Introduction
Microscopic hematuria is a common clinical problem and a frequent reason for urologic referral, accounting for up to 6% of new patients in some practices.1 Standard workup typically includes noninvasive upper urinary tract imaging such as ultrasound, or computed tomography (CT). For cases where standard imaging work up is inconclusive, more invasive techniques such as cystoscopy and ureteroscopy are often employed.2 CT Urography (CTU) is a sensitive, non-invasive radiologic exam to evaluate the upper urinary tract for common etiologies of hematuria. Although literature on the subject is lacking, CTU may also be useful for diagnosing rarer vascular causes of benign hematuria and could reduce the need for more invasive diagnostic exams in such cases.
Arteriovenous malformation (AVM) of the upper urinary tract is a rare cause of hematuria.2 AVM can occur throughout the upper urinary tract, though ureteral cases of AVM are particularly rare. The few existing case reports of ureteral AVM have been diagnosed by ureteroscopy and biopsies.3, 4, 5 While ureteroscopy has the advantage of being both diagnostic and therapeutic, invasive studies may not be necessary or desirable in cases of asymptomatic AVM associated hematuria.
Advanced non-invasive upper urinary tract imaging techniques such as CTU and MRI are often employed for patients with hematuria and a negative initial urologic workup. These imaging modalities should theoretically be able to identify even small vascular lesions; however, there are no existing reports describing radiologic diagnosis of ureteral AVM. Here we present the first case report of a ureteral AVM diagnosed by CTU. This case highlights the increased sensitivity of modern upper urinary tract imaging and demonstrates the advantages of a non-invasive approach to the diagnosis of a rare cause of hematuria.
Case presentation
A 60-year-old Caucasian female presented with a nearly 5-year history of microscopic hematuria of unclear etiology despite a complete urologic workup approximately 3 years prior. She was asymptomatic with no complaints of pain or urinary symptoms. Standard laboratory studies including complete blood count, coagulation profile, serum electrolytes, and creatinine were normal. Urinalysis was remarkable only for microscopic hematuria. Urine culture was negative. After an unrevealing cystoscopy, CTU was ordered to evaluate the upper urinary tract.
CTU was performed according to institutional standards and included three acquisitions consisting of contiguous 1.25 mm axial images from to dome of the liver through the pelvis: 1) prior to intravenous contrast administration (non-contrast), 2) approximately 80 seconds post contrast (nephrographic phase), and 3) approximately 10 minutes post contrast (excretory/pyelographic phase). Coronal and sagittal reformations were also obtained. Non-contrast images showed no evidence of nephrolithiasis. On post-contrast images, the kidneys demonstrated normal symmetric contrast enhancement and showed no significant abnormality other than a few benign appearing renal cysts (Bosniak category I and II). Both ureters were normal in caliber with no abnormal dilation or narrowing.
Nephrographic phase images demonstrated a tangle of tortuous blood vessels surrounding the proximal to mid left ureter (Fig. 1). Further evaluation revealed a feeding artery, originating from the left renal artery, and two major veins draining to the inferior vena cava and left common iliac vein (Fig. 2). The AVM was quite extensive, encasing an approximately 4 cm segment of the ureter (Fig. 3A and B). On excretory phase images, both ureters opacified normally without evidence of intra-ureteral filling defects (Fig. 3, C). The diagnosis of ureteral AVM was made based on characteristic imaging features and an otherwise negative workup for hematuria. Given the absence of symptoms or concerning laboratory abnormalities, the patient elected not to seek further diagnostic or therapeutic intervention.
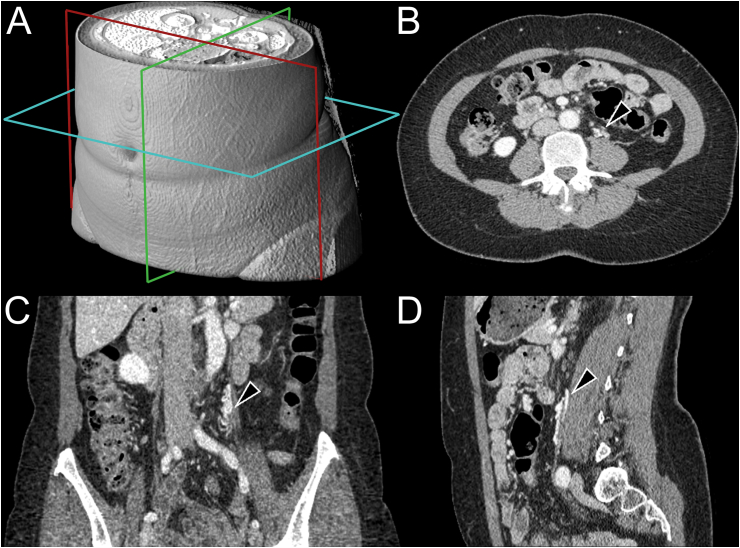
Fig. 1.
Nephrographic phase contrast enhanced abdominopelvic CT in axial (B), coronal (C), and sagittal planes demonstrate a tangle of vessels surrounding the left ureter (black arrowheads). Slice locations are indicated on a three-dimensional volume rendering of the CT data (A).
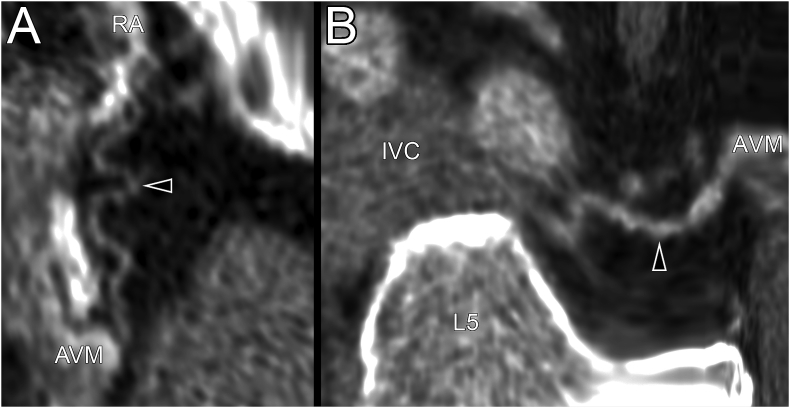
Fig. 2.
Curved plane reformats of the nephrographic phase CT showing the course of the AVM's feeding artery (A, black arrowhead) originating from the renal artery (RA) and a draining vein (B, black arrowhead) draining directly to the inferior vena cava (IVC). The L5 vertebral body is labeled for orientation.
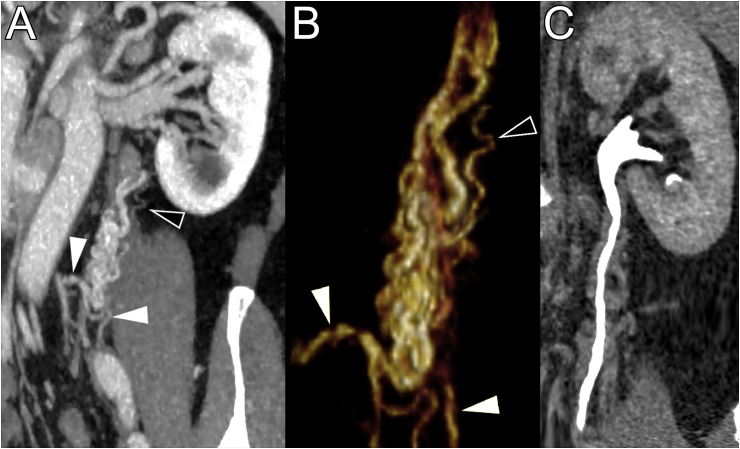
Fig. 3.
A: oblique coronal 5 mm maximum intensity projection of the nephrographic phase acquisition demonstrating the tangle of tortuous vessels encasing the left ureter. B: three-dimensional volume rendering of the ureteral AVM derived from 1.25 mm slice thickness nephrographic phase CT. The feeding artery (black arrowheads) and two early draining veins (white arrowheads) are identified. C: excretory phase imaging showing a patent left ureter without evidence of an intraluminal lesion.
Discussion
Ureteral AVM is a known cause of hematuria that has been described in only a small number of prior case reports.2, 3, 4, 5 The diagnosis of AVM can be confirmed by catheter angiography or histology; however, as our case demonstrates, CTU can also diagnose ureteral AVM when characteristic imaging features are seen. In this case, the presence of a feeding artery and draining veins, and the presence of characteristic contrast enhancement and washout were sufficient to diagnose AVM.
The AVM described is significantly larger than previously described lesions, measuring up to four times the linear dimensions.3 Despite the extent of this AVM, our patient was essentially asymptomatic, while prior reports have described more dramatic clinical presentations including flank pain, gross hematuria, and anemia.3, 4, 5 Differences in clinical presentation likely relate to differences in lesion location; previous reports describe pedunculated intra-ureteral lesions, while our patient's lesion was predominantly extra-ureteral without ureteral filling defects on excretory phase images.
A limitation of this report is the lack of confirmatory studies such as ureteroscopy or catheter angiography. Further testing was unnecessary in this case due to the presence of diagnostic imaging features and the lack of symptoms requiring treatment. While CTU is recognized as an accurate examination for the detection of the more common causes of hematuria, such as urolithiasis and urothelial neoplasms, this case illustrates that vascular causes of hematuria can also be diagnosed by CTU without the need for angiographic examinations. CTU can therefore reduce the need for invasive diagnostic testing or for additional noninvasive examinations, such as CT angiography, in certain cases.
Conclusion
While most cases of hematuria can be diagnosed with a standard urologic workup, rarer etiologies can be a diagnostic challenge. Previous work has highlighted the role of ureteroscopy, however invasive studies may not always be necessary. This case demonstrates the use of CTU for diagnosis of ureteral AVM, a rare vascular cause of hematuria. Both radiologists and urologists should be aware that CTU can be used to diagnose vascular lesions of the urinary tract without the need for invasive studies or more targeted imaging studies such as CT angiography. In this case, the patient was able to forego invasive ureteroscopy, and potentially avoid associated complications. While ureteroscopy is unlikely to be supplanted, it seems reasonable to expect that non-invasive ureteral imaging studies like CTU will become increasingly important for diagnosing upper urinary tract abnormalities.
References
- 1.Grossfeld G.D., Carroll P.R. Evaluation of asymptomatic microscopic hematuria. Urol Clin. 1998;25(4):661–676. doi: 10.1016/s0094-0143(05)70055-0. [DOI] [PubMed] [Google Scholar]
- 2.Rowbotham C., Anson K.M. Benign lateralizing haematuria: the impact of upper tract endoscopy. BJU Int. 2001;88(9):841–849. doi: 10.1046/j.1464-4096.2001.01228.x. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan S.A., Brown W., Bixon R., O'Toole K., Benson M.C. Arteriovenous malformation of ureter. Urology. 1992;40(5):450–452. doi: 10.1016/0090-4295(92)90462-6. [DOI] [PubMed] [Google Scholar]
- 4.Tang C.N., Law I.C., Iu P.P., Yip A.W. Arteriovenous malformation of the ureter–a rare cause of haematuria. Br J Urol. 1997;80(3):500–501. doi: 10.1046/j.1464-410x.1997.00384.x. [DOI] [PubMed] [Google Scholar]
- 5.Donkelaar Ten C.S., Houwert A.C., Kate Ten F.J.W., Lock M.T.W.T. Polypoid arteriovenous malformation of the ureter mimicking a fibroepithelial polyp, a case report. BMC Urol. 2017;17(1):55. doi: 10.1186/s12894-017-0237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]