By linking individual-level health care records and a composite neighborhood-level index, we examine the associations between neighborhood child opportunity and pediatric acute care use.
Abstract
Video Abstract
OBJECTIVES:
Although health care providers and systems are increasingly interested in patients’ nonmedical needs as a means to improve health, little is known about neighborhood conditions that contribute to child health problems. We sought to determine if a novel, publicly available measure of neighborhood context, the Child Opportunity Index, was associated with pediatric acute care visit frequency and diagnoses.
METHODS:
This cross-sectional study included San Francisco residents <18 years of age with an emergency department and/or urgent care visit to any of 3 medical systems (N = 47 175) between 2007 and 2011. Hot-spot analysis was used to compare the spatial distribution of neighborhood child opportunity and income. Generalized estimating equation logistic regression models were used to examine independent associations between neighborhood child opportunity and frequent acute care use (≥4 visits per year) and diagnosis group after adjusting for neighborhood income and patient age, sex, race and/or ethnicity, payer, and health system.
RESULTS:
Neighborhood child opportunity and income had distinct spatial distributions, and we identified different clusters of high- and low-risk neighborhoods. Children living in the lowest opportunity neighborhoods had significantly greater odds of ≥4 acute care visits per year (odds ratio 1.33; 95% confidence interval 1.03–1.73) compared with those in the highest opportunity neighborhoods. Neighborhood child opportunity was negatively associated with visits for respiratory conditions, asthma, assault, and ambulatory care–sensitive conditions but positively associated with injury-related visits.
CONCLUSIONS:
The Child Opportunity Index could be an effective tool for identifying neighborhood factors beyond income related to child health.
What’s Known on This Subject:
Children from low-income neighborhoods are more likely to visit the emergency department. Other neighborhood-level factors are associated with child health problems and may contribute to disparities in health care use for pediatric patients.
What This Study Adds:
This is the first study in which researchers examine associations between neighborhood child opportunity and individual-level pediatric acute care use. Neighborhood child opportunity was significantly associated with frequent acute care visits and diagnoses independent of patient characteristics and neighborhood income.
Pediatric patients account for one-fifth of all US emergency department (ED) visits,1 and children’s ED use has increased in volume and resource use over time.2 Nationally, children living in the lowest-income neighborhoods account for twice as many ED visits as children from the highest-income neighborhoods.1 Research on factors associated with child ED use has been focused primarily on individual-level characteristics, such as age, sex, race and/or ethnicity, insurance status, and family income.2–6 Aside from neighborhood income,7–11 little is known about the associations between neighborhood-level characteristics and pediatric ED use.
Various environmental, economic, and social factors, which are referred to as social determinants of health, can be used to explain a large portion of the variance in health outcomes and disparities in health care use at all ages.12,13 These may act synergistically to affect child health.14–17 Identifying the contextual measures beyond neighborhood income that are associated with child health and health care use can provide additional points of entry for health systems and health care providers to improve child health.18
The Child Opportunity Index is a multidimensional measure of neighborhood context that incorporates traditional and novel indicators that are associated with child development. It includes negative factors, such as school poverty and exposure to toxic waste, and supportive factors, such as adult education and proximity to parks.19 To date, the Child Opportunity Index has been used within and across metropolitan regions to measure the inequitable distribution of child opportunity, and it may be a useful tool for health systems to meet community data-reporting requirements and guide place-based interventions.19 However, there is no empirical evidence of associations between the Child Opportunity Index and child health outcomes.18,20
Our aim was to determine if neighborhood-level child opportunity is uniquely associated with individual-level pediatric ED and urgent medical care use (acute care). We evaluated whether the spatial distribution of child opportunity differed from that of neighborhood income and identified different clusters of high- and low-risk neighborhoods. We then examined the association between pediatric acute care outcomes and neighborhood child opportunity, adjusting for individual-level covariates and neighborhood income.
Methods
Study Data
The patient sample comprised children 1 day to 18 years old in San Francisco, California, who visited an ED and/or adjoined urgent care department at any of 6 hospital sites within 3 medical systems between January 1, 2007, and December 31, 2011. The final sample included 47 175 patients (Supplemental Fig 2). A subset of the patient data used for this study was published previously in relation to housing.21 The University of California, San Francisco and the Sutter Health Institutional Review Boards approved this study.
Outcome Measures
Patient- and visit-level electronic health record (EHR) data were merged within and across medical systems to eliminate duplication and identify total acute care visits by each child. Two types of patient-level, dichotomous outcome measures were evaluated: frequent acute care use and diagnosis group (Supplemental Table 3). The frequent acute care use measure was used to count all ED and urgent care visits within 1 year of a patient’s first visit and was coded as <4 visits versus ≥4 visits.22,23 The diagnosis group outcome measures were based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes assigned to each patient’s visit(s). We included diagnoses for conditions that are likely preventable or treatable in a primary care setting, affect children across all age groups, and have a plausible association with neighborhood factors. These included respiratory conditions,24 injury and/or trauma,25,26 and ambulatory care–sensitive conditions (ACSCs).6,27 We also evaluated asthma28,29 and assault,30 which are specific conditions within the respiratory and injury and/or trauma diagnostic groups, respectively, that have shown socioeconomic health disparities.
Exposure Variable
Neighborhood child opportunity for each patient was measured by using the Child Opportunity Index, which includes 3 domains of neighborhood characteristics that can support or inhibit healthy child development: education, health and environment, and social and economic opportunities.19 Within these domains are 19 component measures (Supplemental Table 4). Raw values for child opportunity measures at the census tract level for the City and County of San Francisco were obtained from Brandeis University.31 Measures were standardized across the study area and combined as described previously.19
Covariates
All adjusted models included patient- and neighborhood-level measures associated with pediatric emergency services use and/or diagnoses1,8,32,33: categorical age, sex, race and/or ethnicity, primary payer, health system, and quintile of census tract median household income. Patient measures were extracted from electronic medical records, and neighborhood median household income was obtained from the US Census Bureau.34
Analyses
Neighborhood-level child opportunity scores were grouped into 5 quintiles (very low, low, moderate, high, and very high) based on the distribution of values in San Francisco. Quintiles have been used in previous work in which researchers evaluated neighborhood-level effects on child health19,24 and can inform programs and policies that rely on risk stratification. We tabulated study population characteristics by neighborhood child opportunity quintile to ensure adequate population counts across strata.
To assess whether the spatial distribution of child opportunity and income differed, we created maps of these 2 neighborhood-level characteristics and used a hot-spot analysis tool35 to calculate local Getis-Ord Gi* statistics36 and detect clusters of high and low values of each measure.24 Visual and quantitative comparisons were used to identify geographic areas where child opportunity and income quintiles were significantly different.
Generalized estimating equation logistic regression models were used to estimate the association between neighborhood child opportunity and acute care outcomes while accounting for covariates. One set of models included child opportunity and income quintiles as categorical variables to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for each quintile. A second set of models included child opportunity and income quintiles as continuous measures to calculate a P value for trend across quintiles. Lastly, we ran a series of models with each of the 3 child opportunity domains to determine if any particular domains were more strongly associated with the outcomes. For all models, an exchangeable correlation structure was used to account for potential clustering by neighborhood (n = 194) and generate population-averaged parameter estimates with robust standard errors.37 All statistical analyses were conducted by using Stata 13 statistical software (StataCorp, College Station, TX). Geocoding and spatial analyses were conducted by using ArcMap 10.3 (Esri, Redlands, CA).
Results
Patient Characteristics and Outcomes
The sample was racially and ethnically diverse; 29% was Hispanic or Latino, 28% was white, 19% was Asian American, 14% was black and/or African American, and 11% was multiracial or of other or unknown race and/or ethnicity (Table 1). Slightly more boys (53%) than girls (47%) had an acute care visit. The distribution of patients across age categories was fairly even. Most patients had public (46%) or private (44%) health insurance coverage. Eight percent of patients had ≥4 visits to a study hospital within 1 year of their initial visit.
TABLE 1.
Patient Characteristics
| N = 47 175, No. (%) | |
|---|---|
| Demographics | |
| Age category at first visit | |
| 0–12 mo | 9559 (20) |
| 1–2 y | 9061 (19) |
| 3–5 y | 8062 (17) |
| 6–11 y | 10 057 (21) |
| 12–18 y | 10 436 (22) |
| Race and/or ethnicity | |
| Hispanic and/or Latino | 13 739 (29) |
| White | 13 086 (28) |
| Asian American | 8800 (19) |
| Black and/or African American | 6553 (14) |
| Multiracial, other, unknown | 4997 (11) |
| Sex | |
| Male | 25 162 (53) |
| Female | 22 013 (47) |
| Payer | |
| Public | 21 726 (46) |
| Private | 20 827 (44) |
| Uninsured | 3392 (7) |
| Unknown | 1230 (3) |
| Health systema | |
| Sutter | 22 041 (47) |
| ZSFGH | 17 401 (37) |
| UCSF | 7733 (16) |
| Acute care outcomes | |
| Diagnosis | |
| Any respiratory | 17 379 (37) |
| Asthma | 2635 (6) |
| Any injury and/or trauma | 15 920 (34) |
| Assault | 521 (1) |
| ACSC | 17 325 (37) |
| Visit frequency | |
| 1–3 visits | 43 376 (92) |
| ≥4 visits | 3799 (8) |
UCSF, University of California, San Francisco; ZSFGH, Zuckerberg San Francisco General Hospital and Trauma Center.
Health system of first visit. Approximately 4% of the population (n = 1858) visited >1 health system for acute care within 1 y of their initial visit.
Of the evaluated diagnoses, respiratory conditions were the most common (37%), and 15% of these patients were diagnosed with asthma (6% of the total sample). A similar proportion of patients had a visit for an ACSC (37%), which included some overlap with those patients with a respiratory diagnosis (Supplemental Table 3). Thirty-four percent of patients had an injury-related visit, and 3% of these (or 1% of the total sample) had a visit for assault.
Neighborhood Child Opportunity
More than half of all patients (58%) lived in neighborhoods that were ranked in the bottom 2 quintiles of child opportunity (Supplemental Table 5). However, this distribution varied by race and/or ethnicity and insurance status. Seventy-five percent of black and/or African American patients and 86% of Hispanic and/or Latino patients lived in neighborhoods with low or very low child opportunity compared with 27% of white children. Eighty-two percent of publicly insured patients lived in neighborhoods with low or very low child opportunity compared with 27% of privately insured patients.
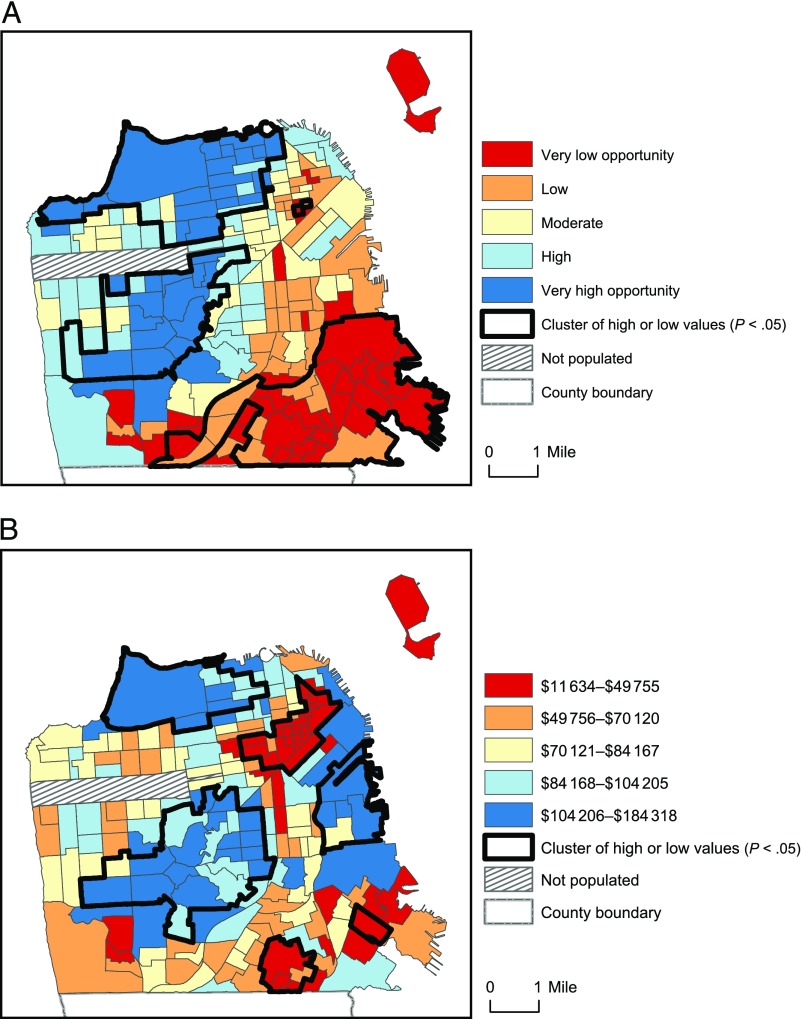
Spatial Analysis of Neighborhood Child Opportunity and Income
Neighborhood child opportunity had a unique spatial distribution compared with median household income (Fig 1). The Gi* cluster detection statistic was used to identify 30 tracts as significant clusters of low child opportunity values, and 27 tracts were in significant clusters of low-income values. Only 7 tracts were part of both low child opportunity and low-income clusters. Clusters of high child opportunity and high-income neighborhoods had greater spatial congruence but were still distinct; 42 and 35 tracts were identified as part of significant clusters of high child opportunity and median income values, respectively, and 17 of these tracts were part of both high child opportunity and high-income clusters. Because child opportunity and income were spatially distinct neighborhood measures and only moderately correlated in a bivariate analysis (r = 0.53), we included neighborhood-level income quintiles in all final adjusted models.
FIGURE 1.
A, Spatial distribution and clustering of the Child Opportunity Index by census tract quintiles in San Francisco, California (2007–2011). B, Spatial distribution and clustering of the median household income by census tract quintiles in San Francisco, California (2007–2011). The clusters of high or low values (black lines) were calculated by using the local Getis-Ord Gi* statistic. Clusters of high values (hot spots) are tracts with high values that are surrounded by tracts with high values; clusters of low values (cold spots) are tracts with low values that are surrounded by tracts with low values. A P value < .05 indicates a probability that is less than our α level that the observed concentration of high (or low) values is the result of a random spatial distribution.
Adjusted Models
After adjusting for individual-level confounders and neighborhood income, child opportunity was significantly associated with all evaluated pediatric acute care outcomes (Table 2). Children living in neighborhoods in the low and very low quintiles of child opportunity had 44% and 33% greater odds, respectively, of having ≥4 acute care visits within 1 year compared with children in the highest child opportunity neighborhoods. When modeled continuously, child opportunity was significantly and negatively associated with frequent acute care use (P trend = .001).
TABLE 2.
Adjusted Association Between Neighborhood Child Opportunity Index and Pediatric Acute Care Outcomes
| Outcome | Quintile Adjusted OR (95% CI)a | P trend | ||||
|---|---|---|---|---|---|---|
| Very Low | Low | Moderate | High | Very Highb | ||
| Frequent usec | 1.33* (1.03–1.73) | 1.44** (1.12–1.85) | 1.22 (0.95–1.59) | 0.95 (0.72–1.27) | 1 | .001 |
| Any respiratory | 1.17** (1.05–1.3) | 1.17** (1.06–1.29) | 1.03 (0.93–1.14) | 0.99 (0.91–1.09) | 1 | <.001 |
| Asthma | 1.27* (1.04–1.54) | 1.15 (0.95–1.40) | 1.08 (0.9–1.3) | 1.00 (0.83–1.19) | 1 | .002 |
| Any injury and/or trauma | 0.86* (0.77–0.97) | 0.87* (0.78–0.97) | 0.92 (0.83–1.01) | 0.97 (0.88–1.06) | 1 | .003 |
| Assault | 2.12** (1.27–3.54) | 1.91* (1.15–3.18) | 1.90* (1.14–3.16) | 1.53 (0.91–2.57) | 1 | .012 |
| ACSC | 1.25*** (1.12–1.39) | 1.24*** (1.12–1.37) | 1.09 (0.99–1.20) | 1.03 (0.94–1.14) | 1 | <.001 |
Adjusted ORs and 95% CIs from generalized estimating equation logistic regression models were adjusted for patient age, sex, race and/or ethnicity, primary payer, health system of first visit, and residential census tract median household income.
Reference group.
Four or more acute care visits to a study hospital within 1 y of first visit (2007–2011).
P < .05;
P < .01;
P < .001.
Results for the respiratory and ACSC diagnoses showed a similar pattern. Children living in low and very low child opportunity neighborhoods had greater odds of having a visit with a respiratory (low: OR 1.17 and 95% CI 1.06–1.29; very low: OR 1.17 and 95% CI 1.05–1.30) or ACSC (low: OR 1.24 and 95% CI 1.12–1.37; very low: OR 1.25 and 95% CI 1.12–1.39) diagnosis compared with children living in very high child opportunity neighborhoods. The graded, negative relationship between child opportunity and these outcomes was significant (P trend < .001). The association between an asthma diagnosis and child opportunity was only significant in the categorical analyses for children who lived in very low child opportunity neighborhoods (OR 1.27; 95% CI 1.04–1.54), but there was a trend of reduced odds for an asthma visit as child opportunity increased continuously (P trend = .002).
The results for injury were strikingly different. The graded association between child opportunity and having an acute care visit for any type of injury was positive (P trend = .003). Children in low and very low child opportunity neighborhoods had lower odds of having an acute care visit for an injury (low: OR 0.87; 95% CI 0.78–0.97; very low: OR 0.86; 95% CI 0.77–0.97) compared with children in the highest child opportunity neighborhoods. However, although the odds of a visit for any type of injury were lower for children in lower child opportunity neighborhoods, the odds of an assault-related injury were higher (P trend = .012). Children in very low–opportunity neighborhoods had >2 times the odds of having an acute care visit for an assault-related injury compared with children in the highest-opportunity neighborhoods (OR 2.12; 95% CI 1.27–3.54).
When modeled separately, neighborhood income and child opportunity had similar associations with all outcomes in terms of magnitude, direction, and significance (Supplemental Tables 7–12). In final models that included both neighborhood measures, the effect sizes for income and child opportunity were only modestly reduced (<15%) for frequent use, respiratory, asthma, injury, and ACSC outcomes (Supplemental Table 6). Neighborhood income remained significantly associated with respiratory, injury, and ACSC outcomes but not frequent use, asthma, or assault outcomes (Supplemental Table 13). Each of the 3 child opportunity domains had similar effect estimates compared with the composite Child Opportunity Index (Supplemental Table 14).
Discussion
This is the first study in which researchers use a population-level database to examine the independent effect of a composite measure of neighborhood risks and resources relevant to child development (the Child Opportunity Index) on individual-level pediatric acute care visits. Comparing the spatial distribution of neighborhood child opportunity and income revealed that child opportunity can be used to capture distinct aspects of neighborhood context and help identify different clusters of high- and low-risk neighborhoods. Neighborhood child opportunity was significantly associated with pediatric acute care visit frequency and a range of diagnoses after controlling for patient-level characteristics and area-level income.
Children who lived in neighborhoods with low levels of child opportunity were substantially more likely to be frequent users of acute care. Compared with children in neighborhoods with the highest levels of child opportunity, children in low-opportunity neighborhoods were also more likely to be treated for any type of respiratory condition (including asthma), require care for assault, or be diagnosed with an ACSC. Consistent with previous work,7–11 neighborhood income was also negatively associated with pediatric acute care visits for these outcomes. However, our final models revealed that neighborhood opportunity had an independent and significant association with all evaluated outcomes, whereas neighborhood income was not significantly associated with frequent acute care use, visits for asthma, or visits for assault. Compared with neighborhood income, child opportunity had a stronger association with those outcomes and an equally strong association with visits for respiratory issues, injury, and ACSCs.
These findings reveal a need to consider a wider range of risks and resources relevant to neighborhood-level disparities in child health care use. The Child Opportunity Index integrates measures used to assess social, economic, education, and environmental domains and provides a more complete picture of modifiable neighborhood conditions that, if altered, might improve child health and health equity. With the Child Opportunity Index, we identified different clusters of high-risk neighborhoods compared with neighborhood income, suggesting that community health needs in these neighborhoods would be overlooked by spatial measures of income alone.
The positive association we found between child opportunity and having an acute care visit for any type of injury runs counter to a previous review that revealed substantial evidence of an inverse association between socioeconomic conditions and unintentional child injuries of all major causes.26 However, researchers in other work have reported greater ED use for injuries for children from neighborhoods of higher socioeconomic status and suggest that this pattern may be related to referral patterns or issues of parental decision-making,11 which are beyond the scope of the current study. Our finding that acute care visits for assault injuries is inversely related to child opportunity points to the need for additional research on the neighborhood-level factors that are associated with these particular types of injuries.
These results have important implications for pediatric patient care, place-based health interventions, and population health science. Patients are increasingly screened for unmet social needs, such as food or housing insecurity, and referred to local service providers.38 However, the uneven spatial distribution of childhood opportunity and its association with pediatric health care use indicates that many neighborhoods are not equipped with the resources needed to support child health. Effective health promotion and the prevention of ED visits for children in these neighborhoods may require place-based interventions to improve access to essential resources and/or reduce exposure to environmental harms.15
The Child Opportunity Index is a valuable tool to inform such efforts. It is publicly available to the 100 largest US metropolitan areas and could be integrated into regional health systems’ and public health agencies’ community health needs assessments and strategies to improve child health equity.39 The variety of measures included in the index can help engage community partners across sectors (such as educators, city planners, housing developers, and public health professionals) in community health evaluation and implementation strategies.
The widespread use of EHRs40 enables new opportunities to use tools such as the Child Opportunity Index for spatial analysis of health data to understand, monitor, and address health disparities for vulnerable populations and places. The Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records recommends incorporating geocodeable addresses in EHRs to allow for the assessment of census tract median incomes.41 Indeed, we found that neighborhood income remained independently associated with 3 of the 6 evaluated pediatric acute care measures in this study. But our findings go further; we suggest that for pediatric patients, neighborhood child opportunity would also be a useful measure to include.
This study has several limitations. First, we were not able to adjust for household socioeconomic characteristics, such as income, because data were not available. We adjusted for insurance status as a proxy for socioeconomic status,42 but this may miss other household-level drivers of health.5,43 Second, our sample does not include all hospitals in San Francisco. However, we linked data across 3 large health systems that cared for 80% of all San Francisco residents 0 to 18 years old with ED visits from 2007 to 2011, and 87% of those who were publicly insured.44 Third, the generalizability of our results may be limited because of the unique characteristics of our study area, such as higher housing costs and median household income, compared with other US cities. Fourth, ICD-9-CM codes are imperfect measures of health,45 but they are the best available measures of population-level health care use. Lastly, the data are cross-sectional and therefore can only be used to infer correlational, rather than causal, relationships between child opportunity and pediatric acute care use.
As with all composite measures of neighborhood context, the Child Opportunity Index offers only partial guidance for determining what programs and policies will have the greatest impact on child health. Analyses in which researchers for this study compare the 3 domains of child opportunity reveal that no single domain was driving the results and that, for most outcomes, the composite Child Opportunity Index was the strongest predictor. Additional research is needed to determine if specific components of child opportunity should be prioritized for place-based or population-level interventions. Nonetheless, other countries have successfully used composite indices to understand the distribution of health outcomes, which suggests that the Child Opportunity Index could be meaningfully used to assess and monitor community needs, guide resource allocation, and ultimately improve health equity.20
Conclusions
By linking individual-level health care use data and a novel measure of neighborhood context, we demonstrate that lower neighborhood child opportunity is associated with increased pediatric use of acute care medical services and visits for diagnoses that are preventable and/or effectively treated in a primary care setting. Even in one of the wealthiest and most progressive cities in the United States, some neighborhoods expose children to harmful risks, have limited access to essential resources, and are associated with greater child health care use. Clinical service providers, health system administrators, public health practitioners, and health equity advocates should consider using the Child Opportunity Index to guide treatment, prevention, and intervention strategies to better address the disparate and multifaceted neighborhood contexts in which children live.
Glossary
- ACSC
ambulatory care–sensitive condition
- CI
confidence interval
- ED
emergency department
- EHR
electronic health record
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- OR
odds ratio
Footnotes
Dr Kersten conceptualized and designed the study, contributed to the acquisition of data, conducted the data integration and analyses, and drafted and revised the manuscript; Dr Adler was the principal investigator of the studies that were used to support the acquisition and integration of the clinical data, contributed to the analyses and interpretation of data, and critically reviewed the manuscript; Drs Jutte and Gottlieb contributed to the acquisition, analyses, and interpretation of data and critically reviewed the manuscript; Dr Roundfield contributed to the conceptualization and design of the study and interpretation of data and critically reviewed the manuscript; Ms Robinson contributed to the acquisition and interpretation of data and critically reviewed the manuscript; Dr LeWinn conceptualized and designed the study, contributed to the acquisition, analyses, and interpretation of data, and contributed to the writing and revision of the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded in part by National Institutes of Health grants 2T32MH018261-31 (Dr Kersten) and K01MH097978 (Dr LeWinn) as well as the Health Disparities Working Group (which is funded by the University of California, San Francisco and the Robert Wood Johnson Foundation [Dr Kersten]) and a Ford Foundation Postdoctoral Fellowship funded by the Ford Foundation and the National Academy of Sciences (Dr Roundfield). The collection and integration of the data were supported by funding from the John D. and Catherine T. MacArthur Foundation Research Network on Socioeconomic Status and Health and from the Lisa and John Pritzker Family Fund (Dr Adler). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Wier L, Yu H, Owens P, Washington R Statistical brief #157: overview of children in the emergency department, 2010. Available at: www.hcup-us.ahrq.gov/reports/statbriefs/sb157.pdf. Accessed November 13, 2016 [PubMed]
- 2.Rasooly IR, Mullins PM, Alpern ER, Pines JM. US emergency department use by children, 2001-2010. Pediatr Emerg Care. 2014;30(9):602–607 [DOI] [PubMed] [Google Scholar]
- 3.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997-2007. JAMA. 2010;304(6):664–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alpern ER, Clark AE, Alessandrini EA, et al. ; Pediatric Emergency Care Applied Research Network . Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21(4):365–373 [DOI] [PubMed] [Google Scholar]
- 5.Ben-Isaac E, Schrager SM, Keefer M, Chen AY. National profile of nonemergent pediatric emergency department visits. Pediatrics. 2010;125(3):454–459 [DOI] [PubMed] [Google Scholar]
- 6.Simpson L, Owens PL, Zodet MW, et al. Health care for children and youth in the United States: annual report on patterns of coverage, utilization, quality, and expenditures by income. Ambul Pediatr. 2005;5(1):6–44 [DOI] [PubMed] [Google Scholar]
- 7.Suruda A, Burns TJ, Knight S, Dean JM. Health insurance, neighborhood income, and emergency department usage by Utah children 1996-1998. BMC Health Serv Res. 2005;5(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaeger MW, Ambadwar PB, King AJ, Onukwube JI, Robbins JM. Emergency care of children with ambulatory care sensitive conditions in the United States. J Emerg Med. 2015;49(5):729–739 [DOI] [PubMed] [Google Scholar]
- 9.Fieldston ES, Zaniletti I, Hall M, et al. Community household income and resource utilization for common inpatient pediatric conditions. Pediatrics. 2013;132(6). Available at: www.pediatrics.org/cgi/content/full/132/6/e1592 [DOI] [PubMed] [Google Scholar]
- 10.Brooks-Gunn J, McCormick MC, Klebanov PK, McCarton C. Health care use of 3-year-old low birth weight premature children: effects of family and neighborhood poverty. J Pediatr. 1998;132(6):971–975 [DOI] [PubMed] [Google Scholar]
- 11.Macy ML, Zonfrillo MR, Cook LJ, et al. ; Pediatric Emergency Care Applied Research Network . Patient- and community-level sociodemographic characteristics associated with emergency department visits for childhood injury. J Pediatr. 2015;167(3):711–718.e1–e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson RC, Schoeni RF, Rogowski JA. Health disparities in mid-to-late life: the role of earlier life family and neighborhood socioeconomic conditions. Soc Sci Med. 2012;74(4):625–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McGovern L, Miller G, Hughes-Cromwick P Health policy brief: the relative contribution of multiple determinants to health. August 21, 2014. Available at: https://www.healthaffairs.org/do/10.1377/hpb20140821.404487/full/
- 14.Shonkoff JP, Phillips DA, eds; National Research Council; Institute of Medicine . From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: The National Academies Press; 2000 [PubMed] [Google Scholar]
- 15.Jutte DP, Miller JL, Erickson DJ. Neighborhood adversity, child health, and the role for community development. Pediatrics. 2015;135(suppl 2):S48–S57 [DOI] [PubMed] [Google Scholar]
- 16.Evans GW, Kim P. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status-health gradient. Ann N Y Acad Sci. 2010;1186:174–189 [DOI] [PubMed] [Google Scholar]
- 17.Lessard LN, Alcala E, Capitman JA. Pollution, poverty, and potentially preventable childhood morbidity in Central California. J Pediatr. 2016;168:198–204 [DOI] [PubMed] [Google Scholar]
- 18.Sandel M, Faugno E, Mingo A, et al. Neighborhood-level interventions to improve childhood opportunity and lift children out of poverty. Acad Pediatr. 2016;16(suppl 3):S128–S135 [DOI] [PubMed] [Google Scholar]
- 19.Acevedo-Garcia D, McArdle N, Hardy EF, et al. The child opportunity index: improving collaboration between community development and public health. Health Aff (Millwood). 2014;33(11):1948–1957 [DOI] [PubMed] [Google Scholar]
- 20.Phillips RL, Liaw W, Crampton P, et al. How other countries use deprivation indices-and why the United States desperately needs one. Health Aff (Millwood). 2016;35(11):1991–1998 [DOI] [PubMed] [Google Scholar]
- 21.Kersten EE, LeWinn KZ, Gottlieb L, Jutte DP, Adler NE. San Francisco children living in redeveloped public housing used acute services less than children in older public housing. Health Aff (Millwood). 2014;33(12):2230–2237 [DOI] [PubMed] [Google Scholar]
- 22.Liu SW, Nagurney JT, Chang Y, Parry BA, Smulowitz P, Atlas SJ. Frequent ED users: are most visits for mental health, alcohol, and drug-related complaints? Am J Emerg Med. 2013;31(10):1512–1515 [DOI] [PubMed] [Google Scholar]
- 23.Berkowitz SA, Traore CY, Singer DE, Atlas SJ. Evaluating area-based socioeconomic status indicators for monitoring disparities within health care systems: results from a primary care network. Health Serv Res. 2015;50(2):398–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beck AF, Florin TA, Campanella S, Shah SS. Geographic variation in hospitalization for lower respiratory tract infections across one county. JAMA Pediatr. 2015;169(9):846–854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McClure R, Kegler S, Davey T, Clay F. Contextual determinants of childhood injury: a systematic review of studies with multilevel analytic methods. Am J Public Health. 2015;105(12):e37–e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laflamme L, Hasselberg M, Burrows S. 20 years of research on socioeconomic inequality and children’s—unintentional injuries understanding the cause-specific evidence at hand. Int J Pediatr. 2010;2010:1–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guttmann A, Shipman SA, Lam K, Goodman DC, Stukel TA. Primary care physician supply and children’s health care use, access, and outcomes: findings from Canada. Pediatrics. 2010;125(6):1119–1126 [DOI] [PubMed] [Google Scholar]
- 28.Beck AF, Simmons JM, Huang B, Kahn RS. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102(12):2308–2314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beck AF, Moncrief T, Huang B, et al. Inequalities in neighborhood child asthma admission rates and underlying community characteristics in one US county. J Pediatr. 2013;163(2):574–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ballard ED, Kalb LG, Vasa RA, Goldstein M, Wilcox HC. Self-harm, assault, and undetermined intent injuries among pediatric emergency department visits. Pediatr Emerg Care. 2015;31(12):813–818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Institute for Child Youth and Family Policy; Brandeis University diversitydatakids.org. 2015. Available at: www.diversitydatakids.org/. Accessed November 20, 2015
- 32.Neuman MI, Alpern ER, Hall M, et al. Characteristics of recurrent utilization in pediatric emergency departments. Pediatrics. 2014;134(4). Available at: www.pediatrics.org/cgi/content/full/134/4/e1025 [DOI] [PubMed] [Google Scholar]
- 33.LeDuc K, Rosebrook H, Rannie M, Gao D. Pediatric emergency department recidivism: demographic characteristics and diagnostic predictors. J Emerg Nurs. 2006;32(2):131–138 [DOI] [PubMed] [Google Scholar]
- 34.American FactFinder; US Census Bureau Community facts. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed October 5, 2016
- 35.Esri Hot spot analysis (Getis-Ord Gi*). 2016. Available at: http://desktop.arcgis.com/en/arcmap/10.3/tools/spatial-statistics-toolbox/hot-spot-analysis.htm. Accessed April 10, 2017
- 36.Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geogr Anal. 1992;24(3):189–206 [Google Scholar]
- 37.Hubbard AE, Ahern J, Fleischer NL, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474 [DOI] [PubMed] [Google Scholar]
- 38.Chung EK, Siegel BS, Garg A, et al. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Curr Probl Pediatr Adolesc Health Care. 2016;46(5):135–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Acevedo-Garcia D, Hardy EF, McArdle N, et al. The Child Opportunity Index: Measuring and Mapping Neighborhood-Based Opportunities for U.S. Children. Waltham, MA and Columbus, OH: Brandeis University and The Ohio State University; 2016 [Google Scholar]
- 40.Casey JA, Schwartz BS, Stewart WF, Adler NE. Using electronic health records for population health research: a review of methods and applications. Annu Rev Public Health. 2016;37:61–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Institute of Medicine Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: The National Academies Press; 2014 [PubMed] [Google Scholar]
- 42.Grineski SE, Staniswalis JG, Peng Y, Atkinson-Palombo C. Children’s asthma hospitalizations and relative risk due to nitrogen dioxide (NO2): effect modification by race, ethnicity, and insurance status. Environ Res. 2010;110(2):178–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flores G, Olson L, Tomany-Korman SC. Racial and ethnic disparities in early childhood health and health care. Pediatrics. 2005;115(2). Available at: www.pediatrics.org/cgi/content/full/115/2/e183 [DOI] [PubMed] [Google Scholar]
- 44.von Bernath H. Emergency Room Database Custom Run #2130128-01. Sacramento, CA: Office of Statewide Health Planning and Development; 2013 [Google Scholar]
- 45.O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40(5, pt 2):1620–1639 [DOI] [PMC free article] [PubMed] [Google Scholar]