Abstract
Introduction
Social interactions are a key mechanism through which health communication efforts, including pictorial cigarette pack warnings, may exert their effects. We sought to better understand social interactions elicited by pictorial cigarette pack warnings.
Methods
A controlled trial randomly assigned US adult smokers (n = 2149) to have their cigarette packs labeled with pictorial or text-only warnings for 4 weeks. Smokers completed surveys during the baseline visit and each of the subsequent 4 weekly visits.
Results
Smokers with pictorial warnings on their packs had more conversations throughout the trial compared to those with text-only warnings (8.2 conversations vs 5.0, p<.01). The highest number of conversations occurred during the first week. Smokers with pictorial warnings were more likely than those with text-only warnings to discuss the health effects of smoking, whether the warnings would make them want to quit and whether the warnings would make others want to quit (all p < .05). Smokers were more likely to describe pictorial warnings as scary, gross, or depressing and gloomy during conversations than text-only warnings (all p < .05).
Conclusions
Pictorial warnings sparked more conversations about the warnings, the health effects of smoking, and quitting smoking than text-only warnings. These social interactions may extend the reach of pictorial warnings beyond the targeted smoker and may be one of the processes by which pictorial warnings have impact.
Implications
Health communication can influence behavior by changing social interactions. Our trial characterized social interactions about pictorial cigarette pack warnings with a large longitudinal sample in a real-world setting. Understanding these conversations can inform the United States and other countries as they improve existing warnings and help tobacco control policy makers and health communication theorists understand how social interactions triggered by warnings affect smoking.
Introduction
Worldwide, tobacco use causes nearly six million deaths per year.1 In the United States, cigarette smoking is responsible for one in five deaths.2 Cigarette packs have proven to be an effective communication device for tobacco companies,3,4 and research has shown they can be effective tools to communicate about the health risks of smoking.5
The World Health Organization Framework Convention on Tobacco Control recommends large pictorial images appear on cigarette packages because of evidence that, compared to text only warnings, pictorial warnings communicate health risks more effectively.6 Compared to text warnings, pictorial warnings elicit more concern about the harms of smoking,5,7 more negative attitudes toward smoking,5,7 greater quit intentions,7,8 and more quit attempts.8 Although tobacco industry lawsuits have delayed implementation of pictorial warnings in the United States, the Food and Drug Administration (FDA) intends to propose a revised set of warnings that will address the concerns raised in the lawsuit.9 Understanding how smokers interact with pictorial warnings in real-world settings may provide important information, as the United States designs new warnings for maximal impact.
Because smoking is a social behavior, heavily influenced by peer and social networks,10–12 social interactions may be particularly important in the context of antismoking communication campaigns and pictorial warnings on cigarette packs.7 Smokers are more likely to socialize with other smokers, and smoking influences the behavior of others within a social network.12 Furthermore, smoking behavior frequently happens in social settings,13,14 offering openings for conversations to take place. Several studies have found face-to-face or online social interactions were positively associated with motivation to stop smoking, such as intentions to quit smoking.15–22
Pictorial warnings have certain advantages over traditional antismoking campaigns. They are found directly on smokers’ cigarette packs, which increases regular exposure to the warnings and offers a unique opportunity to trigger social interactions during the act of smoking. Evidence suggests that pictorial warnings have particular utility in the generation of interpersonal interaction, given the potential of visual content to elicit emotional responses.23,24 Southwell reviewed decades of literature on conversations about health and science. He noted two mechanisms that account for this generative tendency of emotionally evocative pictorial content: they get people thinking and more actively engaged. Pictorial content can provide useful currency in making connections with other people. For these reasons, the potential of pictorial warnings to spark conversations seems substantial, and yet relatively few studies have examined the role of social interactions about pictorial warnings. Those that have primarily examined the frequency rather than the content of these interactions.23–27
In our trial, we sought to describe the frequency, content, and nature of adult smokers’ social interactions about pictorial cigarette pack warnings in the context of a randomized controlled trial that allowed for a robust comparison with text-only warnings. Characterization of social interactions about pictorial cigarette pack warnings with a large sample studied longitudinally can provide tobacco control policy makers and health communication theorists with a better understanding of how social interactions triggered by warnings may affect smoking.
Methods
Participants
We recruited a convenience sample of adult smokers (aged 18 or older) in North Carolina and California, from September 2014 to August 2015. The three most effective methods for identifying participants were Craigslist, word of mouth, and Facebook.28
Procedures
We conducted a randomized controlled trial comparing the impact of pictorial warning labels versus text-only warnings (clinicaltrials.gov identifier: NCT02247908). The trial was effective at increasing quit attempts across the 4 weeks; details regarding methods and main results appear in Brewer et al.8 Briefly, participants brought in an 8-day supply of cigarettes to the baseline visit and were randomly assigned to have one of eight warnings placed on their packs. Participants received the same warning for the duration of the study. Four pictorial warnings contained text required by the Tobacco Control Act and a picture to illustrate a health harm of smoking selected from the United States’s originally proposed set of images.29 Four text-only control warnings used the US Surgeon General’s warning statements that have been required on the side of cigarette packs since 1985. Participants attended four follow-up visits spaced 1 week apart, bringing an 8-day supply of cigarettes to all but the final visit.
Participants completed a computer survey at the baseline visit and at each subsequent weekly visit. While participants completed the surveys at these appointments, research staff placed the assigned warnings on participants’ cigarette packs following a standardized protocol.30 All participants provided their written informed consent, and The University of North Carolina institutional review board approved the study procedures.
Measures
The survey used items previously validated and newly developed survey items that we cognitively tested with 15 adult smokers.31 The baseline survey assessed the frequency of conversation about the current surgeon general’s warning on their pack and demographic characteristics. The subsequent weekly surveys asked about the frequency of conversation about the label we placed on their pack, conversation partners, conversation content, and social media posts about the warnings.
Conversation Frequency
The weekly surveys assessed frequency of conversations about the warnings with one item, “In the last week, how many times did you talk to other people about the health warning on your cigarette packs?” The response options were “never” (coded as 1), “1–2 times” (coded as 1.5), “3–4 times” (coded as 3.5), “5–9 times” (coded as 7), and “10 or more times” (coded as 10).30
Conversation Partners
The weekly surveys provided a list of conversation partners and asked participants to select the people with whom they discussed the warning during the last week. Conversations partners were my “spouse or significant other,” “other family member,” “my child,” “friend,” “co-worker,” “medical professional,” “someone you did not previously know,” and “other.”30
Conversation Content
The weekly surveys provided the participants with a list of topics and asked them to select which topics had come up in conversations during the last week. Topics were “the health effects of smoking,” “the warning would make them want to quit,” “the warning would make other smokers want to quit,” “the warning would stop people from starting to smoke,” “the warning should be on cigarette packs in the US,” “cigarette pack warnings in other countries,” “someone made fun of the warning,” “the research study,” and “other.” A separate survey item provided a list of warning descriptors and asked participants to select descriptors that they or their conversation partner had used in the last week. The descriptors were “scary;” “depressing, gloomy;” “stupid, pointless;” “judgmental, controlling;” “interesting, engaging;” “informative, useful;” “gross;” “silly;” and “other.”30
Social Media
The final survey asked participants if they had posted about the warning on any social media platforms in the last 4 weeks. The platforms listed were “Facebook,” “Instagram,” “Twitter,” “MySpace,” “Reddit,” “Vine,” “other,” and “none of these.”30
Results
The trial enrolled 2149 adult current smokers (1039 men, 1060 women, and 34 transgender people). Their mean age was 40. Trial participants were diverse with respect to race, sexual orientation, education, and income, and participant characteristics did not differ by trial arm (Table 1).
Table 1.
Participant characteristicsa
| Characteristic | Pictorial warnings (n = 1071) |
Text-only warnings (n = 1078) |
|---|---|---|
| Age in years, mean (SD) | 39.8 (13.7) | 39.7 (13.4) |
| Gender | ||
| Female | 512 (48.2) | 548 (51.2) |
| Male | 532 (50.0) | 507 (47.4) |
| Transgender | 19 (1.8) | 15 (1.4) |
| Gay, lesbian or bisexual | 195 (18.8) | 173 (16.3) |
| Hispanic | 89 (8.5) | 92 (8.6) |
| Race | ||
| Asian | 42 (4.0) | 28 (2.7) |
| Black | 510 (48.9) | 484 (45.8) |
| White | 358 (34.3) | 393 (37.2) |
| Other/multi-racial | 134 (12.5) | 152 (14.1) |
| Education | ||
| High school or less | 344 (32.5) | 333 (31.1) |
| Some college | 502 (47.4) | 519 (48.5) |
| College graduate | 156 (14.7) | 156 (14.6) |
| Graduate or professional degree | 58 (5.5) | 63 (5.9) |
| Low income (<150% of federal poverty level) | 589 (55.2) | 570 (53.0) |
| Cigarettes smoked per day, Mean (SD) | 8.7 (7.3) | 8.8 (6.6) |
aData are reported as number (percentage) of participants unless otherwise noted. Characteristics did not differ by trial arm. Missing demographic data range from 0% to 2%.
Frequency of Social Interactions
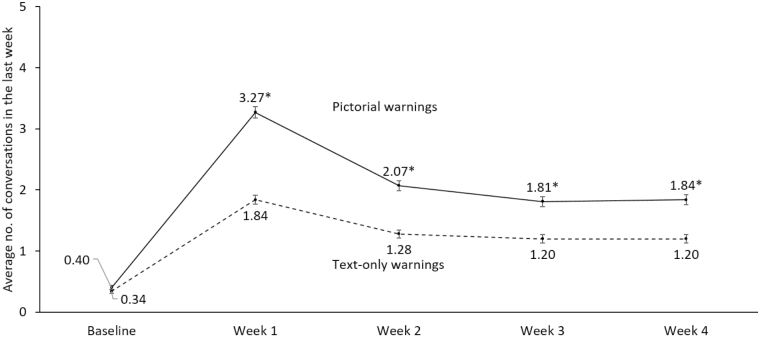
Conversations about the warnings were a common experience with 90% of smokers with pictorial warnings (n = 995) and 78% of smokers with text-only warnings (n = 1003) having at least one conversation during the study (p < .01). While trial arms did not differ in the number of conversations they had about the warnings on their pack at baseline (Figure 1), smokers with pictorial warnings had more conversations throughout the trial compared to those with text-only warnings (mean = 8.18 conversations [SD=7.97] vs. 5.02 [SD = 6.25], p < .01). The highest number of conversations for each group occurred during the first week with an average of 3.27 (SD = 2.93) for the pictorial warnings and 1.84 (SD=2.14) for the text-only warnings (p < .01).
Figure 1.
Frequency of conversations about warnings on cigarette packs. Error bars show standard errors. ap < .05.
Eighty-six percent of smokers with pictorial warnings reported that they intentionally showed the warning to someone compared to 73% in the text-only group (p < .001). During the first week, smokers with pictorial warnings intentionally showed others their warnings an average of 2.88 times (SD = 2.86) compared to 1.66 times (SD = 2.08) for those with text-only warnings (p < .001).
Conversation Partners
During the course of the trial, participants who talked about the warnings (n = 896 for pictorial vs 785 for text-only) conversed with a wide range of people. Most participants reported talking about the warning with a friend (82% pictorial warnings vs 74% text-only warnings, p < .01). Some talked with significant others or spouses (41% vs 41%, ns), other family members (44% vs. 35%, p < .05), coworkers (33% vs 27%, p < .05), and someone they did not previously know (31% vs 17%, p < .05). Fewer participants talked with their children (18% vs 17%, ns) or a medical professional about the warning (10% vs 9%, ns). Participants (n = 893 for pictorial vs 780 for text-only) had conversations about the warning labels with both smokers (91% pictorial vs 85% text-only, p < .05), nonsmokers (63% vs. 61%, ns), and with those whose smoking status they did not know (18% vs 15%, p < .05).
Content of the Conversations
Throughout the trial, participants who talked about the warnings discussed a variety of topics. Most participants discussed the trial (75% pictorial vs 71% text-only, ns), whether the warnings would make them want to quit (75% vs. 59%, p<.05), and the health effects of smoking (74% vs 68%, p < .05; Table 2). Some participants discussed whether the warnings would make other smokers want to quit (64% vs 45%, p < .05), whether the warnings should be on cigarette packs (60% vs 38%, p < .05), and whether the warning would prevent initiation of smoking (60% vs 38%, p < .05).
Table 2.
Topics of the conversations throughout the trial
| Topic of conversations | Pictorial warnings (n = 896), % | Text-only Warnings (n=785), % |
|---|---|---|
| This research study | 75 | 71 |
| Whether the warnings would make me want to quit | 75* | 59 |
| The health effects of smoking | 74* | 68 |
| Whether the warning would make other smokers want to quit | 64* | 45 |
| Whether the warnings should be on cigarette packs in the US | 60* | 38 |
| Whether the warnings would stop people from starting to smoke | 57* | 40 |
| Cigarette pack warnings in other countries | 42* | 35 |
| Made fun of warning | 22* | 16 |
| Other | 15 | 18 |
*p < .05.
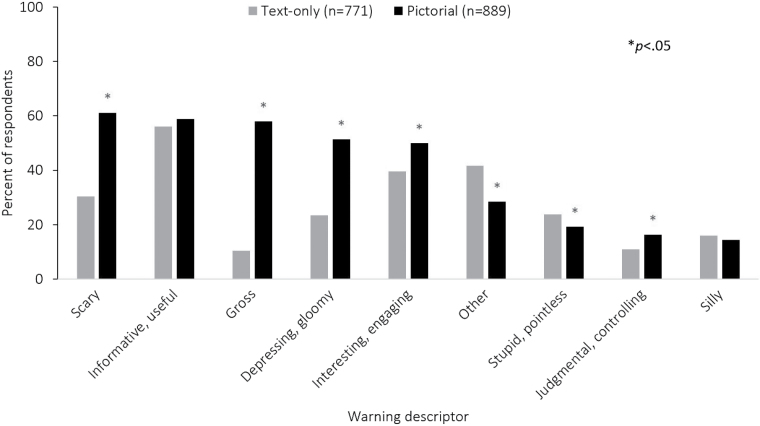
Participants reported having conversations describing the warnings using several adjectives (n = 889 for pictorial vs 771 for text-only; Figure 2). Pictorial warnings were more frequently described as “gross” (58% pictorial vs 10% text-only, p<.05), “scary” (61% vs. 30%, p < .05), and “depressing and gloomy” (51% vs 23%, p < .05) compared to text-only warnings. Both warnings were described as “informative and useful” with similar frequency (59% vs 56%, ns). Text-only warnings were more frequently described as “stupid and pointless” (19% pictorial vs 24% text-only, p<.05) or with other adjectives (28% vs. 42%, p<.05) compared to pictorial warnings.
Figure 2.
How participants described the warnings throughout the study.
Social Media
Fourteen percent of the participants shared the warnings on social media (Facebook, Instagram, Twitter, Myspace, Reddit, Vine, or other), which did not differ between trial arms. Of those sharing (n = 142 for pictorial vs n = 130 for text-only), most participants reported posting on a platform the survey did not list (other; 46% pictorial vs 55% text-only, ns). The top two listed social media platforms participants shared on were Facebook (45% pictorial vs 36% text-only, ns) and Instagram (18% vs 8%, p < .05). Participants reported posting comments about the warnings (40% pictorial vs 41% text-only, ns), comments about the trial (46% vs. 45%, ns), and pictures of the labels (62% vs 42%, p < .05).
Discussion
Social interactions about pictorial cigarette pack warnings occurred more frequently than for text-only warnings during the trial. Moreover, the topics of conversations about pictorial warnings extended past the warnings themselves and included conversations about the health effects of smoking and cessation, generating conversations that may amplify the direct impact of the warning in discouraging smoking. In addition, smokers had conversations with many different partners, which may extend the reach of these warnings beyond the targeted smoker and may be one of the processes by which pictorial warnings have impact. Indeed, the nature of these conversations suggests that smokers are more deeply processing these warning messages in ways that might not occur without such social interactions.
These findings build on previous research from Hall and colleagues who found in a pilot study that nearly all smokers talked about the warning labels on their packs.30 In our trial, conversations increased during the first week, followed by a drop in the second week. This pattern is consistent with work from previous studies which indicate that cigarette pack warnings are most effective when they are new and that responses to the warnings exhibit a partial wear-out effect over the course of months or years.32–34 An important finding is the increase in conversations that pictorial warnings elicited over the entire trial compared to text warnings. Even in the final week of the trial, participants discussed pictorial warnings more often than text-only warnings. Research has shown that one way to maintain these effects is to rotate cigarette warnings labels to keep them fresh.33,35
Social media may amplify the reach and impact of pictorial warnings.36 Almost a sixth of smokers shared an image or comment about the label unprompted, but mass and social media campaigns launched together with pictorial warnings may magnify the effects of pictorial warnings.37 In Mexico, exposure to a mass media campaign launched in conjunction with the introduction of pictorial warning labels was associated with greater attention to pictorial warnings and cognitive elaboration.38 Similarly, an Australian study found that television advertisements heightened the effect of pictorial warning exposure on knowledge of the health effects of smoking.39 Future studies should explore the possible synergistic effects of mass media and social media campaigns on pictorial warnings.
Participants reported some critical or negative commentary regarding the content of the warnings. Not all of the reported conversation was positive or supportive of the warning message. Such critique is not uncommon; David and colleagues also found participant denigration of antitobacco messages in their study of social interactions.40 Simple generation of any conversation, then, is not likely to be universally helpful in extending the reach of intended reaction to the original warning labels. Nonetheless, we also found a substantial amount of relevant conversation that both extended exposure to the warning messages and likely reinforced memory for the warnings among those initially exposed. This is somewhat analogous to the finding that while pictorial warnings may elicit negative reactions among some individual smokers (i.e., message reactance),41 this is greatly outweighed by the positive effects of warnings at the population level.7,42
Strengths of our study include our use of a randomized trial, longitudinal data, the use of cognitively tested measures about social interactions, and a naturalistic pack-labeling protocol that exposed smokers to warnings on their actual cigarette packs.30 However, the trial took place in the United States, where pictorial warnings are not currently on cigarette packs, potentially heightening the immediate novelty of the warnings and providing an impetus for some of the conversations about the warnings. However, the larger number of conversations due to the pictorial warnings, across many topics, suggests that pictorial warnings offer special added value relative to existing text-only warnings. The generalizability of these findings to smokers in other settings and over a longer period merits further study.
Pictorial cigarette pack warnings prompt conversations. It is important for policy makers to consider the social context for pictorial warnings once they are introduced. Future research should explore whether and how naturally occurring and experimentally prompted social interactions about pictorial warning labels impact smoking behavior.
FUNDING
Research reported in this publication was supported by grant number 3P50 CA180907-03S1 from the National Cancer Institute and the FDA Center for Tobacco Products (CTP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration. Grant number P50 CA180907 from the National Cancer Institute and the FDA Center for Tobacco Products (CTP) and a Dissertation Completion Fellowship from The Graduate School at the University of North Carolina at Chapel Hill supported part of Jennifer Morgan’s time spent writing the paper.
Declaration of Interests
KMR has served as an expert consultant against cigarette manufacturers; no other conflicts.
References
- 1. World Health Organization. WHO Report on the Global Tobacco Epidemic, 2013: Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 2. US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Rockville, MD:US Department of Health and Human Services; 2014. [Google Scholar]
- 3. Slade J. The pack as advertisement. Tob Control. 1997;6(3):169–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wakefield M, Morley C, Horan JK, Cummings KM. The cigarette pack as image: new evidence from tobacco industry documents. Tob Control. 2002;11 Suppl 1:I73–I80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20(5):327–337. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization. Framework Convention on Tobacco Control 2013. http://www.who.int/fctc/en/. Accessed April 20, 2013.
- 7. Noar SM, Francis DB, Bridges C, Sontag JM, Brewer NT, Ribisl KM. Effects of strengthening cigarette pack warnings on attention and message processing: A systematic review. Journal Mass Commun Q. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brewer NT, Hall MG, Noar SM, et al. . Effect of Pictorial Cigarette Pack Warnings on Changes in Smoking Behavior: A Randomized Clinical Trial. JAMA Intern Med. 2016;176(7):905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Holder EH. Re: R.J. Reynolds v. Food & Drug Administration, No. 11–5332 (D.C. Cir. 2013) https://www.justice.gov/sites/default/files/oip/legacy/2014/07/23/03-15-2013.pdf. Accessed November 22, 2016.
- 10. Chen PH, White HR, Pandina RJ. Predictors of smoking cessation from adolescence into young adulthood. Addict Behav. 2001;26(4):517–529. [DOI] [PubMed] [Google Scholar]
- 11. Powell LM, Tauras JA, Ross H. The importance of peer effects, cigarette prices and tobacco control policies for youth smoking behavior. J Health Econ. 2005;24(5):950–968. [DOI] [PubMed] [Google Scholar]
- 12. Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moran S, Wechsler H, Rigotti NA. Social smoking among US college students. Pediatrics. 2004;114(4):1028–1034. [DOI] [PubMed] [Google Scholar]
- 14. Schane RE, Glantz SA, Ling PM. Nondaily and social smoking: an increasingly prevalent pattern. Arch Intern Med. 2009;169(19):1742–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dunlop S, Wakefield M, Kashima Y. Can you feel it? Negative emotion, risk, and narrative in health communication. Media Psychol. 2008;11(1):52–75. [Google Scholar]
- 16. Dunlop SM, Wakefield M, Kashima Y. The contribution of antismoking advertising to quitting: intra- and interpersonal processes. J Health Commun. 2008;13(3):250–266. [DOI] [PubMed] [Google Scholar]
- 17. Durkin S, Wakefield M. Maximizing the impact of emotive antitobacco advertising: Effects of interpersonal discussion and program placement. Social Marketing Quarterly. 2006;12(3):3–14. [Google Scholar]
- 18. Hafstad A, Aarø L, Langmark F. Evaluation of an anti-smoking mass media campaign targeting adolescents: The role of affective responses and interpersonal communication. Health Educ Res. 1996;11(1):29–38. [Google Scholar]
- 19. Hafstad A, Aarø LE, Engeland A, Andersen A, Langmark F, Stray-Pedersen B. Provocative appeals in anti-smoking mass media campaigns targeting adolescents–the accumulated effect of multiple exposures. Health Educ Res. 1997;12(2):227–236. [DOI] [PubMed] [Google Scholar]
- 20. Schuster DV, Valente TW, Skara SN, et al. . Intermedia processes in the adoption of tobacco control activities among opinion leaders in California. Commun Theory. 2006;16(1):91–117. [Google Scholar]
- 21. van den Putte B, Yzer M, Southwell BG, de Bruijn GJ, Willemsen MC. Interpersonal communication as an indirect pathway for the effect of antismoking media content on smoking cessation. J Health Commun. 2011;16(5):470–485. [DOI] [PubMed] [Google Scholar]
- 22. Depue JB, Southwell BG, Betzner AE, Walsh BM. Encoded exposure to tobacco use in social media predicts subsequent smoking behavior. Am J Health Promot. 2015;29(4):259–261. [DOI] [PubMed] [Google Scholar]
- 23. Southwell BG. Social Networks and Popular Understanding of Science and Health: Sharing Disparities. Baltimore, MD: Johns Hopkins University Press; 2013. [Google Scholar]
- 24. Berger J. Arousal increases social transmission of information. Psychol Sci. 2011;22(7):891–893. [DOI] [PubMed] [Google Scholar]
- 25. Thrasher JF, Abad-Vivero EN, Huang L, et al. . Interpersonal communication about pictorial health warnings on cigarette packages: Policy-related influences and relationships with smoking cessation attempts. Soc Sci Med. 2016;164:141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. White V, Webster B, Wakefield M. Do graphic health warning labels have an impact on adolescents’ smoking-related beliefs and behaviours?Addiction. 2008;103(9):1562–1571. [DOI] [PubMed] [Google Scholar]
- 27. Ramanadhan S, Nagler RH, McCloud R, Kohler R, Viswanath K. Graphic health warnings as activators of social networks: A field experiment among individuals of low socioeconomic position. Soc Sci Med. 2017;175:219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brodar KE, Hall MG, Butler EN, et al. . Recruiting diverse smokers: enrollment yields and cost. Int J Environ Res Public Health. 2016;13(12):1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nonnemaker J, Farrelly M, Kamyab K, Busey A, Mann N.. Experimental Study of Graphic Cigarette Warning Labels: Final Results Report.Research Triangle Park, NC: RTI International;2010. [Google Scholar]
- 30. Hall MG, Peebles K, Bach LE, Noar SM, Ribisl KM, Brewer NT. Social Interactions Sparked by Pictorial Warnings on Cigarette Packs. Int J Environ Res Public Health. 2015;12(10):13195–13208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- 32. Hammond D, Fong GT, Borland R, Cummings KM, McNeill A, Driezen P. Text and graphic warnings on cigarette packages: findings from the international tobacco control four country study. Am J Prev Med. 2007;32(3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Borland R, Wilson N, Fong GT, et al. . Impact of graphic and text warnings on cigarette packs: findings from four countries over five years. Tob Control. 2009;18(5):358–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hitchman SC, Driezen P, Logel C, Hammond D, Fong GT. Changes in effectiveness of cigarette health warnings over time in Canada and the United States, 2002-2011. Nicotine Tob Res. 2014;16(5):536–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Thrasher JF, Abad-Vivero EN, Huang L, et al. . Interpersonal communication about pictorial health warnings on cigarette packages: Policy-related influences and relationships with smoking cessation attempts. Social Sci Med. (1982). 2015. 164:141–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kornfield R, Smith KC. Earned media and public engagement with CDC’s “Tips from Former Smokers” campaign: an analysis of online news and blog coverage. J Med Internet Res. 2015;17(1):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hammond D, Wakefield M, Durkin S, Brennan E. Tobacco packaging and mass media campaigns: research needs for Articles 11 and 12 of the WHO Framework Convention on Tobacco Control. Nicotine Tob Res. 2013;15(4):817–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Thrasher JF, Murukutla N, Pérez-Hernández R, et al. . Linking mass media campaigns to pictorial warning labels on cigarette packages: a cross-sectional study to evaluate effects among Mexican smokers. Tob Control. 2013;22(e1):e57–e65. [DOI] [PubMed] [Google Scholar]
- 39. Brennan E, Durkin SJ, Cotter T, Harper T, Wakefield MA. Mass media campaigns designed to support new pictorial health warnings on cigarette packets: evidence of a complementary relationship. Tob Control. 2011;20(6):412–418. [DOI] [PubMed] [Google Scholar]
- 40. David C, Cappella JN, Fishbein M. The social diffusion of influence among adolescents: Group interaction in a chat room environment about antidrug advertisements. Communication Theory. 2006;16(1):118–140. [Google Scholar]
- 41. Hall MG, Sheeran P, Noar SM, Ribisl KM, Boynton MH, Brewer NT. A brief measure of reactance to health warnings. J Behav Med. 2017:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, Brewer NT. The impact of strengthening cigarette pack warnings: Systematic review of longitudinal observational studies. Soc Sci Med. 2016;164:118–129. [DOI] [PMC free article] [PubMed] [Google Scholar]