Abstract
Background:
Laparoscopic bariatric surgeries in morbid obese patients may be associated with atelectasis, hypercapnia, and hypoxemia, intra and postoperatively. Several strategies are used for the prevention of these consequences. This study aimed to examine the effects of three different recruitment maneuvers comparatively during surgery and the influence of the maneuvers on some cardiopulmonary indices.
Materials and Methods:
In a clinical trial, ninety participants of laparoscopic surgery with body mass index higher than 40 were randomly divided into three equal groups. The first group was subject to 10 cmH2O positive end-expiratory pressure (PEEP) during surgery, the second group, after venting the pneumoperitoneum, had 5 deep breaths with a positive pressure of 40 cmH2O, and the third group was subject to both. Some pulmonary and hemodynamic parameters were measured every 15 min and compared between three groups.
Results:
The average of peak airway pressure, plateau airway pressure, and SpO2 static and dynamic compliance between the three groups had no meaningful differences (P > 0.05), but PaCO2in the second group was statistically higher than the other two groups (P < 0.05).
Conclusion:
Multiple deep breaths alone are not as effective as PEEP or PEEP plus MDB in preventing adverse pulmonary effects in laparoscopic bariatric surgeries of morbid obese patients.
Keywords: Laparoscopy, morbid obesity, recruitment maneuver
Introduction
Morbid obesity, which is characterized by body mass index (BMI) higher than 40, has become a global health-care problem.[1] This hygienic problem is considered multifactorial, and factors such as psychological, lifestyle, biologic, nutrition, and inactivity are influential.[2]
One of the treatments for morbid obese patients is bariatric surgery. This surgery is often associated with intra- and post-operative pulmonary complications and respiration become highly disturbed in these patients.[3,4] This disorder is the result of different factors including the position of patient during surgery, the prescription of muscle relaxants, and pneumoperitoneum (which results in the reduction of FRC, closing volume, and atelectasis).[5,6]
As a result, the risk of pulmonary complications increases in the postoperative period and during hospitalization.[7,8] Different approaches have been studied to improve gas exchange during surgery such as using higher levels of tidal volume, more breaths or both,[9] using positive end-expiratory pressure (PEEP)[10] and finally putting the patient in reverse Trendelenburg position.[11]
Application of 40 cmH2O inspiratory pressure for 15 s followed by PEEP has been used in morbid obese patients in open bariatric surgery as a successful method for increasing oxygenation in this setting.[12]
In another study by Almarakbi et al., sixty laparoscopic gastric bounding surgeries in obese patients with BMI >30 compared for four different ventilation approaches including 10 cmH2O PEEP, 40 cmH2O inspiratory maneuver for 15 s, the same inspiratory maneuver plus PEEP, and the repetition of inspiratory maneuver every 10 min; they concluded that the fourth strategy has the best compliance and PaO2 during surgeries.[13]
Regarding the limitations of the above-mentioned studies (not considering most of the patients as morbid obese [BMI >40], using 30% oxygen and the hemodynamic fluctuation in the group with higher compliance), this study designed to compare three ventilation approaches (recruitment maneuvers) and determine the influence of these maneuvers on cardiopulmonary indices.
Materials and Methods
This study approved by Ethics Committee of vice research of medical school of Isfahan University of medical sciences (reference number IR.MUI.REC.1394.3.670). In a randomized clinical trial, candidate morbid obese patients for laparoscopic bariatric surgery in Al-Zahra Medical Center from October 2015 to August 2016 enrolled to the study.
The including criteria were ages between 15 and 65 years old, American Society of Anesthesiologists 1 and 2 and BMI ≥40, no smoking, normal intracranial pressure, and finally no pulmonary disease (obstructive or restrictive) and exclusion criteria were change surgery plan to open surgery and bleeding more than 10 cc/kg of the lean body weight (LBW).
After obtaining informed written consent, patients remained nil per os for 8–10 h. They took 10 cc/kg (LBW) of Ringer's solution during 90 min before surgery. Then, standard monitoring including electrocardiogram, SpO2, and blood pressure was hooked to patients and basic vital signs were measured.
Anesthesia induced by intravenous prescription of 3 μg/kg fentanyl (TRITTAU-Germany), 2–3 mg midazolam (Exir - Broojerd, Iran), 1.5 mg/kg propofol (Fresenius kabi Austria), and 1.5 mg/kg Cisatracurium (Daroupakhsh-Tehran Iran), and after 4 min ventilation by 100% oxygen, trachea was intubated by 7.5 internal diameter polyvinyl chloride tracheal tube. Then, patient ventilated by 10 cc/kg tidal volume and respiratory rate at 10 breaths/min. Respiratory rate adjusted every 5–10 min to kept end-tidal CO2 (EtCO2) between 35 and 40 mmHg.
Anesthesia was maintained by 100–200 μg/kg/min propofol and 0.2 mg/kg of cisatracurium every 30 min. Moreover, 0.15 mg/kg (LBW) morphine (Darou Pakhsh - Tehran, Iran) was used to relief pain during the surgery. At the end of the surgery, 0.40 mg/kg of prostigmine (Caspian – Tamin, Iran) and 0.2 mg/kg atropine (Darou Pakhsh – Tehran, Iran) were used for reversing of muscle relaxant effects.
Ten minutes after inducing pneumoperitoneum (gas insufflation), the patients were divided into three groups using computerized randomization list and according to the considered group; intervention was made as follows: Group 1 or PEEP (P): patients received 10 cmH2O PEEP from the beginning to the end of the surgery and Group 2 or multiple deep breaths (MDBs): patients were received five breaths with positive pressure of 40 cmH2O with 5 s of pauses and 5 s intervals as expiration at the end of surgery and after desufflation (venting) pneumoperitoneum.
Group 3 or PEEP plus MDB (PMDB): Like Group P, patients had 10 cmH2O PEEP, and after venting the abdomen, the same MDB as group MDB was performed.
Before insufflation of gas into peritoneum, the patients were put in 15°C head down position and, after initiation of pneumoperitoneum, the patients were shifted to 30°C head up position slowly, the position was kept until the end of surgery. Intra-abdominal pressure maintained between 15 ± 3 cmH2O during surgery.
At the end of the surgery, infusion of propofol was stopped and the effect of muscle relaxants eliminated by reverse drugs, extubation was done after full awakening, and patients transferred to postanesthesia care unit (PACU).
During the transferring and care in PACU, the patient was maintained in 15–30 head up position and was receiving oxygen with the flow of 5–8 L/min. SpO2, heart rate (HR), and mean arterial pressure (MAP) were measured every 15 min for 2 h in PACU.
The data were analyzed by SPSS (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp) The analyses consisted of repeated measured analysis, ANOVA, and Pearson's Chi-square test and differences considered significant at P ◻ 5%.
Results
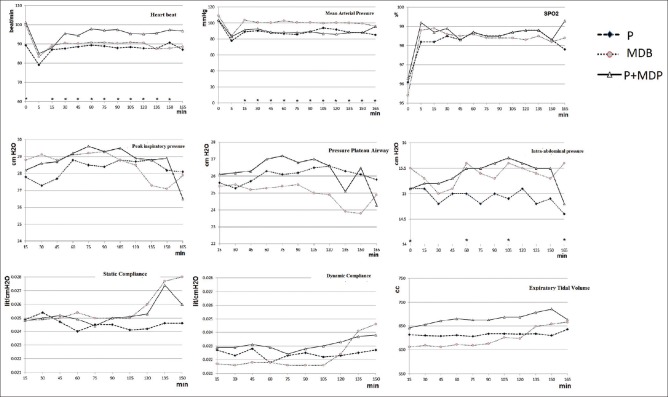
The mean of demographic indexes such as age, weight, height, and BMI of the three groups had no meaningful difference (P > 0.05); frequency distribution of sex among the groups was the same either (P = 0.812), male/female were 6 (20%)/24 (80%) in Group P, 7 (23.3%)/23 (76.7%) in Group MDB, and 5 (16.7%)/25 (83.3%) in Group PMDB. The results showed no meaningful difference in surgery mean time and stay in PACU among the groups (P > 0.05). The comparison of the mean of SpO2, MAP, and HR before anesthesia demonstrated that the mean of SpO2, MAP before anesthesia had no meaningful difference between groups (P > 0.05), and the mean of HR before anesthesia for Group P was meaningfully lower than the other two groups (P = 0.001 < 0.05). The mean of total HR and the mean of arterial pressure had a meaningful difference [Table 1 and Figure 1].
Table 1.
Total mean, standard deviation, and the statistical comparison results of hemodynamic and respiratory indices in three groups of study
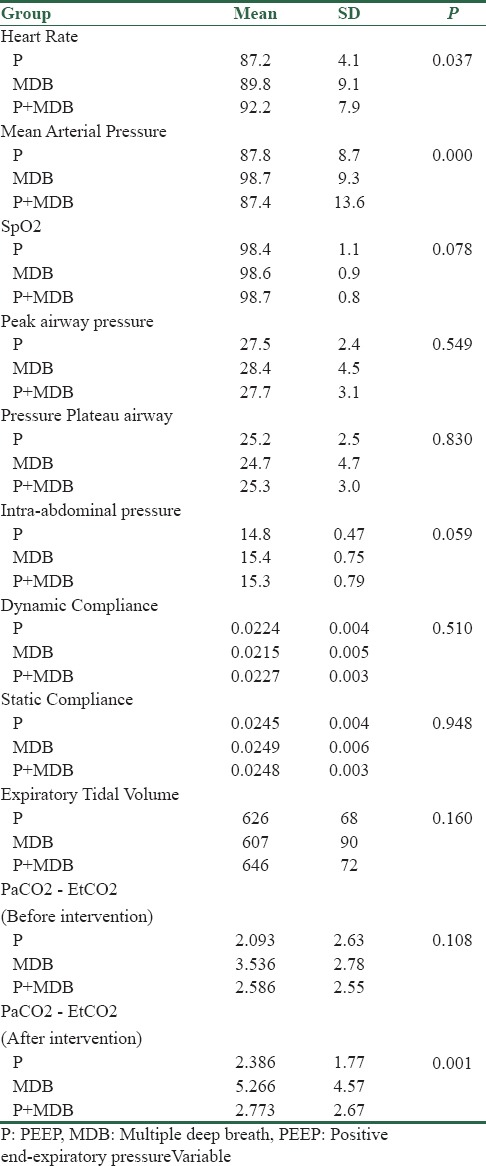
Figure 1.
Diagram of changes of hemodynamic and respiratory indices during the study in three groups. (P: PEEP, MDP: Multiple deep breath, P+MDP: PEEP plus multiple breath)
Peak and plateau airway pressures and intra-abdominal pressure had no statistical meaningful difference in terms of total mean [Table 1].
Intra-abdominal pressure immediately, 60, 105, and 165 min after insufflation had a meaningful difference, in such a way that the mean intra-abdominal pressure in all the mentioned intervals was meaningfully higher in Group MDB compared with Group P.
The three groups had no statistical meaningful differences concerning the total mean of dynamic and static pulmonary compliance and expiratory tidal volume [Table 1]. Comparing the three mentioned variables, we observed no meaningful statistical difference in the intervals [Figure 1].
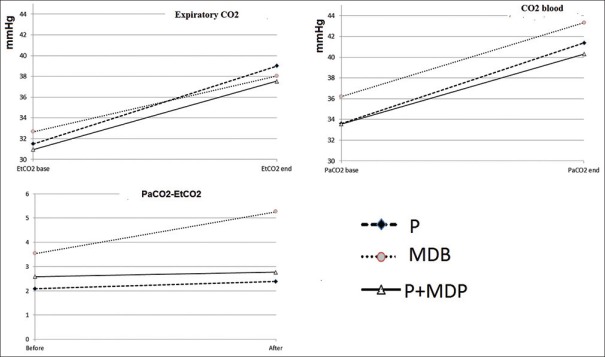
By comparing PaCO2 mean and the difference between EtCO2 and PaCO2, 5 min after anesthesia, and 10 min after desufflation abdominal gas, it was observed that the mean of PaCO25 min after anesthesia and 10 min after venting gas had a meaningful difference among the groups (P < 0.05); in such a way that in the mentioned time, for Group MDB, the mean of PaCO2 was meaningfully higher than the other two groups. The mean difference between EtCO2 and PaCO2 had a meaningful difference among the groups only 10 min after venting gas (P = 0.001 < 0.05); at this time, the difference of Group MDB was meaningfully higher than the other two groups [Table 1 and Figure 2].
Figure 2.
Diagram of changes of PaCO2, P end-tidal CO2 (EtCO2) and PaCO2-EtCO2, before and after intervention in three groups of study (P: PEEP, MDP: Multiple deep breath, P+MDP: PEEP plus multiple breath)
Comparing the mean of SpO2 and MAP during care in PACU showed that the mean of SpO2 and MAP had no significant difference among the groups (P > 0.05) [Table 2].
Table 2.
Mean, standard deviation, statistical analysis results of SpO2, and mean arterial pressure during care in postanesthesia care unit for the groups
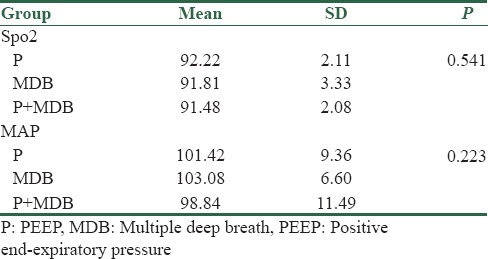
By comparing the mean of urine output and the amount of used liquid for 1, 2, 3, and 4 h for the three groups, it was observed that the mean of urine output had meaningful difference only in the 1st h (P = 0.013 < 0.05), in such a way that the mean of urine output/hour for group PMDB was less than Group P, the mean of used liquid had no meaningful difference in the hours mentioned [Figure 3].
Figure 3.
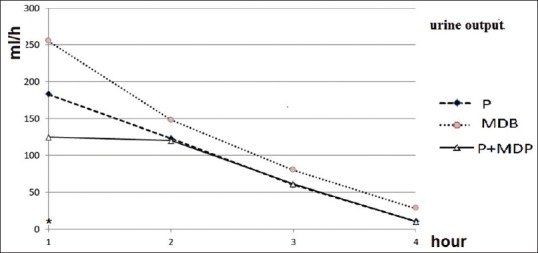
Diagram of urine output volume during surgery in three groups of study (P: PEEP, MDP: Multiple deep breath, P+MDP: PEEP plus multiple breath)
Discussion
The study showed that the mean of MAP for Group MDB was meaningfully higher than other groups, it can be referred to effects of PEEP (which were applied to two other groups) on decreasing preload and thereafter cardiac output and blood pressure (effects of deep breath maneuver on decreasing preload was hidden by effects of longer period of application of PEEP in other groups). The same as our results, Póvoa et al. claimed that MAP of group MDB is higher.[14] However, unlike our results, Santa Cruz et al. reported findings, in which MAP was the same among the groups and had no significant difference.[15]
There was no meaningful difference among the groups regarding peak airway pressure (PAP) and SpO2 as well as EVT. Choi et al. found similar levels of SpO2 in comparison of PEEP (8 cmH2o) and recruitment maneuver (multiple deep positive pressure ventilation) followed by PEEP during one lung ventilation.[16] While Pirrone et al. in their study on morbidly obese patients showed that the positive end-expiratory pressure levels of 11.6 ± 2.9 cmH2O in comparison to recruitment plus PEEP were associated with lower oxygenation [17] and Futier et al. concluded that recruitment plus PEEP improves respiratory mechanics and oxygenation during pneumoperitoneum whereas PEEP alone did not.[18]
HR is another case of our investigation and it is clear that HR of Group PMDB was meaningfully higher than the other groups; this can be discussed by summation of effects of PEEP and deep positive pressure breaths on decreasing preload and blood pressure and then activation of baroreceptors in this group. de Souza et al. in a study on adult patients with Grade III obesity who underwent bariatric surgery did not find meaningful differences in HR between patients whom treated by PEEP and recruitment maneuvers.[19]
There were no meaningful differences between the groups concerning dynamic and static compliances while Almarakbi et al.[13] showed that dynamic and static compliances of patients whom took recruitment plus PEEP (albeit with repeated recruitment) had better lung compliance in comparison to PEEP or recruitment alone.
There is a significant difference for Group MDB regarding the changes of PaCO2-EtCo2; this difference can show the decrease of alveolar capillary exchange level because of atelectasis although this change was not observed in SpO2; it is probably because of ventilating of lungs by 100% oxygen.
Based on the obtained results of this study, applying PEEP (10 cmH2O), recruitment alone (5 deep breath till PAP of 40 cmH2O) after desufllation of intra-abdominal gas and combination of both are comparable in their effects on PAP, plateu airway pressure, (Plat AP), expiratory tidal volume (EVT), and SpO2 and the mean of dynamic and static compliances during laparoscopic bariatric surgeries in morbid obese patients, but according to changes of PaCO2 and EtCO2-PaCO2 gap, the recruitment alone is not as effective as two other strategies.
Conclusion
Recruitment alone (5 deep breath till PAP of 40 cmH2O) after desufllation of intra-abdominal gas is not as effective as PEEP or Recruitment plus PEEP in maintaining EtCO2-PaCO2 gap.
Financial support and sponsorship
This work was done under financial support of vice Research of Medical School of Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Forgiarini Júnior LA, Rezende JC, Forgiarini SG. Alveolar recruitment maneuver and perioperative ventilatory support in obese patients undergoing abdominal surgery. Rev Bras Ter Intensiva. 2013;25:312–8. doi: 10.5935/0103-507X.20130053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salome CM, King GG, Berend N. Physiology of obesity and effects on lung function. J Appl Physiol. 2010;108:206–11. doi: 10.1152/japplphysiol.00694.2009. [DOI] [PubMed] [Google Scholar]
- 3.Dumont L, Mattys M, Mardirosoff C, Vervloesem N, Allé JL, Massaut J. Changes in pulmonary mechanics during laparoscopic gastroplasty in morbidly obese patients. Acta Anaesthesiol Scand. 1997;41:408–13. doi: 10.1111/j.1399-6576.1997.tb04707.x. [DOI] [PubMed] [Google Scholar]
- 4.Casati A, Comotti L, Tommasino C, Leggieri C, Bignami E, Tarantino F, et al. Effects of pneumoperitoneum and reverse Trendelenburg position on cardiopulmonary function in morbidly obese patients receiving laparoscopic gastric banding. Eur J Anaesthesiol. 2000;17:300–5. doi: 10.1046/j.1365-2346.2000.00662.x. [DOI] [PubMed] [Google Scholar]
- 5.Hedenstierna G, Edmark L. The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med. 2005;31:1327–35. doi: 10.1007/s00134-005-2761-7. [DOI] [PubMed] [Google Scholar]
- 6.Hedenstierna G, Rothen HU. Atelectasis formation during anesthesia: Causes and measures to prevent it. J Clin Monit Comput. 2000;16:329–35. doi: 10.1023/a:1011491231934. [DOI] [PubMed] [Google Scholar]
- 7.Pelosi P, Croci M, Ravagnan I, Vicardi P, Gattinoni L. Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest. 1996;109:144–51. doi: 10.1378/chest.109.1.144. [DOI] [PubMed] [Google Scholar]
- 8.Putensen-Himmer G, Putensen C, Lammer H, Lingnau W, Aigner F, Benzer H. Comparison of postoperative respiratory function after laparoscopy or open laparotomy for cholecystectomy. Anesthesiology. 1992;77:675–80. doi: 10.1097/00000542-199210000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Sprung J, Whalley DG, Falcone T, Wilks W, Navratil JE, Bourke DL. The effects of tidal volume and respiratory rate on oxygenation and respiratory mechanics during laparoscopy in morbidly obese patients. Anesth Analg. 2003;97:268–74. doi: 10.1213/01.ane.0000067409.33495.1f. [DOI] [PubMed] [Google Scholar]
- 10.Pelosi P, Ravagnan I, Giurati G, Panigada M, Bottino N, Tredici S, et al. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology. 1999;91:1221–31. doi: 10.1097/00000542-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Perilli V, Sollazzi L, Bozza P, Modesti C, Chierichini A, Tacchino RM, et al. The effects of the reverse trendelenburg position on respiratory mechanics and blood gases in morbidly obese patients during bariatric surgery. Anesth Analg. 2000;91:1520–5. doi: 10.1097/00000539-200012000-00041. [DOI] [PubMed] [Google Scholar]
- 12.Chalhoub V, Yazigi A, Sleilaty G, Haddad F, Noun R, Madi-Jebara S, et al. Effect of vital capacity manoeuvres on arterial oxygenation in morbidly obese patients undergoing open bariatric surgery. Eur J Anaesthesiol. 2007;24:283–8. doi: 10.1017/S0265021506001529. [DOI] [PubMed] [Google Scholar]
- 13.Almarakbi WA, Fawzi HM, Alhashemi JA. Effects of four intraoperative ventilatory strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese patients. Br J Anaesth. 2009;102:862–8. doi: 10.1093/bja/aep084. [DOI] [PubMed] [Google Scholar]
- 14.Póvoa P, Almeida E, Fernandes A, Mealha R, Moreira P, Sabino H. Evaluation of a recruitment maneuver with positive inspiratory pressure and high PEEP in patients with severe ARDS. Acta Anaesthesiol Scand. 2004;48:287–93. doi: 10.1111/j.0001-5172.2004.0305.x. [DOI] [PubMed] [Google Scholar]
- 15.Santa Cruz R, Rojas JI, Nervi R, Heredia R, Ciapponi A. High versus low positive end-expiratory pressure (PEEP) levels for mechanically ventilated adult patients with acute lung injury and acute respiratory distress syndrome. Cochrane Database Syst Rev. 2013;6:CD009098. doi: 10.1002/14651858.CD009098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi YS, Bae MK, Kim SH, Park JE, Kim SY, Oh YJ. Effects of alveolar recruitment and positive end-expiratory pressure on oxygenation during one-lung ventilation in the supine position. Yonsei Med J. 2015;56:1421–7. doi: 10.3349/ymj.2015.56.5.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pirrone M, Fisher D, Chipman D, Imber DA, Corona J, Mietto C, et al. Recruitment maneuvers and positive end-expiratory pressure titration in morbidly obese ICU patients. Crit Care Med. 2016;44:300–7. doi: 10.1097/CCM.0000000000001387. [DOI] [PubMed] [Google Scholar]
- 18.Futier E, Constantin JM, Pelosi P, Chanques G, Kwiatkoskwi F, Jaber S, et al. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology. 2010;113:1310–9. doi: 10.1097/ALN.0b013e3181fc640a. [DOI] [PubMed] [Google Scholar]
- 19.de Souza AP, Buschpigel M, Mathias LA, Malheiros CA, Alves VL. Analysis of the effects of the alveolar recruitment maneuver on blood oxygenation during bariatric surgery. Rev Bras Anestesiol. 2009;59:177–86. doi: 10.1590/s0034-70942009000200005. [DOI] [PubMed] [Google Scholar]