Introduction
Superficial vein thrombosis is a rare pathology that was first described by Mordor,1 although his description of phlebitis was observed exclusively at the thoracic wall. In 1955, Braun-Falco described penile thrombosis and later superficial penile vein thrombosis was first reported by Helm and Hodge.2 Mondor's disease of the penis is a rare entity with a reported incidence of 1.39%. It is described most of the time as a self-limited disease however it causes great morbidity to the patient who suffers from it. The pathogenesis of Mondor's disease is unknown. Its diagnosis is based on clinical signs such as a cordlike induration on the dorsal face of the penis, and imaging studies, doppler ultrasound is the instrument of choice. Treatment is primarily symptomatic but some cases may require surgical management however an accurate diagnostic resolves almost every case. We will describe the symptoms, diagnosis, and treatment of superficial thrombophlebitis of the dorsal vein of the penis.
Case presentation
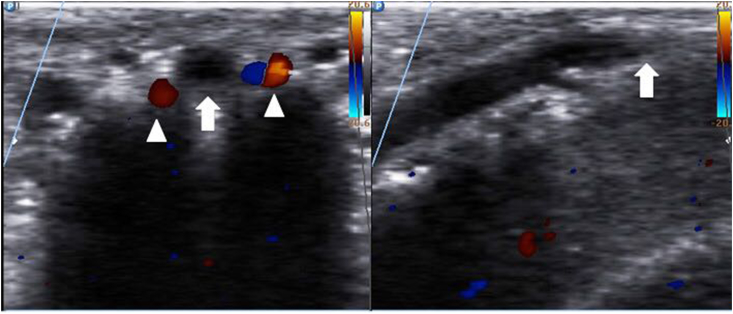
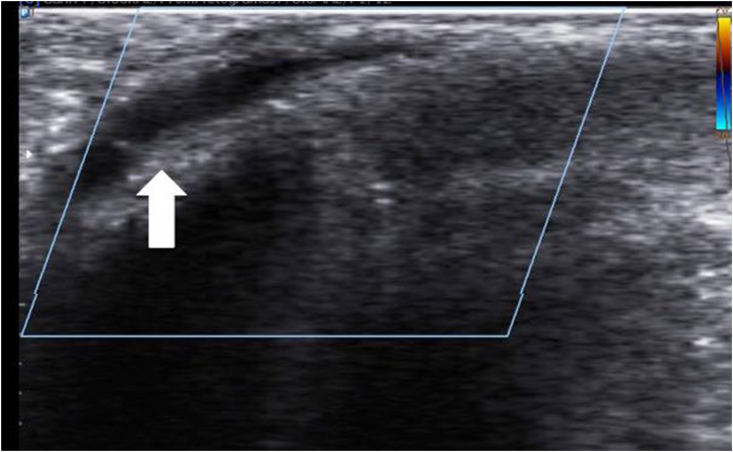
A 56 year-old male patient is admitted into the emergency room due to pain in the middle third of his penis which had been ongoing for 15 days prior to admission. He also complained of dysuria and strangury; he denied fever or transurethral discharge. He is obese, has no important family history, and is a chronic user of nonsteroidal anti-inflammatory drugs and tramadol for lumbar spine arthropathy. The physical exam reveals an indurated and painful 1 cm cord on the dorsal surface of the penis. Pain was referred by the patient as a score 9/10 on a visual analog scale, located to the middle third of the penis and accompanied by vomit only once. The laboratories showed an elevated white blood cell (WBC) count (however there was no fever) and normal urine analysis; the rest of the results were unremarkable. Treatment was started with analgesic drugs and antibiotics. A few hours later, pain persisted with minimal improvement so a Doppler ultrasound was done. The ultrasound identified a noncompressible superficial vein of the penis on the site of the cord, data consistent with the diagnosis of venous thrombosis; the rest of the vein's trajectory was permeable (Fig. 1, Fig. 2). Low Molecular Weight Heparin (LMWH) was indicated for 7 days along with a third generation cephalosporin and etoricoxib for definitive treatment, patient had pain relief of 80% within the first 24 hours; the pain resolved completely 3 weeks after treatment was started.
Fig. 1.
Color Doppler ultrasound of the penile shaft (left) show the absence of a flow signal in the SDPV (arrow) and a flow signal in both of the dorsal penile arteries (arrowheads), (right) thrombosis of the superficial dorsal vein of the penis. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Doppler ultrasound image showing noncompressible superficial vein compatible with superficial penile vein thrombosis.
Discussion
Thrombosis of superficial veins were first described by Mondor in the year 1939, referring to veins of the thoracic wall exclusively.1 Venous thrombosis of the penis was described by Hodge in 1958. Mondor's disease (MD) refers to the thrombosis of the superficial dorsal vein of the penis2; it is a rare disease with a reported incidence of 1.39%.3 It is considered as self-limited, but it puts great stress on the patient who suffers it and most of the cases are not diagnosed correctly. Mondor's disease usually happens in men between the ages of 21–70 years-old. It usually presents as a painful cord or fibrotic area in the dorsal surface of penis accompanied by intense pain. Only in some cases is it possible to identify its etiology. The etiology of Mondor disease is unknown but has been associated with many factors such as sexual activity, prolonged abstinence periods, direct trauma to the penis, penis injections, other venous thrombosis, cancer, previous surgical hernia repair, infection, and deficiency of S and C proteins and antithrombin III (found in 15%–20% of all families with thrombophilia4). Sclerosing lymphangitis and peyronies disease both need to be considered in the differential diagnosis of a painful, fibrotic lesion of the penis. The diagnosis is based on the clinical history and physical examination while the gold standard for imaging is the Doppler ultrasonography which identifies the area of the thrombus, its extension, and the unambiguous data of thrombosis: a non-compressible vein with venous flow absence. More invasive studies tend to be unnecessary for the diagnosis of this disease unless some etiopathogenic causes are suspected, such as cancer or trauma or thrombophilia. In this case, we considered the following to be triggering factors: obesity, his work labor and frequent use of a saddle, although he had no history of acute trauma. The management consists in the control of pain, use of LMWH in some occasions, antibiotics, and treatment of the causal etiology if identified. In this particular case, the treatment used was clexane (enoxaparin) for seven days, etoricoxib and a third generation cephalosporin. There are some reports on the use of surgical thrombectomy in Mondor's disease in recurrent cases or in cases that do not improve with conservative treatment.5
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eucr.2018.04.003.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Mondor H. Tronculite sous-cutanée subaiguë de la paroi thoragigue antéro-latérale. Mem Acad Chir. 1939;65:1271–1278. [Google Scholar]
- 2.Helm J., Hodge I. Thrombophlebitis of a dorsal vein of the penis: report of a case treated by phenylbutazone (Butazolidin) J Urol. 1958;79:306–307. doi: 10.1016/S0022-5347(17)66273-6. [DOI] [PubMed] [Google Scholar]
- 3.Kumar B., Narang T., Radotra B.D., Gupta S. Mondor's disease of penis: a forgotten disease. Sex Transm Infect. 2005;81:480–482. doi: 10.1136/sti.2004.014159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Mwalad M., Loertzer H., Wicht A., Fornara P. Subcutaneous penile vein thrombosis (penile Mondor's disease): pathogenesis, diagnosis, and therapy. Urology. 2006;67:586–588. doi: 10.1016/j.urology.2005.09.054. [DOI] [PubMed] [Google Scholar]
- 5.Shapiro R.S. Superficial dorsal penile vein thrombosis (penile Mondor's phlebitis): ultrasound diagnosis. J Clin Ultrasound. 1996;24:272–274. doi: 10.1002/(SICI)1097-0096(199606)24:5<272::AID-JCU8>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.