Abstract
Background:
Positive psychology uses targeted activities to increase the frequency and intensity of positive emotional experiences. Positive psychology interventions that increase positive constructs may facilitate adjustment and improve well-being in patients with multiple sclerosis (MS). The primary goal of this study was to assess the feasibility and acceptability of a 5-week group positive psychology intervention for patients with MS. In addition, we examined the utility of the group intervention to increase positive psychological constructs and health-related quality of life (HRQOL).
Methods:
11 patients completed 5 weeks of group positive psychology training, one time per week (session duration, 45–60 minutes). Each week, patients completed one of the following positive psychology exercises: gratitude for positive events, personal strengths, gratitude letter, enjoyable and meaningful activities, and remembering past successes. Patients completed patient-reported outcome measures, including measures of positive affect, optimism, depression, anxiety, and HRQOL, at baseline and after 5 weeks.
Results:
All the participants completed the 5-week group positive psychology intervention, and 82% attended four or more sessions. Improvements in fatigue (vitality) and depression after the group intervention were significant (P = .016 and .049, respectively). There were no statistically significant changes in positive or negative affect, optimism, anxiety, HRQOL, or cognition.
Conclusions:
The 5-week group positive psychology intervention was feasible and acceptable to patients with MS. A randomized controlled trial is necessary to further explore the effectiveness of the group intervention.
Living with multiple sclerosis (MS), a chronic disease with an unpredictable and variable course, presents a major challenge for many patients. Depression and anxiety are common, occurring in up to 50%1–3 and 35%4 of patients with MS, respectively, and health-related quality of life (HRQOL) is often reduced.5–8 Positive psychological constructs, such as positive affect, optimism, and subjective well-being, may play an important role in adaptation to chronic disease.9 In patients with MS, positive constructs have been shown to be negatively associated with depression and anxiety10–12 and positively associated with physical, social, and psychological adjustment.12,13 A psychosocial intervention aimed at increasing positive constructs may facilitate adjustment and improve HRQOL in patients with MS.
Positive psychology uses targeted activities to increase the frequency and intensity of positive emotional experiences.14 Targeted activities encompass several domains, including gratitude, using one's personal strengths in a deliberate manner, and altruism. Positive psychology interventions have been applied in individual, group, and self-help settings, and depressed as well as nondepressed individuals have had improvements in psychological and subjective well-being after positive psychology training.15,16 Although the benefits of positive psychology interventions for healthy individuals and those with depression and other negative emotional states have been demonstrated, there are very few trials of these interventions for medically ill patients. We previously developed an 8-week telephone-based positive psychology intervention for patients with acute cardiovascular disease.17 Patients in the intervention condition showed improved optimism at 8-week follow-up compared with baseline. They also demonstrated a greater reduction in depressive symptoms and anxiety and more improvement in HRQOL than active and attention controls.
In this pilot study, the primary goal was to assess the feasibility and acceptability of a 5-week group positive psychology intervention for patients with MS. The intervention was based on previous work in cardiovascular disease and was adapted for a group setting and patients with MS. In addition, we examined the utility of the group positive psychology intervention to increase positive psychological constructs and improve emotional functioning and HRQOL in MS.
Methods
Participants
Patients were recruited from the Comprehensive Longitudinal Investigation of Multiple Sclerosis at Brigham and Women's Hospital, Partners MS Center (CLIMB) (Boston, MA). CLIMB is an ongoing prospective observational cohort study that began enrolling patients in 2000.18 Patients were approached about study participation at the time of their annual CLIMB visit by their treating neurologist. Interested individuals met with a member of the study staff (K.L., A.L., F.S., or B.I.G.) to learn about the study in more detail. No form of alternative care was offered. This study was approved by the Partners Human Research Committee at Brigham and Women's Hospital.
Measures
Patients were administered the following measures at baseline and after completing the positive psychology intervention: the Positive and Negative Affect Scale,19 the Life Orientation Test–Revised,20 the 36-item Short Form Health Status Survey (SF-36),21 the Center for Epidemiologic Studies Depression Scale (CESD), the State-Trait Anxiety Inventory,22 and the Symbol Digit Modalities Test.23,24 The Positive and Negative Affect Scale comprises two mood scales measuring positive and negative affect. The Life Orientation Test–Revised is a measure of optimism and pessimism. The SF-36 is a widely used generic measure of HRQOL. It yields an 8-scale profile of functional health and physical and mental health summary scores. The CESD is a self-report measure of depression that focuses on the cognitive and affective components of depression. The State-Trait Anxiety Inventory includes two questionnaires designed to measure the current temporary condition of state anxiety and the long-standing quality of trait anxiety. The Symbol Digit Modalities Test measures working memory and speed of information processing by having patients substitute numbers for symbols as part of a set code.
Intervention
Patients completed 5 weeks of group positive psychology training, one time per week, with sessions lasting 45 to 60 minutes. The following five positive psychology exercises, previously described by Huffman et al.,9,17,25 were chosen based on their performance in previous studies: 1) Gratitude for positive events: Participants were asked to recall three positive events that occurred in the past week and to write about the events and how they made them feel. 2) Personal strengths: Participants completed a brief survey of personal strengths and selected a strength such as perseverance or humility and used it deliberately for 24 hours. They then wrote about how they used the strength and how they felt while using it. 3) Gratitude letter: Participants were asked to recall another individual's kind act that resulted in joy, relief, serenity, or other positive feelings. They then wrote a letter to the person describing feelings of gratitude associated with this event. Participants were told that the letter did not need to be sent, although they were free to mail it if they wished. 4) Enjoyable and meaningful activities: Participants were asked to intentionally complete three acts in a single day—a pleasurable act done alone, a pleasurable act done with others, and a meaningful or important act. 5) Remembering past successes: Participants were asked to focus on a time when they experienced success and to write about the event and the positive feelings and thoughts that they had during the event.
The positive psychology exercises and study participant manual were adapted for a group setting and patients with MS (A.C., J.H., and B.I.G.). The study participant manual included an introduction and separate chapters for each week's exercise. The positive psychology intervention facilitator was a licensed social worker (A.C.) with extensive clinical experience in MS. The facilitator ran three consecutive intervention groups. Each of the groups was attended by one of three baccalaureate-level research assistants (K.L., A.L., and F.S.). The research assistants acted as observers and met with the facilitator after each session to discuss and record detailed observations regarding participant engagement. During week 1, the facilitator introduced positive psychology as an approach that focuses on improving positive emotions through the practice of simple exercises that are designed to make people feel more hopeful, grateful, and happy. She described the first exercise, gratitude for positive events, and asked patients to use their manuals to write down three positive things that happened in the past week. Patients were then encouraged to share their experiences with the group. At the end of week 1, she introduced the following week's exercise and asked patients to complete it before the next session. All the subsequent sessions began with a group discussion of the previous week's exercise and concluded with an introduction of the next week's exercise. At the conclusion of each session, the facilitator and research assistant met to discuss and record their observations.
Statistical Methods
To characterize study participants, we compared the demographic characteristics of participants and patients who declined to participate using a two-sample t test for continuous outcomes and a χ2 test for dichotomous outcomes. For all the statistical tests, a two-sided α level of 0.05 was used. No correction for multiple comparisons was applied. The primary goal of this study was to assess the feasibility and acceptability of the group positive psychology intervention. We estimated the feasibility using the proportion of patients who completed the intervention, and we calculated a Clopper-Pearson exact binomial 95% CI. Completion of the intervention was defined as completing at least three of the five positive psychology intervention sessions. We assessed the effect of the intervention based on the within-patient change in each of the outcome measures using paired t tests.
Results
Fifty-eight patients were approached about participating, and 53 (91%; 95% CI, 81%–97%) expressed interest in the intervention. Eleven of the 58 patients approached (19%; 95% CI, 10%–31%) were enrolled in the study. The demographic and clinical characteristics of study participants and those who declined participation are provided in Table 1, and reasons for nonenrollment are summarized in Figure 1. Study participants were more likely to be female, older, and with longer disease duration. In addition, the participants were significantly less likely to be fully employed (P = .005). All the study participants completed the group intervention (100%; 95% CI, 72%–100%). Five of the 11 patients (45%; 95% CI, 17%–77%) attended all five sessions, four (36%) attended four sessions, and two (18%) attended three sessions.
Table 1.
Demographic characteristics of patients who participated and declined to participate in a 5-week group positive psychology intervention
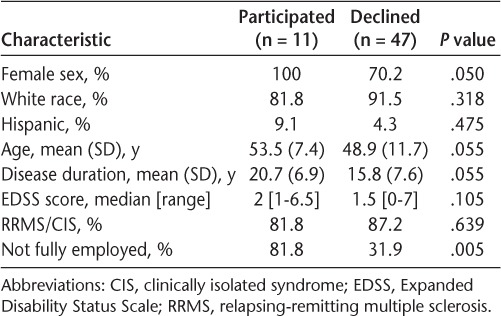
Figure 1.
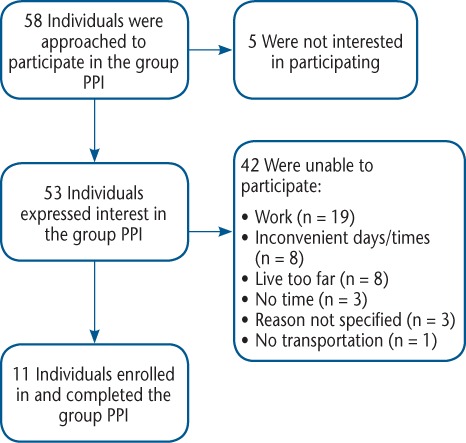
Flow diagram summarizing study approaches and enrollment
PPI, positive psychology intervention.
In terms of the impact of the group intervention on patient-reported outcome (PRO) measures, the summary statistics for each PRO are provided in Table 2 and Figure 2. We observed a significant increase in SF-36 vitality subscale score (P = .016) and a significant decrease in CESD score (P = .049). Changes in positive affect and SF-36 mental health subscale scores were in the right direction but did not reach statistical significance. There were no statistically significant changes in negative affect, optimism, anxiety, mental or physical HRQOL, or cognition.
Table 2.
Baseline, follow-up, and change in patient-reported outcome measures for a 5-week group positive psychology intervention
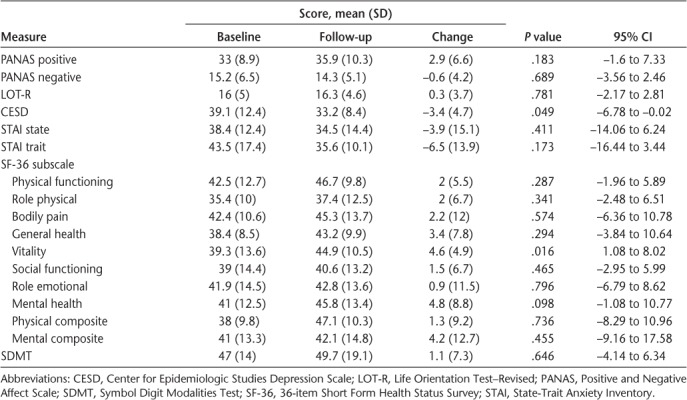
Figure 2.
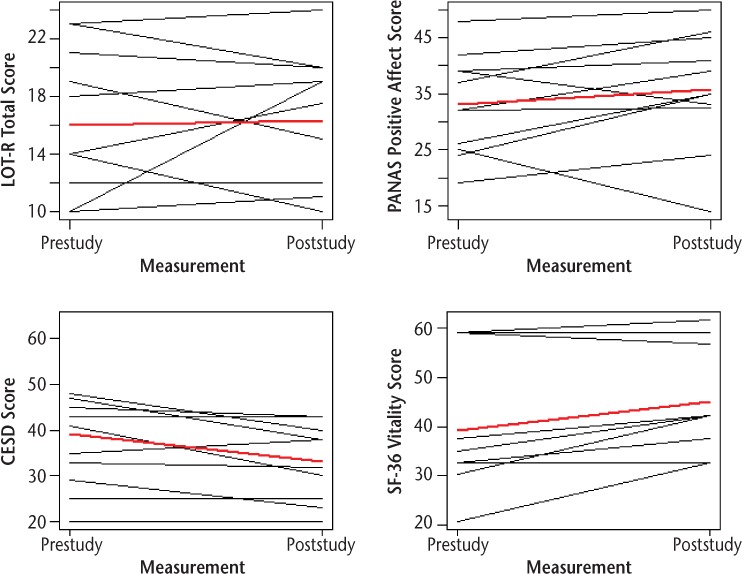
Changes in patient-reported outcome measures after a 5-week group positive psychology intervention
CES-D, Center for Epidemiologic Studies Depression Scale; LOT-R, Life Orientation Test–Revised; PANAS, Positive and Negative Affect Scale; SF-36, 36-item Short Form Health Status Survey.
Discussion
This study demonstrates that group positive psychology is a feasible and acceptable intervention with the potential to affect emotional function in patients with MS. All the participants completed the 5-week intervention, and 82% attended four or more sessions. The facilitator observed that participants were enthusiastic, invested, and eager to participate fully in the intervention. In addition, we observed decreased depression and fatigue after 5 weeks of positive psychology intervention compared with baseline. Although we expected to see improved positive affect based on earlier work with patients with acute cardiovascular disease,17 the increase in positive affect was not statistically significant.
When we compared patients who enrolled in the study and those who declined to participate, we found that study participants were more likely to be female and less likely to be employed full-time. We also identified several barriers that prevented more patients from participating in the intervention, including the group being held at an inconvenient time, living too far from the MS center, and relying on others for transportation. For patients who were employed, taking time off during the middle of the day was a barrier, and for others, the inability to commit to 5 consecutive weeks of participation was a factor. It is interesting to note that of the 58 patients we approached about participation, 53 expressed an interest in the intervention regardless of whether they were able to commit to participating in the study.
This preliminary study has several limitations. First, because the study did not include a control or comparison arm, it is unclear whether the PRO changes would have been observed in the absence of the intervention. It is possible that participation in the group process or engagement with the facilitator were related to the findings. Second, patients may have demonstrated improvement on self-rated measures to justify their participation in the study or to please the researchers.25 Third, all the participants were female, and it is unclear whether the group intervention would be similarly acceptable to male patients. The willingness of males with MS to participate in group psychosocial interventions should be assessed more closely to ensure that their needs are being addressed. Fourth, although all the participants completed the study, demonstrating the feasibility and acceptability of the intervention, there was a high decline-to-participate rate. This suggests that an intervention requiring weekly visits to an MS center may not be feasible for a large segment of the MS population. Alternative approaches to delivering the intervention should be considered, including the development of a virtual group positive psychology intervention that uses web conferencing and would allow patients to participate from home. Finally, given the small sample size, the study was not powered to detect statistically significant changes in several of the PRO measures. A follow-up study with larger numbers of participants and a control arm is required to estimate the impact of this intervention.
In summary, we found that a 5-week group positive psychology intervention adapted for an MS population was feasible and acceptable. At the completion of the intervention, patients with MS demonstrated reduced depression and fatigue. The group positive psychology intervention we describe could represent a low-cost, innovative, and effective tool to decrease depression and fatigue and improve HRQOL in individuals with MS. A follow-up randomized controlled trial is necessary to further explore the effectiveness of the intervention. In addition, the development of a virtual group positive psychology intervention that uses web conferencing software might make the intervention accessible to larger numbers of patients with MS.
PRACTICE POINTS
Psychosocial interventions are needed to address the emotional and psychosocial consequences of living with MS.
We examined the feasibility and utility of a 5-week group positive psychology intervention to increase positive psychological constructs, emotional function, and health-related quality of life.
The group positive psychology intervention was feasible and acceptable to patients with MS and was associated with decreased depression and fatigue.
Financial Disclosures:
Dr. Healy has served as a consultant for Biogen Idec and receives research support from Merck-Serono, Novartis, Genzyme, and Verily Life Sciences. Dr. Chitnis has received personal compensation for advisory board/consulting from Novartis, Bayer, and Biogen and receives financial support for research activities from Merck-Serono, Novartis, and Verily Life Sciences. Dr. Weiner has served as a consultant for Genentech and Tiziana Life Sciences and has received research support from EMD Serono, Miragen Therapeutics, Sanofi, Teva Pharmaceuticals, and Verily Life Sciences. Dr. Huffman's time for scientific input and editing was supported by grants R01HL113272 and R21DK109313 to him from the National Institutes of Health. Dr. Glanz has received research support from Merck-Serono and Verily Life Sciences. Mss. Leclaire, Cecil, LaRussa, and Stuart and Dr. Hemond have no conflicts of interest to disclose.
Funding/Support:
This study was supported by departmental funds (Ann Romney Center for Neurological Diseases at Brigham and Women's Hospital).
Prior Presentation:
Aspects of this study were presented in abstract form at the Consortium of Multiple Sclerosis Center's annual meeting, June 1–4, 2016, National Harbor, MD.
References
- 1. Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T.. The burden of mental comorbidity in multiple sclerosis: frequent, underdiagnosed, and undertreated. Mult Scler. 2009; 15: 385– 392. [DOI] [PubMed] [Google Scholar]
- 2. Sadovnick AD, Remick RA, Allen J, . et al. Depression and multiple sclerosis. Neurology. 1996; 46: 628– 632. [DOI] [PubMed] [Google Scholar]
- 3. Minden SL, Orav J, Reich P.. Depression in multiple sclerosis. Gen Hosp Psychiatry. 1987; 9: 426– 434. [DOI] [PubMed] [Google Scholar]
- 4. Korostil M, Feinstein A.. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007; 13: 67– 72. [DOI] [PubMed] [Google Scholar]
- 5. Olascoaga J. Quality of life and multiple sclerosis [in Spanish]. Rev Neurol. 2010; 51: 279– 288. [PubMed] [Google Scholar]
- 6. Vickrey BG, Hays RD, Harooni R, Myers LW, Ellison GW.. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995; 4: 187– 206. [DOI] [PubMed] [Google Scholar]
- 7. Benito-Leon J, Morales JM, Rivera-Navarro J, Mitchell A.. A review about the impact of multiple sclerosis on health-related quality of life. Disabil Rehabil. 2003; 25: 1291– 1303. [DOI] [PubMed] [Google Scholar]
- 8. Healy BC, Degano IR, Schreck A, . et al. The impact of a recent relapse on patient-reported outcomes in subjects with multiple sclerosis. Qual Life Res. 2012; 21: 1677– 1684. [DOI] [PubMed] [Google Scholar]
- 9. Huffman JC, Millstein RA, Mastromauro CA, . et al. A positive psychology intervention for patients with an acute coronary syndrome: treatment development and proof-of-concept trial. J Happiness Stud. 2016; 17: 1985– 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fournier M, De Ridder D, Bensing J.. Optimism and adaptation to chronic disease: the role of optimism in relation to self-care options of type 1 diabetes mellitus, rheumatoid arthritis and multiple sclerosis. Br J Health Psychol. 2002; 7 pt 4: 409– 432. [DOI] [PubMed] [Google Scholar]
- 11. Fournier M, de Ridder D, Bensing J.. Optimism and adaptation to multiple sclerosis: what does optimism mean? J Behav Med. 1999; 22: 303– 326. [DOI] [PubMed] [Google Scholar]
- 12. Dennison L, Moss-Morris R, Chalder T.. A review of psychological correlates of adjustment in patients with multiple sclerosis. Clin Psychol Rev. 2009; 29: 141– 153. [DOI] [PubMed] [Google Scholar]
- 13. de Ridder D, Schreurs K, Bensing J.. The relative benefits of being optimistic: optimism as a coping resource in multiple sclerosis and Parkinson's disease. Br J Health Psychol. 2000; 5: 141– 155. [Google Scholar]
- 14. Seligman ME, Steen TA, Park N, Peterson C.. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005; 60: 410– 421. [DOI] [PubMed] [Google Scholar]
- 15. Sin NL, Lyubomirsky S.. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009; 65: 467– 487. [DOI] [PubMed] [Google Scholar]
- 16. Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E.. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health. 2013; 13: 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Huffman JC, Mastromauro CA, Boehm JK, . et al. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart Int. 2011; 6: e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gauthier SA, Glanz BI, Mandel M, Weiner HL.. A model for the comprehensive investigation of a chronic autoimmune disease: the multiple sclerosis CLIMB study. Autoimmun Rev. 2006; 5: 532– 536. [DOI] [PubMed] [Google Scholar]
- 19. Watson D, Clark LA, Tellegen A.. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988; 54: 1063– 1070. [DOI] [PubMed] [Google Scholar]
- 20. Scheier MF, Carver CS, Bridges MW.. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994; 67: 1063– 1078. [DOI] [PubMed] [Google Scholar]
- 21. Ware JE Jr, Sherbourne CD.. The MOS 36-item short-form health survey (SF-36), I: conceptual framework and item selection. Med Care. 1992; 30: 473– 483. [PubMed] [Google Scholar]
- 22. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA.. Manual for the State-Trait Anxiety Inventory. Menlo Park, CA: Mind Garden; 1983. [Google Scholar]
- 23. Smith A. Symbol Digit Modalities Test: Manual. Los Angeles, CA: Western Psychological Services; 1982. [Google Scholar]
- 24. Rao SM. A Manual for the Brief Repeatable Battery of Neuropsychological Tests in Multiple Sclerosis. Milwaukee, WI: Medical College of Wisconsin; 1992. [Google Scholar]
- 25. Huffman JC, DuBois CM, Healy BC, . et al. Feasibility and utility of positive psychology exercises for suicidal inpatients. Gen Hosp Psychiatry. 2014; 36: 88– 94. [DOI] [PubMed] [Google Scholar]


