Abstract
Stress is critically involved in the development and progression of disease. From the stress of undergoing treatments to facing your own mortality, the physiological processes that stress drives have a serious detrimental effect on the ability to heal, cope and maintain a positive quality of life. This is becoming increasingly clear in the case of neurodegenerative diseases. Neurodegenerative diseases involve the devastating loss of cognitive and motor function which is stressful in itself, but can also disrupt neural circuits that mediate stress responses. Disrupting these circuits produces aberrant emotional and aggressive behavior that causes long-term care to be especially difficult. In addition, added stress drives progression of the disease and can exacerbate symptoms. In this review, I describe how neural and endocrine pathways activated by stress interact with ongoing neurodegenerative disease from both a clinical and experimental perspective.
Keywords: Alzheimer's disease, Stress, Cortisol, Corticosteroids, CRF, CRH
“Every stress leaves an indelible scar, and the organism pays for its survival after a stressful situation by becoming a little older”Hans Selye (1950)
1. The relationship between stress and neurodegenerative disease – the Vicious Cycle of Stress
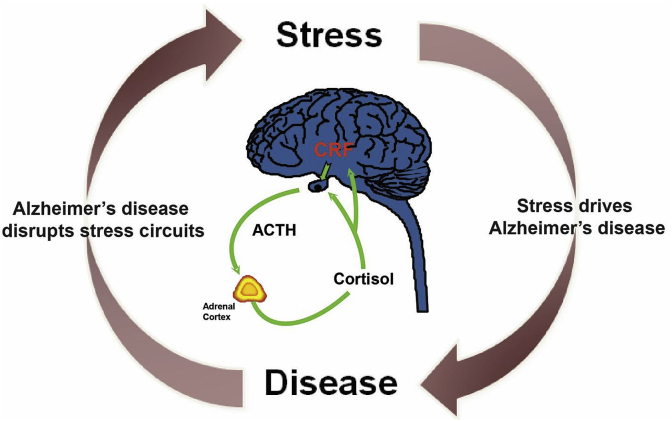
Since the time of Selye, we have known that excessive levels of stress can cause and exacerbate disease, in large part through the activation of the Hypothalamic-Pituitary-Adrenal (HPA) axis which elevates circulating corticosteroid (Cort) levels. This produces a constellation of symptoms that occur in response to any form of stress, which he terms the “general adaptation syndrome” (Selye, 1950). With recent advances, we have come to more fully understand both how stress exacerbates disease symptoms and drives disease progression, and how diseases disrupt stress responses to produce neuropsychiatric symptoms. I term this feed-forward relationship between stress and disease, “The Vicious Cycle of Stress” (Fig. 1).
Fig. 1.
The Vicious Cycle of Stress. On the right arc of the cycle, elevated stress exacerbates Alzheimer's Disease, causing more rapid development of pathology and loss in cognitive function. On the left arc of the cycle, disease perturbs stress responsive neural circuits, producing neuropsychiatric co-morbidities, including depression, anixety, and aggressive behavior. The HPA axis (center), in which hypothalamic CRF activates pituitary ACTH release and subsequent Cortisol release by the adrenal cortex, has a central role in both the exacerbation of AD by stress, and the stress-related symptoms caused by ongoing neurodegeneration.
In the Vicious Cycle of Stress, the right arc of the cycle represents the influence of stress on disease. Countless studies have experimentally demonstrated the negative impact stress has on disease progression, from cancer to cardiovascular disease, neurodegenerative disease and symptoms of aging (for review, see: Bjorntorp, 1997; Wahrborg, 1998; Girod and Brotman, 2004; Reiche et al., 2004; DiMicco et al., 2006; Pasquali et al., 2006; Goosens and Sapolsky, 2007; El Husseini and Laskowitz, 2014; Gupta and Morley, 2014; Prenderville et al., 2015; Herbert and Lucassen, 2016; Martocchia et al., 2016; Shin et al., 2016; Bortolato et al., 2017; Crestani, 2017). However, there are far fewer studies that address the left arc of the cycle. The left arc represents mechanisms by which advancing disease disrupts neural and endocrine circuits that mediate the stress response, producing neuropsychiatric symptoms such as depression, anxiety, insomnia and malaise (for review, see: Pedersen et al., 2001a; Silverman et al., 2005; Du and Pang, 2015; Michael Caudle, 2016; Wulsin et al., 2016). A clear example of this is pituitary tumors that release excess hormones to cause physiologic and psychologic pathologies secondary to tumor growth (e.g. pituitary adenomas release excess ACTH thereby chronically elevating circulating Cort, resulting in Cushing's disease; Boscaro et al., 2001). The recent extensive dissection of the neural circuitry that mediates behavioral and hormonal stress responses has uncovered a plethora of brain regions in which disease-associated dysfunction can produce neuropsychiatric symptoms, particularly in the context of neurodegeneration (Kolanowski et al., 2017; Ross et al., 2017).
The “Vicious Cycle of Stress” posits that stress drives disease and disease causes stress, feeding forward to accelerate disease progression while producing neuropsychiatric complications. Although this is an oversimplified construct, I use it here to illuminate the relationship between stress and Alzheimer's disease (AD) that most certainly is much more complicated. Below, I present both clinical and experimental data using this framework to illustrate how stress and AD interact to drive progression of AD-related dementias.
2. Alzheimer's disease pathogenesis is exacerbated by stress in animal models
Stress increases AD-related pathogenesis in a wide variety of experimental contexts. In wildtype mice and rats, exposure to stress increases the expression of Amyloid Precursor Protein (APP) and the generation of Aβ peptide (Rosa et al., 2005; Sayer et al., 2008; Solas et al., 2010; Ray et al., 2011; Briones et al., 2012), the gene and peptide considered central to AD etiology. In mice that misexpress humanized, disease-causing Familial Alzheimer's Disease (FAD) mutations in APP, stress not only elevates the production of Aβ, it also exacerbates its deposition into amyloid plaques, the pathological hallmark of AD (Dong et al., 2004; Jeong et al., 2006; Kang et al., 2007; Devi et al., 2010; Cuadrado-Tejedor et al., 2012; Rothman et al., 2012; Baglietto-Vargas et al., 2015; Justice et al., 2015; Lesuis et al., 2016). This has been demonstrated using both acute and chronic stressors, from mild to intense stress magnitudes. Elevations in interstitial Aβ are measurable within 1 h of restraint stress (Kang et al., 2007). Short term “modern life”-like stress (Baglietto-Vargas et al., 2015), chronic isolation stress (Dong et al., 2004), chronic mild/variable stress (Cuadrado-Tejedor et al., 2012), chronic mild social stress (Rothman et al., 2012), chronic restraint/immobilization stress (Jeong et al., 2006; Devi et al., 2010), and early life stress (Sierksma et al., 2012; Lesuis et al., 2016; Hoeijmakers et al., 2017; Hui et al., 2017) have all been shown to increase amyloid plaque burden. Stress also accelerates loss in cognitive performance in AD model animals (Dong et al., 2004; Jeong et al., 2006; Han et al., 2016, 2017). Stress-induced physiological changes can persist for the life of the animal, as stress exposure in young animals causes elevated CSF Aβ levels for up to 12 months and increases plaque formation, a process which begins months to years after the stress was applied (Justice et al., 2015; Lesuis et al., 2016; Hoeijmakers et al., 2017).
Neurofibrillary tangles composed of hyperphosphorylated Tau protein, the hallmark intracellular pathology that is thought to be ultimately responsible for neuronal death in AD (Goedert et al., 1988, 1989), are also exacerbated by stress exposure. Levels of hyperphosphorylated Tau are elevated by stress (Korneyev, 1998; Okawa et al., 2003; Feng et al., 2005; Fujio et al., 2007; Rissman et al., 2007, 2012; Carroll et al., 2011; Cuadrado-Tejedor et al., 2011; Sotiropoulos et al., 2011; Filipcik et al., 2012; Kvetnansky et al., 2016). When human AD-associated mutations in Tau are introduced into mice, stress-induced elevations in hyperphosphorylated Tau lead to neurofibrillary tangle formation and neurodegeneration (Carroll et al., 2011).
The exacerbation of both extracellular and intracellular AD pathologies is due, at least in part, to excessive secretion of Cort, as Cort injection alone elevates Aβ, hyperphosphorylated Tau, and amyloid plaque levels (Elliott et al., 1993; Green et al., 2006; Sotiropoulos et al., 2011; Wang et al., 2011; Joshi et al., 2012). However, there is evidence that excess Cort is not the sole mechanism by which stress exacerbates AD. Manipulations of the stress-released neuropeptide Corticotropin Releasing Factor (CRF; alternatively known as CRH) are sufficient to alter AD pathogenic endpoints. Intracerebral CRF injection promotes Aβ release and increases amyloid plaque formation (Kang et al., 2007; Dong et al., 2012). Overexpression of CRF increases Tau hyperphosphorylation and aggregation (Campbell et al., 2015b). Moreover, both Aβ- and Tau-related pathologies are reduced in Crf mutant animals (Filipcik et al., 2012; Kvetnansky et al., 2016), and mutations in Crfr1, the primary receptor for CRF, reduce Tau hyperphosphorylation and Aβ deposition in response to stress (Rissman et al., 2007, 2012; Campbell et al., 2015a).
Given the broad basis of evidence from many labs and different animal models, the consensus is that stress, in almost any form, accelerates AD pathogenesis, including extracellular amyloid plaque deposition and intracellular Tau hyperphosphorylation/tangle formation. Thus, there is a preponderance of evidence supporting this arc of the “Vicious Cycle of Stress” in mouse models of AD. Citing this evidence, many have suggested excessive stress also accelerates the progression of AD in humans.
3. The clinical relationship between Alzheimer's disease and stress
While many studies have applied stress in animals and observed accelerated AD pathogenesis, demonstrating the impact of stress in humans has proven difficult. The vast majority of clinical or epidemiological studies have provided evidence for the converse arc of the “Vicious Cycle of Stress”. Early stage AD-related dementia is associated with elevated Cort and anxiety-related neuropsychiatric conditions that correlate with increased disease risk. This was first shown in cohorts of patients with Mild Cognitive Impairment (MCI). Patients with MCI have higher average circulating Cort levels at all diurnal time points in the daily oscillation of Cort, compared to age matched controls (Davis et al., 1986; Hartmann et al., 1997). In addition, dementia patients show decreased dexamethasone suppression of Cortisol release, indicating impaired negative feedback on the HPA axis (Hatzinger et al., 1995; Nasman et al., 1995; Murialdo et al., 2000). Follow-up studies found that higher levels of circulating Cort correlate with more rapidly advancing disease (Weiner et al., 1997; Lupien et al., 1998; Csernansky et al., 2006). These findings suggest that a hyperactive HPA axis is an indication of more advanced disease. Elevated HPA axis activity and resulting increases in Cort release, in turn, would be predicted to accelerate and intensify disease progression.
Similar correlations have been reported between late-life anxiety/depression and the incidence of dementia. In a cohort of more than thirteen thousand patients who were tracked over the course of 50 years, the coincidence of depressive symptoms and dementia was analyzed (Barnes et al., 2012). They found that those who experience late-life depression had a two-fold elevated risk of a dementia diagnosis (including all potential pathological causes of dementia including AD; Barnes et al., 2012). This effect was specific to late-life onset depression; early-life depression did not predict increased risk and mid-life depression only conferred a twenty percent increase in risk (Barnes et al., 2012; Singh-Manoux et al., 2017). Multiple studies performed using the ADNI database, in which people in the earliest stages of dementia undergo an MRI at first diagnosis and again two years later, have shown that depression-related symptoms correlate with accelerated loss in brain tissue density and an increased likelihood of conversion from MCI to dementia (Lee et al., 2012; Mah et al., 2015; Lebedeva et al., 2017). In the Rush Memory and Aging Project, investigators tested patients for features of neuroticism and found that patients that scored high for “distress proneness” were 2.7-fold more likely to be diagnosed with dementia in the next three years (Wilson et al., 2003, 2004, 2006). It must be noted that many studies have failed to find a correlation between depression or anxiety-related symptoms and dementia (Lindsay et al., 2002; Becker et al., 2009). Clearly the myriad causes of both anxiety/depression and dementia, as well as extensive heterogeneity in patients diagnosed with these diseases, has led to discrepancies in both the findings and interpretation of many studies (Bennett and Thomas, 2014).
4. Post-traumatic stress disorder and AD
One specific example in clinical research that supports the right arc of the “Vicious Cycle of Stress” is from studies of aging veterans that suffer from neurodegenerative disease. In a pair of studies, it was found that those veterans diagnosed with PTSD in the absence of other associated physical traumas, were up to twice as likely to be diagnosed with dementia (Qureshi et al., 2010; Yaffe et al., 2010). One scenario to explain this finding is that symptoms of PTSD, which often include dysregulation of the HPA axis (Yehuda et al., 1991; Kanter et al., 2001; Young and Breslau, 2004), exacerbate or accelerate AD pathogenesis, leading to higher dementia incidence in PTSD. Conversely, early or pre-pathogenic processes that lead to AD (e.g. higher production of Aβ) may cause certain individuals to be susceptible to chronic anxiety-related diseases such as PTSD. A correlate of this second hypothesis is that pathogenic AD processes begin much earlier, possibly even during youth, and manifest as anxiety and depression related symptoms long before critically impacting cognitive function. These two scenarios are not mutually exclusive and involve interaction between neural, endocrine, and physiological processes that occur over a lifetime, making identification of the primary cause of increased risk for dementia (perturbed AD pathogenesis or chronic PTSD) in patients extremely challenging.
Consistent with findings in veterans with PTSD, a handful of studies have examined the correlation between early life trauma and later susceptibility to dementia. In a population of aboriginal Australians over the age of 60, a higher score on a childhood trauma questionnaire correlated with a 1.7-fold increase in the likelihood of dementia (Radford et al., 2017). Other studies have failed to find a correlation (Lindsay et al., 2002). While the evidence for an association with early-life psychological trauma alone is limited, numerous studies have shown that traumatic brain injury (TBI) at a young age is highly correlated with later dementia acquisition (for a recent review, see Griesbach et al., 2018). Psychologic and physical trauma possibly cause similar chronic physiologic changes that lead to increased dementia risk. Potential culprits include altered HPA axis dynamics and Cort levels, early initiation of AD-related pathogenesis, or altered cognitive reserve after trauma. Experiments conducted in model systems are necessary to identify potential priming mechanisms that occur early in life and confer vulnerability to dementia with age.
5. Rodent models of AD have disrupted stress responses
The majority of studies on stress in AD mouse models have focused on how stress accelerates disease. However, beginning with the first AD mouse model, tg2576 (Hsiao et al., 1996), there have been persistent reports that transgenic AD model strains exhibit aberrant aggressive and anxiety-related behavior (Lalonde et al., 2004; Ognibene et al., 2005; Alexander et al., 2011). In tg2576 mice this is so profound that transgenic mice will often kill their cage mates; male tg2576 mice need to be housed alone (unpublished observations; Alexander et al., 2011). This anxiety phenotype has now been quantitatively described in multiple different transgenic AD models, from mice over-expressing APP carrying FAD mutations (Hebda-Bauer et al., 2013; Torres-Lista et al., 2015) to knock-in AD models (Guo et al., 2012), FAD transgenic rats (Pentkowski et al., 2018), and rats intraventricularly injected with Aβ (Dao et al., 2014; Sharma et al., 2016; Tamano et al., 2016). In addition to elevated anxiety, young AD model mice are more susceptible to the development of PTSD-like symptoms after trauma exposure, long before amyloid plaque deposition (Justice et al., 2015). Because elevated anxiety-related behavior is present in so many independently-generated transgenic mice, it is hard to imagine that this is due to the background strain of any particular transgenic mouse. Rather, APP misexpression must in some way perturb stress-responsive neurons to alter their function, which in mouse is expressed as elevated anxiety-related behavior and stress sensitivity.
In addition to aberrant behavior, many AD model animals display elevated Cort, phenocopying results described in human dementia patients. Tg2576 mice have higher Cort levels (Dong et al., 2008), although as mentioned, they display very abnormal behavior indicating severe neural dysfunction. Other models that express APP at near endogenous levels and have relatively normal behavior, also display elevated Cort (Guo et al., 2012; Hebda-Bauer et al., 2013). When first observed in both experimental and clinical settings, elevated Cort was hypothesized to occur because of loss of hippocampal function, which would release inhibition on the HPA axis, increasing Cort release (Meaney et al., 1995; Sapolsky, 1996; Lupien et al., 1998). However, elevated Cort levels appear in very young animals long before amyloid plaque deposition that might disrupt the hippocampus has occurred, suggesting that Cort elevations result from APP misexpression in the absence of plaque deposition or neurodegeneration (Justice et al., 2015). Toxic oligomeric Aβ species would be produced from these transgenes, and are well known to perturb neural function in a variety of contexts (Lambert et al., 1998; Hartley et al., 1999; Bucciantini et al., 2002; Dahlgren et al., 2002; Walsh et al., 2002; Cleary et al., 2005; Holscher et al., 2007). However, it has remained unclear how Aβ produced by expression of familial AD-causing APP mutant isoforms perturbs stress responsive circuits to alter circulating Cort levels (Lucassen et al., 2001, 2006; Muller et al., 2001; Herbert and Lucassen, 2016).
The majority of findings in which AD pathogenesis was elevated by stress employed stress paradigms known to increase HPA axis activity and corresponding circulating Cort concentrations. High Cort compromises neuronal function, pushing neurons closer to cell death (Sapolsky, 1996). The most parsimonious causal scenario for stress exacerbation of AD is that high Cort sensitizes neurons such that in the presence of toxic soluble, oligomeric, or aggregated Aβ, more neurons die. Elevations in Cort due to stress or exogenously delivered corticosteroids in turn increase the production of Aβ, amyloid plaques, and Tau proteins further exacerbating this detrimental cycle. However, this scenario does not explain all contexts in which stress can impact AD. For example, in cases of PTSD, HPA axis activity is blunted, and circulating Cort concentrations are often lower than age-matched asymptomatic controls (Yehuda et al., 1991). If elevated AD risk is Cort dependent in PTSD patients, we would need to posit that chronically lower circulating Cort or severe oscillations in HPA axis activity at the time of the trauma also accelerate pathogenic progression, thereby conferring increased risk for dementia.
We have induced a PTSD-like state in mice (2 h immobilization with a reminder) and measured AD pathogenic endpoints in AD model animals (Justice et al., 2015). In mice carrying disease causing alleles of APP and Presenilin 1, PTSD-like induction produces chronic elevations in anxiety-related behavior, increased startle and chronically decreased circulating Cort, consistent with clinical symptoms of PTSD (Marti et al., 2001; Armario et al., 2008; Belda et al., 2008; Yamamoto et al., 2008; Justice et al., 2015). In PTSD-like induced mice, we observed a chronic increase in soluble Aβ in the CSF after PTSD-like induction, even though Cort levels are lower (Justice et al., 2015). Consistent with this finding, Crfr1 mutant animals (which have near undetectable levels of circulating Cort; Smith et al., 1998) carrying AD-causing disease alleles, have much higher Aβ levels compared to wt AD model animals. Together, these results suggest that Cort is important for limiting Aβ production (Justice et al., 2015). The effects of stress and corticosteroids often display a “U-shaped” curve, where too little stress/Cort or too much stress/Cort can both have deleterious effects, such that homeostasic control of Cort secretion is critical to avoiding disease (Joels, 2006; Sapolsky, 2015). This is one potential explanation for higher Aβ in animals with both high and low Cort. However, it remains possible that changes in Cort levels are not the causes of elevated dementia risk in trauma patients or increased Aβ/plaque deposition in stressed AD model animals. Further studies are needed to explore the mechanisms that connect stress and trauma-induced changes in HPA axis tone and increased risk for dementia.
6. A mechanism linking AD pathogenesis with stress phenotypes
One potential mechanism by which an increase in extracellular Aβ (used as a proxy for AD pathogenesis) might be translated into a “generalized” stress response that activates the HPA axis and elevates Cort release has been proposed by our group (Justice et al., 2015). We showed that CRF neurons can be directly excited by soluble Aβ species (Justice et al., 2015). Aβ produced and secreted by cells misexpressing FAD mutant APP isoforms acutely activates paraventricular hypothalamic CRF neurons, suggesting that CRF neurons can be activated by this “toxic” protein species (Justice et al., 2015). Why would CRF neurons be activated by Aβ? Via this mechanism the brain might signal a failing ability to maintain proteostasis, or the proper folding of proteins by the neuron. As proteostasis fails, more improperly folded soluble and aggregated Aβ is released by neurons (Cohen et al., 2006; Penke et al., 2017). In this model, CRF neurons sense the presence of aberrant protein species and activate the HPA axis, thereby alerting the body that something is amiss in the brain. The subsequent HPA axis activation and elevated Cort release implements a generalized stress response that may be an attempt to address failing proteostasis in the brain. In fact, this elevation in Cort would be predicted to exacerbate underlying AD pathology (Elliott et al., 1993; Green et al., 2006; Sotiropoulos et al., 2011; Wang et al., 2011; Joshi et al., 2012). Peripheral and central CRF release might also have a beneficial influence on neuronal health, as CRF has been shown to be neuroprotective in some circumstances (Lezoualc'h et al., 2000; Pedersen et al., 2001b; Elliott-Hunt et al., 2002; Koutmani et al., 2013). This proposed launching of a generalized physiologic stress response to the cellular stress of failed proteostasis might also be active in other diseases that involve protein aggregation. In this scenario, distinct aggregated or “toxic” protein species that have been found to underlie the etiology of many neurodegenerative diseases, such as α-synuclein in the case of Parkinson's disease (Polymeropoulos et al., 1997), would be predicted to also excite CRF neurons.
7. Stress and Parkinson's disease
While many studies have investigated how stress impacts AD, fewer have looked into the role that stress plays in other neurodegenerative diseases, such as the second most prevalent neurodegenerative disease, Parkinson's Disease (PD). Evidence from the clinic has pointed to an important role for stress on both sides of the “Vicious Cycle of Stress” in PD etiology. PD elevates anxiety, depression, and panic attacks, all common in Parkinsonian patients, perhaps due to the degeneration of dopaminergic or other neural circuits (Henderson et al., 1992; Lauterbach et al., 2003; Aarsland et al., 2007; Prediger et al., 2012). Anxiety is the most common neuropsychiatric symptom in PD patients, found in up to 69 percent, followed by depression in ∼30 percent and generalized anxiety disorder in ∼11 percent of PD patients (Nuti et al., 2004; Kulisevsky et al., 2008; Dissanayaka et al., 2010; Leentjens et al., 2011). An even greater correlation with neuropsychiatric symptoms is found in the PD-related, Dementia with Lewy Bodies (Kao et al., 2009; Sadiq et al., 2017; Donaghy et al., 2018). There is less experimental evidence that stress exacerbates PD. However, it has been reported that in PD patients, stress can dramatically exacerbate common symptoms of PD including rigidity and tremors (Siemers et al., 1993; Giladi and Hausdorff, 2006). In a rat model of PD, chronic variable stress worsens motor performance and increases dopamine neuron loss. Given that circuits degenerate that are critical for the appropriate maintenance of stress responses and HPA axis tone in PD and other neurodegenerative diseases, it is likely that many more connections will be found between stress and the pathology, symptoms, and progression of neurodegenerative diseases other than AD.
8. Stress in AD treatment
Given the increasing evidence that stress can have a deleterious effect on AD and other neurodegenerative disease progression, the question remains whether this information will aid in the treatment of AD. This can be looked at in a number of ways. Stress clearly exacerbates AD pathogenesis in AD model animals; lifestyle changes that reduce stress should be endorsed as protective against dementias, although this has not yet been proven in humans. In addition, pharmacologic therapies that selectively lower stress hormone levels (e.g. CRFR1 antagonists) should be tested for efficacy in slowing AD progression in humans. Treatment with the CRFR1 antagonist R121919 has been shown to decrease amyloid pathology and improve synaptic and cognitive function in AD model mice; however, this compound has not yet been tested in dementia patients (Zhang et al., 2015, 2016). Pharmacologic strategies that inhibit other aspects of the HPA axis have been tested in AD patients, with limited success. Glucocorticoid receptor antagonist treatment (RU486), which has been shown to decrease AD pathogenesis in mouse models (Baglietto-Vargas et al., 2015; Lante et al., 2015), led to a moderate improvement in cognitive scores in a small clinical trial (Belanoff et al., 2002; Pomara et al., 2002). Inhibition of the production of corticosteroids with an 11-β-hydroxysteroid dehydrogenase (11-β-HSD) inhibitor did not have an impact on cognitive scores of dementia patients in a randomized clinical trial (Marek et al., 2014). Increasing GR signaling by administration of the corticosteroid, prednisone, had no effect on cognitive performance in dementia patients (Aisen et al., 2000). Differences between laboratory (mouse) and clinical (human) experimental results may be due to different dosage or timing of drug delivery, or because most preliminary trials are conducted in patients that already experience substantial loss in cognitive ability, perhaps too late in disease progression to improve cognition by addressing aberrant stress hormone signaling.
The effects of AD progression on stress signaling must also be considered in the treatment of AD. Certain sub-populations of AD/dementia patients experience abnormal stress responses, depression, apathy, aggression or some combination of these symptoms (Amore et al., 2007). It is tempting to speculate that these subsets of symptoms are produced by degeneration of selective neural circuits important for each symptom. The subsets of AD cases that display depression, excessive anxiety, and/or aggression should receive additional neuropsychiatric attention and possible pharmacologic intervention to alleviate symptoms. Although anti-depressive medications are well tolerated in the elderly, many common anxiolytics (e.g. benzodiazepines) are counter-indicated in cases of dementia because they worsen cognitive performance and acuity (Crocco et al., 2017; Picton et al., 2018). New anxiolytics that do not have this side effect would be useful for the treatment of anxiety symptoms in dementia. Alternatively, non-pharmacologic treatments might have an important role in the treatment of neuropsychiatric symptoms in AD. For example, therapeutic touch, which is thought to decrease stress levels, reduced anxiety-related vocalizations and pacing, and mildly decreased salivary Cort levels in clinical trials in dementia patients (Woods et al., 2009). In addition, music therapy has been shown to provide stress relief and slow cognitive loss in dementia patients (for a recent review, see Baird and Thompson, 2018). While these studies suggest that stress reduction is beneficial to AD patients, whether this also decelerates disease progression remains to be determined.
As we strive to understand the inherently cyclical nature of the relationship between stress and AD to determine the causal events that precipitate dementia, by addressing stress-related symptoms we can improve quality of life for dementia patients with the hope that decreasing stress signaling might slow or prevent the progression of this devastating disease.
Conflicts of interest
The author declares no conflicts of interest.
Acknowledgements
I would like to thank Laura N. Niles for help with editing the manuscript. Please excuse the failure to cite all relevant studies. This work was supported by funding from the University of Texas Health Science Center at Houston, and the NIH R56MH114032 (N.J.), and R01MH112768 (N.J.).
References
- Aarsland D., Bronnick K., Ehrt U., De Deyn P.P., Tekin S., Emre M., Cummings J.L. Neuropsychiatric symptoms in patients with Parkinson's disease and dementia: frequency, profile and associated care giver stress. J. Neurol. Neurosurg. Psychiatry. 2007;78:36–42. doi: 10.1136/jnnp.2005.083113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aisen P.S., Davis K.L., Berg J.D., Schafer K., Campbell K., Thomas R.G., Weiner M.F., Farlow M.R., Sano M., Grundman M., Thal L.J. A randomized controlled trial of prednisone in Alzheimer's disease. Alzheimer's Disease Cooperative Study. Neurology. 2000;54:588–593. doi: 10.1212/wnl.54.3.588. [DOI] [PubMed] [Google Scholar]
- Alexander G., Hanna A., Serna V., Younkin L., Younkin S., Janus C. Increased aggression in males in transgenic Tg2576 mouse model of Alzheimer's disease. Behav. Brain Res. 2011;216:77–83. doi: 10.1016/j.bbr.2010.07.016. [DOI] [PubMed] [Google Scholar]
- Amore M., Tagariello P., Laterza C., Savoia E.M. Subtypes of depression in dementia. Arch. Gerontol. Geriatr. 2007;44(Suppl. 1):23–33. doi: 10.1016/j.archger.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Armario A., Escorihuela R.M., Nadal R. Long-term neuroendocrine and behavioural effects of a single exposure to stress in adult animals. Neurosci. Biobehav. Rev. 2008;32:1121–1135. doi: 10.1016/j.neubiorev.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Baglietto-Vargas D., Chen Y., Suh D., Ager R.R., Rodriguez-Ortiz C.J., Medeiros R., Myczek K., Green K.N., Baram T.Z., LaFerla F.M. Short-term modern life-like stress exacerbates Abeta-pathology and synapse loss in 3xTg-AD mice. J. Neurochem. 2015;134:915–926. doi: 10.1111/jnc.13195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird A., Thompson W.F. The impact of music on the self in dementia. J Alzheimers Dis. 2018;61:827–841. doi: 10.3233/JAD-170737. [DOI] [PubMed] [Google Scholar]
- Barnes D.E., Yaffe K., Byers A.L., McCormick M., Schaefer C., Whitmer R.A. Midlife vs late-life depressive symptoms and risk of dementia: differential effects for Alzheimer disease and vascular dementia. Arch. Gen. Psychiatr. 2012;69:493–498. doi: 10.1001/archgenpsychiatry.2011.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker J.T., Chang Y.F., Lopez O.L., Dew M.A., Sweet R.A., Barnes D., Yaffe K., Young J., Kuller L., Reynolds C.F., 3rd Depressed mood is not a risk factor for incident dementia in a community-based cohort. Am. J. Geriatr. Psychiatr. 2009;17:653–663. doi: 10.1097/jgp.0b013e3181aad1fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belanoff J.K., Jurik J., Schatzberg L.D., DeBattista C., Schatzberg A.F. Slowing the progression of cognitive decline in Alzheimer's disease using mifepristone. J. Mol. Neurosci. 2002;19:201–206. doi: 10.1007/s12031-002-0033-3. [DOI] [PubMed] [Google Scholar]
- Belda X., Fuentes S., Nadal R., Armario A. A single exposure to immobilization causes long-lasting pituitary-adrenal and behavioral sensitization to mild stressors. Horm. Behav. 2008;54:654–661. doi: 10.1016/j.yhbeh.2008.07.003. [DOI] [PubMed] [Google Scholar]
- Bennett S., Thomas A.J. Depression and dementia: cause, consequence or coincidence? Maturitas. 2014;79:184–190. doi: 10.1016/j.maturitas.2014.05.009. [DOI] [PubMed] [Google Scholar]
- Bjorntorp P. Stress and cardiovascular disease. Acta Physiol. Scand. Suppl. 1997;640:144–148. [PubMed] [Google Scholar]
- Bortolato B., Hyphantis T.N., Valpione S., Perini G., Maes M., Morris G., Kubera M., Kohler C.A., Fernandes B.S., Stubbs B., Pavlidis N., Carvalho A.F. Depression in cancer: the many biobehavioral pathways driving tumor progression. Canc. Treat Rev. 2017;52:58–70. doi: 10.1016/j.ctrv.2016.11.004. [DOI] [PubMed] [Google Scholar]
- Boscaro M., Barzon L., Fallo F., Sonino N. Cushing's syndrome. Lancet. 2001;357:783–791. doi: 10.1016/S0140-6736(00)04172-6. [DOI] [PubMed] [Google Scholar]
- Briones A., Gagno S., Martisova E., Dobarro M., Aisa B., Solas M., Tordera R., Ramirez M. Stress-induced anhedonia is associated with an increase in Alzheimer's disease-related markers. Br. J. Pharmacol. 2012;165:897–907. doi: 10.1111/j.1476-5381.2011.01602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucciantini M., Giannoni E., Chiti F., Baroni F., Formigli L., Zurdo J., Taddei N., Ramponi G., Dobson C.M., Stefani M. Inherent toxicity of aggregates implies a common mechanism for protein misfolding diseases. Nature. 2002;416:507–511. doi: 10.1038/416507a. [DOI] [PubMed] [Google Scholar]
- Campbell S.N., Zhang C., Roe A.D., Lee N., Lao K.U., Monte L., Donohue M.C., Rissman R.A. Impact of CRFR1 ablation on amyloid-beta production and accumulation in a mouse model of Alzheimer's disease. J Alzheimers Dis. 2015;45:1175–1184. doi: 10.3233/JAD-142844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell S.N., Zhang C., Monte L., Roe A.D., Rice K.C., Tache Y., Masliah E., Rissman R.A. Increased tau phosphorylation and aggregation in the hippocampus of mice overexpressing corticotropin-releasing factor. J Alzheimers Dis. 2015;43:967–976. doi: 10.3233/JAD-141281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll J.C., Iba M., Bangasser D.A., Valentino R.J., James M.J., Brunden K.R., Lee V.M., Trojanowski J.Q. Chronic stress exacerbates tau pathology, neurodegeneration, and cognitive performance through a corticotropin-releasing factor receptor-dependent mechanism in a transgenic mouse model of tauopathy. J. Neurosci. 2011;31:14436–14449. doi: 10.1523/JNEUROSCI.3836-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleary J.P., Walsh D.M., Hofmeister J.J., Shankar G.M., Kuskowski M.A., Selkoe D.J., Ashe K.H. Natural oligomers of the amyloid-beta protein specifically disrupt cognitive function. Nat. Neurosci. 2005;8:79–84. doi: 10.1038/nn1372. [DOI] [PubMed] [Google Scholar]
- Cohen E., Bieschke J., Perciavalle R.M., Kelly J.W., Dillin A. Opposing activities protect against age-onset proteotoxicity. Science. 2006;313:1604–1610. doi: 10.1126/science.1124646. [DOI] [PubMed] [Google Scholar]
- Crestani C.C. Adolescent vulnerability to cardiovascular consequences of chronic emotional stress: review and perspectives for future research. Neurosci. Biobehav. Rev. 2017;74:466–475. doi: 10.1016/j.neubiorev.2016.03.027. [DOI] [PubMed] [Google Scholar]
- Crocco E.A., Jaramillo S., Cruz-Ortiz C., Camfield K. Pharmacological management of anxiety disorders in the elderly. Curr Treat Options Psychiatry. 2017;4:33–46. doi: 10.1007/s40501-017-0102-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csernansky J.G., Dong H., Fagan A.M., Wang L., Xiong C., Holtzman D.M., Morris J.C. Plasma cortisol and progression of dementia in subjects with Alzheimer-type dementia. Am. J. Psychiatr. 2006;163:2164–2169. doi: 10.1176/appi.ajp.163.12.2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuadrado-Tejedor M., Ricobaraza A., Frechilla D., Franco R., Perez-Mediavilla A., Garcia-Osta A. Chronic mild stress accelerates the onset and progression of the Alzheimer's disease phenotype in Tg2576 mice. J Alzheimers Dis. 2012;28:567–578. doi: 10.3233/JAD-2011-110572. [DOI] [PubMed] [Google Scholar]
- Cuadrado-Tejedor M., Ricobaraza A., Del Rio J., Frechilla D., Franco R., Perez-Mediavilla A., Garcia-Osta A. Chronic mild stress in mice promotes cognitive impairment and CDK5-dependent tau hyperphosphorylation. Behav. Brain Res. 2011;220:338–343. doi: 10.1016/j.bbr.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Dahlgren K.N., Manelli A.M., Stine W.B., Jr., Baker L.K., Krafft G.A., LaDu M.J. Oligomeric and fibrillar species of amyloid-beta peptides differentially affect neuronal viability. J. Biol. Chem. 2002;277:32046–32053. doi: 10.1074/jbc.M201750200. [DOI] [PubMed] [Google Scholar]
- Dao A.T., Zagaar M.A., Salim S., Eriksen J.L., Alkadhi K.A. Regular exercise prevents non-cognitive disturbances in a rat model of Alzheimer's disease. Int. J. Neuropsychopharmacol. 2014;17:593–602. doi: 10.1017/S1461145713001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis K.L., Davis B.M., Greenwald B.S., Mohs R.C., Mathe A.A., Johns C.A., Horvath T.B. Cortisol and Alzheimer's disease, I: basal studies. Am. J. Psychiatr. 1986;143:300–305. doi: 10.1176/ajp.143.3.300. [DOI] [PubMed] [Google Scholar]
- Devi L., Alldred M.J., Ginsberg S.D., Ohno M. Sex- and brain region-specific acceleration of beta-amyloidogenesis following behavioral stress in a mouse model of Alzheimer's disease. Mol. Brain. 2010;3:34. doi: 10.1186/1756-6606-3-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMicco J.A., Sarkar S., Zaretskaia M.V., Zaretsky D.V. Stress-induced cardiac stimulation and fever: common hypothalamic origins and brainstem mechanisms. Auton. Neurosci. 2006;126–127:106–119. doi: 10.1016/j.autneu.2006.02.010. [DOI] [PubMed] [Google Scholar]
- Dissanayaka N.N., Sellbach A., Matheson S., O'Sullivan J.D., Silburn P.A., Byrne G.J., Marsh R., Mellick G.D. Anxiety disorders in Parkinson's disease: prevalence and risk factors. Mov. Disord. 2010;25:838–845. doi: 10.1002/mds.22833. [DOI] [PubMed] [Google Scholar]
- Donaghy P.C., Taylor J.P., O'Brien J.T., Barnett N., Olsen K., Colloby S.J., Lloyd J., Petrides G., McKeith I.G., Thomas A.J. Neuropsychiatric symptoms and cognitive profile in mild cognitive impairment with Lewy bodies. Psychol. Med. 2018:1–7. doi: 10.1017/S0033291717003956. [DOI] [PubMed] [Google Scholar]
- Dong H., Goico B., Martin M., Csernansky C.A., Bertchume A., Csernansky J.G. Modulation of hippocampal cell proliferation, memory, and amyloid plaque deposition in APPsw (Tg2576) mutant mice by isolation stress. Neuroscience. 2004;127:601–609. doi: 10.1016/j.neuroscience.2004.05.040. [DOI] [PubMed] [Google Scholar]
- Dong H., Yuede C.M., Yoo H.S., Martin M.V., Deal C., Mace A.G., Csernansky J.G. Corticosterone and related receptor expression are associated with increased beta-amyloid plaques in isolated Tg2576 mice. Neuroscience. 2008;155:154–163. doi: 10.1016/j.neuroscience.2008.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong H., Murphy K.M., Meng L., Montalvo-Ortiz J., Zeng Z., Kolber B.J., Zhang S., Muglia L.J., Csernansky J.G. Corticotrophin releasing factor accelerates neuropathology and cognitive decline in a mouse model of Alzheimer's disease. J Alzheimers Dis. 2012;28:579–592. doi: 10.3233/JAD-2011-111328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du X., Pang T.Y. Is dysregulation of the HPA-Axis a core pathophysiology mediating Co-Morbid depression in neurodegenerative diseases? Front. Psychiatr. 2015;6:32. doi: 10.3389/fpsyt.2015.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Husseini N., Laskowitz D.T. The role of neuroendocrine pathways in prognosis after stroke. Expert Rev. Neurother. 2014;14:217–232. doi: 10.1586/14737175.2014.877841. [DOI] [PubMed] [Google Scholar]
- Elliott-Hunt C.R., Kazlauskaite J., Wilde G.J., Grammatopoulos D.K., Hillhouse E.W. Potential signalling pathways underlying corticotrophin-releasing hormone-mediated neuroprotection from excitotoxicity in rat hippocampus. J. Neurochem. 2002;80:416–425. doi: 10.1046/j.0022-3042.2001.00712.x. [DOI] [PubMed] [Google Scholar]
- Elliott E.M., Mattson M.P., Vanderklish P., Lynch G., Chang I., Sapolsky R.M. Corticosterone exacerbates kainate-induced alterations in hippocampal tau immunoreactivity and spectrin proteolysis in vivo. J. Neurochem. 1993;61:57–67. doi: 10.1111/j.1471-4159.1993.tb03537.x. [DOI] [PubMed] [Google Scholar]
- Feng Q., Cheng B., Yang R., Sun F.Y., Zhu C.Q. Dynamic changes of phosphorylated tau in mouse hippocampus after cold water stress. Neurosci. Lett. 2005;388:13–16. doi: 10.1016/j.neulet.2005.06.022. [DOI] [PubMed] [Google Scholar]
- Filipcik P., Novak P., Mravec B., Ondicova K., Krajciova G., Novak M., Kvetnansky R. Tau protein phosphorylation in diverse brain areas of normal and CRH deficient mice: up-regulation by stress. Cell. Mol. Neurobiol. 2012;32:837–845. doi: 10.1007/s10571-011-9788-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujio J., Hosono H., Ishiguro K., Ikegami S., Fujita S.C. Tau phosphorylation in the mouse brain during aversive conditioning. Neurochem. Int. 2007;51:200–208. doi: 10.1016/j.neuint.2007.04.024. [DOI] [PubMed] [Google Scholar]
- Giladi N., Hausdorff J.M. The role of mental function in the pathogenesis of freezing of gait in Parkinson's disease. J. Neurol. Sci. 2006;248:173–176. doi: 10.1016/j.jns.2006.05.015. [DOI] [PubMed] [Google Scholar]
- Girod J.P., Brotman D.J. Does altered glucocorticoid homeostasis increase cardiovascular risk? Cardiovasc. Res. 2004;64:217–226. doi: 10.1016/j.cardiores.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Goedert M., Wischik C.M., Crowther R.A., Walker J.E., Klug A. Cloning and sequencing of the cDNA encoding a core protein of the paired helical filament of Alzheimer disease: identification as the microtubule-associated protein tau. Proc. Natl. Acad. Sci. U. S. A. 1988;85:4051–4055. doi: 10.1073/pnas.85.11.4051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goedert M., Spillantini M.G., Jakes R., Rutherford D., Crowther R.A. Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer's disease. Neuron. 1989;3:519–526. doi: 10.1016/0896-6273(89)90210-9. [DOI] [PubMed] [Google Scholar]
- Goosens K.A., Sapolsky R.M. Stress and glucocorticoid contributions to normal and pathological aging. In: Riddle D.R., editor. Brain Aging: Models, Methods, and Mechanisms. 2007. Boca Raton (FL) [PubMed] [Google Scholar]
- Green K.N., Billings L.M., Roozendaal B., McGaugh J.L., LaFerla F.M. Glucocorticoids increase amyloid-beta and tau pathology in a mouse model of Alzheimer's disease. J. Neurosci. 2006;26:9047–9056. doi: 10.1523/JNEUROSCI.2797-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griesbach G.S., Masel B.E., Helvie R.E., Ashley M.J. The impact of traumatic brain injury on later life: effects on normal aging and neurodegenerative diseases. J. Neurotrauma. 2018;35:17–24. doi: 10.1089/neu.2017.5103. [DOI] [PubMed] [Google Scholar]
- Guo Q., Zheng H., Justice N.J. Central CRF system perturbation in an Alzheimer's disease knockin mouse model. Neurobiol. Aging. 2012;33:2678–2691. doi: 10.1016/j.neurobiolaging.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta D., Morley J.E. Hypothalamic-pituitary-adrenal (HPA) axis and aging. Comp. Physiol. 2014;4:1495–1510. doi: 10.1002/cphy.c130049. [DOI] [PubMed] [Google Scholar]
- Han B., Wang J.H., Geng Y., Shen L., Wang H.L., Wang Y.Y., Wang M.W. Chronic stress contributes to cognitive dysfunction and hippocampal metabolic abnormalities in APP/PS1 mice. Cell. Physiol. Biochem. 2017;41:1766–1776. doi: 10.1159/000471869. [DOI] [PubMed] [Google Scholar]
- Han B., Yu L., Geng Y., Shen L., Wang H., Wang Y., Wang J., Wang M. Chronic stress aggravates cognitive impairment and suppresses insulin associated signaling pathway in APP/PS1 mice. J Alzheimers Dis. 2016;53:1539–1552. doi: 10.3233/JAD-160189. [DOI] [PubMed] [Google Scholar]
- Hartley D.M., Walsh D.M., Ye C.P., Diehl T., Vasquez S., Vassilev P.M., Teplow D.B., Selkoe D.J. Protofibrillar intermediates of amyloid beta-protein induce acute electrophysiological changes and progressive neurotoxicity in cortical neurons. J. Neurosci. 1999;19:8876–8884. doi: 10.1523/JNEUROSCI.19-20-08876.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann A., Veldhuis J.D., Deuschle M., Standhardt H., Heuser I. Twenty-four hour cortisol release profiles in patients with Alzheimer's and Parkinson's disease compared to normal controls: ultradian secretory pulsatility and diurnal variation. Neurobiol. Aging. 1997;18:285–289. doi: 10.1016/s0197-4580(97)80309-0. [DOI] [PubMed] [Google Scholar]
- Hatzinger M., Z'Brun A., Hemmeter U., Seifritz E., Baumann F., Holsboer-Trachsler E., Heuser I.J. Hypothalamic-pituitary-adrenal system function in patients with Alzheimer's disease. Neurobiol. Aging. 1995;16:205–209. doi: 10.1016/0197-4580(94)00159-6. [DOI] [PubMed] [Google Scholar]
- Hebda-Bauer E.K., Simmons T.A., Sugg A., Ural E., Stewart J.A., Beals J.L., Wei Q., Watson S.J., Akil H. 3xTg-AD mice exhibit an activated central stress axis during early-stage pathology. J Alzheimers Dis. 2013;33:407–422. doi: 10.3233/JAD-2012-121438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson R., Kurlan R., Kersun J.M., Como P. Preliminary examination of the comorbidity of anxiety and depression in Parkinson's disease. J. Neuropsychiatry Clin. Neurosci. 1992;4:257–264. doi: 10.1176/jnp.4.3.257. [DOI] [PubMed] [Google Scholar]
- Herbert J., Lucassen P.J. Depression as a risk factor for Alzheimer's disease: genes, steroids, cytokines and neurogenesis - what do we need to know? Front. Neuroendocrinol. 2016;41:153–171. doi: 10.1016/j.yfrne.2015.12.001. [DOI] [PubMed] [Google Scholar]
- Hoeijmakers L., Ruigrok S.R., Amelianchik A., Ivan D., van Dam A.M., Lucassen P.J., Korosi A. Early-life stress lastingly alters the neuroinflammatory response to amyloid pathology in an Alzheimer's disease mouse model. Brain Behav. Immun. 2017;63:160–175. doi: 10.1016/j.bbi.2016.12.023. [DOI] [PubMed] [Google Scholar]
- Holscher C., Gengler S., Gault V.A., Harriott P., Mallot H.A. Soluble beta-amyloid[25-35] reversibly impairs hippocampal synaptic plasticity and spatial learning. Eur. J. Pharmacol. 2007;561:85–90. doi: 10.1016/j.ejphar.2007.01.040. [DOI] [PubMed] [Google Scholar]
- Hsiao K., Chapman P., Nilsen S., Eckman C., Harigaya Y., Younkin S., Yang F., Cole G. Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. Science. 1996;274:99–102. doi: 10.1126/science.274.5284.99. [DOI] [PubMed] [Google Scholar]
- Hui J., Feng G., Zheng C., Jin H., Jia N. Maternal separation exacerbates Alzheimer's disease-like behavioral and pathological changes in adult APPswe/PS1dE9 mice. Behav. Brain Res. 2017;318:18–23. doi: 10.1016/j.bbr.2016.10.030. [DOI] [PubMed] [Google Scholar]
- Jeong Y.H., Park C.H., Yoo J., Shin K.Y., Ahn S.M., Kim H.S., Lee S.H., Emson P.C., Suh Y.H. Chronic stress accelerates learning and memory impairments and increases amyloid deposition in APPV717I-CT100 transgenic mice, an Alzheimer's disease model. FASEB J. 2006;20:729–731. doi: 10.1096/fj.05-4265fje. [DOI] [PubMed] [Google Scholar]
- Joels M. Corticosteroid effects in the brain: U-shape it. Trends Pharmacol. Sci. 2006;27:244–250. doi: 10.1016/j.tips.2006.03.007. [DOI] [PubMed] [Google Scholar]
- Joshi Y.B., Chu J., Pratico D. Stress hormone leads to memory deficits and altered tau phosphorylation in a model of Alzheimer's disease. J Alzheimers Dis. 2012;31:167–176. doi: 10.3233/JAD-2012-120328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice N.J., Huang L., Tian J.B., Cole A., Pruski M., Hunt A.J., Jr., Flores R., Zhu M.X., Arenkiel B.R., Zheng H. Posttraumatic stress disorder-like induction elevates beta-amyloid levels, which directly activates corticotropin-releasing factor neurons to exacerbate stress responses. J. Neurosci. 2015;35:2612–2623. doi: 10.1523/JNEUROSCI.3333-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang J.E., Cirrito J.R., Dong H., Csernansky J.G., Holtzman D.M. Acute stress increases interstitial fluid amyloid-beta via corticotropin-releasing factor and neuronal activity. Proc. Natl. Acad. Sci. U. S. A. 2007;104:10673–10678. doi: 10.1073/pnas.0700148104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanter E.D., Wilkinson C.W., Radant A.D., Petrie E.C., Dobie D.J., McFall M.E., Peskind E.R., Raskind M.A. Glucocorticoid feedback sensitivity and adrenocortical responsiveness in posttraumatic stress disorder. Biol. Psychiatr. 2001;50:238–245. doi: 10.1016/s0006-3223(01)01158-1. [DOI] [PubMed] [Google Scholar]
- Kao A.W., Racine C.A., Quitania L.C., Kramer J.H., Christine C.W., Miller B.L. Cognitive and neuropsychiatric profile of the synucleinopathies: Parkinson disease, dementia with Lewy bodies, and multiple system atrophy. Alzheimer Dis. Assoc. Disord. 2009;23:365–370. doi: 10.1097/WAD.0b013e3181b5065d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolanowski A., Boltz M., Galik E., Gitlin L.N., Kales H.C., Resnick B., Van Haitsma K.S., Knehans A., Sutterlin J.E., Sefcik J.S., Liu W., Petrovsky D.V., Massimo L., Gilmore-Bykovskyi A., MacAndrew M., Brewster G., Nalls V., Jao Y.L., Duffort N., Scerpella D. Determinants of behavioral and psychological symptoms of dementia: a scoping review of the evidence. Nurs. Outlook. 2017;65:515–529. doi: 10.1016/j.outlook.2017.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korneyev A.Y. Stress-induced tau phosphorylation in mouse strains with different brain Erk 1 + 2 immunoreactivity. Neurochem. Res. 1998;23:1539–1543. doi: 10.1023/a:1020980004539. [DOI] [PubMed] [Google Scholar]
- Koutmani Y., Politis P.K., Elkouris M., Agrogiannis G., Kemerli M., Patsouris E., Remboutsika E., Karalis K.P. Corticotropin-releasing hormone exerts direct effects on neuronal progenitor cells: implications for neuroprotection. Mol. Psychiatr. 2013;18:300–307. doi: 10.1038/mp.2012.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulisevsky J., Pagonabarraga J., Pascual-Sedano B., Garcia-Sanchez C., Gironell A., Trapecio Group S. Prevalence and correlates of neuropsychiatric symptoms in Parkinson's disease without dementia. Mov. Disord. 2008;23:1889–1896. doi: 10.1002/mds.22246. [DOI] [PubMed] [Google Scholar]
- Kvetnansky R., Novak P., Vargovic P., Lejavova K., Horvathova L., Ondicova K., Manz G., Filipcik P., Novak M., Mravec B. Exaggerated phosphorylation of brain tau protein in CRH KO mice exposed to repeated immobilization stress. Stress. 2016;19:395–405. doi: 10.1080/10253890.2016.1183119. [DOI] [PubMed] [Google Scholar]
- Lalonde R., Kim H.D., Fukuchi K. Exploratory activity, anxiety, and motor coordination in bigenic APPswe + PS1/DeltaE9 mice. Neurosci. Lett. 2004;369:156–161. doi: 10.1016/j.neulet.2004.07.069. [DOI] [PubMed] [Google Scholar]
- Lambert M.P., Barlow A.K., Chromy B.A., Edwards C., Freed R., Liosatos M., Morgan T.E., Rozovsky I., Trommer B., Viola K.L., Wals P., Zhang C., Finch C.E., Krafft G.A., Klein W.L. Diffusible, nonfibrillar ligands derived from Abeta1-42 are potent central nervous system neurotoxins. Proc. Natl. Acad. Sci. U. S. A. 1998;95:6448–6453. doi: 10.1073/pnas.95.11.6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lante F., Chafai M., Raymond E.F., Pereira A.R., Mouska X., Kootar S., Barik J., Bethus I., Marie H. Subchronic glucocorticoid receptor inhibition rescues early episodic memory and synaptic plasticity deficits in a mouse model of Alzheimer's disease. Neuropsychopharmacology. 2015;40:1772–1781. doi: 10.1038/npp.2015.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauterbach E.C., Freeman A., Vogel R.L. Correlates of generalized anxiety and panic attacks in dystonia and Parkinson disease. Cogn Behav Neurol. 2003;16:225–233. doi: 10.1097/00146965-200312000-00004. [DOI] [PubMed] [Google Scholar]
- Lebedeva A.K., Westman E., Borza T., Beyer M.K., Engedal K., Aarsland D., Selbaek G., Haberg A.K. MRI-Based classification models in prediction of mild cognitive impairment and dementia in late-life depression. Front. Aging Neurosci. 2017;9:13. doi: 10.3389/fnagi.2017.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee G.J., Lu P.H., Hua X., Lee S., Wu S., Nguyen K., Teng E., Leow A.D., Jack C.R., Jr., Toga A.W., Weiner M.W., Bartzokis G., Thompson P.M., Alzheimer's disease neuroimaging I Depressive symptoms in mild cognitive impairment predict greater atrophy in Alzheimer's disease-related regions. Biol. Psychiatr. 2012;71:814–821. doi: 10.1016/j.biopsych.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leentjens A.F., Dujardin K., Marsh L., Martinez-Martin P., Richard I.H., Starkstein S.E. Symptomatology and markers of anxiety disorders in Parkinson's disease: a cross-sectional study. Mov. Disord. 2011;26:484–492. doi: 10.1002/mds.23528. [DOI] [PubMed] [Google Scholar]
- Lesuis S.L., Maurin H., Borghgraef P., Lucassen P.J., Van Leuven F., Krugers H.J. Positive and negative early life experiences differentially modulate long term survival and amyloid protein levels in a mouse model of Alzheimer's disease. Oncotarget. 2016;7:39118–39135. doi: 10.18632/oncotarget.9776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezoualc'h F., Engert S., Berning B., Behl C. Corticotropin-releasing hormone-mediated neuroprotection against oxidative stress is associated with the increased release of non-amyloidogenic amyloid beta precursor protein and with the suppression of nuclear factor-kappaB. Mol. Endocrinol. 2000;14:147–159. doi: 10.1210/mend.14.1.0403. [DOI] [PubMed] [Google Scholar]
- Lindsay J., Laurin D., Verreault R., Hebert R., Helliwell B., Hill G.B., McDowell I. Risk factors for Alzheimer's disease: a prospective analysis from the canadian study of health and aging. Am. J. Epidemiol. 2002;156:445–453. doi: 10.1093/aje/kwf074. [DOI] [PubMed] [Google Scholar]
- Lucassen P.J., Muller M.B., Holsboer F., Bauer J., Holtrop A., Wouda J., Hoogendijk W.J., De Kloet E.R., Swaab D.F. Hippocampal apoptosis in major depression is a minor event and absent from subareas at risk for glucocorticoid overexposure. Am. J. Pathol. 2001;158:453–468. doi: 10.1016/S0002-9440(10)63988-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucassen P.J., Heine V.M., Muller M.B., van der Beek E.M., Wiegant V.M., De Kloet E.R., Joels M., Fuchs E., Swaab D.F., Czeh B. Stress, depression and hippocampal apoptosis. CNS Neurol. Disord. - Drug Targets. 2006;5:531–546. doi: 10.2174/187152706778559273. [DOI] [PubMed] [Google Scholar]
- Lupien S.J., de Leon M., de Santi S., Convit A., Tarshish C., Nair N.P., Thakur M., McEwen B.S., Hauger R.L., Meaney M.J. Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat. Neurosci. 1998;1:69–73. doi: 10.1038/271. [DOI] [PubMed] [Google Scholar]
- Mah L., Binns M.A., Steffens D.C. Anxiety symptoms in amnestic mild cognitive impairment are associated with medial temporal atrophy and predict conversion to Alzheimer disease. Am. J. Geriatr. Psychiatr. 2015;23:466–476. doi: 10.1016/j.jagp.2014.10.005. Alzheimer's disease Neuroimaging I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marek G.J., Katz D.A., Meier A., Nt Greco, Zhang W., Liu W., Lenz R.A. Efficacy and safety evaluation of HSD-1 inhibitor ABT-384 in Alzheimer's disease. Alzheimers Dement. 2014;10:S364–S373. doi: 10.1016/j.jalz.2013.09.010. [DOI] [PubMed] [Google Scholar]
- Marti O., Garcia A., Valles A., Harbuz M.S., Armario A. Evidence that a single exposure to aversive stimuli triggers long-lasting effects in the hypothalamus-pituitary-adrenal axis that consolidate with time. Eur. J. Neurosci. 2001;13:129–136. [PubMed] [Google Scholar]
- Martocchia A., Stefanelli M., Falaschi G.M., Toussan L., Ferri C., Falaschi P. Recent advances in the role of cortisol and metabolic syndrome in age-related degenerative diseases. Aging Clin. Exp. Res. 2016;28:17–23. doi: 10.1007/s40520-015-0353-0. [DOI] [PubMed] [Google Scholar]
- Meaney M.J., O'Donnell D., Rowe W., Tannenbaum B., Steverman A., Walker M., Nair N.P., Lupien S. Individual differences in hypothalamic-pituitary-adrenal activity in later life and hippocampal aging. Exp. Gerontol. 1995;30:229–251. doi: 10.1016/0531-5565(94)00065-b. [DOI] [PubMed] [Google Scholar]
- Michael Caudle W. This can't be stressed enough: the contribution of select environmental toxicants to disruption of the stress circuitry and response. Physiol. Behav. 2016;166:65–75. doi: 10.1016/j.physbeh.2015.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller M.B., Lucassen P.J., Yassouridis A., Hoogendijk W.J., Holsboer F., Swaab D.F. Neither major depression nor glucocorticoid treatment affects the cellular integrity of the human hippocampus. Eur. J. Neurosci. 2001;14:1603–1612. doi: 10.1046/j.0953-816x.2001.01784.x. [DOI] [PubMed] [Google Scholar]
- Murialdo G., Barreca A., Nobili F., Rollero A., Timossi G., Gianelli M.V., Copello F., Rodriguez G., Polleri A. Dexamethasone effects on cortisol secretion in Alzheimer's disease: some clinical and hormonal features in suppressor and nonsuppressor patients. J. Endocrinol. Invest. 2000;23:178–186. doi: 10.1007/BF03343703. [DOI] [PubMed] [Google Scholar]
- Nasman B., Olsson T., Viitanen M., Carlstrom K. A subtle disturbance in the feedback regulation of the hypothalamic-pituitary-adrenal axis in the early phase of Alzheimer's disease. Psychoneuroendocrinology. 1995;20:211–220. doi: 10.1016/0306-4530(94)00054-e. [DOI] [PubMed] [Google Scholar]
- Nuti A., Ceravolo R., Piccinni A., Dell'Agnello G., Bellini G., Gambaccini G., Rossi C., Logi C., Dell'Osso L., Bonuccelli U. Psychiatric comorbidity in a population of Parkinson's disease patients. Eur. J. Neurol. 2004;11:315–320. doi: 10.1111/j.1468-1331.2004.00781.x. [DOI] [PubMed] [Google Scholar]
- Ognibene E., Middei S., Daniele S., Adriani W., Ghirardi O., Caprioli A., Laviola G. Aspects of spatial memory and behavioral disinhibition in Tg2576 transgenic mice as a model of Alzheimer's disease. Behav. Brain Res. 2005;156:225–232. doi: 10.1016/j.bbr.2004.05.028. [DOI] [PubMed] [Google Scholar]
- Okawa Y., Ishiguro K., Fujita S.C. Stress-induced hyperphosphorylation of tau in the mouse brain. FEBS Lett. 2003;535:183–189. doi: 10.1016/s0014-5793(02)03883-8. [DOI] [PubMed] [Google Scholar]
- Pasquali R., Vicennati V., Cacciari M., Pagotto U. The hypothalamic-pituitary-adrenal axis activity in obesity and the metabolic syndrome. Ann. N. Y. Acad. Sci. 2006;1083:111–128. doi: 10.1196/annals.1367.009. [DOI] [PubMed] [Google Scholar]
- Pedersen W.A., Wan R., Mattson M.P. Impact of aging on stress-responsive neuroendocrine systems. Mech. Ageing Dev. 2001;122:963–983. doi: 10.1016/s0047-6374(01)00250-0. [DOI] [PubMed] [Google Scholar]
- Pedersen W.A., McCullers D., Culmsee C., Haughey N.J., Herman J.P., Mattson M.P. Corticotropin-releasing hormone protects neurons against insults relevant to the pathogenesis of Alzheimer's disease. Neurobiol. Dis. 2001;8:492–503. doi: 10.1006/nbdi.2001.0395. [DOI] [PubMed] [Google Scholar]
- Penke B., Bogar F., Fulop L. Beta-amyloid and the pathomechanisms of Alzheimer's disease: a comprehensive view. Molecules. 2017;22 doi: 10.3390/molecules22101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pentkowski N.S., Berkowitz L.E., Thompson S.M., Drake E.N., Olguin C.R., Clark B.J. Anxiety-like behavior as an early endophenotype in the TgF344-AD rat model of Alzheimer's disease. Neurobiol. Aging. 2018;61:169–176. doi: 10.1016/j.neurobiolaging.2017.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picton J.D., Marino A.B., Nealy K.L. Benzodiazepine use and cognitive decline in the elderly. Am. J. Health Syst. Pharm. 2018;75:e6–e12. doi: 10.2146/ajhp160381. [DOI] [PubMed] [Google Scholar]
- Polymeropoulos M.H., Lavedan C., Leroy E., Ide S.E., Dehejia A., Dutra A., Pike B., Root H., Rubenstein J., Boyer R., Stenroos E.S., Chandrasekharappa S., Athanassiadou A., Papapetropoulos T., Johnson W.G., Lazzarini A.M., Duvoisin R.C., Di Iorio G., Golbe L.I., Nussbaum R.L. Mutation in the alpha-synuclein gene identified in families with Parkinson's disease. Science. 1997;276:2045–2047. doi: 10.1126/science.276.5321.2045. [DOI] [PubMed] [Google Scholar]
- Pomara N., Doraiswamy P.M., Tun H., Ferris S. Mifepristone (RU 486) for Alzheimer's disease. Neurology. 2002;58:1436. doi: 10.1212/wnl.58.9.1436. [DOI] [PubMed] [Google Scholar]
- Prediger R.D., Matheus F.C., Schwarzbold M.L., Lima M.M., Vital M.A. Anxiety in Parkinson's disease: a critical review of experimental and clinical studies. Neuropharmacology. 2012;62:115–124. doi: 10.1016/j.neuropharm.2011.08.039. [DOI] [PubMed] [Google Scholar]
- Prenderville J.A., Kennedy P.J., Dinan T.G., Cryan J.F. Adding fuel to the fire: the impact of stress on the ageing brain. Trends Neurosci. 2015;38:13–25. doi: 10.1016/j.tins.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Qureshi S.U., Kimbrell T., Pyne J.M., Magruder K.M., Hudson T.J., Petersen N.J., Yu H.J., Schulz P.E., Kunik M.E. Greater prevalence and incidence of dementia in older veterans with posttraumatic stress disorder. J. Am. Geriatr. Soc. 2010;58:1627–1633. doi: 10.1111/j.1532-5415.2010.02977.x. [DOI] [PubMed] [Google Scholar]
- Radford K., Delbaere K., Draper B., Mack H.A., Daylight G., Cumming R., Chalkley S., Minogue C., Broe G.A. Childhood stress and adversity is associated with late-life dementia in aboriginal Australians. Am. J. Geriatr. Psychiatr. 2017;25:1097–1106. doi: 10.1016/j.jagp.2017.05.008. [DOI] [PubMed] [Google Scholar]
- Ray B., Gaskins D.L., Sajdyk T.J., Spence J.P., Fitz S.D., Shekhar A., Lahiri D.K. Restraint stress and repeated corticotrophin-releasing factor receptor activation in the amygdala both increase amyloid-beta precursor protein and amyloid-beta peptide but have divergent effects on brain-derived neurotrophic factor and pre-synaptic proteins in the prefrontal cortex of rats. Neuroscience. 2011;184:139–150. doi: 10.1016/j.neuroscience.2011.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiche E.M., Nunes S.O., Morimoto H.K. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004;5:617–625. doi: 10.1016/S1470-2045(04)01597-9. [DOI] [PubMed] [Google Scholar]
- Rissman R.A., Lee K.F., Vale W., Sawchenko P.E. Corticotropin-releasing factor receptors differentially regulate stress-induced tau phosphorylation. J. Neurosci. 2007;27:6552–6562. doi: 10.1523/JNEUROSCI.5173-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rissman R.A., Staup M.A., Lee A.R., Justice N.J., Rice K.C., Vale W., Sawchenko P.E. Corticotropin-releasing factor receptor-dependent effects of repeated stress on tau phosphorylation, solubility, and aggregation. Proc. Natl. Acad. Sci. U. S. A. 2012;109:6277–6282. doi: 10.1073/pnas.1203140109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa M.L., Guimaraes F.S., de Oliveira R.M., Padovan C.M., Pearson R.C., Del Bel E.A. Restraint stress induces beta-amyloid precursor protein mRNA expression in the rat basolateral amygdala. Brain Res. Bull. 2005;65:69–75. doi: 10.1016/j.brainresbull.2004.11.011. [DOI] [PubMed] [Google Scholar]
- Ross J.A., Gliebus G., Van Bockstaele E.J. Stress induced neural reorganization: a conceptual framework linking depression and Alzheimer's disease. Prog. Neuropsychopharmacol. Biol Psychiatr. 2017 doi: 10.1016/j.pnpbp.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman S.M., Herdener N., Camandola S., Texel S.J., Mughal M.R., Cong W.N., Martin B., Mattson M.P. 3xTgAD mice exhibit altered behavior and elevated Abeta after chronic mild social stress. Neurobiol. Aging. 2012;33(830) doi: 10.1016/j.neurobiolaging.2011.07.005. e831–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadiq D., Whitfield T., Lee L., Stevens T., Costafreda S., Walker Z. Prodromal dementia with Lewy bodies and prodromal Alzheimer's disease: a comparison of the cognitive and clinical profiles. J Alzheimers Dis. 2017;58:463–470. doi: 10.3233/JAD-161089. [DOI] [PubMed] [Google Scholar]
- Sapolsky R.M. Stress, glucocorticoids, and damage to the nervous system: the current state of confusion. Stress. 1996;1:1–19. doi: 10.3109/10253899609001092. [DOI] [PubMed] [Google Scholar]
- Sapolsky R.M. Stress and the brain: individual variability and the inverted-U. Nat. Neurosci. 2015;18:1344–1346. doi: 10.1038/nn.4109. [DOI] [PubMed] [Google Scholar]
- Sayer R., Robertson D., Balfour D.J., Breen K.C., Stewart C.A. The effect of stress on the expression of the amyloid precursor protein in rat brain. Neurosci. Lett. 2008;431:197–200. doi: 10.1016/j.neulet.2007.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selye H. Stress and the general adaptation syndrome. Br. Med. J. 1950;1:1383–1392. doi: 10.1136/bmj.1.4667.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S., Verma S., Kapoor M., Saini A., Nehru B. Alzheimer's disease like pathology induced six weeks after aggregated amyloid-beta injection in rats: increased oxidative stress and impaired long-term memory with anxiety-like behavior. Neurol. Res. 2016;38:838–850. doi: 10.1080/01616412.2016.1209337. [DOI] [PubMed] [Google Scholar]
- Shin K.J., Lee Y.J., Yang Y.R., Park S., Suh P.G., Follo M.Y., Cocco L., Ryu S.H. Molecular mechanisms underlying psychological stress and cancer. Curr Pharm Des. 2016;22:2389–2402. doi: 10.2174/1381612822666160226144025. [DOI] [PubMed] [Google Scholar]
- Siemers E.R., Shekhar A., Quaid K., Dickson H. Anxiety and motor performance in Parkinson's disease. Mov. Disord. 1993;8:501–506. doi: 10.1002/mds.870080415. [DOI] [PubMed] [Google Scholar]
- Sierksma A.S., Vanmierlo T., De Vry J., Raijmakers M.E., Steinbusch H.W., van den Hove D.L., Prickaerts J. Effects of prenatal stress exposure on soluble Abeta and brain-derived neurotrophic factor signaling in male and female APPswe/PS1dE9 mice. Neurochem. Int. 2012;61:697–701. doi: 10.1016/j.neuint.2012.06.022. [DOI] [PubMed] [Google Scholar]
- Silverman M.N., Pearce B.D., Biron C.A., Miller A.H. Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunol. 2005;18:41–78. doi: 10.1089/vim.2005.18.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh-Manoux A., Dugravot A., Fournier A., Abell J., Ebmeier K., Kivimaki M., Sabia S. Trajectories of depressive symptoms before diagnosis of dementia: a 28-year follow-up study. JAMA Psychiatry. 2017 doi: 10.1001/jamapsychiatry.2017.0660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G.W., Aubry J.M., Dellu F., Contarino A., Bilezikjian L.M., Gold L.H., Chen R., Marchuk Y., Hauser C., Bentley C.A., Sawchenko P.E., Koob G.F., Vale W., Lee K.F. Corticotropin releasing factor receptor 1-deficient mice display decreased anxiety, impaired stress response, and aberrant neuroendocrine development. Neuron. 1998;20:1093–1102. doi: 10.1016/s0896-6273(00)80491-2. [DOI] [PubMed] [Google Scholar]
- Solas M., Aisa B., Mugueta M.C., Del Rio J., Tordera R.M., Ramirez M.J. Interactions between age, stress and insulin on cognition: implications for Alzheimer's disease. Neuropsychopharmacology. 2010;35:1664–1673. doi: 10.1038/npp.2010.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotiropoulos I., Catania C., Pinto L.G., Silva R., Pollerberg G.E., Takashima A., Sousa N., Almeida O.F. Stress acts cumulatively to precipitate Alzheimer's disease-like tau pathology and cognitive deficits. J. Neurosci. 2011;31:7840–7847. doi: 10.1523/JNEUROSCI.0730-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamano H., Ide K., Adlard P.A., Bush A.I., Takeda A. Involvement of hippocampal excitability in amyloid beta-induced behavioral and psychological symptoms of dementia. J. Toxicol. Sci. 2016;41:449–457. doi: 10.2131/jts.41.449. [DOI] [PubMed] [Google Scholar]
- Torres-Lista V., Lopez-Pousa S., Gimenez-Llort L. Marble-burying is enhanced in 3xTg-AD mice, can be reversed by risperidone and it is modulable by handling. Behav. Process. 2015;116:69–74. doi: 10.1016/j.beproc.2015.05.001. [DOI] [PubMed] [Google Scholar]
- Wahrborg P. Mental stress and ischaemic heart disease: an underestimated connection. Eur. Heart J. 1998;19(Suppl. O):O20–O23. [PubMed] [Google Scholar]
- Walsh D.M., Klyubin I., Fadeeva J.V., Cullen W.K., Anwyl R., Wolfe M.S., Rowan M.J., Selkoe D.J. Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature. 2002;416:535–539. doi: 10.1038/416535a. [DOI] [PubMed] [Google Scholar]
- Wang Y., Li M., Tang J., Song M., Xu X., Xiong J., Li J., Bai Y. Glucocorticoids facilitate astrocytic amyloid-beta peptide deposition by increasing the expression of APP and BACE1 and decreasing the expression of amyloid-beta-degrading proteases. Endocrinology. 2011;152:2704–2715. doi: 10.1210/en.2011-0145. [DOI] [PubMed] [Google Scholar]
- Weiner M.F., Vobach S., Olsson K., Svetlik D., Risser R.C. Cortisol secretion and Alzheimer's disease progression. Biol. Psychiatr. 1997;42:1030–1038. doi: 10.1016/s0006-3223(97)00165-0. [DOI] [PubMed] [Google Scholar]
- Wilson R.S., Evans D.A., Bienias J.L., Mendes de Leon C.F., Schneider J.A., Bennett D.A. Proneness to psychological distress is associated with risk of Alzheimer's disease. Neurology. 2003;61:1479–1485. doi: 10.1212/01.wnl.0000096167.56734.59. [DOI] [PubMed] [Google Scholar]
- Wilson R.S., Arnold S.E., Schneider J.A., Kelly J.F., Tang Y., Bennett D.A. Chronic psychological distress and risk of Alzheimer's disease in old age. Neuroepidemiology. 2006;27:143–153. doi: 10.1159/000095761. [DOI] [PubMed] [Google Scholar]
- Wilson R.S., Fleischman D.A., Myers R.A., Bennett D.A., Bienias J.L., Gilley D.W., Evans D.A. Premorbid proneness to distress and episodic memory impairment in Alzheimer's disease. J. Neurol. Neurosurg. Psychiatry. 2004;75:191–195. [PMC free article] [PubMed] [Google Scholar]
- Woods D.L., Beck C., Sinha K. The effect of therapeutic touch on behavioral symptoms and cortisol in persons with dementia. Forsch Komplementmed. 2009;16:181–189. doi: 10.1159/000220479. [DOI] [PubMed] [Google Scholar]
- Wulsin A.C., Solomon M.B., Privitera M.D., Danzer S.C., Herman J.P. Hypothalamic-pituitary-adrenocortical axis dysfunction in epilepsy. Physiol. Behav. 2016;166:22–31. doi: 10.1016/j.physbeh.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K., Vittinghoff E., Lindquist K., Barnes D., Covinsky K.E., Neylan T., Kluse M., Marmar C. Posttraumatic stress disorder and risk of dementia among US veterans. Arch. Gen. Psychiatr. 2010;67:608–613. doi: 10.1001/archgenpsychiatry.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto S., Morinobu S., Fuchikami M., Kurata A., Kozuru T., Yamawaki S. Effects of single prolonged stress and D-cycloserine on contextual fear extinction and hippocampal NMDA receptor expression in a rat model of PTSD. Neuropsychopharmacology. 2008;33:2108–2116. doi: 10.1038/sj.npp.1301605. [DOI] [PubMed] [Google Scholar]
- Yehuda R., Giller E.L., Southwick S.M., Lowy M.T., Mason J.W. Hypothalamic-pituitary-adrenal dysfunction in posttraumatic stress disorder. Biol. Psychiatr. 1991;30:1031–1048. doi: 10.1016/0006-3223(91)90123-4. [DOI] [PubMed] [Google Scholar]
- Young E.A., Breslau N. Saliva cortisol in posttraumatic stress disorder: a community epidemiologic study. Biol. Psychiatr. 2004;56:205–209. doi: 10.1016/j.biopsych.2004.05.011. [DOI] [PubMed] [Google Scholar]
- Zhang C., Kuo C.C., Moghadam S.H., Monte L., Rice K.C., Rissman R.A. Corticotropin-Releasing factor Receptor-1 antagonism reduces oxidative damage in an Alzheimer's disease transgenic mouse model. J Alzheimers Dis. 2015;45:639–650. doi: 10.3233/JAD-141722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Kuo C.C., Moghadam S.H., Monte L., Campbell S.N., Rice K.C., Sawchenko P.E., Masliah E., Rissman R.A. Corticotropin-releasing factor receptor-1 antagonism mitigates beta amyloid pathology and cognitive and synaptic deficits in a mouse model of Alzheimer's disease. Alzheimers Dement. 2016;12:527–537. doi: 10.1016/j.jalz.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]