Debilitating pain is the predominant symptom in chronic pancreatitis, especially alcoholic pancreatitis,1 possibly from obstructing stones that increase intraductal pressure.2 Pancreatic duct (PD) stones occur in up to 90% of patients with alcoholic chronic pancreatitis.3 Unlike common bile duct stones, extraction of PD stones is challenging. They are harder and spiculated, and passage of a guidewire or endoscope is difficult because of the angulation of the PD at the genu. ERCP with pancreatic sphincterotomy and balloon/basket extraction can extract up to 75% of stones <10 mm.4 For larger or lumen-occluding stones, extracorporeal shock wave lithotripsy (ESWL) has become first-line management.4 However, ESWL is not widely available, it may require multiple sessions, and ERCP is required to clear the PD of stone fragments. Newer technologies such as digital pancreatoscopy with electohydraulic lithotripsy (EHL) may be able to achieve stone clearance in a single session or fewer sessions. We describe such a case.
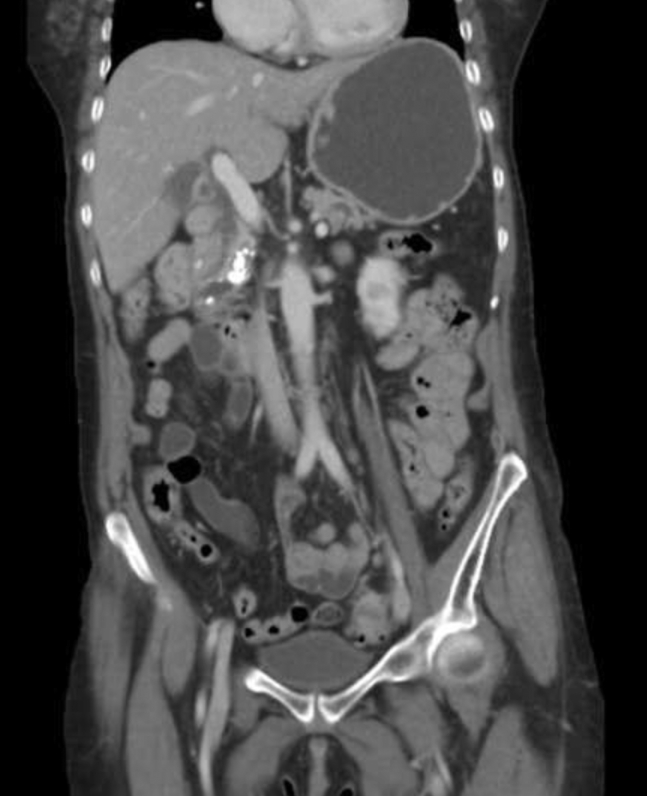
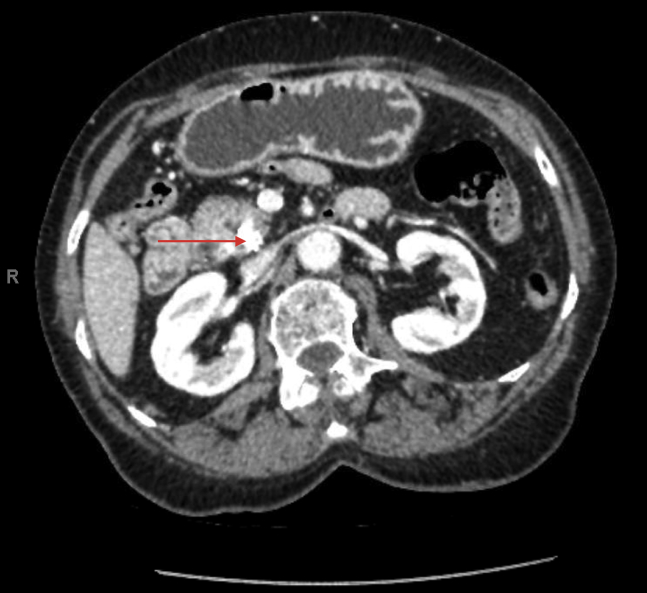
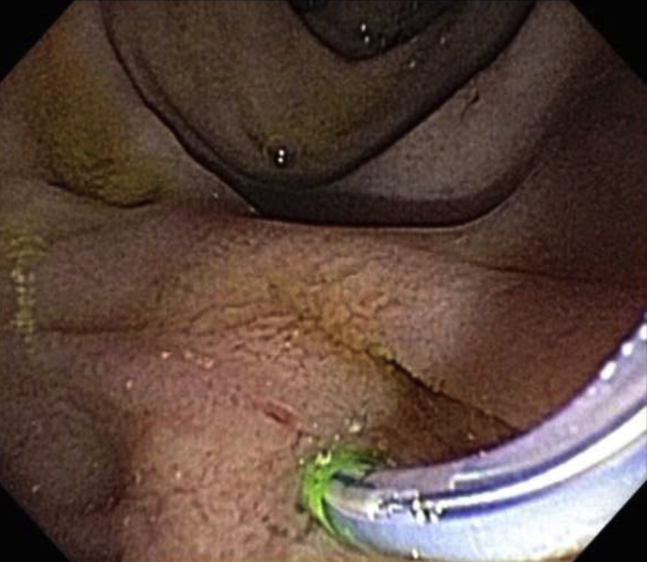
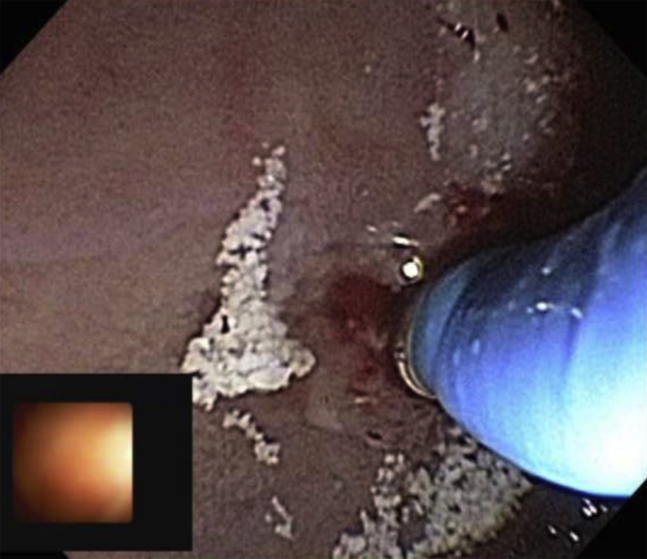
A 63-year-old woman with chronic alcoholic pancreatitis and recurrent acute pancreatitis was admitted for severe epigastric pain. Laboratory tests showed a lipase level of 1518 U/L and normal liver function test results. CA19-9 was 10.1 U/mL. CT showed new pancreatic calcifications (Fig. 1) and diffuse ductal dilatation to 11 mm (Fig. 2) with 2 stones measuring 11 mm in the head (Fig. 3) and uncinate process (Fig. 4). ERCP showed a tortuous PD with occluding stone in the head (Fig. 5). The digital cholangioscope catheter was advanced into the PD, and a large, impacted, spiculated stone was found proximal to the ampulla. Attempts at passing a guidewire were unsuccessful (Fig. 6). EHL was successfully performed through the cholangioscope catheter (Video 1, available online at www.VideoGIE.org). Stone fragments clogged the accessory channel of the catheter, preventing EHL of the second stone. Deep guidewire cannulation of the pancreatic duct was not possible because of the tortuous duct and difficult endoscope position. This also prevented balloon and basket sweeps and pancreatic duct stent placement. Stone fragments were seen spontaneously exiting the pancreatic orifice (Fig. 7). Pancreatic sphincterotomy was performed to allow stone fragments to exit freely, with a plan to repeat pancreatoscopy to clear the second stone.
Figure 1.
CT view showing stones in the pancreatic duct.
Figure 2.
Dilated pancreatic duct in the body and tail.
Figure 3.
Pancreatic duct stone in head of the pancreas.
Figure 4.
Pancreatic duct stone in uncinate process.
Figure 5.
ERCP performed in an attempt to remove the pancreatic ductal stones (ampulla shown).
Figure 6.
Resistance to guidewire advancement in head of pancreas.
Figure 7.
Stone fragments exiting the ampulla.
The patient was readmitted 3 weeks later with similar symptoms. US showed mild PD dilatation, with no pancreatic duct calcifications. Repeated ERCP with digital pancreatoscopy found no stone in the pancreatic head, but an occluding white spiculated stone in the uncinate process was treated with EHL. Once again, deep cannulation of a guidewire into the pancreatic duct was not possible because of duct tortuosity and difficult position of the endoscope; hence, balloon or basket sweep of the duct or PD stenting was not possible. Stone fragments were allowed to freely pass out of the ampulla through the large pancreatic sphincterotomy. The patient has been pain free since the procedure.
The role of ESWL followed by ERCP is well established for management of large (>10 mm) or impacted PD stones.3 Unfortunately, not many centers have ESWL capability. Also, patients may not be able to afford the often-needed multiple ESWL sessions. Unlike complex common bile duct stones, the role of pancreatoscopy with EHL is less studied for PD stones. Our experience demonstrates this to be a viable alternative to the ESWL followed by ERCP approach.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Video demonstrating use of digital pancreatoscopy with electrohydraulic lithrotripsy to treat 2 impacted pancreatic duct stones.
References
- 1.Andren-Sandberg A., Hoem D., Gislason H. Pain management in chronic pancreatitis. Eur J Gastro Hepatol. 2002;14:957–970. doi: 10.1097/00042737-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Choi E.K., Lehman G.A. Update on endoscopic management of main pancreatic duct stones in chronic calcific pancreatitis. Korean J Intern Med. 2012;27:20–29. doi: 10.3904/kjim.2012.27.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ammann R.W., Akovbiantz A., Largiader F. Course and outcome of chronic pancreatitis: longitudinal study of a mixed medical-surgical series of 245 patients. Gastroenterology. 1984;86:820–828. [PubMed] [Google Scholar]
- 4.Thomas M., Howell D., Carr-Locke D. Mechanical lithotripsy of pancreatic and biliary stones: complications and available treatment options collected from expert centers. Am J Gastroenterol. 2007;102:1896–1902. doi: 10.1111/j.1572-0241.2007.01350.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video demonstrating use of digital pancreatoscopy with electrohydraulic lithrotripsy to treat 2 impacted pancreatic duct stones.