Abstract
Background:
Falls are a common concern for wheeled mobility device users with multiple sclerosis (MS); however, no evidence-based fall prevention programs have been developed to meet the specific needs of the population. We examine the preliminary feasibility of a fall management intervention in wheeled mobility device users with MS.
Methods:
Study participants were exposed to an intervention program targeting risk factors for falls, including transfer skills and seated postural control. The feasibility of the program was evaluated by assessing participant perspectives, cost, recruitment rates, study adherence, participant retention, safety, and the ability to collect primary and secondary outcomes, including fall frequency, concerns about falling, transfer quality, and seated postural control.
Results:
16 wheeled mobility device users completed the program, which was found to be feasible and was positively evaluated by participants. No adverse events were experienced. After exposure to the intervention, fall frequency significantly decreased (P < .001) and transfer quality (P = .001) and seated postural control (P = .002) significantly improved. No significant differences were found regarding concerns about falling (P = .728).
Conclusions:
This study examined the feasibility of an intervention program to manage fall risk in wheeled mobility device users with MS. The program was found to be feasible, and preliminary results showed the intervention to be effective in decreasing fall frequency. Additional testing is needed to further examine the efficacy and long-term impact of the intervention.
Falls are a common concern in persons affected by multiple sclerosis (MS). Falls may result in physical injury that requires hospitalization1 and/or development of a dysfunctional fear of falling.2 Approximately two-thirds of the MS population report concerns about falling3 that might result in self-imposed activity curtailment, loss of confidence, difficulty performing typical societal roles, loss of independence, and physiologic deconditioning.4 Ultimately, this disuse-disability cycle may place individuals at greater risk for falls.
The adverse physical and psychosocial impact of falls has led to a growing amount of research examining prevention strategies to decrease the frequency of falls in ambulatory individuals.5 Overall, this work has highlighted that some fall risk factors, such as impaired balance and functional mobility, are modifiable, and there is great potential to prevent falls in people with MS using targeted rehabilitation interventions.6
Unfortunately, most research in the MS population thus far has focused almost exclusively on community ambulators. This focus ignores the approximately 25% of the MS population who use a wheeled mobility device (manual wheelchair, power wheelchair, scooter, etc.) as their primary means of community mobility.7 Owing to the differences in physical characteristics (eg, muscle strength, balance impairments) and functional mobility limitations (eg, assistive devices used) between ambulatory and wheeled mobility device users with MS, individualized investigation of unique strategies to prevent falls is needed. Indeed, there is evidence that approximately 45% of individuals with MS who use a wheeled mobility device as their primary means of mobility report at least one fall per 6-month period, and approximately 30% of those fallers report frequent falls.8
A recent literature review of wheeled mobility device users with various disabilities evaluated factors related to fall risk.9 Results indicate that transfers (ie, moving from a wheelchair/scooter to another surface, such as a bed or chair) were found to be associated with falls in 54.5% of the studies reviewed and impaired seated balance control was associated with falls in 36.3% of the studies evaluated. A lack of fall prevention interventions for wheeled mobility device users was also noted. Importantly, there were no fall prevention programs specifically for individuals with MS who use wheeled mobility devices.9
Therefore, the purpose of this article is to describe an intervention program designed to prevent falls and concerns about falling by targeting risk factors associated with falls in wheeled mobility device users, to describe the preliminary feasibility of the program, and to report preliminary results. To our knowledge, this is the first study to describe the implementation of an intervention program to manage falls and concerns about falling in wheeled mobility device users with MS. It was hypothesized that the program will be feasible and that, after exposure to the intervention program, participants will display improved transfer quality and seated postural control and a decreased frequency of falls and concerns about falling.
Methods
Study Design
A single-group interventional study was performed to examine the preliminary feasibility and efficacy of an intervention program to decrease fall frequency and concerns about falling in wheeled mobility device users with MS. All study-related procedures were approved by the institutional review board of the University of Illinois at Urbana-Champaign. A sample of convenience of 16 participants was recruited through the North American Research Committee on Multiple Sclerosis (NAR-COMS) research registry, posting of flyers, and word of mouth. Individuals were invited to participate if they met the following inclusion criteria: a diagnosis of MS, older than 18 years, self-reported Patient-Determined Disease Steps10 level of 7 (ie, main form of mobility is via a wheeled mobility device), self-reported inability to ambulate outside the home, and self-reported ability to transfer with moderate assistance (participant expends 50%–74% of the effort) or less. Exclusion criteria included an MS exacerbation in the past 30 days and unable to sit upright for at least 1 hour.
After participants were enrolled in the study and signed an institutional review board–approved informed consent form, a baseline assessment was performed, as described herein. After collection of baseline data, an intervention program to manage fall risk and concerns about falling was implemented. Details regarding the content of the intervention are provided herein. All the participants were reevaluated 12 weeks later using the same protocol performed during the baseline assessment.
Feasibility
As suggested by Thabane et al.,11 feasibility outcomes include the assessment of cost, recruitment and retention rates, adherence to the proposed program, safety, and the ability to collect primary and secondary outcomes. The cost of the study was calculated by summing all of the direct costs associated with performance of the study. Indirect costs to support administrative activities were not included. The recruitment rate was assessed by calculating the percentage of participants who enrolled in the study from the pool of known participants who were exposed to the recruitment materials. Study adherence was evaluated by assessing the number of self-reported exercise sessions performed by participants and the number of times participants self-reported that they reviewed the transfer education materials. The retention rate was calculated as a percentage of the number of participants who completed both study visits and engaged in the intervention program. Safety was evaluated by assessing the number of adverse events self-reported by participants. Finally, the ability to collect primary and secondary outcomes was assessed by evaluating the amount of missing data that occurred during each assessment and examination of the outcome assessments performed.
Participant Perspectives
Participant perspectives on the study were evaluated by asking direct questions about the content of the intervention program. Perspectives were examined in a one-on-one interview during the postintervention assessment. Participants were asked whether they found the transfer education to be helpful, whether they significantly changed the way they performed their transfers, and whether they felt that the exercise program significantly improved their sitting balance abilities. Finally, participants were asked to provide any other feedback they had about the program.
Outcome Assessments
During the baseline assessment, participants completed a general demographic questionnaire and were asked information about the length of time they had had MS, wheeled mobility use, and the frequency of falls in the previous 6 months. A fall was defined as “unintentionally coming to rest on the ground or lower level.”12 Participants were also asked to complete the Spinal Cord Injury–Falls Concern Scale (SCI-FCS).13 The SCI-FCS examines concerns about falling by asking participants to rate the level of concern they have about falling on a 4-point scale ranging from 1 = not at all concerned to 4 = very concerned when performing 16 common activities of daily living. Total scores range from 16 to 64. The SCI-FCS has not been validated in individuals with MS but evaluates activities pertinent to a variety of nonambulatory individuals. In the spinal cord injury population, the SCI-FCS has excellent internal and test-retest reliability (Cronbach α = 0.92, intraclass correlation coefficient = 0.93).13 There is currently no validated tool available to evaluate fall concerns during functional activities in individuals with MS who use a wheeled mobility device.9
After completion of the surveys, participants were asked to perform up to four transfers to and from a solid mat table. Participants were instructed to perform the transfers as they normally would at home, and they could use any type of assistive device, such as a transfer board, as preferred. Participants could also receive assistance from a caregiver, if necessary. Transfer quality was objectively evaluated using the Transfer Assessment Instrument (TAI)14 by a trained researcher. Items such as hand placement or the distance from the target surface are assessed, not how much assistance the participant requires. A final score is given ranging from 0 = very poor transfer quality to 10 = excellent transfer quality. The TAI has been found to be valid and reliable in full-time wheelchair users, including individuals with MS.15
Seated postural control was evaluated using a Bertec force plate (model FP4060-05; Bertec Inc, Columbus, OH). Per the protocol established by Shin and Sosnoff,16 seated postural control was assessed by having participants sit with their arms resting in their lap with both their feet and back unsupported for 30 seconds. After the quiet sitting trial, participants were instructed to lean as far forward, backward, and side-to-side as possible in a circular pattern for 30 seconds to assess the functional boundary of stability. The functional boundary of stability examines how far a participant is capable of leaning without loss of balance. From the force plate data obtained, virtual time to contact was calculated.17 Virtual time to contact quantifies the temporal proximity of an individual to their functional stability boundary16 and takes into consideration the relationship between center of pressure and the borders of the functional base of support,18 as described in Figure 1.
Figure 1.
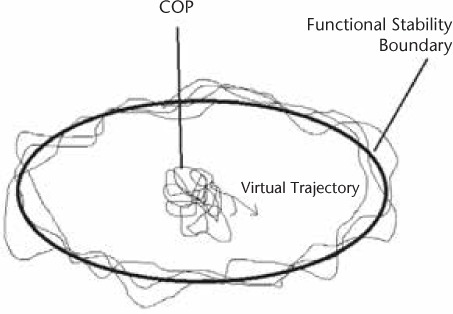
Visual representation of the functional boundary of stability and center of pressure (COP)
Per Slobounov et al.,17 virtual time to contact was calculated using a position vector of the center of pressure on a virtual trajectory, τi (t), determined for each moment in time, ti during static sitting, on the basis of the instantaneous center of pressure velocity and acceleration:
where rxi,yi(ti) is the instantaneous position vector, vxi,yi(ti) is the instantaneous velocity vector, and axi,yi (ti) is the instantaneous acceleration vector in the x and y directions. Higher values indicate increased stability. The entire assessment performed at the baseline study visit was repeated at the 12-week study visit. After completion of the 12-week study visit, participants were asked a series of questions to examine their perceived functional changes as a result of the intervention program.
Intervention Program
After completing the baseline assessment, participants were exposed to an education intervention focused on improving the quality of transfer skills and seated postural control to decrease fall frequency and concerns about falling. The education was provided to study participants in individual sessions by a physical therapist during a single session that lasted approximately 45 minutes. The education was implemented in a private room with a height-adjustable mat table with sufficient room for participants to perform transfers and seated exercises. The intervention was developed by a physical therapist (L.A.R.) with more than 10 years of experience providing instruction to wheeled mobility device users.
Transfer Quality
First, participants received instruction on transfer quality focused on how to perform transfers in a safe manner to reduce the frequency of falls and concerns about falling. The information presented was informed from previous research describing the circumstances of falls among wheeled mobility device users with other disabilities19 and transfer biomechanics.20 To our knowledge, there are currently no other peer-reviewed fall prevention interventions designed for wheeled mobility device users with MS.9 During the intervention, participants were individually shown a 9-minute video describing how to correctly perform a transfer. The video broke down the performance of a transfer into three phases: setup, flight, and end phases. For example, participants were educated to place their feet on the floor, whenever possible, to create a solid base of support during the flight phase of the transfer. Paper handouts that mirrored the information presented in the video were also given to participants. Separate materials were developed for participants performing independent and assisted transfers (Appendix S1 [parts a and b] (1.7MB, pdf) , which is published in the online version of this article at ijmsc.org). As the video played, the physical therapist would frequently stop the video to discuss specific aspects of the transfer that the participant had difficulty performing during the baseline assessment or to answer questions posed by the participant. After completion of the video, the participant was given an opportunity to practice the transfers. Feedback on performance was provided and individual technique was fine-tuned by the physical therapist. Participants were given a copy of the paper handouts and video to take home. Participants were instructed to review the materials at least once every other week.
Exercise Protocol
Next, participants were instructed on exercises designed to improve seated postural control. The protocol was designed by a physical therapist (L.A.R.) using exercises described by Kisner and Colby21 to be performed in the participant's home without any equipment. Participants were individually instructed on how to perform the exercises and were given a paper handout describing exercise techniques (Appendix S2 (1.7MB, pdf) ). After instruction, participants were given an opportunity to practice the exercises and received feedback on their performance by the physical therapist. If needed, the exercises were modified for individual participants based on their strength impairments and other limitations. Participants were instructed to perform the exercises three times per week.
Participant Monitoring
Between the baseline and 12-week study visits, participants were called every other week to inquire about their adherence to the intervention program. Participants were asked whether they had any questions about the transfer techniques and to remind them to watch the instructional transfer video every other week. Participants were also asked how well they were tolerating the exercise program. If participants reported that the exercises were too easy, they were instructed to increase the frequency of performance, and to reduce the frequency if too difficult. Participants were also asked to report the frequency of their falls during the past 2 weeks. To ensure that the frequency of falls was collected in an objective, nonbiased manner, a standardized script was used.
Data Analysis
Data were analyzed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp, Armonk, NY). Descriptive statistics were used to evaluate feasibility. To evaluate program outcomes, general exploratory analysis was performed, and Shapiro-Wilk testing found virtual time to contact to be normally distributed. All other variables of interest were found to be nonnormally distributed or used ordinal data. To examine the differences before and after exposure to the intervention, paired t tests (normally distributed data) and a generalized linear model (nonnormally distributed/ordinal data) were used. Effect sizes (d) were calculated using Cohen's dz. Per Lakens,22 Cohen's dz values were calculated by examining the differences in mean scores between assessment points divided by the SD of the difference scores and were interpreted as small (d ≤ 0.2), moderate (d ∼ 0.5), or large (d ≥ 0.8). Significance was set a priori at P = .05. Due to the pilot nature of the study, no corrections were made for multiple comparisons.
Results
Study Participants
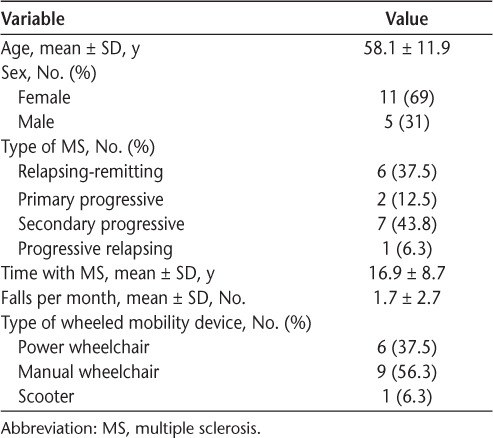
Between May 1, 2014, and May 31, 2015, 16 participants were enrolled and tested (Figure 2). All the participants completed both study visits. Participants had a mean ± SD age of 58.1 ± 11.9 years and duration of diagnosis of MS of 16.9 ± 8.7 years. At the start of the study, 75% of participants reported at least one fall in the past 6 months, with a mean ± SD fall frequency of 1.7 ± 2.7 per month (Table 1).
Figure 2.
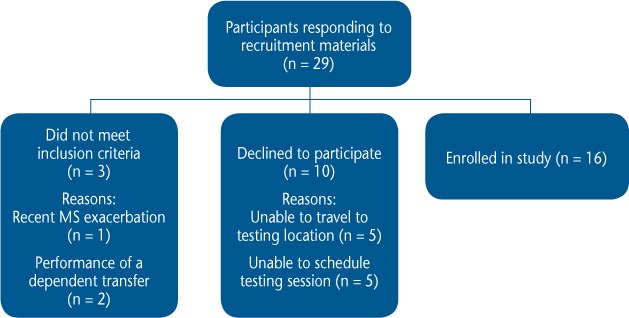
Participant recruitment
MS, multiple sclerosis
Table 1.
Demographic and baseline data for the 16 study participants
Feasibility
Based on the criteria established by Thabane et al.,11 the study was found to be feasible but requires modifications. All the participants who started the study completed both assessment sessions and the intervention program, and no participants reported injuries or impairments associated with the intervention program. The direct costs associated with the study were approximately $30,000 ($1875 per participant) and included salary support for personnel ($25,000), development and production of transfer education videos ($800), general materials to support the study (including participant handouts) ($500), participant payments ($2000), and recruitment expenses ($1700). In addition, a $10,000 force platform was used to evaluate seated postural control that was previously owned by the research team.
Study recruitment materials were sent to 137 individuals within an approximately 3-hour driving distance from the research laboratory, and 29 (21%) responded. Of the 29 people who responded, 16 (55%) were enrolled in the study, 10 (35%) declined to participate after learning more about the study, and 3 (10%) did not meet the inclusion criteria (Figure 2).
Participants self-reported viewing the transfer education video a mean ± SD of 3.5 ± 2.7 times and performing the exercises a mean ± SD of 2.86 ± 1.92 times per week. Regarding data collection, missing data occurred for two participants during collection of the SCI-FCS data, and one participant did not complete the patient perspective questions. No missing data occurred for the other outcomes of interest.
Participant-Perceived Improvements
The intervention was well-tolerated, and no participants reported injuries or impairments associated with the intervention. When asked “Did you find the transfer education helpful?” most participants (n = 14 [87.5%]) reported that they did. Twelve of 15 participants (80%; one participant did not provide a response) responded in a positive manner when asked “Did you significantly change the way you perform your transfers?” When asked to describe the changes that were made, six participants reported that they changed how they positioned their body, five changed how they positioned their chair, four reported changing their overall technique, and four reported taking more precautions during their transfers.
Regarding the exercises, when asked “Do you feel that the exercises significantly improved your sitting balance,” 13 of 15 participants (86.7%; one participant did not provide a response) reported significant improvements. In response to the question “Do you have any other comments about the transfer and exercise education?” eight participants provided a response. Regarding the structure of the education materials, two participants thought the materials were organized well, and one participant did not like the materials (but did not specify why). Regarding the difficulty of the exercises, two participants felt that the exercises were too hard, and one felt that they were too easy. Finally, one participant wished that the materials were more specific to individuals with MS, and one thought that the monitoring was helpful.
Fall Frequency and Concerns About Falling
Fall frequency was found to be nonnormally distributed (Shapiro-Wilk P < .001), and the SCI-FCS score is measured on an ordinal scale; therefore, nonparametric statistics were used to evaluate both variables. At the 12-week study visit, participants reported a significant mean ± SD reduction in fall frequency (preintervention: 1.7 ± 2.7 falls/mo; postintervention: 1.0 ± 1.2 falls/mo; P < .001, dz = 0.26) (Table 2). No significant differences were found in mean ± SD SCI-FCS scores (preintervention: 33.07 ± 7.5, postintervention: 32.8 ± 11.3, P = .728, dz = 0.01).
Table 2.
Differences in outcomes preintervention to postintervention
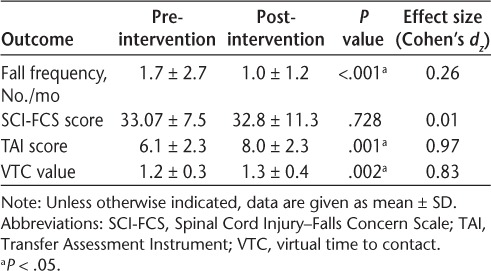
Transfer Quality
Transfer quality, as measured by the TAI, is ordinal in nature; therefore, nonparametric statistics were used. After exposure to the intervention, participants showed significant improvements in mean ± SD TAI scores (preintervention: 6.1 ± 2.3, postintervention: 8.0 ± 2.3, P = .001, dz = 0.97) (Table 2).
Seated Postural Control
Seated postural control, as evaluated by virtual time to contact, was found to be normally distributed (Shapiro-Wilk P = .553). After exposure to the intervention, mean ± SD values of virtual time to contact significantly improved (preintervention: 1.2 ± 0.3, postintervention: 1.3 ± 0.4, P = .002, dz = 0.83) (Table 2).
Discussion
The primary results of this feasibility study indicate that an intervention program designed to decrease fall frequency and concerns about falling by providing education on methods to improve transfer quality and exercises to improve seated postural control was feasible to perform, well tolerated, and received in a positive manner by study participants. Subjectively, most participants reported that they significantly changed the way they performed their transfers and that the exercises significantly improved sitting balance. Objectively, fall frequency significantly decreased and transfer quality and seated postural control significantly improved after exposure to the intervention. No significant differences were found regarding concerns about falling. Further testing is needed to examine the long-term impact of the intervention in a larger group of wheeled mobility device users with MS. Due to the complex nature of falls, a longer follow-up period with additional study participants is necessary to examine the full impact of the intervention.
The results of the feasibility and subjective analysis indicate that the intervention is possible, well tolerated, and perceived to be beneficial by study participants. The cost of the study is an area of concern. The direct costs associated with the study totaled approximately $40,000, including the cost of the force plate ($10,000), which, although not excessive, requires considerable resources. To reduce cost, future studies may consider use of the Function In Sitting Test23 to assess seated postural control instead of using a force plate. Our research team recently assessed the reliability and validity of the tool in nonambulatory individuals with MS and found it to be reliable and valid.24 Funds to support the salaries of the study investigators developing the study protocol may also be reduced in future iterations of the study. To perform the study intervention using the currently developed materials, we anticipate the cost to be approximately $12,200. These costs would include general study materials, including participant handouts, DVDs, etc. ($500); participant payments ($2000: $100/participant plus travel expenses); recruitment expenses ($1700); and payment of a research assistant to implement the study intervention ($8000).
The recruitment rate of study participants is also an area of concern. Five of the ten participants who declined to participate did so due to transportation limitations. Independent transportation is particularly difficult for individuals who would meet the inclusion criteria. Also, the study was performed in a rural area with limited accessible public transportation. In the future, researchers should consider performing the study in a metropolitan area in which participants can use an extensive network of accessible public or paratransit resources. In addition, future studies should examine the feasibility and validity of converting the intervention program into an Internet-based program with the capacity to remotely evaluate transfer and exercise performance for individuals with limited resources to participate in in-person therapeutic activities.
After exposure to the education intervention, preliminary results showed that transfer quality significantly improved, and a large effect size was noted. Such improvements are noteworthy as transfers are frequently associated with falls.9 Improving quality, therefore, has a good potential to positively influence fall frequency. Improvements in functional mobility and community participation may also be seen as a result of improved transfer quality, however further testing is needed to examine these concepts.
Similar results were found by Rice et al.25 in an examination of full-time wheelchair users with spinal cord injury who received a structured transfer education intervention during acute inpatient rehabilitation. In this previous study, however, the program had a greater impact on participants who required assistance to transfer. The present results, however, found the program to be effective among participants performing independent transfers.
In addition to transfers, impaired seated postural control has previously been found to be associated with falls in wheeled mobility device users.9 Thus, the significant improvements seen in seated postural control potentially had an influence on fall frequency. To our knowledge, no previous studies have examined the impact of an exercise program targeting improvements in seated postural control on fall frequency. A recent study in older ambulatory adults with MS by Sosnoff et al.26 found similar results that indicate that a home-based exercise program can reduce fall risk.
In addition to the potential effect on fall frequency, improvements in seated postural control are important because impaired balance can affect a variety of functional activities necessary for performing activities of daily living. Not only does impaired balance affect an individual's ability to transfer and remain upright when sitting unsupported, necessary functional activities such as cooking, bathing, and dressing are also negatively affected. Further investigation is needed to examine the long-term impact of the intervention program and to determine whether differences exist in a larger group of participants over a longer period.
After exposure to the intervention, fall frequency significantly decreased, although a small effect size was found. Programs designed to prevent falls from occurring are important because falls can result in substantial physical1 and psychological impairments.2 A recent study by Bisson et al.27 found that after a fall, 27.6% of individuals with MS lay on the floor or ground for more than 10 minutes and 4.7% were on the ground for more than an hour. Such wait times can result in further development of a fear of falling and decreased participation in activities of daily living.28 Thus, the development of programs to prevent falls is important for the overall health and well-being of wheeled mobility device users with MS. To our knowledge, there are currently no interventions focused on fall prevention in wheeled mobility device users with MS and few available for wheeled mobility device users in general.9 Dyer et al.29 examined the impact of an intervention program designed to decrease fall frequency in individuals after amputation of a lower-extremity limb. After implementation of the intervention, fall frequency decreased by 5%. In comparison, the intervention in the present study resulted in a 41.2% decrease in fall incidence.
Although a significant difference was found in fall frequency, the effect size was small (dz = 0.26). In addition, no significant difference and a small effect size were found regarding concerns about falling. As a result of the complex nature of falls and concerns about falling, it is likely that longer follow-up is necessary to fully assess the impact of the program on this important outcome. Making a significant change regarding the concerns that people feel about falling may require several months of a reduction in fall frequency for the individual to feel increased confidence.
There are several limitations associated with this study that require consideration. The small sample size (N = 16) may reduce the generalizability of the results to a larger group of individuals with MS who use a wheeled mobility device as their primary means of mobility. Another limitation is the limited follow-up period. Participants were evaluated 3 months after implementation of the intervention, thus limiting our ability to investigate the long-term impact of these findings. Future studies with longer follow-up are needed to examine the long-term impact of the intervention on fall frequency and concerns about falling. It is likely that changes in fall frequency and concerns about falling require more than 3 months to fully manifest. Finally, the home-based nature of the study limits our ability to determine whether participants were performing the exercises and reviewing the transfer materials, as instructed. Although follow-up telephone calls were made to participants every other week to inquire about their adherence to the program, participants may have misreported what actually occurred.
In conclusion, this preliminary feasibility study evaluated the impact of an intervention on fall frequency, concerns about falling, transfer skills, and seated postural control of wheeled mobility device users with MS. Preliminary results indicate that the educational intervention was well tolerated by participants and was found to be helpful. In addition, the preliminary assessment indicates that fall frequency decreased but concerns about falling did not. Transfer quality and seated postural control significantly improved.
Although the findings of the study are preliminary, such results are noteworthy because this seems to be the first research study to examine methods to manage fall frequency in wheeled mobility device users with MS. The improvements found in transfer quality and seated postural control may have an added benefit of improving functional mobility and community participation. Use of such an intervention may be of benefit to wheeled mobility device users with MS and has the potential to be used in a clinical setting by occupational and physical therapists. Further investigation is needed to examine the long-term impact of the intervention on concerns about falling and other MS-related symptoms.
PRACTICE POINTS
Falls are common in wheeled mobility device users with MS; however, few peer-reviewed intervention programs are available that are designed to decrease fall risk and enhance functional mobility.
The preliminary investigation of a home-based intervention program designed to reduce fall frequency was found to be feasible to perform, was well received by study participants, and resulted in a significant reduction in fall frequency.
Supplementary Material
Financial Disclosures:
The authors have no conflicts of interest to disclose.
Funding/Support:
This study was funded by the National Multiple Sclerosis Society Pilot Project (grant PP2185). NARCOMS is supported in part by the Consortium of Multiple Sclerosis Centers (CMSC) and the Foundation of the CMSC.
Prior Presentation:
Aspects of this study have been presented in abstract form at the 33rd International Seating Symposium; March 2–4, 2017; Nashville, TN.
References
- 1. Cameron MH, Poel AJ, Haselkorn JK, Linke A, Bourdette D.. Falls requiring medical attention among veterans with multiple sclerosis: a cohort study. J Rehabil Res Dev. 2011; 48: 13– 20. [DOI] [PubMed] [Google Scholar]
- 2. Finlayson ML, Peterson EW.. Falls, aging, and disability. Phys Med Rehabil Clin N Am. 2010; 21: 357– 373. [DOI] [PubMed] [Google Scholar]
- 3. Matsuda PN, Shumway-Cook A, Ciol MA, Bombardier CH, Kartin DA.. Understanding falls in multiple sclerosis: association of mobility status, concerns about falling, and accumulated impairments. Phys Ther. 2012; 92: 407– 415. [DOI] [PubMed] [Google Scholar]
- 4. Peterson EW, Cho CC, Finlayson ML.. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler. 2007; 13: 1168– 1175. [DOI] [PubMed] [Google Scholar]
- 5. Sosnoff JJ, Finlayson M, McAuley E, Morrison S, Motl RW.. Home-based exercise program and fall-risk reduction in older adults with multiple sclerosis: phase 1 randomized controlled trial. Clin Rehabil. 2014; 28: 254– 263. [DOI] [PubMed] [Google Scholar]
- 6. Cattaneo D, Jonsdottir J, Zocchi M, Regola A.. Effects of balance exercises on people with multiple sclerosis: a pilot study. Clin Rehabil. 2007; 21: 771– 781. [DOI] [PubMed] [Google Scholar]
- 7. Einarsson U, Gottberg K, Fredrikson S, Bergendal G, von Koch L, Holmqvist LW.. Multiple sclerosis in Stockholm County: a pilot study exploring the feasibility of assessment of impairment, disability and handicap by home visits. Clin Rehabil. 2003; 17: 294– 303. [DOI] [PubMed] [Google Scholar]
- 8. Coote S, Hogan N, Franklin S.. Falls in people with multiple sclerosis who use a walking aid: prevalence, factors, and effect of strength and balance interventions. Arch Phys Med Rehabil. 2013; 94: 616– 621. [DOI] [PubMed] [Google Scholar]
- 9. Rice LA, Ousley C, Sosnoff JJ.. A systematic review of risk factors associated with accidental falls, outcome measures and interventions to manage fall risk in non-ambulatory adults. Disabil Rehabil. 2015; 37: 1697– 1705. [DOI] [PubMed] [Google Scholar]
- 10. Learmonth YC, Motl RW, Sandroff BM, Pula JH, Cadavid D.. Validation of patient determined disease steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurol. 2013; 13: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thabane L, Ma J, Chu R, . et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010; 10: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Al-Faisal W, Beattie L, Fu H, . et al. WHO Global Report on Falls Prevention in Older Age. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 13. Boswell-Ruys CL, Harvey LA, Delbaere K, Lord SR.. A Falls Concern Scale for people with spinal cord injury (SCI-FCS). Spinal Cord. 2010; 48: 704– 709. [DOI] [PubMed] [Google Scholar]
- 14. Tsai CY, Rice LA, Hoelmer C, Boninger ML, Koontz AM.. Basic psychometric properties of the transfer assessment instrument (version 3.0). Arch Phys Med Rehabil. 2013; 94: 2456– 2464. [DOI] [PubMed] [Google Scholar]
- 15. McClure LA, Boninger ML, Ozawa H, Koontz A.. Reliability and validity analysis of the transfer assessment instrument. Arch Phys Med Rehabil. 2011; 92: 499– 508. [DOI] [PubMed] [Google Scholar]
- 16. Shin S, Sosnoff JJ.. Spinal cord injury and time to instability in seated posture. Arch Phys Med Rehabil. 2013; 94: 1615– 1620. [DOI] [PubMed] [Google Scholar]
- 17. Slobounov S, Cao C, Jaiswal N, Newell KM.. Neural basis of postural instability identified by VTC and EEG. Exp Brain Res. 2009; 199: 1– 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cattaneo D, Ferrarin M, Jonsdottir J, Montesano A, Bove M.. The virtual time to contact in the evaluation of balance disorders and prediction of falls in people with multiple sclerosis. Disabil Rehabil. 2012; 34: 470– 477. [DOI] [PubMed] [Google Scholar]
- 19. Chen WY, Jang Y, Wang JD, . et al. Wheelchair-related accidents: relationship with wheelchair-using behavior in active community wheelchair users. Arch Phys Med Rehabil. 2011; 92: 892– 898. [DOI] [PubMed] [Google Scholar]
- 20. Gagnon D, Koontz A, Mulroy S, . et al. Biomechanics of sitting pivot transfers among individuals with spinal cord injury: a review of the current knowledge. Top Spinal Cord Inj Rehabil. 2009; 15: 33– 58. [Google Scholar]
- 21. Kisner C, Colby L.. Therapeutic Exercise: Foundations and Techniques. 4th ed Philadelphia, PA: FA Davis; 2002. [Google Scholar]
- 22. Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013; 4: 863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gorman SL, Radtka S, Melnick ME, Abrams GM, Byl NN.. Development and validation of the Function In Sitting Test in adults with acute stroke. J Neurol Phys Ther. 2010; 34: 150– 160. [DOI] [PubMed] [Google Scholar]
- 24. Sung JH, Ousley C, Shen S, Issacs Z, Sosnoff J, Rice LA.. Reliability and validity of the function in sitting test in non-ambulatory individuals with multiple sclerosis. Int J Rehabil Res. 2016; 39: 308– 312. [DOI] [PubMed] [Google Scholar]
- 25. Rice LA, Smith I, Kelleher AR, Greenwald K, Hoelmer C, Boninger ML.. Impact of the clinical practice guideline for preservation of upper limb function on transfer skills of persons with acute spinal cord injury. Arch Phys Med Rehabil. 2013; 94: 1230– 1246. [DOI] [PubMed] [Google Scholar]
- 26. Sosnoff JJ, Moon Y, Wajda DA, . et al. Fall risk and incidence reduction in high risk individuals with multiple sclerosis: a pilot randomized control trial. Clin Rehabil. 2015; 29: 952– 960. [DOI] [PubMed] [Google Scholar]
- 27. Bisson EJ, Peterson EW, Finlayson M.. Delayed initial recovery and long lie after a fall among middle-aged and older people with multiple sclerosis. Arch Phys Med Rehabil. 2015; 96: 1499– 1505. [DOI] [PubMed] [Google Scholar]
- 28. Fleming J, Brayne C; Cambridge City over-75s Cohort (CC75C) study collaboration. . Inability to get up after falling, subsequent time on floor, and summoning help: prospective cohort study in people over 90. BMJ. 2008; 337: a2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dyer D, Bouman B, Davey M, Ismond KP.. An intervention program to reduce falls for adult in-patients following major lower limb amputation. Healthc Q. 2008; 11: 117– 121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


