Abstract
Study Objectives:
To examine the prevalence and correlates of nighttime awakenings and to explore the association between sleep and cognitive development in a community sample of infants and toddlers.
Methods:
A total of 590 healthy infants (aged 2–11 months) and 512 toddlers (aged 12–30 months) from 8 provinces of China were assessed for their sleep and cognitive development. Data on sleep duration and nighttime awakenings were collected through the Brief Infant Sleep Questionnaire. Cognitive development was assessed by trained pediatricians using the Bayley Scales of Infant Development.
Results:
Prevalence of no nighttime awakening, and nighttime awakening(s) for 1×/night, 2×/night, and ≥ 3×/night was 6.8%, 20.2%, 33.2%, and 39.3% in infants, and was 25.8%, 34.6%, 23.8%, and 15.8% in toddlers, respectively. Nighttime awakenings were generally associated with younger age, lower maternal education level, and being currently breastfed. In addition, nighttime awakenings were associated with being boys in toddlers. After controlling for potential confounders, infants with nighttime awakenings for 2×/night were found to have significantly higher Mental Development Index (MDI) score, as compared to those without and those with more frequent nighttime awakenings. However, toddlers with nighttime awakenings for ≥ 3×/night had significantly lower MDI, as compared to those with fewer nighttime awakenings. Total sleep duration was not associated with any developmental indices in both infants and toddlers.
Conclusions:
Frequent nighttime awakenings are associated with poor cognitive functions in toddlers. Meanwhile, a nonlinear association between nighttime awakenings and cognitive performance was found among infants. The findings provide a developmental context for the effect of sleep on cognitive abilities in young children. Further longitudinal studies and interventional studies on the effects of parent-based sleep-focused intervention on cognitive abilities among young children are warranted.
Citation:
Sun W, Li SX, Jiang Y, Xu X, Spruyt K, Zhu Q, Tseng C, Jiang F. A community-based study of sleep and cognitive development in infants and toddlers. J Clin Sleep Med. 2018;14(6):977–984.
Keywords: cognition, infant, psychomotor performance, sleep, toddler
BRIEF SUMMARY
Current Knowledge/Study Rationale: There is some evidence on the effects of sleep in early development, yet the existing studies are limited by a relatively small sample size and selected clinical populations (eg, preterm babies, infants with snoring). Data on sleep and cognitive abilities in physically healthy young children remain scanty. Therefore, we conducted an epidemiological study to investigate different aspects of sleep in relation to cognitive abilities in a large representative community sample of infants and toddlers.
Study Impact: A distinct pattern of association between sleep quality (ie, frequency of nighttime awakenings) and cognitive abilities in young children at different developmental stages was found. The findings provide a developmental context for the implications of nighttime awakenings in early years and underscore the need to address frequent nighttime awakenings particularly in toddlers. Future research is warranted to develop parent-based, sleep-focused educational intervention in the community and to examine the effects of such intervention on children's early development.
INTRODUCTION
Inadequate sleep may have disruptive effects on the cognitive functions and learning capacity in children and adolescents.1–4 A meta-analytic review has reported a positive relationship between sleep duration and cognitive performance among 5- to 12-year-old children.5 Although the effects of sleep duration on cognition and behavioral problems have been clearly demonstrated in older children,5 the evidence of this association is less consistent in young children. For example, some studies found that short sleep duration during toddlerhood is associated with preschoolers' verbal and nonverbal performance,6,7 whereas others did not find an association between sleep duration and executive function from infancy to preschool age.8,9
Sleep problems are common in infants and toddlers (eg, 75.9% in mainland China, 24.4% in the United States).10–12 Specifically, the prevalence of nighttime awakenings among children 0 to 3 years of age ranges from 20% to 66%, depending on the defining criteria and age.13–18 Apart from insufficient sleep, behavioral sleep problems may potentially have a negative effect on several aspects of child development, including cognitive functioning.19,20 Frequent nighttime awakenings could lead to fragmented sleep and compromise the quality of sleep in young children. However, few studies have explored nighttime awakenings in relation to cognitive development in infants and toddlers.21 A previous study conducted in 10-month-old infants found that those with more fragmented sleep showed poorer performance on the Bayley Scales of Infant Development. Nonetheless, this study was limited by a small sample size (n = 50) and a narrow age range of the study participants.22 Meanwhile, other existing studies only focused on the clinical samples (eg, infants with frequent snoring),23,24 or high-risk young children (eg, those with autism).25 There has been a paucity of data to explore the relationship between nighttime awakenings and cognitive abilities in the healthy full-term developing children.
Sleep during early childhood is often affected by a constellation of biological, behavioral, psychosocial, and cultural factors.26 Increased nighttime awakenings in young children have been found to be related to the practice of co-sleeping with parents, receiving breastfeeding, and maternal mental health problems such as anxiety and depression.27–29 In a cross-cultural survey, young Asian children were found to have shorter sleep duration, and to be more likely to have frequent nighttime awakenings and to co-sleep with their parents, as compared to their white counterparts.10 Although sleep may be implicated in a child's cognitive development, whether such sleep characteristics, commonly observed in young Asian children, are linked to the development of cognitive abilities remains unclear.
To address the limitations in the existing literature, we aimed to conduct a large-scale epidemiological study to examine the prevalence and associated factors of nighttime awakenings in Chinese infants and toddlers, and to investigate the association of sleep quantity and sleep quality as reflected by nighttime awakenings with cognitive abilities in these young children.
METHODS
Study Procedure and Participants
The current study was conducted from October 2012 to March 2013, in collaboration with 16 hospitals from 8 provinces in mainland China. A multistage, stratified random sampling technique was applied to obtain a nationally representative sample of young children. The eight representative provinces (Inner Mongolia, Guangxi and Yunan in the western region, Hunan in the central region, Hebei, Shangdong, Zhejiang, and Jiangsu in the eastern region) were selected according to the geographical distribution of health-system coverage in China.30 One downtown hospital and one suburban hospital from each selected province were randomly selected to cover the populations in both urban and rural regions. All the participating hospitals have a clinic to provide maternal and child health care services to the community. All healthy full-term infants and toddlers within the target age (2 to 30 months) visiting the clinic for their regular health examination during the research period were invited to take part in the study. Children were excluded from the study if they were twins or triplets, or if they had any congenital diseases or experienced any complication at birth.
The study protocol was approved by the Shanghai Children's Medical Centre Human Ethics Committee (SCMCIRB-2012047). Written informed consent was obtained from the caregiver of each child. Participants did not receive any incentives for taking part in the study.
Sleep Measure
The Chinese version of the Brief Infant Sleep Questionnaire (BISQ),31,32 adopted from a previous cross-cultural study,10 was used to measure a child's sleep quantity and quality. This widely used questionnaire has been validated against actigraphy and sleep logs, and includes specific questions about a child's daytime and nighttime sleep patterns. The child's primary caregiver was asked to complete BISQ based on the child's sleep characteristics during the previous 2 weeks before visiting the clinic, such as sleep duration, nighttime awakenings, and sleep practices (eg, bedroom sharing). Total sleep duration was calculated by summing daytime and nighttime sleep duration. Nighttime awakenings were assessed by the following two questions: (1) How often does your child awaken during the night? (2) On average, how long in total was your child awake during the night?
Developmental Assessment
General development of the young children between the age of 2 to 30 months was assessed with the Chinese version of the Bayley Scales of Infant Development (BSID-I). It is a standardized diagnostic test of cognitive and motor development used in children aged 2 to 30 months, which has been validated in mainland China in 1993.33 The Mental Development Index (MDI) derived from the BSID-I is an indicator of the level of a child's cognitive and language development. The Psychomotor Development Index (PDI) provides an estimate of a child's fine and gross motor abilities. A higher score on BSID-I suggests better performance. The mean and standard deviation of BSID-I Chinese-adjusted norms are 100 and 16, respectively. The original psychometric reliability calculated by the Spearman-Brown prediction formula was 0.73–0.97 for MDI and was 0.67–0.97 for PDI. All assessments were conducted by well-trained pediatricians and the approximate duration of the assessment was 45 to 60 minutes. Interrater reliability as measured by kappa analysis had to reach 80% for all the pediatricians in the training phase before proceeding to the assessment phase of this study. Pediatricians conducted the BSID-I as part of a comprehensive assessment with the children in the study, which also included a physical examination and laboratory tests. To avoid assessor bias, they were not informed of specific study hypotheses at the time of conducting the assessments with the participating families.
Sociodemographic Information
Shanghai Children's Medical Center Socio-Demographic Questionnaire was used to collect demographic information, such as parental age, parental education level, birth condition, and feeding patterns.
Statistical Analyses
An initial examination of the data was performed to test for normality and outliers. Independent t tests and Mann-Whitney U tests were conducted to compare sleep duration and frequency of nighttime awakenings between infants (aged 2 to 11 months) and toddlers (aged 12 to 30 months). In light of the substantial changes of the sleep development in early years,34,35 further analyses were subsequently conducted separately for the two age groups: infants aged 2 to 11 months (n = 590), and toddlers aged 12 to 30 months (n = 512). Infants and toddlers were further divided into four groups for analyses according to their frequency of nighttime awakenings: no awakening, once per night (1×/night), twice per night (2×/night), and at least three times per night (≥ 3×/night). Comparisons of the sociodemographic characteristics, sleep-related parenting practices (eg, bedroom sharing), and sleep duration across different frequency of nighttime awakening groups were performed using the χ2 test for discrete variables, and one-way analysis of variance (ANOVA) for continuous variables. The frequency of nighttime awakenings and the duration of nighttime awakenings were highly correlated with each other (rs = .65, P < .001); as such, nighttime awakening frequency was used as the main indicator of sleep quality and was included in the major analyses.
The associations between the frequency of nighttime awakenings and BSID-I scores (MDI and PDI) were tested by the analysis of covariance (ANCOVA) in which recruited provinces and the child's age and sex were adjusted. In addition, linear regression models were established separately for each age group (ie, infants and toddlers) to examine the associations between sleep parameters (eg, total sleep duration, frequency of nighttime awakenings) and MDI. In fully-adjusted models, total sleep duration and nighttime awakening frequency were entered as independent variables, and recruited provinces, child's age and sex, birth weight, maternal education level, bedroom sharing, and current feeding pattern (breastfeeding) were entered as covariates. Covariates were selected on the basis of preliminary univariate statistical results and the previous reports of the factors associated with cognitive development in young children (see Table S1 in the supplemental material).36,37
All analyses were performed using the Statistical Package for Social Sciences (SPSS) for Windows 22.0 (SPSS Inc., Chicago, Illinois, United States). The effect sizes of significant results were calculated and reported with the followings: Cohen d for t test, r for Pearson correlation, Cramér V for chi-square analysis, partial η2 for ANOVA and ANCOVA analysis, and ΔR2 for the linear regression analysis. The statistical significance level was set at .05.
RESULTS
Sample Characteristics
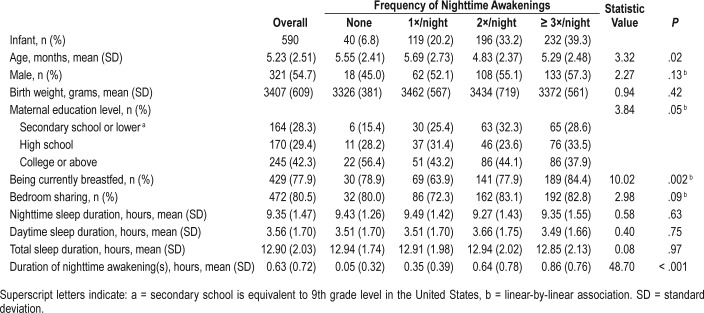
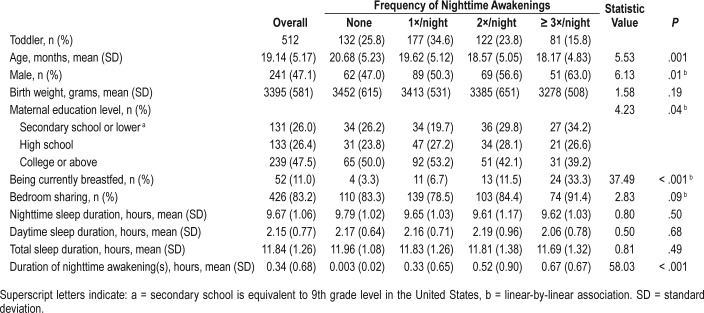
A total of 1,102 young children (590 infants and 512 toddlers) were recruited and assessed (mean age: 12.40 [standard deviation 8.13] months, 53.8% male). Sample characteristics of the recruited infants and toddlers are presented in Table 1 and Table 2. Approximately 69% of the infants obtained the recommended amount of daily sleep (12 to 16 h/d), and 80% of the toddlers slept for 11 to 14 h/d as recommended by the American Academy of Sleep Medicine.34 On average, infants slept longer during the day than toddlers (3.56 ± 1.70 versus 2.15 ± 0.77 hours, t = 17.97, d = 1.08, P < .001), but infants slept shorter during the night (9.35 ± 1.47 versus 9.67 ± 1.06 hours, t = −4.17, d = −0.25, P < .001). Infants had a longer total sleep duration as compared to toddlers (12.90 ± 2.03 versus 11.83 ± 1.26 hours, t = 10.49, d = 0.63, P < .001). Infants had more frequent nighttime awakenings than toddlers (2.19 ± 1.22 versus 1.28 ± 1.09×/night, t = 13.10, d = 0.79, P < .001), and the total duration of nighttime awakenings was longer in infants as compared to toddlers (0.63 ± 0.72 versus 0.34 ± 0.68 hours, log-transformed: t = 9.71, d = 0.59, P < .001).
Table 1.
Characteristics of infants (aged 2 to 11 months) with different frequency of nighttime awakenings.
Table 2.
Characteristics of toddlers (aged 12 to 30 months) with different frequency of nighttime awakenings.
The average MDI and PDI were 103.13 ± 17.12 and 101.97 ± 15.91, respectively. In the overall sample, lower MDI was associated with younger age (r = .23, P < .001), lower birth weight (r = .12, P < .001), lower maternal education level (F = 34.57, η2 = 0.19, P < .001), and being currently breastfed (t = 6.78, d = 0.42, P < .001); lower PDI was associated with lower birth weight (r = .10, P = .001) and lower maternal education level (F = 10.74, η2 = 0.19, P < .001). There were differences in MDI (F = 47.85, η2 = 0.23, P < .001) and PDI scores (F = 33.03, η2 = 0.17, P < .001) in the children recruited from different provinces (Table S1).
Prevalence and Correlates of Frequent Nighttime Awakenings
Prevalence of no nighttime awakening, and nighttime awakening(s) for 1×/night, 2×/night, and ≥ 3×/night was 6.8%, 20.2%, 33.2%, and 39.3% in infants, respectively. Table 1 shows the characteristics of sociodemographic features, current feeding pattern, sleep practice, and sleep duration among infants with different frequency of nighttime awakenings. Frequency of nighttime awakenings was significantly associated with younger age (η2 = 0.02, P = .02), lower maternal education level (V = 0.10, P = .05), and being currently breastfed (V = 0.18, P = .002) in infants.
Prevalence of no nighttime awakening, and nighttime awakening(s) for 1×/night, 2×/night and ≥ 3×/night was 25.8%, 34.6%, 23.8%, and 15.8% in toddlers, respectively. Table 2 shows the characteristics of sociodemographic features, current feeding pattern, sleep practice, and sleep duration among toddlers with different frequency of nighttime awakenings. Frequency of nighttime awakenings was significantly associated with younger age (η2 = 0.03, P = .001), being boys (V = 0.11, P = .01), lower maternal educational level (V = 0.10, P = .04), and being currently breastfed (V = 0.32, P < .001) in toddlers.
Association Between Sleep and Cognitive Functions
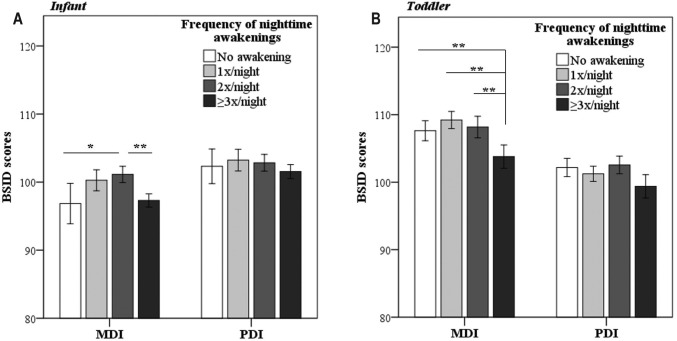
As shown in Figure 1A, the results of ANCOVA suggested that the frequency of nighttime awakenings was associated with MDI score (F = 3.00, partial η2 = 0.02, P = .03) but not PDI score (P > .05) among infants. Post hoc analysis indicated that infants with nighttime awakenings for 2×/night had higher MDI scores than those without nighttime awakening (P < .05) and those with more frequent nighttime awakenings (≥ 3×/ night) (P < .05). Figure 1B shows the comparison of BSID scores among toddlers with different frequency of nighttime awakenings. Higher frequency of nighttime awakenings (≥ 3×/ night) was related to lower MDI (F = 3.84, partial η2 = 0.02, P = .01) but not PDI (P > .05) in toddlers.
Figure 1. The comparisons of MDI score by different frequency of nighttime awakenings.
The comparisons of MDI score by different frequency of nighttime awakenings among infants (A) and toddlers (B). Error bars are standard error. Analysis of covariance (adjusted for recruited province, age and sex) and least significant difference post hoc analysis were conducted. Asterisks indicate statistical significance: * = P < .05, ** = P < .01. BSID = Bayley Scales of Infant Development, MDI = Mental Development Index, PDI = Psychomotor Development Index.
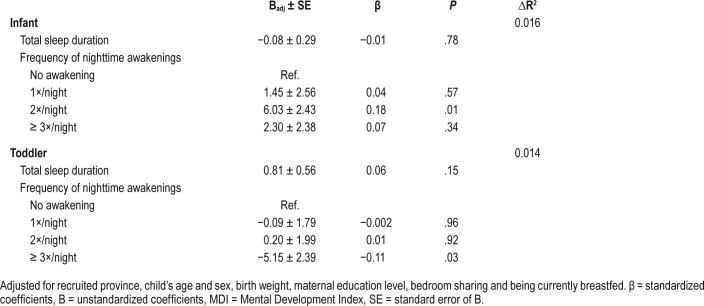
Results from linear regression analyses on the association between sleep characteristics and MDI are presented in Table 3. In the fully-adjusted model, nighttime awakenings for 2×/night were significantly associated with higher MDI in infants (P = .01, ΔR2sleep = 0.016), although this association was not observed for nighttime awakenings for ≥ 3×/night (P > .05). However, the analyses in the toddler group showed that nighttime awakenings for ≥ 3×/night were significantly associated with lower MDI (P = .03, ΔR2sleep = 0.014). Total sleep duration was not found to be associated with MDI in both infant and toddler samples.
Table 3.
Results of linear regression analyses on the association between sleep characteristics and MDI.
DISCUSSION
The current study provided community-based data on the prevalence and associated factors of reported nighttime awakenings in Chinese infants and toddlers. The findings showed an association between sleep quality as reflected by the frequency of nighttime awakenings and cognitive abilities in young children, with a distinct pattern found at different developmental stages. In particular, poorer cognitive performance was observed in toddlers with more frequent nighttime awakenings, whereas infants with modest frequency of night awakenings (about twice per night) showed better cognitive performance.
In line with the findings of a previous cross-cultural survey,10 our study showed that the average frequency of nighttime awakenings in Chinese young children (1.8×/night) was higher as compared to the figure (0.8×/night) reported by a recent review that included the studies conducted predominantly in white populations.38 The observed cultural difference in the reported frequency of nighttime awakenings might be due to some distinct sleep-related parenting practices, such as bedroom sharing, that are more common in Asian culture.10 Similar to other studies,28 we found that a marginally signifi-cant association between bedroom sharing and the frequency of reported nighttime awakenings in infants and toddlers. Although the exact causes of increased nighttime awakenings in young children in association with bedroom sharing remain unclear, there are several possible explanations that may account for this observation. It is possible that improper sleep-related parenting practices may have contributed to night waking problems in these young children. Meanwhile, sleep proximity could potentially affect the parental report of nighttime awakenings. Co-sleeping parents might be more likely to notice the movements of their child during sleep that were not necessarily suggestive of a waking state. It is also possible that co-sleeping parents might have more mental health difficulties or sleep problems themselves, which could potentially affect their child's sleep29 or might result in a biased evaluation of their child's sleep.39
In addition to co-sleeping, we found that young children who were currently breastfed were more likely to have more frequent nighttime awakenings. Nighttime awakenings in infants may naturally serve the adaptive functions for the child's need of feeding and seeking comfort during the night. However, the association between current breastfeeding and frequent nighttime awakenings might be modulated by other factors, such as improper parenting practices during nighttime breastfeeding (eg, nursing to sleep) that could hinder the development of the abilities required for the young children to fall asleep independently.40 In addition, some parents may assume breastfeeding to be a comforting behavior to facilitate their child's sleep.41 Although such a strategy is effective in reducing sleep latency in the short term, it may prevent young children from learning self-soothing skills to maintain self-regulated sleep at night.
Our study showed a distinct pattern of association between the frequency of nighttime awakenings and cognitive abilities in young children at different developmental stages. Interestingly, infants with modest frequency of nighttime awakenings were found to show better cognitive abilities than those rarely waking up during the night (ie, no nighttime awakening). This finding was in line with that of previous studies showing that neonates and young infants with reduced arousals or longer noninterrupted sleep period have slower brain development in their first year.42,43 Meanwhile, the association between frequent nighttime awakenings and poorer cognitive development was found in infants and toddlers after controlling for potential confounding influence of maternal education level on both cognitive performance and nighttime awakenings. Sleep consolidation is an age-dependent process that develops throughout the first few years of life.44–46 When children grow older, they are expected to gradually develop the ability to maintain self-regulated sleep throughout the night, along with the well-established attachment and mature self-soothing skills.47 As a result, the frequency of nighttime awakenings is expected to decrease significantly with increasing age.31,48 A previous study conducted in Chinese preschoolers has also found that preschoolers with behavioral sleep problems (eg, difficulty maintaining sleep, bedtime resistance) had lower total IQ scores.49 In this regard, it is possible that sleep fragmentation and poor sleep quality as reflected by frequent nighttime awakenings might lead to a neurocognitive decrement. Experimental studies using animal models have shown that chronic sleep fragmentation impairs hippocampal-dependent cognitive functions by reducing neurogenesis.50 From a clinical perspective, frequent nighttime awakenings are often found in young children with developmental concerns, such as autism and intellectual disability, which might potentially explain the findings in some toddlers.51,52 Nonetheless, there is a need for prospective follow-up studies to delineate the association between these developmental outcomes and frequent nighttime awakenings.
The current study did not find an association between total sleep duration and cognitive performance in infants and toddlers. This result was in line with that of previous studies conducted among young children, emphasizing the importance of other aspects of sleep in relation to cognitive development during this developmental stage. A previous study has shown that infants with better ultradian sleep regulation (eg, lower sleep fragmentation) had higher MDI scores.22 In addition, infants with better circadian sleep regulation (ie, higher proportion of nighttime sleep) have been found to perform better on executive function tasks.53 Another speculation of the insignificant association observed between sleep duration and cognitive performance might be because most of the young children in the current sample obtained the recommended amount of sleep.
The findings of this study provide a developmental context for the implications of nighttime awakenings in early years and underscore the need to address frequent nighttime awakenings particularly in toddlers. Although poor sleep may not be the only factor contributing to impaired cognitive functioning in young children, sleep problem is a potentially modifiable risk factor that can be the target for clinical intervention and prevention. In this regard, there has been some evidence to support the efficacy of behavioral treatment in improving nighttime awakenings in young children.54 Future longitudinal studies are needed to investigate the effects of age-appropriate sleep-focused intervention on the cognitive development in young children.
The main strengths of our study included the recruitment of a large number of low-risk young children from the community, and the formal assessment of a child's cognitive abilities by clinicians using a standardized test, instead of the parent-reported questionnaires. Meanwhile, the findings of this study should be considered in light of several limitations. First, the sleep assessment in this study was based on the parental report. Future studies should incorporate objective measures (eg, actigraphy, video or polysomnographic recordings) to corroborate subjective reports. In a previous study conducted in 10-month-old infants, although the parental report of nighttime awakenings was not related to lower MDI, nighttime awakenings as measured by actigraphy were shown to be negatively associated with cognitive function.22 Second, the current study was limited by its cross-sectional design, which precluded the inference of causal relationship. Further studies are warranted to delineate the causal factors associated with frequent nighttime awakenings in young children and to further explore the potential mechanisms underlying the association between frequent nighttime awakenings and poor cognitive development. Third, some of the factors that might confound the association between sleep and cognitive abilities were not measured in this study, such as parent-child interactions, maternal mental health, parental knowledge of children's sleep patterns, and parental smoking, as well as other environmental factors. Finally, the objective assessment of a child's cognitive abilities was based on an older version of the BSID, which was the only version with well-established norms available in the Chinese population. Future studies should adopt other validated, standardized assessment tools to further explore specific cognitive functions that may be affected by sleep during early child development.
In conclusion, our study showed a distinct pattern of association between nighttime awakenings and cognitive performance in young children. During the first year of life, nighttime awakenings with varied frequency are common as reported across different studies.55,56 However, to the authors' knowledge, this is the first study, albeit with a cross-sectional design, to show the developmental implication of nighttime awakenings, particularly on cognitive abilities, in young children. Future longitudinal studies are warranted to further examine the developmental outcomes in relation to nighttime awakenings in young children. Further research is also needed to explore the effects of parent-based, sleep-focused educational intervention in the community on children's early development.
DISCLOSURE STATEMENT
The work was performed in Shanghai Children's Medical Center in collaboration with Shijiazhuang City Maternal and Child Health Hospital (Hebei), Shijiazhuang Qiaodong Maternal and Child Health Station (Hebei), Yiwu City Maternal and Child Health Hospital (Zhejiang), Yiwu Choucheng Health Center (Zhejiang), Rizhao Juxian People's Hospital (Shandong), Rizhao City People's Hospital (Shandong), Hongze County Maternal and Child Health Hospital (Jiangsu), Huai'an City Maternal and Child Health Hospital (Jiangsu), Kunming Children's Hospital (Yunnan), Inner Mongolia Maternal and Child Health Hospital (Inner Mongolia), Liuyang City Maternal and Child Health Hospital (Hunan), Liuyang Gugang Health Center (Hunan), Nandan County Maternal and Child Health Hospital (Guangxi), and Guangxi Autonomous Region Maternal and Child Health Hospital (Guangxi). All the authors have seen and approved the manuscript. The authors report no conflicts of interest. The study was supported by the Chinese National Natural Science Foundation (81422040, 81172685); MOE New Century Excellent Talents (NCET-13-0362); Ministry of Science and Technology (2010CB535000); Shanghai Science and Technology Commission (12411950405, 14441904004, 13QH1401800, 2016YFC1305203); Shanghai Municipal Committee of Education (D1502); The fourth round of Three-Year Public Health Action Plan (2015-2017) (GWIV-36). All funding was awarded to Dr. Fan Jiang. The funding body had no role in the conception, design, conduct, interpretation, or analysis of the study or in the approval of the publication.
ACKNOWLEDGMENTS
The authors thank the children and their families for their participation and the 16 hospitals in the eight provinces for facilitating the recruitment of this study. We appreciate Dr. Chingfan Sheu from the Institute of Education, National Cheng Kung University, Taiwan for his advice on data analysis.
ABBREVIATIONS
- BSID-I
Bayley Scales of Infant Development
- MDI
Mental Development Index
- PDI
Psychomotor Development Index
REFERENCES
- 1.Jiang F, VanDyke RD, Zhang J, Li F, Gozal D, Shen X. Effect of chronic sleep restriction on sleepiness and working memory in adolescents and young adults. J Clin Exp Neuropsychol. 2011;33(8):892–900. doi: 10.1080/13803395.2011.570252. [DOI] [PubMed] [Google Scholar]
- 2.Randazzo A, Muehlbach M, Schweitzer P, Walsh J. Cognitive function following acute sleep restriction in children ages 10-14. Sleep. 1998;21(8):861–868. [PubMed] [Google Scholar]
- 3.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;74(2):444–455. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 4.Lo JC, Ong JL, Leong RLF, Gooley JJ, Chee MWL. Cognitive performance, sleepiness, and mood in partially sleep deprived adolescents: the need for sleep study. Sleep. 2015;39(3):687–698. doi: 10.5665/sleep.5552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van Someren EJW. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychol Bull. 2012;138(6):1109–1138. doi: 10.1037/a0028204. [DOI] [PubMed] [Google Scholar]
- 6.Touchette E, Petit D, Séguin JR, Boivin M, Tremblay RE, Montplaisir JY. Associations between sleep duration patterns and behavioral/cognitive functioning at school entry. Sleep. 2007;30(9):1213–1219. doi: 10.1093/sleep/30.9.1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tso W, Rao N, Jiang F, et al. Sleep duration and school readiness of chinese preschool children. J Pediatr. 2016;169(743413):266–271. doi: 10.1016/j.jpeds.2015.10.064. [DOI] [PubMed] [Google Scholar]
- 8.Spruyt K, Aitken RJ, So K, Charlton M, Adamson TM, Horne RSC. Relationship between sleep/wake patterns, temperament and overall development in term infants over the first year of life. Early Hum Dev. 2008;84(5):289–296. doi: 10.1016/j.earlhumdev.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Bernier A, Beauchamp MH, Bouvette-Turcot AA, Carlson SM, Carrier J. Sleep and cognition in preschool years: specific links to executive functioning. Child Dev. 2013;84(5):1542–1553. doi: 10.1111/cdev.12063. [DOI] [PubMed] [Google Scholar]
- 10.Mindell J, Sadeh A, Wiegand B, How T, Goh D. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010;11(3):274–280. doi: 10.1016/j.sleep.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Sadeh A, Mindell J, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2011;12(5):478–482. doi: 10.1016/j.sleep.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics. 2012;129(2):e276–e284. doi: 10.1542/peds.2011-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baird J, Hill C, Kendrick T, Inskip H. Infant sleep disturbance is associated with preconceptional psychological distress: findings from the Southampton Women's Survey. Sleep. 2009;32(4):566–568. doi: 10.1093/sleep/32.4.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaylor E, Goodlin-Jones B, Anders T. Classification of young children's sleep problems: a pilot study. J Am Acad Child Adolesc Psychiatry. 2001;40(1):61–67. doi: 10.1097/00004583-200101000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Galbally M, Lewis AJ, McEgan K, Scalzo K, Islam FA. Breastfeeding and infant sleep patterns: an Australian population study. J Paediatr Child Health. 2013;49(2):e147–e152. doi: 10.1111/jpc.12089. [DOI] [PubMed] [Google Scholar]
- 16.Anuntaseree W, Mo-suwan L, Vasiknanonte P, Kuasirikul S, Ma-a-lee A, Choprapawan C. Night waking in Thai infants at 3 months of age: association between parental practices and infant sleep. Sleep Med. 2008;9(5):564–571. doi: 10.1016/j.sleep.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 17.Chou YH. Survey of sleep in infants and young children in northern Taiwan. Sleep Biol Rhythm. 2007;5(1):40–49. [Google Scholar]
- 18.Jiang F, Shen X, Yan C, et al. Epidemiological study of sleep characteristics in Chinese children 1-23 months of age. Pediatr Int. 2007;49(6):811–816. doi: 10.1111/j.1442-200X.2007.02449.x. [DOI] [PubMed] [Google Scholar]
- 19.Velten-Schurian K, Hautzinger M, Poets CF, Schlarb AA. Association between sleep patterns and daytime functioning in children with insomnia: the contribution of parent-reported frequency of night waking and wake time after sleep onset. Sleep Med. 2010;11(3):281–288. doi: 10.1016/j.sleep.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Turnbull K, Reid GJ, Morton JB. Behavioral sleep problems and their potential impact on developing executive function in children. Sleep. 2013;36(7):1077–1084. doi: 10.5665/sleep.2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ednick M, Cohen A, McPhail G. A review of the effects of sleep during the first year of life on cognitive, psychomotor, and temperament development. Sleep. 2009;32(11):1449–1458. doi: 10.1093/sleep/32.11.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scher A. Infant sleep at 10 months of age as a window to cognitive development. Early Hum Dev. 2005;81:289–292. doi: 10.1016/j.earlhumdev.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Piteo AM, Kennedy JD, Roberts RM, et al. Snoring and cognitive development in infancy. Sleep Med. 2011;12(10):981–987. doi: 10.1016/j.sleep.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 24.Piteo AM, Lushington K, Roberts RM, et al. Parental-reported snoring from the first month of life and cognitive development at 12 months of age. Sleep Med. 2011;12(10):975–980. doi: 10.1016/j.sleep.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 25.Krakowiak P, Goodlin-Jones B, Hertz-Picciotto I, Croen LA, Hansen RL. Sleep problems in children with autism spectrum disorders, developmental delays, and typical development: a population-based study. J Sleep Res. 2008;17(2):197–206. doi: 10.1111/j.1365-2869.2008.00650.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jenni OG, O'Connor BB. Children's sleep: an interplay between culture and biology. Pediatrics. 2005;115(1 Suppl):204–216. doi: 10.1542/peds.2004-0815B. [DOI] [PubMed] [Google Scholar]
- 27.Mindell JA, Sadeh A, Kohyama J, Hwei T. Parental behaviors and sleep outcomes in infants and toddlers: A cross-cultural comparison. Sleep Med. 2010;11(4):393–399. doi: 10.1016/j.sleep.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 28.Volkovich E, Ben-Zion H, Karny D, Meiri G, Tikotzky L. Sleep patterns of co-sleeping and solitary sleeping infants and mothers: a longitudinal study. Sleep Med. 2015;16(11):1305–1312. doi: 10.1016/j.sleep.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 29.Teti DM, Crosby B. Maternal depressive symptoms, dysfunctional cognitions, and infant night waking: the role of maternal nighttime behavior. Child Dev. 2012;83(3):939–953. doi: 10.1111/j.1467-8624.2012.01760.x. [DOI] [PubMed] [Google Scholar]
- 30.Meng Q, Xu L, Zhang Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–814. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- 31.Sadeh A, Mindell JA, Luedtke K, Wiegand B. Sleep and sleep ecology in the first 3 years: A web-based study. J Sleep Res. 2009;18(1):60–73. doi: 10.1111/j.1365-2869.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 32.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–e577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 33.Huang H, Tao SD, Xu JD, et al. Standardization of Bayley Scales for Infant Development in Shanghai. Chin J Child Heal. 1993;1(3):158–160. [Google Scholar]
- 34.Paruthi S, Brooks LJ, Ambrosio CD, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. doi: 10.5664/jcsm.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Heal. 2015;1(4):233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 36.Dee DL, Li R, Lee LC, Grummer-Strawn LM. Associations between breastfeeding practices and young children's language and motor skill development. Pediatrics. 2007;119(Suppl 1):S92–S98. doi: 10.1542/peds.2006-2089N. [DOI] [PubMed] [Google Scholar]
- 37.Barajas RG, Martin A, Brooks-Gunn J, Hale L. Mother-child bed-sharing in toddlerhood and cognitive and behavioral outcomes. Pediatrics. 2011;128(2):e339–e347. doi: 10.1542/peds.2010-3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 2012;16(3):213–222. doi: 10.1016/j.smrv.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 39.Goldberg WA, Lucas-Thompson RG, Germo GR, Keller MA, Davis EP, Sandman CA. Eye of the beholder? Maternal mental health and the quality of infant sleep. Soc Sci Med. 2013;79:101–108. doi: 10.1016/j.socscimed.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ramamurthy MB, Sekartini R, Ruangdaraganon N, Huynh DHT, Sadeh A, Mindell JA. Effect of current breastfeeding on sleep patterns in infants from Asia-Pacific region. J Paediatr Child Health. 2012;48(8):669–674. doi: 10.1111/j.1440-1754.2012.02453.x. [DOI] [PubMed] [Google Scholar]
- 41.Paul IM, Savage JS, Anzman-Frasca S, Marini ME, Mindell JA, Birch LL. INSIGHT responsive parenting intervention and infant sleep. Pediatrics. 2016;138(1):e20160762. doi: 10.1542/peds.2016-0762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anders TF, Keener M. Developmental course of nighttime sleep-wake patterns in full-term and premature infants during the first year of life. Sleep. 1985;8(3):173–192. doi: 10.1093/sleep/8.3.173. [DOI] [PubMed] [Google Scholar]
- 43.Scher MS, Steppe DA, Banks DL. Prediction of lower developmental performances of healthy neonates by neonatal EEG-sleep measures. Pediatr Neurol. 1996;14(2):137–144. doi: 10.1016/0887-8994(96)00013-6. [DOI] [PubMed] [Google Scholar]
- 44.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111(2):302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 45.Louis J, Cannard C, Bastuji H, Challamel MJ. Sleep ontogenesis revisited: a longitudinal 24-hour home polygraphic study on 15 normal infants during the first two years of life. Sleep. 1997;20(5):323–333. doi: 10.1093/sleep/20.5.323. [DOI] [PubMed] [Google Scholar]
- 46.Scher A. Continuity and change in infants' sleep from 8 to 14 months: a longitudinal actigraphy study. Infant Behav Dev. 2012;35(4):870–875. doi: 10.1016/j.infbeh.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 47.Henderson JMT, France KG, Blampied NM. The consolidation of infants' nocturnal sleep across the first year of life. Sleep Med Rev. 2011;15(4):211–220. doi: 10.1016/j.smrv.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 48.Scher A, Epstein R, Tirosh E. Stability and changes in sleep regulation: a longitudinal study from 3 months to 3 years. Int J Behav Dev. 2004;28(3):268–274. [Google Scholar]
- 49.Liu J, Zhou G, Wang Y, Ai Y, Pinto-Martin J, Liu X. Sleep problems, fatigue, and cognitive performance in Chinese kindergarten children. J Pediatr. 2012;161(3):520.e2–525.e2. doi: 10.1016/j.jpeds.2012.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sportiche N, Suntsova N, Methippara M, et al. Sustained sleep fragmentation results in delayed changes in hippocampal-dependent cognitive function associated with reduced dentate gyrus neurogenesis. Neuroscience. 2010;170(1):247–258. doi: 10.1016/j.neuroscience.2010.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Souders MC, Mason TBA, Valladares O, et al. Sleep behaviors and sleep quality in children with autism spectrum disorders. Sleep. 2009;32(12):1566–1578. doi: 10.1093/sleep/32.12.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Didden R, Korzilius H, Van Aperlo B, Van Overloop C, De Vries M. Sleep problems and daytime problem behaviours in children with intellectual disability. J Intellect Disabil Res. 2002;46(7):537–547. doi: 10.1046/j.1365-2788.2002.00404.x. [DOI] [PubMed] [Google Scholar]
- 53.Bernier A, Carlson S. Relations between physiological and cognitive regulatory systems: infant sleep regulation and subsequent executive functioning. Child Dev. 2010;81(6):1739–1752. doi: 10.1111/j.1467-8624.2010.01507.x. [DOI] [PubMed] [Google Scholar]
- 54.Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A. Behavioral treatment of bedtime problems and night wakings in infants and young children - an American Academy of Sleep Medicine review. Sleep. 2006;29(10):1263–1276. [PubMed] [Google Scholar]
- 55.Moore T, Ucko C. Night waking in early infancy. Arch Dis Child. 1957;32:333–342. doi: 10.1136/adc.32.164.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scher A. A longitudinal study of night waking in the first year. Child Care Health Dev. 1991;17(5):295–302. doi: 10.1111/j.1365-2214.1991.tb00699.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.