Abstract
Israel is known as a pronatalist country. Whether due to the Biblical commandment to ‘be fruitful and multiply’ or the traumas of the Holocaust and perennial wars, reproduction is a central life goal for most Israelis. Israeli women bear substantially more children than their counterparts in industrialized countries and view child-rearing as a key life accomplishment. These personal world-view and real-life individual quests take place in a context of equally pronatalist state policies and religious openness to assisted reproductive technologies. In this paper, I outline 35 years of assisted reproductive technologies in Israel by tracing a principal axis in the development of three major technologies of assisted reproduction: the proliferation of IVF-ICSI; the globalization of gamete donation; and the privatization of surrogacy. The paper is based on a policy analysis as well as various studies of assisted reproductive technologies, conducted in Israel over this period.
Keywords: Israel, IVF, privatization, reproductive technologies, surrogacy, third-party reproduction
Introduction
Israel is well known as a pronatalist country. Whether due to the Biblical commandment to ‘be fruitful and multiply’ or the traumas of the Holocaust and perennial wars, reproduction has been a central goal in Israel, some would say a preoccupation, since its foundation. Indeed, Israeli women bear substantially more children than their counterparts in industrialized countries (3.03 versus, for example, 2.01 and 1.56 in the USA and Western Europe, respectively; CIA factbook, 2015a and Eurostat, 2015, respectively) and tend to view child rearing as ‘life’s greatest joy’ (Glickman, 2003). By the same token, barrenness often represents the quintessential female suffering, and voluntary childlessness is strongly condemned (Donath, 2014, Donath, 2015). Jewish religious authorities are equally pronatalist and gladly accommodate assisted reproductive technologies. Doctors, for their part, seek to serve the multiparous religious communities and thus accommodate traditional sensitivities in their practice (Ivry, 2010). Demography-related ecological concerns are completely absent from Israeli reproductive discourses.
Israel’s first ‘IVF baby’, the world’s fifth, was born in 1982, signalling the dawn of a prosperous assisted reproductive technology industry: Israeli women undergo, on average, more IVF cycles than women in any other country. Practically all of the latest reproductive technologies are available to them: intracytoplasmic sperm injection (ICSI) has become integral to IVF; gamete ‘donation’ freezing and banking, as well as embryo freezing, surrogacy and preimplantation genetic diagnosis, are all practised legally. Whereas some treatments (e.g. surrogacy) entail extremely high costs, others (e.g. donor sperm) are available for relatively affordable sums. A few of these technologies are largely state subsidized. Sex selection is tightly regulated but is also allowed under some circumstances, as is posthumous reproduction. The adjacent field of human embryonic stem cell research is also booming.
In the following, I outline 35 years of assisted reproductive technologies in Israel by tracing a principal axis in the development of three major technologies: the proliferation of IVF-ICSI; the globalization of gamete donation; and the privatization of surrogacy. Evidently, all three axes are present to some degree in the trajectories of each technology. The paper is based on a policy analysis as well as on additional studies of assisted reproductive technologies, which I have conducted in Israel over this period. The latter have all been conducted in accordance with ethical guidelines and have received the required ethics approval. The paper’s primary focus on assisted reproductive technology policies highlights the state’s role in the shaping of Israel’s assisted reproductive technology landscape. While the state’s influence appears to be extremely significant, it is crucial to acknowledge that Israeli women have been agential in numerous assisted reproductive technology contexts, ranging from ensuring religion-compatible practice (Ivry, 2010) to withdrawing from treatment (Haelyon, 2007) to actively participating in the formation of the egg donation law (Hashash et al., 2008).
Proliferation: IVF-ICSI
Fertility treatments have been state funded in Israel since their establishment. The introduction of IVF by local doctors, in 1981, was welcomed as a ground-breaking addition to the existing, publicly funded fertility treatments and the birth of the first local ‘IVF baby’ was celebrated in the media as a collective national accomplishment, led by saviour local experts (Birenbaum-Carmeli, 1997, Birenbaum-Carmeli et al., 2000). In the subsequent two decades, IVF units opened in most Israeli hospitals. Politicians, service providers, rabbis, doctors, feminists and laypersons all praised the innovative technology.
State support for assisted reproductive technologies was swiftly inscribed into Ministry of Health (MOH) regulations that entitled every Israeli woman aged 18 to 45, irrespective of her family status or sexual orientation, to unlimited, funded treatment up to the birth of two live children with her current partner, if applicable. Attempts to ration IVF have all resulted in an outcry from politicians, professionals, consumers and feminists (Birenbaum-Carmeli, 2004), leaving the unlimited funding intact. Conservative estimates assess IVF expenditure, without concomitant costs (e.g. associated with twin births), at 2% of Israel’s health budget.
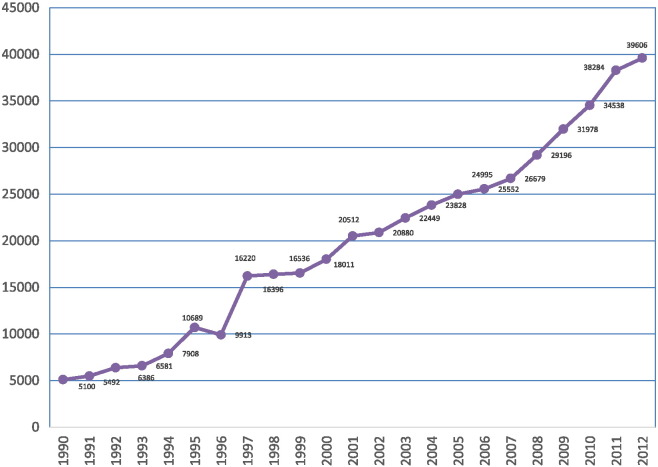
Maintaining the world’s highest rate of clinics per capita for some two decades (Collins, 2002), Israel’s 25 IVF clinics constantly expand their activity (MOH, 2015a). As shown in Fig. 1, the number of IVF cycles performed annually rose from 5000 in 1990 to 40,000 in 2012, visibly outpacing the local population growth.
Fig. 1.
Number of IVF cycles per year in Israel.
The steep rise in IVF use in 1996 reflects the fast adoption of ICSI in Israel, which turned IVF-ICSI into the standard treatment for male infertility as well. Given the presence of male factor in roughly half of all infertility cases in Israel (Berman et al., 2012), the endorsement of ICSI practically doubled the number of IVF clientele. The expansion continued, however. Between 2000 and 2012, the rate of treatment cycles rose by 82.7% (MOH, 2015a). Israeli women are the world’s greatest consumers of IVF (see Table 1), undergoing twice as many cycles per capita as Danish women, who are in second place. Israel’s usage of IVF is over five times the European average and ten times the international average (Sullivan et al., 2013).
Table 1.
Prevalence of IVF in selected countries.
| Country | Population size (million)a | No. of IVF cyclesb | No. of IVF cycles/million people |
|---|---|---|---|
| Israel | 7.209 | 38,284 | 5311 |
| Denmark | 5.569 | 14,578 | 2618 |
| Australia/NZ | 26.909 | 66,347 | 2466 |
| Sweden | 9.723 | 18,510 | 1904 |
| Spain | 47.737 | 66,120 | 1385 |
| France | 66.259 | 85,433 | 1289 |
| EU | 511.434 | 588,629 | 1151 |
| Italy | 61.680 | 63,777 | 1034 |
| UK | 63.742 | 59,807 | 938 |
| Germany | 80.996 | 67,596 | 835 |
| USA | 318.892 | 151,923 | 476 |
| Russia | 142.470 | 56,253 | 395 |
Accordingly, IVF live births rose from 1.7% of Israel’s total live births in 1995 to 4.3% in 2013 (Haklai, 2015). The mean live births per delivery has slightly dropped, from 1.3 to 1.2 from 2003 onward (ibid), reflecting the limited implementation of the single embryo transfer policy, possibly due to the relatively advanced age of Israeli IVF users (Israeli Fertility Association, 2010).
The exceptional usage is linked to the high age limit (45 years) of eligibility for funded IVF, as reproductively older women normally require more treatment cycles to conceive. Indeed, a third of IVF treatments in Israel are delivered to women above 40 (Sela et al., 2013). Israeli fertility doctors are well aware of the reduced success rate of IVF-assisted delivery in advanced age. When asked, they attribute their practice to women’s insistence, which is bolstered by the state’s funding policy.
Notably, the potential health risks posed by multiple IVF cycles are hardly discussed, or systematically researched, even though Israeli doctors have unique access to the subject, due to the exceptional local usage. Doctors explain the research lacunae by the lack of a national IVF registry, which was founded only in 2012, three decades after the technology arrived and spread in the country.
In 2014, partly in conjunction with the establishment of the new registry, moderate restrictions were placed on the provision of IVF (i.e. if no embryo was transferred in four consecutive cycles, or no conception occurred in eight cycles, the woman should undergo reassessment before further treatment). Some politicians protested even against these lenient limitations as injurious to women and to Jewish reproduction. The routinization of IVF in Israel was well captured by an Israeli woman who attributed her choice to undergo IVF as being ‘the easiest route to pregnancy’ (Birenbaum-Carmeli and Dirnfeld, 2008).
Israel’s IVF industry has become world famous and as a result, it attracts international consumers. Some users, primarily Russian clients, seek prestigious IVF services. For them, the geographical proximity, the relatively affordable prices and the numerous Russian-speaking professionals – Jewish doctors and nurses who immigrated to Israel in the 1990s – render Israel the destination of choice. Other reproductive travellers arrive from countries where IVF is substantially costlier, such as the USA (Shamah, 2012). Some of these travellers, although not all, are Jewish. Occasionally, some Jewish Americans immigrate to Israel in order to receive state-funded IVF as Israeli citizens.
In an attempt to attract this international clientele, Israeli clinics, including major medical centres like Hadassah in Jerusalem, advertise their services in foreign languages. International brokers entice consumers by using tourism language: ‘Need IVF? Want to visit Israel? Combine the two with us’ and suggest ‘the idea that Christians can come and get healed in the place where Jesus did his healing’ (Shamah, 2012).
Globalization: gamete donation
Globalization has great prominence in Israel’s donor gamete economy. Until the early 1990s, the simple technology of donor insemination (DI) was informally practised in Israel. A gynaecologist would synchronize the clinic appointment of a receiving couple with a donor’s visit, so he could perform insemination while ensuring that the parties didn’t meet (Birenbaum-Carmeli et al., 2000, Carmeli and Birenbaum-Carmeli, 2000). In 1992, still before ICSI, when DI was used mainly to overcome male infertility among heterosexual couples, new MOH regulations confined DI to hospital-based sperm banks and banned the use of fresh sperm due to HIV risk. The state regulations also required that prior to DI the doctor established ‘the woman’s inability to conceive… by her partner’s sperm exclusively’. The state was thus willing to pay for IVF and to jeopardize women’s health in order to enhance the supremacy of biogenetic reproduction over alternatives. When DI was unavoidable, the regulations sought to feign a ‘natural family’ appearance: the state bestowed the responsibility for donor matching on the doctor alone and enforced permanent secrecy on the procedure. Moreover, it recommended that whenever possible, the doctor mixed the donor’s sperm with the husband’s, so as to blur the baby’s genetic origin (Carmeli and Birenbaum-Carmeli, 2000). Lacking an alternative solution to male infertility or a source for donor sperm, and largely sharing the ‘natural family’ ideology, Israeli recipients, mostly heterosexual couples, complied with the regulations.
At that time, sperm banking already had an international component. According to traditional Jewish law, the ‘wasting’ of sperm, even for the purpose of DI, is a sin. Orthodox couples therefore prefer to use sperm of non-Jewish men, thereby also removing the concern of future incest. To serve this population, a peripheral hospital in Israel ran a small sperm bank of non-Jewish kibbutz volunteers (Kahn, 2000).
Since the introduction of ICSI, heterosexual couples hardly seek DI. Sperm banks currently serve primarily single and lesbian women. Incidentally, the change in clientele coincided with a decline in sperm donors, forcing recipients to wait long months for suitable sperm (Rosenblum, 2010). Various explanations may account for the decline in sperm donors: the relatively modest payment to donors ($80–150 per sample); the fear of upcoming disclosure policy (ibid); lower willingness to assist single and lesbian women (rather than infertile men); a State Comptroller report (2006) that disclosed irregularities in the management of sperm banks, including allowing over 25 babies per donor (State Comptroller, 2006). Additionally, foreign kibbutz volunteers grew rarer, leading to a decline in non-Jewish sperm donors and closing of the local non-Jewish sperm bank. (Muslim and Christian Arab men hardly donate sperm in Israel. For discussions of the prohibition of gamete donation in Sunni Islam, see Inhorn and Gurtin, this issue.)
Births out of wedlock are rare in Israel (roughly 5%). However, whether due to growing legitimacy of this parental formation or further intensification of the maternal imperative (Donath, 2015), the figure has been increasing consistently during the last two decades (Central Bureau of Statistics, 2011). In line with this trend, the demand for donor sperm has also risen. With the mounting demand and dwindling supply, in the context of intense globalization, purchasing sperm abroad has become both necessary and feasible. Israeli women, as well as Orthodox couples, started to avail themselves of this option. In response, the MOH issued licences for individual women or couples to import sperm from sperm banks abroad. This practice has gradually spread and a substantial portion of donor sperm in Israel is now imported. Notably, both local and ‘foreign’ sperm are not state subsidized and prices are constantly increasing. In 2011, the price of domestic donor sperm had doubled from $100 to $210 per sample. Imported sperm currently varies between $650 and $1000 (Doron, 2011). Given the average Israeli monthly salary of $1900 ($2200 for men and $1450 for women; annual income is $26,000 and $17,400, respectively; Bendlak, 2012), these sums are significant but not unaffordable.
In 2008, years after the routinization of ICSI, which resolved most male infertility problems and rendered sperm donation a technology that serves mostly single and lesbian women, when the field had been thoroughly globalized, Israel’s MOH removed from its DI regulations the prerequisite to ‘establish the woman’s inability to conceive by her partner’s sperm’, which in practice subjected fertile women to IVF as a condition for DI. It also banned the mixing of the donor’s sperm with that of the husband. This revision offers a good illustration of both the state’s power to channel assisted reproductive technology practice so as to promote particular interests (e.g. the superiority of biogenetic over social kinship) and the capacity of laypersons to circumvent state diktats in the age of globalization (e.g. by finding alternative sources abroad). In March 2015 the state further simplified the importation of sperm, when it licensed several foreign sperm banks to serve Israelis without the need for personal approvals (MOH, 2015b).
Egg donation presents a different set of challenges. Until 2010, only women undergoing IVF were allowed to donate eggs in Israel. Other donations – commercial or altruistic – were banned. In this context of a shortage of donor eggs, a major clinical scandal broke out in 2000. A senior fertility expert was found to have over-medicated patients in order to procure numerous eggs – as many as 100 per woman – many of which he sold to his other patients. The ‘donating’ women were either partly or completely unaware of the procedure. The exposure of this malpractice stirred great disquiet, following which Israeli gynaecologists hardly ever bring up the option of egg donation. Meanwhile, more and more women of advanced reproductive age were seeking conception, increasing the demand for eggs. Seeking eggs abroad has been virtually the only option for these Israeli women.
Since Jewish identity is inherited matrilineally, the involvement of non-Jewish egg donors is religiously sensitive. Traditionally the birth mother, namely ‘the womb’, was considered the defining component (Kahn, 2000). The ability to separate the womb from the egg has destabilized this criterion. Some Rabbis contend that only an egg of a Jewish donor ensures the child’s Jewishness (David, n.d.). Others adhere to the womb as the decisive factor and apply the ‘foreign sperm logic’, i.e. preferring eggs of non-Jewish donors as they remove the concern of future incest (ibid).
The landscape of transnational egg donation reveals that Israelis endorse both approaches. Some Israelis seek ‘Jewish eggs’ despite their sky-rocketing prices ($30,000–50,000; Cain-Nielsen, 2013, Embryon, 2015, NY LifeSpring, 2015, Or-El, 2010, Ryan, 2012). This practice suggests that ova donation may enhance the weight of genetic materiality as a defining factor in contemporary Jewish identity (Nahman, 2006).
Most Israelis opt, however, for ova of non-Jewish donors, which they obtain via Israeli doctors who run egg donation clinics abroad, primarily in Eastern Europe (Nahman, 2006, Nahman, 2011, Nahman, 2013). Such traffic of ova and women has been in place for well over a decade and is well established. Notably, in all transnational donations the foreign donors and the Israeli recipients remain anonymous to each other. At present, following several cases in which Israeli practitioners were suspected of breaching the local law of the ova donors’ country of origin (e.g. Romania), and similar to DI licensing, the MOH approved certain clinics in Eastern Europe and the USA to provide donor ova to Israeli recipients (MOH, 2015c).
The source countries for donor eggs are noteworthy, as Israelis, even those who obtain non-Jewish donor eggs, apparently attribute social significance to the gametes. Somewhat similar to the sperm bank director who said he ‘wouldn’t give “Arab sperm” to a Jewish woman’ (Carmeli and Birenbaum-Carmeli, 2000), most Israeli recipients would refuse Palestinian ova, although most are happy to accept ‘Romanian eggs’ (Nahman, 2013). The openness to some ova alongside the rejection of others suggests that the application of assisted reproductive technologies is greatly influenced by extra-genetic nationalist notions of ‘chosenness’ (Weiss, 2002) as well as consumerist, class ideas about white and European identities (Nahman, 2006). Some recipients possibly take the use of ‘foreign eggs’ as an opportunity to influence the child’s appearance, so they look more European or Ashkenazi (Birenbaum-Carmeli and Carmeli, 2002a, Birenbaum-Carmeli and Carmeli, 2002b, Nahman, 2006, Nahman, 2013, Carmeli et al., 2001). The total disregard of neighbouring countries like Greece or Turkey as sources for donor eggs is especially significant, given that about half of Jewish Israelis are of Middle Eastern descent.
Like donor sperm, donor eggs are not state funded. In the rare cases where the donation is carried out in Israel, the payment to the egg donor is $5000. However, as mentioned, few Israelis step forward as egg donors. Foreign egg donations reach $7000–8000 per cycle, or $12,000 for a shared risk cycle, which covers a second cycle if the first one fails (Hadassah Medical Centre, 2015). Private health insurances reimburse up to $3000 for all the cycles towards each of the woman’s first two children (Clalit, 2015). Egg donation thus requires over half an average annual income, which renders the treatment inaccessible for many Israelis, especially for single women, whose income is, as mentioned, about a third lower than men’s.
Possibly because it entails complex international transactions and potential harm to donors, the regulation of egg donation has invoked relatively intense reactions among Israeli feminists (Eyal et al., 2008, Noy et al., 2007). In 2010, following discussion with the latter, new MOH regulations were published, allowing any healthy, single woman aged 21–35 to donate eggs up to three times in her life, paying close attention to the donor’s well-being. The regulations dictate permanent donor–recipient anonymity. If one of the women is Jewish they also mandate similarity in religious affiliation, tacitly reasserting the acuteness of genetic materiality as a constituent of Jewish identity. As mentioned, the new regulations did not yield the expected change and Israeli women who need donor ova, and can afford it, keep travelling abroad.
Privatization – surrogacy
The proliferation and globalization of assisted reproductive technologies was accompanied by extensive privatization of services. Although renowned for its free IVF policy, Israel’s assisted reproductive technology sector has seen an ever-growing personal investment. Nowhere is this trend more prominent than in surrogacy, the most complex and expensive of assisted reproductive technologies. As will be shown below, however, financial privatization does not mean freedom from state inspection or licensing. Rather, the opposite is true. Surrogacy is tightly controlled by the state of Israel: domestic surrogacy places every applying couple under close state scrutiny as a prerequisite to contract approval; same-sex couples are effectively forced to look for surrogacy solutions outside the country but even they must comply with a wide set of state requirements in order to be granted the right to register their babies as Israeli citizens. The term ‘privatization’ thus designates in the present context two principal features: private funding and private initiative in attending to all surrogacy-related logistics.
Until the early 1990s, surrogacy was illegal in Israel. In 1991, an Israeli estranged couple, Ruti and Danny Nahmani, had a fierce legal dispute over the transplantation of their embryos in an American gestational surrogate. Ruti was over 40 and had had her womb removed due to illness. When she was about to fly to the USA to have the embryos transplanted, Danny withdrew his consent as he had formed a new relationship. Ruti sued Dani and won her case. Danny appealed to the Supreme Court and won, but then lost again in Ruti’s subsequent re-appeal to the Supreme Court (Birenbaum-Carmeli, 2007). In 1996, shortly after this perplexing case, Israel formed its Embryo Carrying Agreement Law, becoming the world’s first country to regulate surrogacy by means of dedicated primary law. The swift ratification of the law suggests the deep disquiet that surrogacy has stirred in Israel (Teman, 2010). Israel’s law permits only gestational surrogacy, namely using an egg that is not the surrogate’s. Moreover, it is available only to stable heterosexual couples. By restricting access to heteronormative couples, the state has contained surrogacy within the bounds of traditional families, thereby largely neutralizing its revolutionary potential. Like all other forms of assisted reproductive technology, surrogacy was rapidly endorsed by Israelis. As of 2013, 516 babies had been born in Israel via surrogacy (Hashiloni Dolev, 2013).
Israeli scholars, especially feminists, are divided regarding the surrogacy law. Some criticize the use of the bodies and lives of surrogates for the benefit of others (Lipkin and Samama, 2011) while others (Teman, 2010) described meaningful relations between surrogates and intended parents. The general public, however, showed no active interest in the law and accepted it as peacefully as it had received previous assisted reproductive technology laws and regulations.
Surrogacy entails extensive financial investment. When it takes place in Israel, the treatment of the women – the surrogate and the intended mother – is covered by the latter’s public health insurance. Additional costs, like legal advice to the surrogate, insurance and compensation for her time, suffering and loss of income, are paid by the commissioning couple. The total sum, exceeding $40,000 (Pundekaut.com, 2015), equals two average annual Israeli incomes. Carrying twins or delivering by Caesarean section entitles the surrogate to additional payment (Gal, 2008).
Cross-border surrogacy, which is the only option available to single and gay Israelis, is costlier still. (Some heterosexual couples, who wish to distance the surrogate from their lives, also turn to cross-border surrogacy.) Gay Israelis often claim that unlike their counterparts abroad, many of whom reject the hegemonic idea of the traditional nuclear family, numerous gay Israelis, mostly couples, are keen to raise children in a pretty conservative manner. Although data regarding the relative prevalence of this trend are unavailable, the recurrent statements represent a spirit that flows through Israel’s gay community. In 2012, 255 formal requests to register children born abroad through surrogacy were submitted to Israel’s Ministry of Foreign Affairs (State Comptroller, 2014, 798). These babies are converted to Judaism shortly after their arrival in Israel. The Israeli documentary, Google Baby (2012), captures the enormous investment that Israelis make in such surrogacy procedures and illustrates the globalized system that they have developed in their quest for biogenetic parenthood. Having said that, many gay Israelis declare that they are indifferent to biogenetic relatedness, claiming they were effectively forced into surrogacy because no country would place healthy adoptive newborns with gay couples (Farber, 2014).
Cross-border surrogacy depends entirely on private initiative and financing. The first Israelis who opted for this technology, over a decade ago, travelled mostly to the USA. Paying an American egg donor and an American gestational surrogate amounted to $150,000–250,000, roughly equal to 8–12 annual average Israeli salaries (2006 figures). Some gay men, senior professionals in their late 30s or 40s, who are earning two full male salaries, or those who come from wealthy supportive families, can embark on such reproductive journeys. Yet, for many gay Israelis, these sums are unrealistic.
The popularization of cross-border surrogacy occurred around 2008, when several agencies started offering surrogacy services in multiple countries. Donor eggs were purchased almost invariably from Caucasian women, primarily in Eastern Europe, the USA and occasionally in South Africa. Some agencies also offer donor eggs from non-Caucasian women, e.g. from India and Nepal. The donor or the embryos are then flown to the gestational surrogate’s clinic, often located in developing countries in Asia, depending on legislation and price shifts. This complex international combination is cheaper than the USA route, costing around $50,000–60,000. However, even this reduced price is far beyond reach for many Israelis, gay and heterosexual alike.
With the proliferation of cross-border surrogacy, some gay parents decided to try to have twins. This goal certainly represents an attempt to optimize the high expense. At the same time, it seems to embody the desire of many gay Israelis to have ‘a full family’ rather than raise a child. Formal data on the subject is unavailable. Evidently, however, Israeli gay families often comprise twins and/or siblings.
Beyond the cost, cross-border surrogacy entails a ‘private’ encounter with the state bureaucracy. This encounter is obstacle-ridden, requiring lawyer services from early pregnancy until months after the birth. The parents must wait in the birth country for a court order, followed by tissue typing in a designated laboratory. Until recently, the partner of the biological father had to undergo full adoption procedure and had no custody rights until its completion (Farber, 2014). The cumbersome procedures force commissioning parents to spend long weeks and months in the birth country, often in inconvenient accommodation, sometimes without proper health insurance for the newborns, incurring excessive costs. In the prevalent case of twin births, the babies are especially likely to require intensive medical care. The procedures further extend due to bureaucratic delays that prevent the new family from returning to Israel. Incidental problems like a clerk’s mistake or a national holiday in either country further prolong the parents’ imposed stay abroad. Some gay Israelis expressed great frustration at the state’s alienating approach, which they criticize in a national-political context:
‘The state treats us and our families as if we were second-class citizens, as if we were law breakers who took too much liberty, despite the fact that we are barred from surrogacy in Israel. For fact, we are not equal citizens like other Israelis, who don’t have to take a lawyer and go to court for every trivial issue. Though I and my partner pay our taxes fully, though I served in a prime military unit, then studied and today I work and represent my country with great honor in international conferences abroad, the state doesn’t represent me properly in whatever relates to my basic needs. All I ask for is to have a family and be a parent like any other parent in Israel.’ (Farber, 2014)
From gay men’s accounts, their use of cross-border surrogacy was not only lacking state support, but was also actively antagonized by state authorities. The excessive hardships that users of cross-border surrogacy endure was formally acknowledged by Israel’s Supreme Court as discriminatory (Supreme Court 2011, 566/11: 1–81).
This description somewhat contradicts the prevalent image of pronatalist Israel. Whereas the state does allow domestic surrogacy and accepts cross-border surrogacy, including for gay men, the state nonetheless conveys a clear message regarding its reproductive hierarchy: IVF with the parents’ gametes receives full funding even when the chance of success is remote; donor gametes are allowed but not funded and are increasingly outsourced to foreign countries (the related medical services are publicly funded); surrogacy is allowed for heterosexual couples subject to the approval of committee and is extremely costly; gay men have no option but to go overseas to fend for themselves when trying to found families. Whereas the reluctance might be advocated in the name of the human rights of gestational surrogates, the state-imposed difficulties hardly refer to this aspect and rather focus on the new families’ relatedness, for instance, in requiring genetic tests from the parents.
In the past few years, homosexual couples have repeatedly protested against their exclusion from domestic surrogacy, with some claiming their right to contact a Jewish surrogate in order to ensure the child’s Jewishness. In 2010, the MOH responded to the mounting discontent by convening the Mor-Yosef Committee to consider surrogacy and assisted reproductive technologies in general. The committee acknowledged gay men’s demands, and proposed to entitle single and gay applicants to domestic surrogacy. If applied, these recommendations would further expand the scope of surrogacy in Israel and intensify moral issues regarding the rights of surrogates. At the same time, it will promote the reproductive rights of gay people. (Notably, a minority in the committee expressed concern that the relative financial fortitude of gay couples might push up surrogacy prices, thereby rendering it inaccessible for the generally poorer heterosexual couples for whom the law was originally devised.)
Meanwhile, minor changes make cross-border surrogacy somewhat more gay-friendly. As of 2009, gay men are entitled to maternity benefits and as of March 2015, the highly complex adoption procedure was replaced by the simpler and swifter legal procedure that leads to the issuing of ‘parenting order’.
Discussion
The expansion of assisted reproductive technologies in Israel over the last three decades has reflected and furthered their normalization. Present-day reproduction in Israel is thoroughly technologized, with assisted reproductive technologies perceived by both professionals and laypersons as integral to procreation. From pre-conception testing to pregnancy follow-up, practically all Israeli women subject themselves to repro-technological monitoring that has become part and parcel of ‘normal pregnancy’ (Ivry, 2010).
When facing a fertility problem, assisted reproductive technologies come to the fore. As discussed, Israelis make use of multiple reproductive technologies, from IVF-ICSI to gamete donation and surrogacy. Indeed, due to the generous public funding policy, assisted reproductive technologies are more accessible in Israel than anywhere else and are within the reach of wider population segments. Whereas this policy can – and should – be probed critically, its enabling impact does allow Israelis, including poorer couples and single women, to materialize the quest for parenthood, with its far-reaching personal and social implications in Israel. Potentially, the sweeping endorsement of assisted reproductive technologies might have distanced conception from ‘nature’ and even erode ‘nature’ as the basis for kinship. The findings suggest, however, the opposite, that following the spread of assisted reproductive technologies, notions of biogenetic relatedness dominate reproduction in Israel. DI was replaced by ICSI and adoption by egg donation and surrogacy; a thriving donor-matching industry helps recipients of donor gametes ‘pass as natural’ and the media praises women who persist in exceptionally long fertility treatments. Biological parenthood, previously ‘destiny’, has been largely reconfigured as ‘accomplishment’, rendering childlessness and even adoption as nearly a ‘failure’, for presumably anyone passionate and determined enough can have their ‘own’ biogenetic offspring. In this social climate, biological parenthood has become an embodiment of parents’ desire, resourcefulness and financial fortitude.
The trajectories outlined above – proliferation, globalization and privatization – paint a polarized assisted reproductive technology landscape. On the one hand, the state provides comprehensive funding for an expanding IVF-ICSI industry, thereby conveying its strong support of traditional biogenetic families and constituting such relatedness as a life goal that is worth ‘fighting’ for. On the other hand, the state leaves Israelis who require donor gametes or surrogacy (let alone adoption) to fend for themselves in a globalized, privatized world. Although the state legally regulates these modes of family formation, it offers no support to local users who must rely on, and possibly deplete, their private resources. Israel’s assisted reproductive technology policy has thus set up a two-tier system wherein biogenetic relatedness is state-enshrined and privileged while also requiring massive technological assistance, whereas ‘incomplete’ forms of biogenetic kinning are relegated to the personal domain where seekers must pursue options by themselves.
Given the polarized funding policy and the exceptional usage of all forms of assisted reproductive technologies in Israel, one wonders whether this assisted reproductive technology landscape possibly captures broader local dynamics. Two major trends seem relevant in this context: the expansion of neoliberalism and rising primordialism. In the spirit of neoliberal autonomy, Israelis are called to set their own personal life goals freely. Striving for a biogenetic family is widely viewed as a worthy personal goal. Thus, when Israelis undergo tens of IVF cycles or travel the world in search of donor gametes or gestational surrogates, they pursue an autonomous desire for biogenetic relatedness. Other Israelis – and non-Israelis – may decide to sell their gametes or carry a surrogate pregnancy. Although all are governed by state laws, these actors embark on their quests at their own discretion as well as responsibility and risk.
This autonomous – or presumably autonomous – personal quest advances, however, several state interests. Economically, it generates market activity, stimulating the local public and private health sectors as well as international commerce. Demographically, by endorsing the pronatalist ‘imperative’, Israelis contribute, of their own free will, to enlarging the country’s Jewish population. Although IVF-ICSI is available to all Israelis, including non-Jewish citizens, with growing globalization and privatization, assisted reproductive technology conception becomes increasingly stratified and accessible to wealthier sectors that consist, primarily, of Jewish Israelis.
A probably more foundational contribution of Israel’s two-tier assisted reproductive technology policy is, however, to its regional politics. It is in this sphere that the intensifying primordialism comes into play. Zionism, since its early days, constituted the biological as a symbolic currency for grounding claims about collective Jewish genealogies and concomitant national rights (Falk, 2006a, Falk, 2006b, Hirsch, 2009). The emphasis on biogenetic relatedness highlights the primordial aspect in individual families as well as in the Jewish collectivity. Assisted reproductive technologies, which enable novel forms of kinning, destabilize traditional notions of biogenetic relatedness. As such, they pose a threat to the ‘naturalness’ of genealogy and hence, of the Jewish collectivity as primordial. If notions of biological relatedness indeed resonate with and indirectly advance Israel’s political claims, including the claim to the ‘land of our forefathers’, a proactive state effort to sustain this crucial idiom of relatedness seems plausible. The toll that this assisted reproductive technology policy takes from Israelis – women who undergo tens of treatment cycles and seekers of less traditional kinning who receive no state support – might be viewed as an aspect of the liberty that the state can take when it defines an issue as the protection of life itself. In a neoliberal reality, this toll may sometimes be largely self-inflicted.
From this perspective, Israel’s polarized assisted reproductive technology policy, which reaffirms the priority of biogenetic relatedness over social kinning, enhances the centrality of the former as a constituent of Jewish collectivity. This interpretation helps elucidate the vast state investment in assisted reproductive technologies that can now be understood as an element in the state’s broader national project.
Biography

Daphna Birenbaum-Carmeli is a health sociologist in the Department of Nursing at the University of Haifa, Israel. Her main research is in the domain of women’s health, with a focus on reproduction-related issues: assisted reproductive technologies, power relations and reproductive policies. More generally, Birenbaum-Carmeli is interested in the interface of healthcare and international politics, particularly the implications of the Israeli–Palestinian conflict on healthcare in the region. Her current major project (with Marcia C Inhorn) focuses on medical and social egg freezing in Israel and the USA. Birenbaum-Carmeli has published extensively in books and professional journals.
Declaration: The author reports no financial or commercial conflicts of interest.
References
- Bendlak J. Average salary and income by settlement and various economic variable 2010, Institute of National Security, Survey 240, Jerusalem, p. 14. 2012. https://www.btl.gov.il/Publications/survey/Documents/seker_240.pdf
- Berman T., Levine H., Gamzu R., Grotto I. Trends in reproductive health in Israel: implications for environmental health policy. Israel Journal of Health Policy Research. 2012;1:34. doi: 10.1186/2045-4015-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birenbaum-Carmeli D. Pioneering Procreation: Israel’s First Test-Tube Baby. Science as Culture. 1997;6(4):525–540. [Google Scholar]
- Birenbaum-Carmeli D. Cheaper than a Newcomer: On the political economy of IVF in Israel. Sociology of Health & Illness. 2004;26(7):897–924. doi: 10.1111/j.0141-9889.2004.00422.x. [DOI] [PubMed] [Google Scholar]
- Birenbaum-Carmeli D. Contested Surrogacy and the Gender Order: An Israeli Case Study. Journal of Middle East Women Studies. 2007;3(3):21–44. [Google Scholar]
- Birenbaum-Carmeli D., Carmeli Y.S. Hegemony and homogeneity: Donor Preferences of recipients of donor insemination. Journal of Material Culture. 2002;7(1):73–94. [Google Scholar]
- Birenbaum-Carmeli D., Carmeli Y.S. Physiognomy, familism and consumerism: Preferences among Jewish Israeli recipients of donor insemination. Social Science and Medicine. 2002;54(3):363–376. doi: 10.1016/s0277-9536(01)00035-1. [DOI] [PubMed] [Google Scholar]
- Birenbaum-Carmeli D., Dirnfeld M. The more the better? IVF policy in Israel and women’s views. Reproductive Health Matters. 2008;16(31):1–10. doi: 10.1016/S0968-8080(08)31352-4. [DOI] [PubMed] [Google Scholar]
- Birenbaum-Carmeli D., Carmeli Y.S., Cohen R. ‘Our first ‘IVF baby’: Israel’s and Canada’s Press coverage of procreative technology. International Journal of Sociology and Social Policy. 2000;20(7):1–38. [Google Scholar]
- Cain-Nielsen K. Selling my eggs to make rent, Salon, FEB 3, 2013. 2013. http://www.salon.com/2013/02/03/selling_my_eggs_to_make_rent_partner/
- Carmeli Y.S., Birenbaum-Carmeli D. Ritualizing the ‘Natural Family’: Secrecy in Israeli Donor Insemination. Science as Culture. 2000;9(3):301–325. [Google Scholar]
- Carmeli Y.S., Birenbaum-Carmeli D., Madgar I., Weissenberg R. Donor insemination in Israel: Recipients’ choices of donors. The Journal of Reproductive Medicine. 2001;46(8):757–763. [PubMed] [Google Scholar]
- Central Bureau of Statistics Births and Fertility in Israel. 2011. http://www.cbs.gov.il/publications11/rep_04/pdf/5box1_h.pdf (p. 210)
- CIA factbook Total Fertility Rate by country. 2015. https://www.cia.gov/library/publications/the-world-factbook/rankorder/2127rank.html (accessed September 30, 2015)
- CIA Factbook Population by country. 2015. https://www.cia.gov/library/publications/the-world-factbook/rankorder/2119rank.html
- Clalit Egg donation from a foreign country. 2015. https://mushlam.clalit.co.il/Woman/PREGNANCY_PREPARATION/Pages/ovum_donation_abroad.aspx#ServiceGetter
- Collins J.A. An International Survey of the Health Economics of IVF and ICSI. Human Reproduction Update. 2002;8:265–277. doi: 10.1093/humupd/8.3.265. [DOI] [PubMed] [Google Scholar]
- David S. n.d. Summary of the Hallachah view on fertility treatments, http://www.tik-tak.co.il/web/project/katava1.asp?codeClient=469 and id = 8100
- Donath O. Women’s Studies International Forum, Pergamon. 2014. Choosing motherhood? Agency and regret within reproduction and mothering retrospective accounts. [Google Scholar]
- Donath O. Regretting motherhood: A Sociopolitical Analysis. Signs. 2015;40(2):343–367. [Google Scholar]
- Doron A. What is the most highly demanded product? Donor sperm, NRG, May 5, 2011. 2011. http://www.nrg.co.il/online/1/ART2/244/578.html
- Embryon 2015. http://www.embryon.co.il/%D7%9E%D7%A1%D7%9C%D7%95%D7%9C%D7%99%D7%9D/%D7%AA%D7%95%D7%A8%D7%9E%D7%AA-%D7%99%D7%94%D7%95%D7%93%D7%99%D7%94
- ESHRE Fact sheet. 2014. http://www.eshre.eu/Guidelines-and-Legal/ART-fact-sheet.aspx; (Israel figures: http://www.health.gov.il/PublicationsFiles/IVF1986_2012.pdf)
- Eurostat 2015. http://ec.europa.eu/eurostat/tgm/table.do?tab=table and init = 1 and language = en and pcode = tsdde220 and plugin = 1
- Eyal H., Hashash Y., Lipkin N. Report: Egg Donation bill situation report, Woman to Woman. 2008. http://isha.org.il/wp-content/uploads/2014/08/egg-donation.pdf
- Falk R. Resling; Tel Aviv: 2006. Zionism and the Biology of the Jews. (Hebrew) [Google Scholar]
- Falk R. Zionism, race and eugenics. In: Cantor G., Swetlitz M., editors. Jewish Tradition and the Challenge of Darwinism. University of Chicago Press; Chicago: 2006. pp. 137–162. [Google Scholar]
- Farber A.R. University of Haifa; Haifa, Israel: 2014. Surrogacy and Fatherhood among Homosexual Couples in Israel. MA thesis. [Google Scholar]
- Gal I. Study shows: How much does surrogacy cost in Israel and abroad, Ynet, April 15, 2008. 2008. http://www.ynet.co.il/articles/0,7340,L-3532171,00.html
- Glickman A. Public Opinion [De’ot Ba’am], no. 7. 2003. Marriage in Israel on the threshold of the 21st century [Hebrew] [Google Scholar]
- Google Baby YouTube. 2012. https://www.youtube.com/watch?v=pQGlAM0iWFM
- Hadassah Medical Centre Egg donation. 2015. http://www.hadassah-med.com/medical-care/departments/obstetrics-and-gynecology-ein-karem/egg-donation.aspx
- Haelyon H. Pardes Publishers; Haifa: 2007. Locked Garden–Experience of Israeli women undergoing in-vitro fertilization treatments. (In Hebrew) [Google Scholar]
- Haklai Z. IVF Treatments, 1990–2013 [Hebrew], MOH. 2015. http://www.health.gov.il/PublicationsFiles/IVF1986_2013.pdf
- Hashash Y., Lipkin N., Eyal H. Isha Le’isha; Haifa: 2008. Report: Egg Donation Law Proposal. [Google Scholar]
- Hashiloni Dolev Y. Modan; Ben Shemen: 2013. The Fertility Revolution. [Google Scholar]
- Hirsch D. Zionist eugenics, mixed marriage, and the creation of a ‘new Jewish type. Journal of the Royal Anthropological Institute. 2009;15:592–609. [Google Scholar]
- Israeli Fertility Association . Position paper no. 201, April 15, 2010. 2010. Embryo Transfer in IVF. ( http://www.ayala.org.il/?CategoryID = 239 and ArticleID = 180 [Hebrew]) [Google Scholar]
- Ivry T. Kosher medicine and medicalized halacha: An exploration of triadic relations among Israeli rabbis, doctors, and infertility patients. American Ethnologist. 2010;37(4):662–680. [Google Scholar]
- Kahn S.M. Duke University Press; Durham and London: 2000. Reproducing Jews: a Cultural Account of Assisted Conception in Israel. [Google Scholar]
- Lipkin N., Samama E. Isha l’Isha (Woman to Woman), Haifa. Hebrew (WTW Report) 2011. Surrogacy in Israel: Status Report 2010 and Proposals for Legislative Amendment. ( http://isha.org.il/wp-content/uploads/2014/08/surrogacy_web.pdf) [Google Scholar]
- MOH 2015. http://www.health.gov.il/PublicationsFiles/IVF1986_2012.pdf
- MOH Donor sperm – Sperm banking. 2015. http://www.health.gov.il/Subjects/fertility/Pages/sperm-bank.aspx
- MOH Egg donation. 2015. http://www.health.gov.il/Subjects/fertility/ovum_donation/Pages/default.aspx
- Nahman M. Materializing Israeliness: Difference and Mixture in Transnational Ova Donation. Science as Culture. 2006;15(3):199–213. [Google Scholar]
- Nahman M. Reverse traffic: intersecting inequalities in human egg donation. Reproductive Biomedicine Online. 2011;23(5):626–633. doi: 10.1016/j.rbmo.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Nahman M. Palgrave MacMillan; Houndmills, Basingstoke: 2013. Extractions: An Ethnography of Reproductive Tourism. [Google Scholar]
- Noy S., Hashash-Daniel Y., Mishori D. Goose laying golden eggs–Egg Donation Bill, 2007. Medicine and Law. 2007;36:161–179. (Hebrew) [Google Scholar]
- NY LifeSpring 2015. http://www.nylifespring.com/ e.g.
- Or-El A. Golden Eggs, Yedioth America, December 12, 2010. 2010. http://www.ynet.co.il/articles/0,7340,L-3997050,00.html
- Pundekaut.com 2015. http://www.pundekaut.com/default.asp?include=donation
- Rosenblum S. Israelis buy donor sperm abroad due to scarcity of local donors, ynet website, August 1, 2010. 2010. http://www.ynet.co.il/articles/0,7340,L-3927847,00.html
- Ryan E.G. Want to Sell Your Eggs to Pay for College? Be Asian, Jezebel, 5/04/12. 2012. http://jezebel.com/5907657/want-to-sell-your-eggs-to-pay-for-college-be-asian
- Sela T. IVF treatments in Maccabi HMO 2007–2010 – State of Affairs. Harefuah. 2013;152(1):11–15. ([Hebrew]. http://ivf.co.il/harefua.pdf) [PubMed] [Google Scholar]
- Shamah D. Israeli medical tourism industry slowly forges ahead. 2012. http://www.timesofisrael.com/expert-israeli-medical-tourism-industry-slowly-forges-ahead/
- State Comptroller 2006. http://old.mevaker.gov.il/serve/showHtml.asp?id=2&bookid=487&contentid=8894&direction=1&frompage=458
- State Comptroller 2014. http://www.mevaker.gov.il/he/Reports/Report_248/9295a9dc-fa05-4b43-b83b-0bdef6e5d309/219-ver-4.pdf
- Sullivan E.A., Zegers-Hochschild F., Mansour R., Ishihara O., de Mouzon J., Nygren K.G., Adamson G.D. International Committee for Monitoring Assisted Reproductive Technologies (ICMART) world report: assisted reproductive technology 2004. Human Reproduction. 2013;28(5):1375–1390. doi: 10.1093/humrep/det036. [DOI] [PubMed] [Google Scholar]
- Teman E. University of California Press; Berkeley: 2010. Birthing a Mother: The Surrogate Body and the Pregnant Self. [Google Scholar]
- Weiss M. Stanford University Press; Stanford: 2002. The Chosen Body: The Politics of the Body in Israeli Society. [Google Scholar]