Abstract
We present a case of a 76 year-old, non-smoking Honduran female who was referred to our clinic for years of persistent dry cough. Cardiac evaluation was unremarkable. She denied symptoms of heartburn, allergic rhinitis, and there was no personal or family history of asthma. Her physical exam demonstrated wheezing over the right mid-posterior chest. Spirometry was within normal limits. CT-imaging of the chest demonstrated right middle lobe bronchus and lingular segmental bronchus narrowing with bibasilar atelectasis and mild interlobular septal thickening with prominent mediastinal adenopathy. Bronchoscopy showed diffuse airway hyperpigmentation, right middle lobe medial segmental bronchial stenosis and lingular segmental bronchial stenosis. Endobronchial ultrasound demonstrated enlarged mediastinal lymph nodes, and transbronchial needle aspirates revealed necrotic tissue with black anthracotic pigment. Cultures were negative. Post-procedurally, the patient revealed regular use of a wood stove in an enclosed, poorly-ventilated kitchen. Anthracosis is the black discoloration of bronchial mucosa due to deposition of carbon-based particles in the airway, usually related to chronic environmental exposures. It can eventually result in endobronchial and parenchymal fibrosis and is mostly seen in non-smokers. Burning biomass fuel from wood smoke is a risk factor in the developing world. Symptoms include cough, dyspnea, and wheezing. Spirometry will usually demonstrate obstruction. CT-based imaging can show intraluminal narrowing, predominantly affecting the right middle and right upper lobe bronchi, resulting in distal segmental collapse. Extrapulmonary findings are rare, but usually are in the form of calcified mediastinal adenopathy on CT-based imaging, which allows for differentiation from lung cancer. There is no reliable treatment though bronchodilators can achieve clinical benefit.
1. Introduction
Anthracosis is the black discoloration of bronchial mucosa due to deposition of carbon-based particles in airway mucosa, usually related to chronic environmental exposures. It can eventually result in endobronchial and parenchymal fibrosis, a condition known as bronchial anthracofibrosis. Extrapulmonary manifestations include mediastinal lymphadenopathy [1], mimicking both infection and malignancy.
2. Case presentation
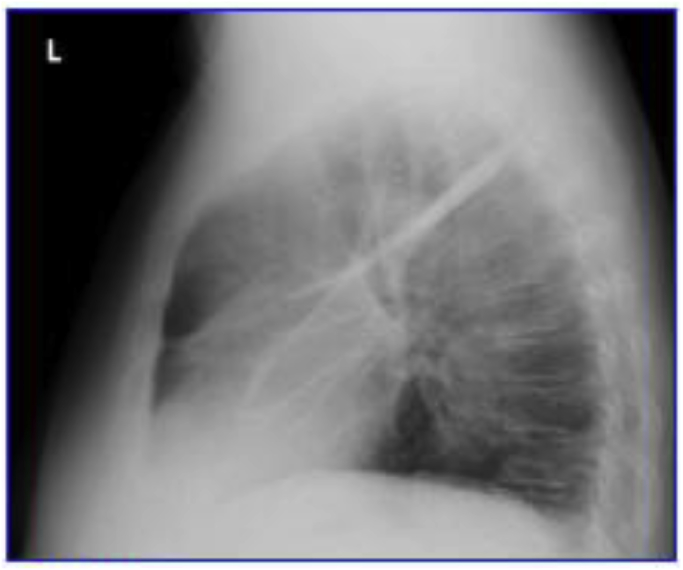
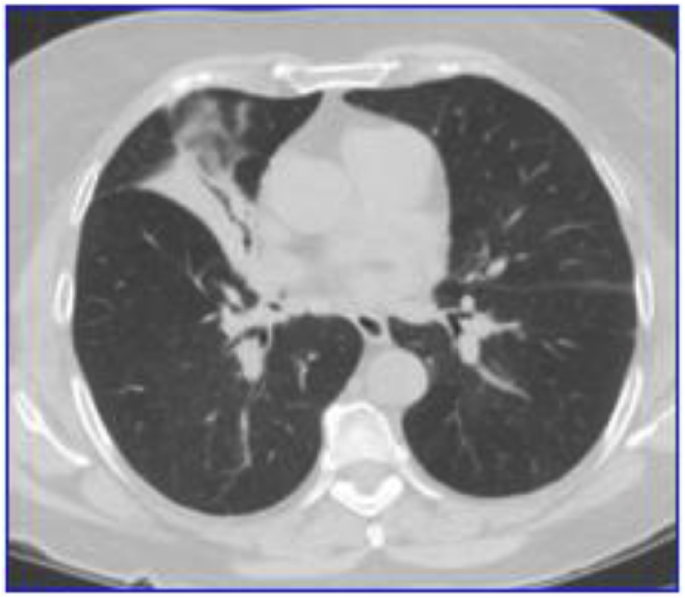
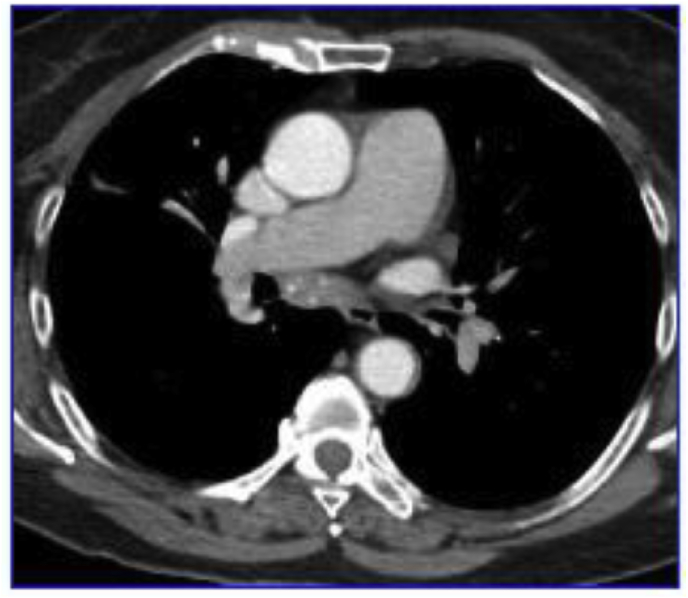
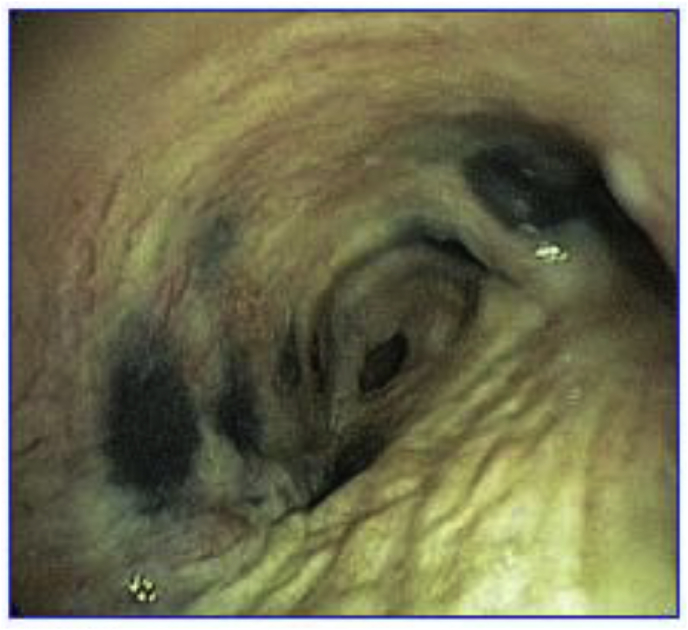
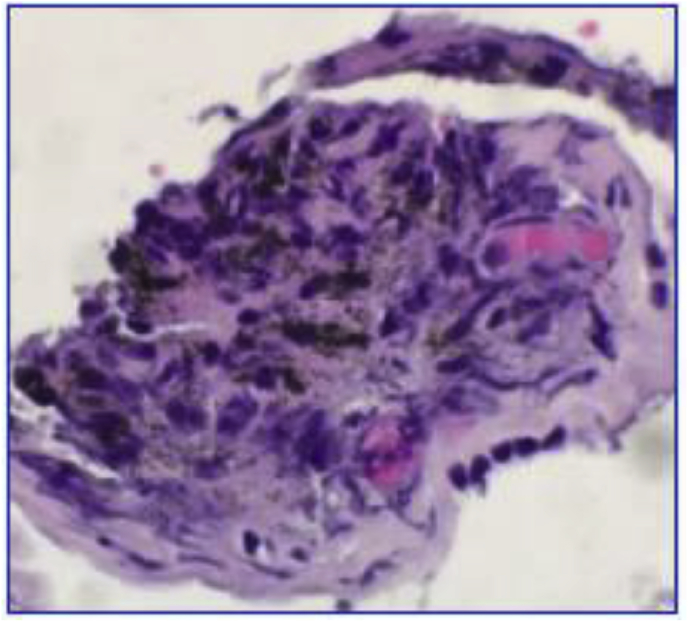
This is the case of a 76 year-old, non-smoking Honduran female with history of diabetes who was referred to our pulmonary clinic for years of persistent dry cough and non-exertional chest discomfort. Prior cardiac evaluation was unremarkable. She was treated with antibiotics by her primary care physician, which did not improve her symptoms. She did not use an angiotensin-converting enzyme inhibitor and denied symptoms of gastroesophageal reflux, allergic rhinitis, and there was no personal or family history of asthma. Her lung exam demonstrated wheezing heard over the right mid-posterior chest. Pulmonary function testing was inconclusive on multiple occasions, as she was unable to perform the required maneuvers due to excessive cough. Posterior-anterior and lateral chest radiographs demonstrated reticular thickening at the right major fissure and are shown in Fig. 1, Fig. 2. A non-contrast computed tomography (CT) scan (Fig. 3) demonstrated multiple sub-centimeter nodules, right middle lobe and lingular segmental bronchial narrowing with bibasilar atelectasis and mild interlobular septal thickening. A contrast-enhanced chest CT (Fig. 4) followed which further demonstrated distinct, enlarged mediastinal adenopathy. The differential diagnosis was broad, but it included systemic inflammatory conditions such as sarcoidosis, infections such as endobronchial tuberculosis, endemic mycosis infection and malignancy such as lymphoma and bronchogenic carcinoma. She underwent elective bronchoscopy, which showed diffuse airway mucosal hyperpigmentation and right upper lobe multi-segmental narrowing, right middle lobe medial segmental narrowing and lingular multi-segmental narrowing (Fig. 5). Endobronchial ultrasound (EBUS) demonstrated enlarged mediastinal lymph nodes, and transbronchial needle aspirates were taken at multiple stations. Sampling revealed necrotic tissue with black anthracotic pigment both grossly and microscopically (Fig. 6). Acid-fast-staining and cultures of samples were negative, though serum interferon gamma release assay was positive. Post-procedurally, the patient revealed her regular use of a wood stove in an enclosed, poorly-ventilated kitchen while a resident of Honduras for more than 40 years. She declined treatment for latent tuberculosis.
Fig. 1.
Posterior-anterior (PA) chest radiograph.
Fig. 2.
Lateral chest radiograph.
Fig. 3.
Non-contrast computed tomography of the chest.
Fig. 4.
Contrast-enhanced computed tomography of the chest.
Fig. 5.
Airway anthracosis viewed with bronchoscope.
Fig. 6.
Lymph node fine-needle aspirate demonstrating black pigment.
3. Discussion
Airway anthracosis is a well-described bronchoscopic diagnosis characterized by airway mucosal hyperpigmentation. Some patients can progress to bronchial anthracofibrosis (BAF), a distortion of the normal airway anatomy caused by scarring, which can lead to obstructive lung disease. Anthracosis and BAF are commonly a result of chronic environmental exposure to burning biomass fuel from wood smoke, charcoal, animal dung, or certain dusts [2]. Biomass fuel is commonly used in cooking [2]. This is especially significant in developing countries, where 50% of all deaths from COPD are attributed to biomass smoke exposure, and 75% of those deaths are in women. Therefore, it is perhaps unsurprising that 80% of BAF cases are diagnosed in non-smokers [1]. Biomass fuel smoke is composed of small-diameter particulate matter from multiple compounds, often at much higher concentrations than recommended [6]. It is postulated that repeated exposure to these compounds results in chronic inflammatory changes with eventual submucosal fibrosis and focal arrow narrowing. There is also particulate matter uptake by regional lymph nodes, which enlarge and can eventually perforate into the bronchial mucosa, which may be one mechanism by which airway narrowing occurs [7]. Symptoms of BAF most often include cough, dyspnea, and wheezing. Pulmonary function testing will usually demonstrate obstruction, which is quantitatively irreversible by bronchodilators. CT-based imaging can demonstrate intraluminal bronchial narrowing, predominantly affecting the right middle and right upper lobes and resulting in distal segmental collapse [7,8]. In one case series, 69% of patients with BAF were found to have multifocal airway narrowing [8]. Extrapulmonary findings of BAF are usually in the form of calcified mediastinal adenopathy on CT-based imaging [4], which helps differentiate the CT findings from metastatic disease.
BAF bears a strong association with Mycobacterium tuberculosis infection with disparate coinfection rates from 16.6 to 60% [1,3,5]. In a seminal study by Chung et al., less than 25% of BAF patients with tuberculosis co-infection presented with classic constitutional symptoms like fever, night sweats and weight loss [7]. The most common symptoms were respiratory in nature though, such as cough and dyspnea. There is no reliable treatment for BAF beyond conservative management, though patients do often respond clinically to systemic steroids and bronchodilator therapies. In severe cases of BAF, small case series have shown there may a role for endobronchial balloon dilation and stents [9].
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.rmcr.2018.05.022.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Mirsadraee M. Frequency of tuberculosis in anthracosis of the lung: a systematic review. Arch. Iran. Med. 2013;16(11):661–664. [PubMed] [Google Scholar]
- 2.Mirsadraee M. Anthracosis of the lungs: etiology, clinical manifestations and diagnosis: a review. Tanaffos. 2014;13(4):1–13. [PMC free article] [PubMed] [Google Scholar]
- 3.Park H.J. CT differentiation of anthracofibrosis from endobronchial tuberculosis. AJR Am. J. Roentgenol. 2008;191(1):247–251. doi: 10.2214/AJR.07.2161. [DOI] [PubMed] [Google Scholar]
- 4.Bilici A. A case of anthracosis presenting with mediastinal lymph nodes mimicking tuberculous lymphadenitis or malignancy. Eur. J. Intern. Med. 2003;14(7):444–446. doi: 10.1016/j.ejim.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Gupta A. Bronchial anthracofibrosis: an emerging pulmonary disease due to biomass fuel exposure. Int. J. Tubercul. Lung Dis. 2011;15(5):602–612. doi: 10.5588/ijtld.10.0308. [DOI] [PubMed] [Google Scholar]
- 6.Salvi Sundeep. Chronic obstructive disease in non-smokers. Lancet. 2009;374:733–743. doi: 10.1016/S0140-6736(09)61303-9. [DOI] [PubMed] [Google Scholar]
- 7.Chung Man Pyo. Bronchial stenosis due to anthracofibrosis. Chest. 1998;113:344–350. doi: 10.1378/chest.113.2.344. [DOI] [PubMed] [Google Scholar]
- 8.Kim Yeon Jae. Biomass smoke induced bronchial anthracofibrosis: presenting features and clinical course. Respir. Med. 2009;103:757–765. doi: 10.1016/j.rmed.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 9.El Raouf B.A. Bronchial anthracofibrosis: treatment using airway stents. Int. J. Tubercul. Lung Dis. 2013;17(8):1118–1120. doi: 10.5588/ijtld.13.0116. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.