Abstract
Background
Patent foramen ovale (PFO) may contribute to nocturnal desaturation in patients with obstructive sleep apnea (OSA), and the effect of PFO closure in OSA is unknown. Our study tested the hypotheses that: (1) patients with severe OSA have a higher prevalence of PFO compared with healthy control subjects, (2) patients with severe OSA with clinically significant PFO experience more nocturnal desaturation than those without, and (3) PFO closure reduces nocturnal desaturation.
Methods
Patients with severe OSA and healthy control subjects underwent contrast transthoracic echocardiography and transcranial Doppler to detect PFO and determine shunt size. A subgroup of patients with OSA with large shunts underwent percutaneous PFO closure. Polysomnography was performed at baseline and 1, 6, and 12 months postclosure.
Results
One hundred patients with OSA (mean [SD] age, 52 [10] years; apnea-hypopnea index [AHI], 54 [18] events/h) and 50 control subjects (age, 52 [11] years; AHI, 2 [2] events/h) were studied. PFO prevalence was 43% in patients with OSA and 30% in control subjects (P = .16). Large shunts were detected in 18% of patients with OSA and 6% of control subjects (P = .049). Patients with OSA with clinically significant shunts had higher oxygen-desaturation index (ODI)/AHI ratios than patients without (ratio, 1.05 [0.27] vs 0.86 [0.26], P = .004). Six patients with OSA underwent PFO closure, which was not associated with a reduction in ODI (baseline, 48 [18]; 12 months, 51 [19] events/h; P = .92) or percentage of the night with arterial oxygen saturation < 90% (baseline, 23% [16%]; 12 months, 20% [22%]; P = .35).
Conclusions
Patients with severe OSA have a higher prevalence of PFO with large shunts compared with control subjects. The ODI/AHI ratio is increased in patients with OSA with clinically significant shunts. PFO closure does not reduce nocturnal desaturation.
Abbreviations
- AHI
apnea-hypopnea index
- ESS
Epworth Sleepiness Score
- HIT6
Headache Impact Test-6
- ODI
oxygen-desaturation index
- OSA
obstructive sleep apnea
- PFO
patent foramen ovale
- SaO2
arterial oxygen saturation
- SF-36v2
Short Form-36 General Health Survey, version 2
- TCD
transcranial Doppler
- TTE
transthoracic echocardiography
Patent foramen ovale (PFO) is a congenital cardiac defect present in approximately 25% of healthy adults. 1 Obstructive sleep apnea (OSA) is also a prevalent condition 2 associated with significant cardiovascular consequences,3, 4, 5 believed to be mediated via the intermittent hypoxia produced during apneas and hypopneas. The prevalence of PFO in patients with OSA is unknown; some reports suggest it is increased.6, 7 However, since these studies were undertaken, PFO detection techniques have advanced, and there is a need for new data.8, 9 In OSA, PFO may exacerbate the apnea-induced hypoxemia through right-to-left shunting, 10 therefore increasing the cardiovascular morbidity and mortality.
Clinical experience suggests that PFO can be safely closed percutaneously, 11 and where there is substantial right-to-left shunting, waking arterial oxygen tensions may be improved.12, 13, 14, 15, 16, 17 Data on the effect of PFO closure in OSA are limited to one case report, which documented a resolution of exercise-induced dyspnea. 18 An improvement in OSA following PFO closure could occur from a reduction in the frequency of respiratory events or from improvements in desaturation. An improvement in baseline hypoxemia could also stabilize ventilatory control, 19 analogous to periodic breathing resolution following descent from altitude.
We conducted a case-finding study of PFO in patients with severe OSA (referred to a sleep clinic) to test the hypothesis that patients with severe OSA have a higher prevalence of PFO compared with healthy control subjects and to determine the size of the associated shunt. In addition, the hypothesis that patients with severe OSA with clinically significant shunting through PFO experience greater nocturnal oxygen desaturation than those without PFO or clinically insignificant shunts was tested. Moreover, in a prospective proof-of-concept study the hypothesis that percutaneous PFO closure of large shunts in patients with severe OSA would reduce nocturnal desaturation was investigated.
Materials and Methods
Case-Finding Study
Subjects
Patients with severe OSA were recruited from the Royal Brompton Hospital sleep clinics. Patients with an apnea-hypopnea index (AHI) > 30 events/h, measured up to 24 months prior to enrollment, were eligible for the study. Healthy control subjects matched for age and sex were recruited from the local population by advertisement; inclusion criteria were an AHI < 5 events/h. Exclusion criteria (OSA and control subjects) were weight > 150 kg, FEV1/FVC < 70%, and FVC < 70% predicted. The study was approved by the Kings College Hospital Research Ethics Committee (Research Ethics Committee number 07/Q0703/33), and all subjects gave written informed consent.
Measurements
Baseline Assessments
Resting arterial blood gas tensions, spirometry, and a 6-min walk test were performed. Participants completed questionnaires to assess subjective sleepiness (Epworth Sleepiness Score [ESS]), 20 headache (Headache Impact Test-6 [HIT6] questionnaire), 21 and quality of life (Short Form-36 General Health Survey, version 2 [SF-36v2] questionnaire). 22
Overnight Respiratory Monitoring
Respiratory polygraphy was performed with measurements of nasal and oral airflow (nasal cannula and thermistor) and thoracic and abdominal respiratory effort (respiratory inductance plethysmography). Cardiac frequency, arterial oxygen saturation, snoring, and body position were also measured using standard clinical monitoring (SOMNOscreen; S-Med).
PFO Detection
Contrast transthoracic echocardiography (TTE) with second harmonic imaging was performed to determine the presence of PFO and size of the associated shunt.9, 23, 24 Measurements were performed at rest and following a Valsalva maneuver (e-Appendix 1). Obese patients with OSA have limited acoustic windows; therefore, contrast transcranial Doppler (TCD) was also performed as previously described25, 26, 27, 28 to help to quantify PFO shunt size. The Doppler measurements were performed at rest and following a Valsalva maneuver (e-Appendix 1).
Closure Study
Subjects
Patients with severe OSA with large shunts suitable for PFO closure were recruited from the case-finding study. Patients between 18 and 70 years of age with an AHI > 30 events/h and a large PFO suitable for closure were eligible to take part in this study. The multiple exclusion criteria are detailed in e-Appendix 1.
Measurements and Protocol
Polysomnography was performed using standard measurements (e-Appendix 1). Patients being treated with CPAP discontinued treatment for 3 nights prior to baseline polysomnography and restarted CPAP the evening following closure. Percutaneous PFO closure was performed by a single operator as previously described. 29 Defects were closed using a BioSTAR device (NMT Medical, Inc). Following the procedure, patients were discharged on aspirin 75 mg daily for 6 months and clopidogrel 75 mg daily for 90 days. Follow-up at 1, 6, and 12 months included polysomnography, TTE, and TCD.
Analysis
Overnight Respiratory and Nocturnal Polysomnography Studies
Apnea and hypopnea were defined as a 10-s cessation or > 50% reduction of baseline airflow, respectively. For polysomnography studies, additional hypopnea criteria were ≥ 4% oxygen desaturation or EEG arousal. Oxygen desaturation index (ODI) was defined as the average number of arterial oxygen saturation (SaO 2) dips ≥ 4%/h. The percentage of the night with SaO 2 < 90% was also calculated, along with the ODI/AHI ratio as a marker of the amount of desaturation for a given respiratory disturbance. Sleep was scored according to published guidelines. 30
Grade of PFO
A PFO was defined as present if a shunt of any magnitude was detected following a Valsalva maneuver. PFO shunt size was graded as small, moderate, or large in accordance with published criteria.8, 28, 31 Using TTE, the shunt magnitude was graded on the bubbles entering the left side of the heart after contrast injection; no shunt: no bubbles; small shunt: scattered individual bubbles; moderate shunt: obvious bubbles but not sufficient to completely opacify any section; large shunt: a shunt of contrast that completely opacified a section or all of the left side of the heart.
Using TCD, the shunt magnitude was graded on the number of microbubbles detected in the middle cerebral artery up to 1 min following contrast injection: no shunt: up to three bubbles over the minute; small shunt: four to 30 bubbles; moderate shunt: 31 to 100 bubbles; large shunt: bubbles filling the spectrum for more than three heartbeats. The size of shunt assigned to each PFO was the maximum shunt detected following Valsalva maneuver. Clinically significant PFO was defined as those with moderate to large shunts following Valsalva maneuver. If there was a disagreement between TTE and TCD, the largest detected shunt was recorded. Studies were scored blinded to subject group.
Statistical Analysis
Sample Size Calculations
The prevalence of PFO in OSA has previously been reported as 69% and 27% and in healthy control subjects as 17% and 15%.6, 7 Although these values were obtained using older technology, combining them produced a mean PFO prevalence of 48% in OSA vs 16% in control subjects. Assuming a more conservative estimate of PFO in OSA (45%) and a higher prevalence in the control subjects (20%) in a ratio of 2:1, a sample of 96 patients with OSA and 48 healthy control subjects was required to achieve 80% power at a significance level of 0.05 (STATA version 10.1; StataCorp LP). These numbers were rounded to 100 and 50, respectively; a ratio of 2:1 allowed us to enlarge the pool of potential patients for the PFO closure study.
Statistical analysis was performed using SPSS (version 16.0; IBM). Data are presented as mean (SD) or median (range). Categorical variables were compared using the χ2 test. Student t test was used to compare measurements in patients with OSA vs healthy control subjects. Patients with OSA were divided into two groups—no PFO or a small shunt vs those with a moderate to large clinically significant shunt—and compared using the Student t test or Mann-Whitney U test. The effects of PFO closure were compared over time using one-way analysis of variance on repeated measures (parametric) or the Kruskal-Wallis test (nonparametric); P < .05 was considered statistically significant.
Results
Case-Finding Study
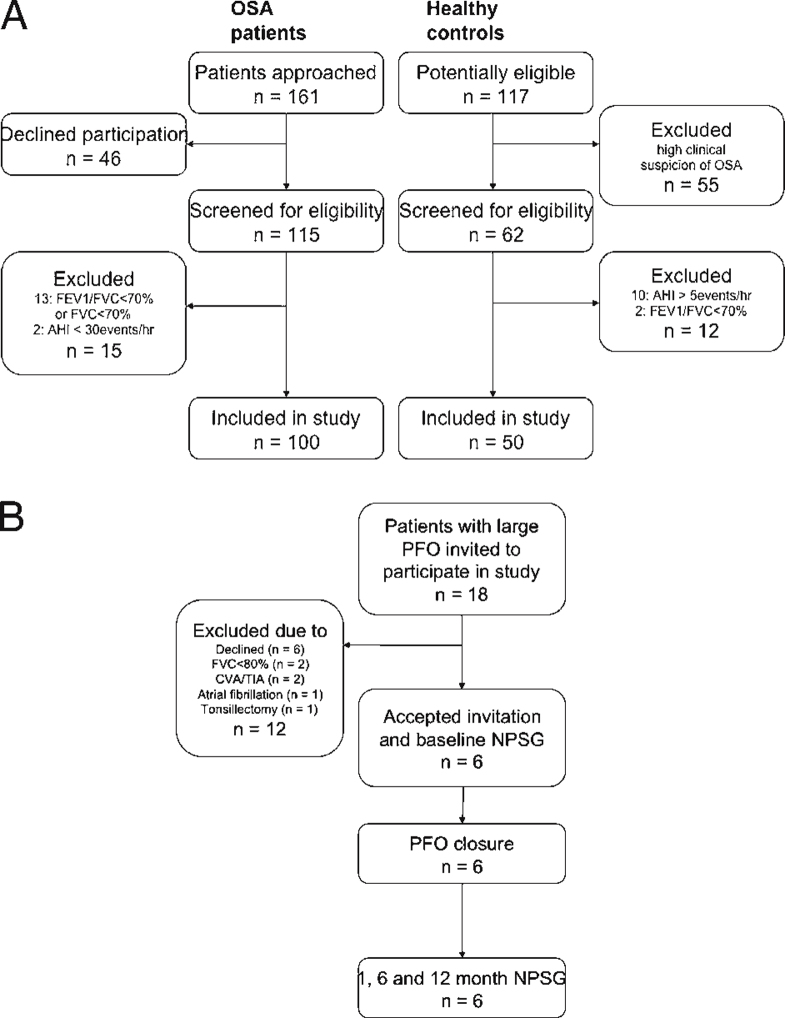
One hundred patients with severe OSA and 50 healthy control subjects were included in the study (Fig 1A). Baseline characteristics for both groups are given in Table 1, and details of comorbidities are given in Table 2. There were no significant differences in age, sex, and FEV1/FVC ratio between the patients with OSA and healthy control subjects. Patients with OSA had higher BMI, lower predicted FEV1 and FVC, lower PaO 2 and PaCO 2, higher ESS and HIT6 scores, and lower SF-36v2 quality-of-life scores. Eighty-six of the patients with OSA were using CPAP (median [range] duration of usage, 2.5 [0.25-24] months).
Figure 1.
A, Diagram illustrating recruitment of patients with severe OSA and healthy control subjects in the case-finding study. B, Diagram illustrating recruitment of patients with severe OSA in the closure study. AHI = apnea-hypopnea index; CVA = cerebrovascular accident; NPSG = nocturnal polysomnography; OSA = obstructive sleep apnea; PFO = patent foramen ovale; TIA = transient ischemic attack.
Table 1.
Baseline Characteristics
| Characteristic | Patients With OSA (n = 100) | Healthy Control Subjects (n = 50) | P Value |
|---|---|---|---|
| Age, y | 52 (10) | 52 (11) | .83 |
| Male (female) | 87 (13) | 42 (8) | .41 |
| BMI, kg/m2 | 34.5 (6.4) | 24.3 (2.7) | < .001 |
| FEV1, % predicted | 93 (2) | 101 (13) | < .001 |
| FVC, % predicted | 94 (11) | 104 (13) | < .001 |
| FEV1/FVC | 80 (5) | 79 (6) | .22 |
| PaO 2, kPa | 11.6 (1.3) | 12.3 (1.4) | .004 |
| PaCO 2, kPa | 5.3 (0.5) | 5.6 (0.5) | .01 |
| Epworth Sleepiness Score | 9 (5) | 5 (4) | < .001 |
| HIT6 headache score | 45 (9) | 42 (7) | .02 |
| SF-36v2: physical component | 47 (11) | 57 (5) | < .001 |
| SF-36v2: mental component | 48 (10) | 53 (8) | < .001 |
| AHI, events/h | 53.9 (17.8) | 2.0 (1.9) | … |
| ODI, events/h | 49.5 (21.0) | 1.9 (1.8) | … |
Values are expressed as mean (SD) except as otherwise noted. AHI = apnea-hypopnea index; HIT6 = Headache Impact Test-6; ODI = oxygen-desaturation index; OSA = obstructive sleep apnea; SF-36v2 = Short Form-36 General Health Survey version 2.
Table 2.
Comorbidities of Patients With OSA and Healthy Control Subjects
| Comorbidity | OSA, No. | Healthy Control Subjects, No. |
|---|---|---|
| No comorbidity | 21 | 45 |
| Ischemic heart disease | 11 | … |
| Hypertension | 43 | 3 |
| Atrial fibrillation/flutter | 4 | … |
| Hypercholesterolemia | 12 | … |
| Previous stroke/transient ischemic attack | 3 | … |
| Diabetes (type 1 and II) | 16 | 2 |
| Migraine | 5 | … |
| Cluster headache | 1 | … |
| Normal spirometry with previous diagnosis of mild airflow obstruction | 4 | … |
| Gastroenterologica | 10 | … |
| Musculoskeletalb | 14 | 2 |
| Otherc | 19 | … |
See Table 1 legend for expansion of abbreviation.
Gastroenterologic: irritable bowel syndrome (n = 2), inflammatory bowel disease (n = 1), gastroesophageal reflux disease (n = 5), diverticular disease (n = 1), hepatitis C (n = 1).
Musculoskeletal: osteoarthritis (n = 10), gout (n = 2), rheumatoid arthritis (n = 1), systemic lupus erythematosus (n = 1).
Other: myalgic encephalomyelitis (n = 1); schizoaffective disorder (n = 1); depression (n = 2); previous ear, nose, and throat surgery (n = 2); prostate conditions (n = 3); undiagnosed menorrhagia (n = 1); renal stones (n = 1); ocular hypertension (n = 1); ophthalmic artery occlusion (n = 1); pituitary adenoma (n = 1); hypothyroidism (n = 1); alcohol excess (n = 1); psoriasis (n = 1); acoustic neuroma (n = 1); vitiligo (n = 1).
PFO Prevalence
The prevalence of PFO was not significantly different in patients with severe OSA compared with healthy control subjects (43% [43 of 100] vs 30% [15 of 50], P = .16). Patients with OSA had a higher prevalence of large shunts following Valsalva maneuver compared with healthy control subjects (18% [18 of 100] vs 6% [3 of 50], P = .049). Patients with OSA and healthy control subjects had a similar prevalence of small and moderate size shunts. Details of shunt size at rest and following Valsalva maneuvers are given in Table 3. Details of the 24 patients in whom TTE and TCD results conflicted are given in e-Appendix 1.
Table 3.
PFO Shunt Size in Patients With OSA and Healthy Control Subjects at Rest and Following Valsalva Maneuver
| Shunt Size | At Rest |
Following Valsalva Maneuver |
||||
|---|---|---|---|---|---|---|
| OSA (n = 100) | Control Subjects (n = 50) | P Value | OSA (n = 100) | Control Subjects (n = 50) | P Value | |
| No shunt | 79 | 44 | .26 | 57a | 35a | .16 |
| Small shunt | 11 | 4 | .77 | 17 | 8 | 1.00 |
| Moderate shunt | 10 | 1 | .10 | 8 | 4 | 1.00 |
| Large shunt | 0 | 1 | .33 | 18 | 3 | .049 |
See Table 1 legend for expansion of abbreviations.
These subjects had no detectable shunts at rest or following Valsalva maneuver and, therefore, did not have a PFO.
Patients With OSA With and Without Clinically Significant Shunts
Patients with OSA with clinically significant shunts had a lower AHI (P = .01) and a higher ODI/AHI ratio (P = .004) compared with those with no clinically significant shunt (Table 4). PaCO 2 was lower in the clinically significant shunt group, despite similar PaO 2. Age, BMI, spirometry, ODI, the percentage of the night with SaO 2 < 90%, 6-min walk test distance, ESS, and HIT6 headache score were similar across groups.
Table 4.
Comparison of Patients With OSA With and Without Clinically Significant Shunting Through PFO
| Characteristic | Clinically Significant Shunt (n = 26) | Clinically Insignificant or No Shunt (n = 74) | P Value |
|---|---|---|---|
| Age, y | 54 (9) | 51 (10) | .20 |
| BMI, kg/m2 | 34.2 (7.2) | 34.6 (6.1) | .77 |
| FEV1, % predicted | 92 (16) | 93 (11) | .67 |
| FVC, % predicted | 93 (13) | 94 (11) | .63 |
| FEV1/FVC | 81 (6) | 80 (5) | .65 |
| AHI, events/h | 46.8 (14.3) | 56.5 (18.3) | .01 |
| ODI, events/h | 48.6 (16.1) | 49.8 (22.5) | .78 |
| ODI/AHI | 1.05 (0.27) | 0.86 (0.26) | .004 |
| Percentage time SaO 2 < 90%a | 27 (25) | 26 (25) | .85 |
| 6MWT distance, m | 511 (138) | 564 (83) | .07 |
| PaO 2, kPa | 11.8 (1.4) | 11.6 (1.2) | .43 |
| PaCO 2, kPa | 5.1 (0.5) | 5.4 (0.5) | .02 |
| Epworth Sleepiness Score | 11 (6–15) | 7 (4–12) | .08 |
| HIT6 headache score | 48 (38–55) | 40 (36–50) | .09 |
| SF-36v2: physical component | 43 (13) | 48 (10) | .10 |
| SF-36v2: mental health component | 45 (12) | 50 (9) | .08 |
Values expressed as mean (SD) or median (range). 6MWT = 6-min walk test. See Table 1 legend for expansion of other abbreviations.
Values expressed for 23 of 26 patients with clinically significant shunt and 64 of 74 patients with clinically insignificant or no shunt.
Closure Study
Six of the 18 patients with OSA with a large shunt after Valsalva maneuver underwent percutaneous PFO closure (Fig 1B). Patient details are given in Table 5. At 12 months, three PFOs were sealed, one had minimal shunting, and two had residual large shunts after Valsalva maneuver. Four of the six patients were using CPAP prior to closure; these patients continued to use CPAP after closure, and nocturnal use was 5 (3.5-7) h per night.
Table 5.
Details of PFO Closure Procedure, Outcomes, and Complications
| Detail | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Age, y | 66 | 59 | 56 | 47 | 35 | 60 |
| Procedure time, min | 58 | 29 | 37 | 28 | 71 | 40 |
| Interatrial septal aneurysm present | No | No | No | No | No | No |
| Device size | 28 | 28 | 23 | 23 | 23 | 28 |
| Follow up shunt sizea | ||||||
| 1 mo | Large | Small | No shunt | Large | No shunt | Large |
| 6 mo | Large | Small | Small | Large | No shunt | Small |
| 12 mo | Large | No shunt | Small | Large | No shunt | No shunt |
| Procedure-related complicationsb | Nil reported | Nil reported | Nil reported | Nil reported | Nil reported | Left foot bruising, palpitations, blood in stools |
See Table 1 legend for expansion of abbreviations.
Shunt sizes are given for those detected following a Valsalva maneuver.
Patients 1 to 5 reported no procedure related complications. Patient 6 reported three issues within 1 mo of PFO closure: left foot bruising that resolved; intermittent self-limiting palpitations that resolved after 1 mo; and blood in stools, which was investigated by the general practitioner, no sinister cause found, and resolved.
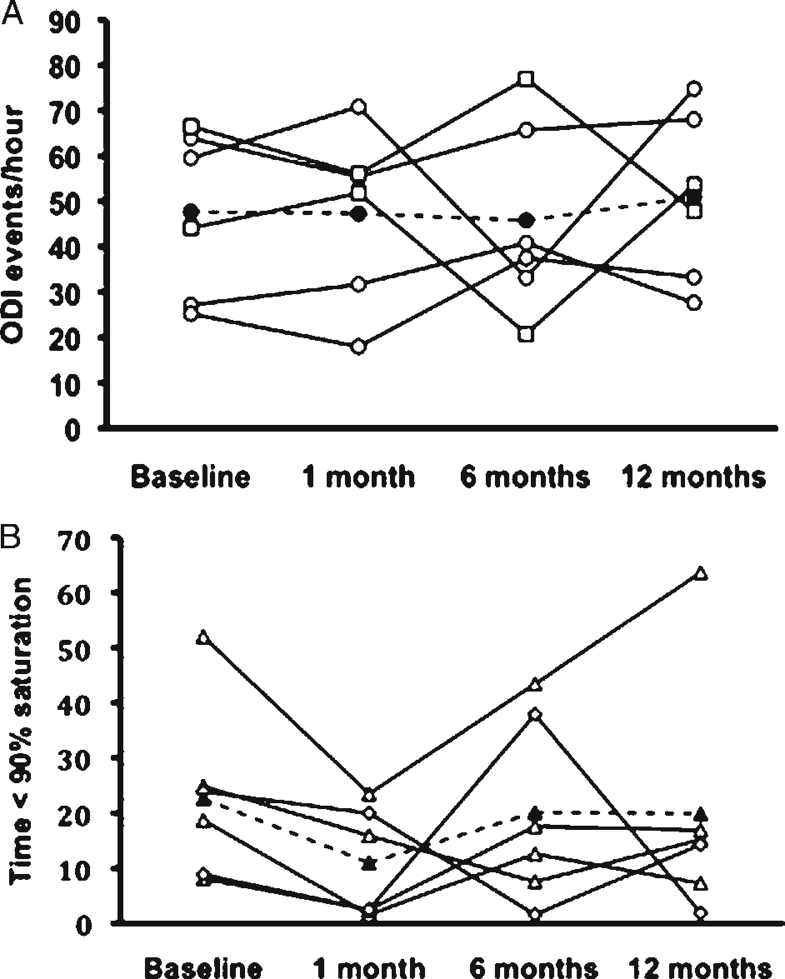
PFO closure was not associated with a significant change in ODI (Fig 2A) or time with SaO 2 < 90% (Fig 2B). Closure was not associated with any significant changes in PaO 2, PaCO 2, AHI, ODI/AHI ratio, BMI, 6-min walk test distance, ESS, HIT6 questionnaire, or SF-36v2 physical or mental health component. Values for each time period are given in Table 6.
Figure 2.
A, ODI at baseline and 1, 6, and 12 mo following PFO closure. ○ = individual values for patients with sealed PFO/small residual shunt; □ = individual values for patients with residual large shunts; • = mean value. B, The percentage of overnight time spent with arterial oxygen saturation < 90% was recorded at baseline and 1, 6, and 12 mo later. ▵ = individual values for patients with sealed PFO/small residual shunt; ◊ = individual value for patients with residual large shunts; ▴ = mean value. ODI = oxygen-desaturation index. See Figure 1 legend for expansion of other abbreviation.
Table 6.
Secondary Outcome Measures at Baseline and 1, 6, and 12 mo Following PFO Closure
| Measure | Baseline | 1 mo | 6 mo | 12 mo | P Value |
|---|---|---|---|---|---|
| PaO 2, kPa | 11.2 (0.7) | 11.8 (0.5) | 10.7 (0.7) | 10.8 (1.5) | .23 |
| PaCO 2, kPa | 5.6 (4.5–5.8) | 5.6 (5.0–5.8) | 5.6 (5.3–6.1) | 5.5 (4.7–6.1) | .74 |
| AHI, events/h | 67.2 (24.9) | 67.7 (21.9) | 66.6 (31.0) | 68.5 (31.0) | .99 |
| ODI/AHI | 0.73 (0.34–0.87) | 0.73 (0.53–0.87) | 0.70 (0.44–0.90) | 0.85 (0.40–1.01) | .28 |
| BMI, kg/m2 | 33.7 (3.5) | 32.8 (3.5) | 34.3 (3.2) | 33.2 (3.4) | .06 |
| 6MWT distance, m | 558 (102) | 578 (81) | 584 (69) | 593 (79) | .17 |
| Epworth Sleepiness Score | 13 (3) | 11 (4) | 10 (5) | 11 (5) | .14 |
| HIT6 | 42 (40–59) | 43 (36–46) | 37 (36–52) | 41 (38–65) | .28 |
| SF-36v2: physical component | 47 (9) | 48 (7) | 52 (7) | 46 (9) | .08 |
| SF-36v2: mental health component | 51 (5) | 52 (4) | 47 (8) | 49 (7) | .43 |
Discussion
The main findings of this study are that patients with severe OSA had a higher prevalence of large PFO shunts than healthy control subjects, although the significance was marginal. Overall PFO prevalence was not different from that in the general population. Patients with OSA with clinically significant shunts desaturated more for a given respiratory disturbance than those without clinically significant shunts. PFO closure did not reduce nocturnal desaturation, nor did it improve subjective sleepiness or quality of life.
Previous studies have identified different prevalences of PFO in patients with OSA than we found. Shanoudy et al 7 detected PFO in 69% of patients with OSA and in 17% of control subjects. The higher prevalence of PFO in this study may have occurred because the patients with OSA were recruited from those undergoing elective transesophageal echocardiography for other reasons and therefore may have been more likely to have a PFO. Beelke et al 6 detected PFO in 27% of patients with OSA and 15% of control subjects. In contrast, the lower prevalence of PFO in this study may be a consequence of using an older TCD machine without Power M Mode, which has been shown to improve PFO detection rates. 8 Also, the smaller shunts, common in control subjects, may have been missed. Both studies used saline and air contrast to detect PFO, which is not as effective as the saline, blood, and air mixture used in our study. 32
The patients with OSA with clinically significant shunts had higher ODI/AHI ratios than those without. Although the significance was marginal, the finding may support the suggestion that shunting through PFO in OSA exacerbates nocturnal desaturation. To our knowledge, Johansson et al 10 were the first to use the ODI/AHI ratio as an index of the amount of desaturation for a given level of respiratory disturbance. They found that in patients with OSA with a high ODI/AHI ratio (≥ 0.66), the PFO prevalence was 60%, vs 13% in patients with OSA with a low ratio. 10 Delivery of mixed venous blood to the systemic circulation through a large PFO could lead to a reduction in arterial oxygen saturation and an increase in the ODI/AHI ratio. However, in the present study, the increased nocturnal hypoxemia was not observed in other measures (SaO 2 < 90%), nor was it in the study of Johansson et al, 10 in which mean and minimum oxygen saturation were reported.
PFO Detection
We used contrast TTE and TCD to detect and size PFO. Both tests have good sensitivity and specificity and are comparable to contrast transesophageal echocardiography, the commonly regarded gold standard.9, 28 Obese patients with OSA have poor echo windows; therefore, combining echocardiography with TCD enabled us to accurately detect and estimate the size of each PFO shunt. 33
Mechanisms for the High Prevalence of Large PFO in OSA
The increased prevalence of large PFO may be explained by mechanisms that alter the anatomic configuration of the interatrial septum, ultimately stretching preexisting PFO and increasing the size of shunt. OSA can cause large elevations in pulmonary artery pressure (due to hypoxic pulmonary vasoconstriction),34, 35 increasing right ventricular afterload and promoting an increase in right atrial pressure. Combined with this increase, obstructive apneas generate negative intrathoracic pressures, which increases venous return and augments right ventricular preload. The increased venous return leads to further increases in right atrial pressure with resulting strain on the interatrial septum. Taken together, these effects are likely to promote right-to-left shunting; therefore, we speculate that this volume effect explains the physiologic association between PFO size during wakefulness and the ODI/AHI ratio during sleep. Termination of apneas is followed by a reflex hyperventilatory response. The inspiratory phase of this response increases venous return. In patients with persistent Eustachian valves or anatomy that streamlines inferior vena caval flow toward the atrial septum, this venous return is directed through a PFO. In combination with elevated right atrial pressure, we speculate that over time this may stretch a PFO.
PFO Closure
To our knowledge, this is the first prospective PFO closure study in patients with OSA. We found that although the procedure can be safely performed, it was also technically difficult, due to body habitus and the frequency of lipomatous hypertrophy of the secundum septum. PFO closure was not associated with a reduction in ODI or the percentage of the night spent with SaO 2 < 90%, even in patients who had complete closure, suggesting an alternative mechanism for desaturation in these patients. PFO closure cannot currently be recommended as a means of improving nocturnal oxygenation.
Critique of Methods
A number of factors need to be considered in the present study. Patients with severe OSA were studied; the PFO prevalence and associated nocturnal desaturation may be different in those with less severe disease. Six of 18 patients with OSA identified with large PFO underwent closure. This small sample size limits the ability to detect a significant change, although we have likely excluded a major effect in our sample.
The median duration from diagnosis of OSA to the study visit varied in the case-finding prevalence study (median time, 70; interquartile range, 28-160 days); therefore, the severity of OSA may have been overestimated or underestimated. However, there was no significant difference in the weight of the patients with OSA at the time of diagnosis compared with the time of study (mean [SD] weight at diagnosis, 104 [18.3] kg; at study, 105 [19.1] kg; P = .19), suggesting spontaneous disease progression/resolution did not occur in the 2- to 3-month median duration.
Conclusions
Patients with severe OSA have a slightly higher prevalence of PFO with large shunts than the general population but not a higher prevalence of PFO in total. This finding may represent a pathophysiological consequence of increased right-sided heart pressure, and although in these patients greater nocturnal desaturations were noted for a given respiratory disturbance, there was no benefit from PFO closure. Based on these data, PFO closure is not recommended for treating intermittent hypoxemia in OSA.
Supplementary Material
Acknowledgments
Author contributions: Drs Shaikh and Morrell are the guarantors of the manuscript and take responsibility for the integrity of the data and accuracy of the data analysis.
Dr Shaikh: contributed to conception and design, analysis and interpretation of data, drafting of the manuscript and revising, and final approval of the manuscript submitted.
Ms Jaye: contributed to study design, analysis of data, review of manuscript, and final approval of the manuscript submitted.
Dr Ward: contributed to conception and study design, interpretation of data, revising of the manuscript, and final approval of the manuscript submitted.
Dr Malhotra: contributed to conception and study design, interpretation of data, revising of the manuscript, and final approval of the manuscript submitted.
Mr de Villa: contributed to study design, analysis of data, review of manuscript, and final approval of the manuscript submitted.
Dr Polkey: contributed to conception and design, analysis and interpretation of data, drafting of the manuscript and revising, and final approval of the manuscript submitted.
Dr Mullen: contributed to conception and design, analysis and interpretation of data, drafting of the manuscript and revising, and final approval of the manuscript submitted.
Dr Morrell: contributed to conception and design, analysis and interpretation of data, drafting of the manuscript and revising, and final approval of the manuscript submitted.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Ms Jaye received a salary from ResMed and sits on a medical advisory board for a homecare company. Dr Malhotra has received consulting and/or research income from National Institutes of Health; American Heart Association; NMT Medical, Inc; Philips Respironics; Sleep Group Solution; Sleep Health Centers; Apnex Medical, Inc; ApniCure, Inc; Ethicon, Inc; Medtronic, Inc; Galleon Pharmaceuticals, Inc; Pfizer, Inc; Merck & Co, Inc; Sunovion Pharmaceuticals; and Cephalon, Inc. Since May 2012, Dr Malhotra has relinquished all outside personal income. Dr Mullen acts as a consultant and a proctor for Coherex Medical, Inc. Dr Morrell has received research grants from National Institutes of Health Research, British Heart Foundation, Wellcome Trust, and ResMed; none of these projects are related to the present study. This work was supported in part by the NIHR Respiratory Biomedical Research Unit at the Royal Brompton and Harefield NHS Foundation Trust and Imperial College, who partly fund Dr Polkey's salary. Drs Shaikh and Ward and Mr de Villa have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsor, NMT Medical Inc, provided insurance and indemnity.
Other contributions: We thank Anita Simonds, MD, for allowing recruitment of patients from her sleep clinic; the Echocardiography Department, in particular Caroline Flick, for the outstanding help with scanning subjects; the clinical sleep team for their assistance with recruitment; Michael Roughton, MSc, and Winston Banya, MSc, Medical Statistician Royal Brompton Hospital NHS Foundation Trust and Imperial College for their statistical assistance; and Angela Atalla, MBChB, and Dinesh Shrikrishna, MD, for their assistance during this project. The study was performed at Imperial College London, Royal Brompton Hospital campus.
Additional information: The e-Appendix can be found in the “Supplemental Materials” area of the online article.
Footnotes
Funding/Support: This study was supported by a grant from NMT Medical Inc.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59(1):17–20. doi: 10.1016/s0025-6196(12)60336-x. [DOI] [PubMed] [Google Scholar]
- 2.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 3.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–1384. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 4.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 5.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–2041. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 6.Beelke M, Angeli S, Del Sette M. Prevalence of patent foramen ovale in subjects with obstructive sleep apnea: a transcranial Doppler ultrasound study. Sleep Med. 2003;4(3):219–223. doi: 10.1016/s1389-9457(02)00256-3. [DOI] [PubMed] [Google Scholar]
- 7.Shanoudy H, Soliman A, Raggi P, Liu JW, Russell DC, Jarmukli NF. Prevalence of patent foramen ovale and its contribution to hypoxemia in patients with obstructive sleep apnea. Chest. 1998;113(1):91–96. doi: 10.1378/chest.113.1.91. [DOI] [PubMed] [Google Scholar]
- 8.Spencer MP, Moehring MA, Jesurum J, Gray WA, Olsen JV, Reisman M. Power m-mode transcranial Doppler for diagnosis of patent foramen ovale and assessing transcatheter closure. J Neuroimaging. 2004;14(4):342–349. doi: 10.1177/1051228404268743. [DOI] [PubMed] [Google Scholar]
- 9.Daniëls C, Weytjens C, Cosyns B. Second harmonic transthoracic echocardiography: the new reference screening method for the detection of patent foramen ovale. Eur J Echocardiogr. 2004;5(6):449–452. doi: 10.1016/j.euje.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Johansson MC, Eriksson P, Peker Y, Hedner J, Råstam L, Lindblad U. The influence of patent foramen ovale on oxygen desaturation in obstructive sleep apnoea. Eur Respir J. 2007;29(1):149–155. doi: 10.1183/09031936.00035906. [DOI] [PubMed] [Google Scholar]
- 11.Verma SK, Tobis JM. Explantation of patent foramen ovale closure devices: a multicenter survey. JACC Cardiovasc Interv. 2011;4(5):579–585. doi: 10.1016/j.jcin.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Allan JJ, Marinelli C, Dellsperger KC, Winniford MD. Percutaneous balloon catheter closure of a patent foramen ovale in a patient with pulmonary disease, profound hypoxemia, and normal right heart pressures. Clin Cardiol. 1997;20(3):307–309. doi: 10.1002/clc.4960200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuch B, Riehle M, von Scheidt W. Hypoxemia from right-to-left shunting through a patent foramen ovale in right ventricular infarction: treatment by revascularization, preload reduction, and, finally, interventional PFO closure. Clin Res Cardiol. 2006;95(12):680–684. doi: 10.1007/s00392-006-0442-3. [DOI] [PubMed] [Google Scholar]
- 14.Mottram PM, McGaw DJ, Meredith IT. Profound hypoxaemia corrected by PFO closure device in carcinoid heart disease. Eur J Echocardiogr. 2008;9(1):47–49. doi: 10.1016/j.euje.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Remy-Jardin M, Remy J, Wallaert B. Right-to-left shunting through a patent foramen ovale without pulmonary hypertension. Transient improvement after balloon catheter closure. Chest. 1990;97(5):1250–1252. doi: 10.1378/chest.97.5.1250. [DOI] [PubMed] [Google Scholar]
- 16.Shnaider H, Shiran A, Lorber A. Right ventricular diastolic dysfunction and patent foramen ovale causing profound cyanosis. Heart. 2004;90(6):e31. doi: 10.1136/hrt.2003.026468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piéchaud JF. Hypoxemia related to right-to-left shunting through a patent foramen ovale: successful percutaneous treatment with the CardioSeal device. J Interv Cardiol. 2001;14(1):57–60. doi: 10.1111/j.1540-8183.2001.tb00712.x. [DOI] [PubMed] [Google Scholar]
- 18.Agnoletti G, Iserin L, Lafont A, Sidi D, Desnos M. Obstructive sleep apnoea and patent foramen ovale: successful treatment of symptoms by percutaneous foramen ovale closure. J Interv Cardiol. 2005;18(5):393–395. doi: 10.1111/j.1540-8183.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- 19.Wellman A, Malhotra A, Fogel RB, Edwards JK, Schory K, White DP. Respiratory system loop gain in normal men and women measured with proportional-assist ventilation. J Appl Physiol. 2003;94(1):205–212. doi: 10.1152/japplphysiol.00585.2002. [DOI] [PubMed] [Google Scholar]
- 20.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 21.Kosinski M, Bayliss MS, Bjorner JB. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12(8):963–974. doi: 10.1023/a:1026119331193. [DOI] [PubMed] [Google Scholar]
- 22.Hawthorne G, Osborne RH, Taylor A, Sansoni J. The SF36 Version 2: critical analyses of population weights, scoring algorithms and population norms. Qual Life Res. 2007;16(4):661–673. doi: 10.1007/s11136-006-9154-4. [DOI] [PubMed] [Google Scholar]
- 23.Trevelyan J, Steeds RP. Comparison of transthoracic echocardiography with harmonic imaging with transoesophageal echocardiography for the diagnosis of patent foramen ovale. Postgrad Med J. 2006;82(971):613–614. doi: 10.1136/pgmj.2006.045021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Madala D, Zaroff JG, Hourigan L, Foster E. Harmonic imaging improves sensitivity at the expense of specificity in the detection of patent foramen ovale. Echocardiography. 2004;21(1):33–36. doi: 10.1111/j.0742-2822.2004.02168.x. [DOI] [PubMed] [Google Scholar]
- 25.Klötzsch C, Janssen G, Berlit P. Transesophageal echocardiography and contrast-TCD in the detection of a patent foramen ovale: experiences with 111 patients. Neurology. 1994;44(9):1603–1606. doi: 10.1212/wnl.44.9.1603. [DOI] [PubMed] [Google Scholar]
- 26.Karnik R, Stöllberger C, Valentin A, Winkler WB, Slany J. Detection of patent foramen ovale by transcranial contrast Doppler ultrasound. Am J Cardiol. 1992;69(5):560–562. doi: 10.1016/0002-9149(92)91006-p. [DOI] [PubMed] [Google Scholar]
- 27.Job FP, Ringelstein EB, Grafen Y. Comparison of transcranial contrast Doppler sonography and transesophageal contrast echocardiography for the detection of patent foramen ovale in young stroke patients. Am J Cardiol. 1994;74(4):381–384. doi: 10.1016/0002-9149(94)90407-3. [DOI] [PubMed] [Google Scholar]
- 28.Saqqur M, Dean N, Schebel M. Improved detection of microbubble signals using power M-mode Doppler. Stroke. 2004;35(1):e14–e17. doi: 10.1161/01.STR.0000106771.62928.66. [DOI] [PubMed] [Google Scholar]
- 29.Mullen MJ, Hildick-Smith D, De Giovanni JV. BioSTAR Evaluation STudy (BEST): a prospective, multicenter, phase I clinical trial to evaluate the feasibility, efficacy, and safety of the BioSTAR bioabsorbable septal repair implant for the closure of atrial-level shunts. Circulation. 2006;114(18):1962–1967. doi: 10.1161/CIRCULATIONAHA.106.664672. [DOI] [PubMed] [Google Scholar]
- 30.Iber C, Ancoli-Israel S, Chesson A. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. AASM Manual for Scoring Sleep; West Chester, IL: 2007. [Google Scholar]
- 31.Dowson A, Mullen MJ, Peatfield R. Migraine Intervention With STARFlex Technology (MIST) trial: a prospective, multicenter, double-blind, sham-controlled trial to evaluate the effectiveness of patent foramen ovale closure with STARFlex septal repair implant to resolve refractory migraine headache. Circulation. 2008;117(11):1397–1404. doi: 10.1161/CIRCULATIONAHA.107.727271. [DOI] [PubMed] [Google Scholar]
- 32.Sastry S, Daly K, Chengodu T, McCollum C. Is transcranial Doppler for the detection of venous-to-arterial circulation shunts reproducible? Cerebrovasc Dis. 2007;23(5–6):424–429. doi: 10.1159/000101466. [DOI] [PubMed] [Google Scholar]
- 33.Zito C, Dattilo G, Oreto G. Patent foramen ovale: comparison among diagnostic strategies in cryptogenic stroke and migraine. Echocardiography. 2009;26(5):495–503. doi: 10.1111/j.1540-8175.2008.00852.x. [DOI] [PubMed] [Google Scholar]
- 34.Tilkian AG, Guilleminault C, Schroeder JS, Lehrman KL, Simmons FB, Dement WC. Hemodynamics in sleep-induced apnea. Studies during wakefulness and sleep. Ann Intern Med. 1976;85(6):714–719. doi: 10.7326/0003-4819-85-6-714. [DOI] [PubMed] [Google Scholar]
- 35.Niijima M, Kimura H, Edo H. Manifestation of pulmonary hypertension during REM sleep in obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 1999;159(6):1766–1772. doi: 10.1164/ajrccm.159.6.9808064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.