current smokers and employers. The total indirect costs observed were higher for current smokers than former smokers, as described in previous studies.9,49
Quitting smoking improves work productivity and decreases direct and indirect costs, resulting in substantial cost-savings for employers.11,19,50 Among respondents who quit within 0 to 4 years prior to their survey participation, the highest proportion of respondents (48%) quit at 1 year or less, and almost two thirds within 2 years, indicating that the benefits of quitting smoking are likely to be experienced early. This finding could help assuage employers’ concerns that smoking cessation program outcomes will not be able to outpace rapid employee turnover.
Quitting smoking can be challenging for many smokers. Individuals trying to quit smoking were reported to have poor outcomes in terms of stress and withdrawal symptoms including pain.22–25 This highlights the need for support and services for quit attempters. Those trying to quit may initially experience deficits in work productivity (eg, increased stress). However, there is the potential for long-term gain in productivity among people who have quit smoking successfully, even within several months. A cost estimation approach of previously published studies reported that US employers face an excess cost of approximately $5816 per year for each smoking employee.51 While high turnover rates at some companies might deter them from investing in cessation programs, the economic benefits of smoking cessation programs by employers and primary health authorities are far greater than the costs involved on a long-term basis, as reduced smoking at the workplace may translate into increased productivity, lower indirect costs, and a higher overall cost–benefit ratio.13,52
The strength of the current study lies in its insight into quitting smoking based on reported duration of quitting, as well as assessing the corresponding work-related costs and potential improvement with time since smoking cessation. At the same time, this study has a few limitations. NHWS responses were self-reported, and some respondents may not have revealed their smoking status correctly. However, the survey questions were designed to be simple and non-intrusive. The survey was also confidential, reducing the incentive to misrepresent one's reporting. Data were collected using cross-sectional methodology and therefore preclude most causal inferences. Moreover, data were collected in 2013 and therefore, future studies should provide updates in case the pattern of results has shifted substantially over time. Whereas multivariable models adjusted for relevant demographic and health characteristics, other variables not included in these analyses may help account for the observed pattern of results. Costs among recent quitters in our study and among current smokers (especially those intending to quit) may in part reflect the impact of acute health care events that could have prompted smoking cessation attempts while also contributing directly to increased productivity loss and associated costs.53 Therefore, the costs or cost savings among those who quit due to a comorbid condition may have differed systematically from those seen among respondents who quit in the absence of such a precipitating event. Future research, incorporating an assessment of reasons for quitting, can help tease apart the impact on these different cohorts. The human capital approach was used for the valuation of all potentially lost productivity and is most relevant when there is full use of labor or no unemployment, as is the case in our study where we included only currently employed respondents.54 Lost productivity was valued by calculating the expected or potential earnings lost, for which age- and sex-adjusted standard wages were used. Other approaches, such as multipliers or friction costs, may account for additional aspects of indirect costs related to employment (eg, cost of replacing employees, effects of one employee's lost productivity on that of coworkers, etc.), but rely on assumptions and data not captured in the current analysis.
In conclusion, the current study findings reveal that smoking poses a substantial burden on employers in terms of increased indirect costs from lost productivity. This burden suggests an unmet need for better treatments and other interventions to help current smokers quit smoking. It would be beneficial for companies to support smoking cessation programs that facilitate quitting among employees.
Acknowledgments
The authors acknowledge Swapna Gurrala, Ph.D., and Ramu Periyasamy, Ph.D., at Indegene Pvt Ltd., and Michael J. Doane, Ph.D., at Kantar Health, for assistance with literature review and writing.
Footnotes
Funding Source: Pfizer Inc. funded the execution of this study and the development of this manuscript.
Disclosures: This study was sponsored by Pfizer Inc. CL Baker, B Emir and M Bruno are employees and stockholders of Pfizer Inc. A Goren and VW Li are employees of Kantar Health. Kantar Health received funding from Pfizer for conducting this study and for the development of this manuscript.
Authors Goren, Baker, Bruno, Emir, and Li have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
REFERENCES
- 1.World Health Organization. Tobacco fact sheet. Available at: http://www.who.int/mediacentre/factsheets/fs339/en/. Updated May 2017. Accessed May 30, 2017. [Google Scholar]
- 2.World Health Organization. Global Health Observatory data. Prevalence of tobacco smoking. Available at: http://www.who.int/gho/tobacco/use/en/. Accessed June 2, 2017. [Google Scholar]
- 3.Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults—United States, 2005-2015. MMWR Morb Mortal Wkly Rep 2016; 65:1205–1211. [DOI] [PubMed] [Google Scholar]
- 4.Strine TW, Okoro CA, Chapman DP, et al. Health-related quality of life and health risk behaviors among smokers. Am J Prev Med 2005; 28:182–187. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States. Available at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm. Accessed May 30, 2017. [Google Scholar]
- 6.U.S. Department of Health and Human Services. The health consequences of smoking-50 years of progress: a report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014. Available at: https://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf. Accessed May 30, 2017. [Google Scholar]
- 7.U.S. Department of Health and Human Services. The health consequences of smoking-50 years of progress. A report of the surgeon general. Executive summary. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. Available at: https://www.surgeongeneral.gov/library/reports/50-years-of-progress/exec-summary.pdf. Accessed May 30, 2017. [Google Scholar]
- 8.Jia H, Zack MM, Thompson WW, Dube SR. Quality-adjusted life expectancy (QALE) loss due to smoking in the United States. Qual Life Res 2013; 22:27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bunn WB, III, Stave GM, Downs KE, Alvir JM, Dirani R. Effect of smoking status on productivity loss. J Occup Environ Med 2006; 48:1099–1108. [DOI] [PubMed] [Google Scholar]
- 10.Baker CL, Flores NM, Zou KH, Bruno M, Harrison VJ. Benefits of quitting smoking on work productivity and activity impairment in the United States, the European Union and China. Int J Clin Pract 2017; 71:e12900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weng SF, Ali S, Leonardi-Bee J. Smoking and absence from work: systematic review and meta-analysis of occupational studies. Addiction 2013; 108:307–319. [DOI] [PubMed] [Google Scholar]
- 12.Asay GRB, Roy K, Lang JE, Payne RL, Howard DH. Absenteeism and employer costs associated with chronic diseases and health risk factors in the US workforce. Prev Chronic Dis 2016; 13:E141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ekpu VU, Brown AK. The economic impact of smoking and of reducing smoking prevalence: review of evidence. Tob Use Insights 2015; 8:1–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gratziou C. Respiratory, cardiovascular and other physiological consequences of smoking cessation. Curr Med Res Opin 2009; 25:535–545. [DOI] [PubMed] [Google Scholar]
- 15.Benefits of quitting over time. American Cancer Society Website. Available at: https://www.cancer.org/healthy/stay-away-from-tobacco/benefits-of-quitting-smoking-over-time.html. Updated September 9, 2016. Accessed June 6, 2017. [Google Scholar]
- 16.Menzin J, Lines LM, Marton J. Estimating the short-term clinical and economic benefits of smoking cessation: do we have it right? Expert Rev Pharmacoecon Outcomes Res 2009; 9:257–264. [DOI] [PubMed] [Google Scholar]
- 17.Tomioka H, Sekiya R, Nishio C, Ishimoto G. Impact of smoking cessation therapy on health-related quality of life. BMJ Open Respir Res 2014; 1:e000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asay GRB, Homa DM, Abramsohn EM, Xu X, O’Connor EL, Wang G. Reducing smoking in the US federal workforce: 5-year health and economic impacts from improved cardiovascular disease outcomes. Public Health Rep 2017; 132:646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rasmussen SR, Prescott E, Sorensen TI, Sogaard J. The total lifetime health cost savings of smoking cessation to society. Eur J Public Health 2005; 15:601–606. [DOI] [PubMed] [Google Scholar]
- 20.Wang LY, Michael SL. Long-term health and medical cost impact of smoking prevention in adolescence. J Adolesc Health 2015; 56:160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pell JP, Haw S, Cobbe S, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med 2008; 359:482–491. [DOI] [PubMed] [Google Scholar]
- 22.Robles Z, Garey L, Hogan J, Bakhshaie J, Schmidt NB, Zvolensky MJ. Examining an underlying mechanism between perceived stress and smoking cessation-related outcomes. Addict Behav 2016; 58:149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skov-Ettrup LS, Egan KK, Dalum P, Tolstrup JS. Stress-related expectations about smoking cessation and future quit attempts and abstinence - a prospective study in daily smokers who wish to quit. Prev Med Rep 2017; 6:187–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Villanti AC, Bover Manderski MT, Gundersen DA, Steinberg MB, Delnevo CD. Reasons to quit and barriers to quitting smoking in US young adults. Fam Pract 2016; 33:133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nakajima M, Al’Absi M. Nicotine withdrawal and stress-induced changes in pain sensitivity: a cross-sectional investigation between abstinent smokers and nonsmokers. Psychophysiology 2014; 51:1015–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Champassak SL, Catley D, Finocchario-Kessler S, et al. Physician smoking cessation counseling and adherence to a clinical practice guideline. Eur J Pers Cent Healthc 2014; 2:477–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorndike AN, Regan S, Rigotti NA. The treatment of smoking by US physicians during ambulatory visits: 1994–2003. Am J Public Health 2007; 97:1878–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fiore MC, Novotny TE, Pierce JP, et al. Methods used to quit smoking in the United States. Do cessation programs help? JAMA 1990; 263:2760–2765. [PubMed] [Google Scholar]
- 29.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med 2016; 4:116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Igarashi A, Negishi S, Goto R, Suwa K. Web-based survey on smoking cessation behaviors of current and former smokers in Japan. Curr Med Res Opin 2014; 30:1911–1921. [DOI] [PubMed] [Google Scholar]
- 31.Abu Shomar RT, Lubbad IK, El AW, Al-Khatib IA, Alharazin HJ. Smoking, awareness of smoking-associated health risks, and knowledge of national tobacco legislation in Gaza, Palestine. Cent Eur J Public Health 2014; 22:80–89. [DOI] [PubMed] [Google Scholar]
- 32.Colomar M, Tong VT, Morello P, et al. Barriers and promoters of an evidenced-based smoking cessation counseling during prenatal care in Argentina and Uruguay. Matern Child Health J 2015; 19:1481–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blumenthal DS. Barriers to the provision of smoking cessation services reported by clinicians in underserved communities. J Am Board Fam Med 2007; 20:272–279. [DOI] [PubMed] [Google Scholar]
- 34.Yeomans K, Payne KA, Marton JP, et al. Smoking, smoking cessation and smoking relapse patterns: a web-based survey of current and former smokers in the US. Int J Clin Pract 2011; 65:1043–1054. [DOI] [PubMed] [Google Scholar]
- 35.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med 2004; 46:398–412. [DOI] [PubMed] [Google Scholar]
- 36.Halpern MT, Shikiar R, Rentz AM, Khan ZM. Impact of smoking status on workplace absenteeism and productivity. Tob Control 2001; 10:233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J Occup Environ Med 2003; 45:1234–1246. [DOI] [PubMed] [Google Scholar]
- 38.DiBonaventura MD, Wagner JS, Yuan Y, L’Italien G, Langley P, Ray KW. Humanistic and economic impacts of hepatitis C infection in the United States. J Med Econ 2010; 13:709–718. [DOI] [PubMed] [Google Scholar]
- 39.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40:373–383. [DOI] [PubMed] [Google Scholar]
- 40.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993; 4:353–365. [DOI] [PubMed] [Google Scholar]
- 41.Belotti F, Deb P, Manning WG, Norton EC. twopm: Two-part models. Stata J 2015; 15:3–20. [Google Scholar]
- 42.Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. J Health Econ 2011; 20:897–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bishu KG, Gebregziabher M, Dismuke CE, Egede LE. Quantifying the incremental and aggregate cost of missed workdays in adults with diabetes. J Gen Intern Med 2015; 30:1773–1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupte-Singh K, Singh RR, Lawson KA. Economic burden of attention-deficit/hyperactivity disorder among pediatric patients in the United States. Value Health 2017; 20:602–609. [DOI] [PubMed] [Google Scholar]
- 45.Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep 2007; 30:263–273. [DOI] [PubMed] [Google Scholar]
- 46.Max W. The financial impact of smoking on health-related costs: a review of the literature. Am J Health Promot 2001; 15:321–331. [DOI] [PubMed] [Google Scholar]
- 47.Sherman BW, Lynch WD. The relationship between smoking and health care, workers’ compensation, and productivity costs for a large employer. J Occup Environ Med 2013; 55:879–884. [DOI] [PubMed] [Google Scholar]
- 48.Suarez-Bonel MP, Villaverde-Royo MV, Nerin I, Sanz-Andres C, Mezquida-Arno J, Cordoba-Garcia R. Health care costs and work absenteeism in smokers: study in an urban community. Arch Bronconeumol 2015; 51:615–620. [DOI] [PubMed] [Google Scholar]
- 49.Rabacow FM, Luiz OC, Malik AM, Burdorf A. Lifestyle factors, direct and indirect costs for a Brazilian airline company. Rev Saude Publica 2014; 48:949–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oster G, Colditz GA, Kelly NL. The economic costs of smoking and benefits of quitting for individual smokers. Prev Med 1984; 13:377–389. [DOI] [PubMed] [Google Scholar]
- 51.Berman M, Crane R, Seiber E, Munur M. Estimating the cost of a smoking employee. Tob Control 2014; 23:428–433. [DOI] [PubMed] [Google Scholar]
- 52.Jackson KC, Nahoopii R, Said Q, Dirani R, Brixner D. An employer-based cost-benefit analysis of a novel pharmacotherapy agent for smoking cessation. J Occup Environ Med 2007; 49:453–460. [DOI] [PubMed] [Google Scholar]
- 53.Fishman PA, Thompson EE, Merikle E, Curry SJ. Changes in health care costs before and after smoking cessation. Nicotine Tob Res 2006; 8:393–401. [DOI] [PubMed] [Google Scholar]
- 54.Lensberg BR, Drummond MF, Danchenko N, Despiegel N, Francois C. Challenges in measuring and valuing productivity costs, and their relevance in mood disorders. Clinicoecon Outcomes Res 2013; 5:565–573. [DOI] [PMC free article] [PubMed] [Google Scholar]


