Abstract
Exercise provides a wide range of health-promoting benefits, but support is limited for clinical programs that use exercise as a means of health promotion. This stands in contrast to restorative or rehabilitative exercise, which is considered an essential medical service. We propose that there is a place for ongoing, structured wellness and health promotion programs, with exercise as the primary therapeutic focus. Such programs have long-lasting health benefits, are easily implementable, and are associated with high levels of participant satisfaction. We describe the dissemination and implementation of a long-standing exercise and health promotion program, Gerofit, for which significant gains in physical function that have been maintained over 5 years of follow-up, improvements in well-being, and a 10-year 25% survival benefit among program adherents have been documented. The program has been replicated at 6 Veterans Affairs Medical Centers. The pooled characteristics of enrolled participants (n=691) demonstrate substantial baseline functional impairment (usual gait speed 1.05±0.3 m/s, 8-foot up and go 8.7±6.7 seconds, 30-second chair stands 10.7±5.1, 6-minute walk distance 404.31±141.9 m), highlighting the need for such programs. Change scores over baseline for 3, 6, and 12 months of follow-up are clinically and statistically significant (p<.05 all measures) and replicate findings from the parent program. Patient satisfaction ratings of high ranged from 88% to 94%. We describe the implementation process and present 1-year outcomes. We suggest that such programs be considered essential elements of healthcare systems.
Keywords: exercise, implementation, prevention, elderly, mobility
Physical activity decreases with age. Only 15% of adults aged 65 and older and 5% of those aged 85 and older report regular physical activity.1 A strong and substantial body of evidence linking low physical activity to poor health outcomes such death, functional limitations, disability, certain cancers, obesity, metabolic and cardiovascular disease, and cognitive impairment supports the significance of low physical activity.2, 3 Approximately 11% of aggregate healthcare expenditures may be due to inadequate levels of physical activity,4 supporting the importance of physical activity programs as an opportunity to transition from a disease-based to a wellness-based model of care.5–7
The Durham Veterans Affairs (VA) Medical Center (Durham, NC) has supported a long-standing exercise and health promotion program for older veterans called Gerofit. Gerofit targets individuals who, because of deconditioning, chronic disease, or use of assistive devices, are at risk of premature functional decline. Primary care providers refer program participants to attend a 3-day-per-week facility-based exercise program that offers structured exercise customized to individual health status and underlying impairments. Eligible participants must be aged 65 and older and able to function independently in a group setting. Inability to perform basic activities of daily living and transfers, oxygen dependency, unstable cardiac disease, and moderate to severe cognitive impairment are exclusion criteria. Each person is taught to self-manage an exercise program customized to his or her functional deficits that is aimed at improving function and making progress toward meeting national recommended guidelines.8 A functional assessment is conducted at baseline; 3, 6, and 12 months; and yearly thereafter. Staff works individually with each person to develop a personalized program that includes aerobic and strength training and group-based classes to improve mobility and balance, such as tai chi or dancing. Over its 30-year history, the program has reported participant outcomes, including physical function, sickness, quality of life, and survival.9–14 Physical gains are maintained for 2 to 3 years after enrollment; at 5-year follow-up, individuals remain above or near baseline levels and have essential compression of morbidity, which may delay the need for institutional or assistive care for 5 years.14 When asked about the effect of the program, a long-term (≥20 years) 95-year-old participant (still living in the community) stated, “If it were not for this program, I don’t think we would be walking at all (talking about herself and her 97-year old veteran spouse).” Despite robust programmatic outcomes, funding for dissemination for this program did not exist until the Veterans Health Administration (VHA) initiated a transformation in the delivery of healthcare, emphasizing a wellness approach to care. With this initiative, 6 medical centers, 4 in Year 1 and 2 in Year 2, implemented Gerofit in their facilities. This objective of this article is to describe the Gerofit implementation process, characteristics of participating veterans at the new sites, and program outcomes for each new site; compare outcomes with outcomes of the parent Durham VA Gerofit program; and compare outcomes of rural- and urban-based medical centers.
METHODS
Implementation Process
Under the VHA system, wide “transformation to a 21st century healthcare system,” funding was made available to pilot innovative alternatives to nursing homes. The Gerofit program secured funding for dissemination as a model of care promoting attenuation of functional decline of veterans, who because of their sedentary lifestyle, were deemed at high risk of institutionalization. Initial eligibility criteria for program implementation required that partner sites be ready for rapid implementation by having committed personnel available for the program with a research or clinical background in geriatric exercise, access to a gym or space that could be used for exercise programming, and a commitment of support from facility leadership. The goal was to enroll 30 new people in the program at each site with sufficient time to obtain 3-month follow-up data on program participants by the end of the first year. The application process to apply for such funding was time sensitive. During the first round of applications, only 4 (Baltimore, MD; Canandaigua, NY; Los Angeles, CA; Miami, FL) of 13 potential sites obtained the required letters of support within the required timeframe.
Costs
Each site received $179,000 in start-up funds, allocated as follows: $135,000 for 1.5 personnel staffing, $30,000 for equipment, $10,500 for supplies, $2,500 for educational training costs, and $1,500 for a site visit to the Durham VA. Projected second-year costs would be similar minus the $30,000 in equipment funds. Each site contributed additional donated personnel time that varied according to site.
Implementation followed a structured approach beginning with weekly and then every-other-week group telephone conferences for planning purposes. A website for sharing materials was developed. The initial months focused on sharing the clinical and administrative infrastructure necessary to set up a new program. Standardized templates and operative procedures were posted on the website along with short videos demonstrating each process with step-by-step instructions. Four months after funding, members from each site traveled to the Durham VA for an intensive 2-day training site visit. The training visit began with a visit to the Gerofit program during which site visitors were partnered with various Gerofit program participants and performed their exercise routines with them. See https://www.youtube.com/watch?v=Ws6Imgq54QU for a short video documenting the partnered visit. The balance of the site visit centered on training in functional assessments, scoring and performing chart reviews, mock team presentations of reviewed consultations, and evaluations of sample individuals referred to the program. A reverse site visit, Durham staff to each site, was scheduled within 1 to 2 months of initiation of participant enrollment to assess program fidelity to adherence to enrollment procedures, program content, functional assessments, data collection, and data tracking. The content of the reverse site visit typically included focused training to address deficits in program fidelity and formal presentations to staff or leadership promoting the new program to garner additional support from medical leadership and introduce the program to primary care and geriatric providers. The every-other-week telephone calls continued throughout the year and evolved into a “learning collaborative” in which each site contributed and shared experiences that benefitted other sites. A second year of funding was obtained to increase dissemination (Salem, VA and Honolulu, HI VA Medical Centers).
Statistical Analysis
Each site was given a database for storing and tracking program-related data that was stored behind their medical center firewalls for data security. Data were downloaded and shared in a password-protected website, for pooling of data. Analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary NC). Descriptive statistics of baseline characteristics at each site include means and standard deviations for continuous variables and percentages for categorical variables. Changes in physical function between 3 testing time points (3, 6, 12 months) and baseline were examined using the 5 new sites (except Durham). Baseline data and data for specific testing time points were regarded as paired observations. T-tests were used to test whether mean changes in physical function were significantly different from 0 with control for baseline of the outcome of interest. In addition, a t-test was used to determine whether the mean of 3-, 6-, and 12-month changes in physical function in Durham differed significantly from the mean changes in new sites. The t-test was also applied to compare the means of 3-, 6-, and 12-month changes in physical function between rural and urban sites. We also examined the linear trend of overall patterns of change in physical function over time, in which time from baseline was treated as a continuous independent variable. Repeated-measures analyses were conducted across 3 testing time points (3, 6, 12 months). The dependent variable is the difference in physical function between the specific testing time point and baseline. We used 4 models for each outcome; the first adjusted for baseline value of the outcome, the second adjusted for baseline value and age, the third adjusted for baseline value and body mass index, and the fourth model adjusted for baseline value and site.
RESULTS
Implementation was considered highly successful, with all but one site meeting or exceeding initial enrollment targets and reporting high levels of participant and provider satisfaction. One site did not use the database and did not meet program fidelity metrics, and participant outcomes were not available for this report. Baseline characteristics of participants across the country largely mirrored the baseline profile of the Durham Gerofit program participants, whose baseline functional data score below norms for healthy, older, community-dwelling adults (Table 1). On average, the baseline gait speed (1.05 m/s) of program participants was very close to what is considered the cut point between healthy and impaired mobility.15 Other assessed parameters, 30-second chair stands, 8-foot up and go, and 6-minute walk time, were between the 10th and 25th percentiles of age-based norms, indicating substantial functional impairment and low likelihood of reaching age 90 without dependency.16, 17 Self-reported levels of satisfaction indicated that most program participants were highly satisfied with the program, with 93% of participants reporting high satisfaction at 3 months, 88% at 6 months, and 94% at 12 months. There were no differences in attrition between the new sites overall and the Durham site for either wave of data collection.
Table 1.
Enrollment, Baseline Characteristics, and Functional Profile of Enrolled Veterans from Durham and Newly Developed Sites, and Adherence over Time
| Durham | Overall New Sites | Baltimore | Greater Los Angeles | Honolulu | Canandaigua (Rural) | Salem (Rural) | |
|---|---|---|---|---|---|---|---|
| Consultations | 571 | 1,190 | 480 | 129 | 85 | 347 | 149 |
| Not eligible | 49 | 256 | 162 | 1 | 16 | 46 | 31 |
| Not interested | 161 | 230 | 66 | 35 | 18 | 91 | 20 |
| Home counsel | 81 | 13 | 0 | 0 | 6 | 4 | 3 |
| Enrolled | 280 | 691 | 252 | 93 | 45 | 206 | 95 |
| Age, mean±SD (range) | 73.0±6.8 (65–93) | 75.2±8.2 (65–98) | 72.5±6.6 (65–95) | 79.7±9.7 (65–98) | 80.0±7.7 (66–92) | 75.5±8.4 (65–97) | 75.2±7.2 (66–92) |
| Caucasian, % | 59.2 | 55.8 | 30.3 | 59.3 | 15.6 | 85.4 | 74.7 |
| Male. % | 97.5 | 96.4 | 96.4 | 96.8 | 97.8 | 96.1 | 95.8 |
| Body mass index, kg/m2, mean±SD | 30.7±5.8 | 30.8±5.9 | 31.5±6.0 | 30.6±6.9 | 26.8±4.9 | 31.3±5.5 | 30.0±5.0 |
| Gait speed, m/s, mean±SD | 1.08±0.3 | 1.05±0.3 | 1.04±0.3 | 0.96±0.3 | 0.89±0.3 | 1.14±0.3 | 1.03±0.2 |
| Number of 30-second chair stands, mean±SD | 10.9±4.7 | 10.7±5.1 | 11.2±5.0 | 8.4±4.8 | 10.0±5.5 | 11.4±5.6 | 10.2±3.4 |
| Six-minute walk, m, mean±SD | 448.0±139.0 | 381.1±133.7 | 406.0±142.2 | 340.7±147.8 | 324.8±142.3 | 438.8±133.2 | 426.7±145.0 |
| 8-foot up and go, seconds, mean±SD | 8.1±7.3 | 8.7±6.7 | 8.6±5.0 | 10.7±6.9 | 11.3±10.3 | 8.2±8.3 | 7.0±3.1 |
| Adherence over timea | |||||||
| Total 3-month sample, n | 276 | 622 | 230 | 188 | 37 | 83 | 84 |
| Active, n (%) | 154 (55.8) | 332 (53.4) | 116 (50.4) | 86 (45.7) | 24 (64.9) | 44 (53) | 62 (73.8) |
| Total 6-month sample, n | 268 | 543 | 203 | 175 | 21 | 76 | 68 |
| Active, n (%) | 127 (47.4) | 233 (42.9) | 81 (39.9) | 68 (38.9) | 10 (47.6) | 28 (36.8) | 46 (67.7) |
Because of rolling enrollment of participants, total sample was calculated for each individual based upon date of enrollment and of assessment wave. Some participants did not have enough time in the program to reach a particular wave (e.g., 3 month, 6 month) of assessment. Adherence status was calculated based whether a participant was active in the program for a particular wave of assessment and at least one subsequent assessment. As a consequence, activity status for the 12-month assessment is not available because data collection for this article did not go beyond 12 months. There were no significant differences in adherence rates between the new sites overall and Durham. Individual adherence site comparisons were not conducted.
SD=standard deviation.
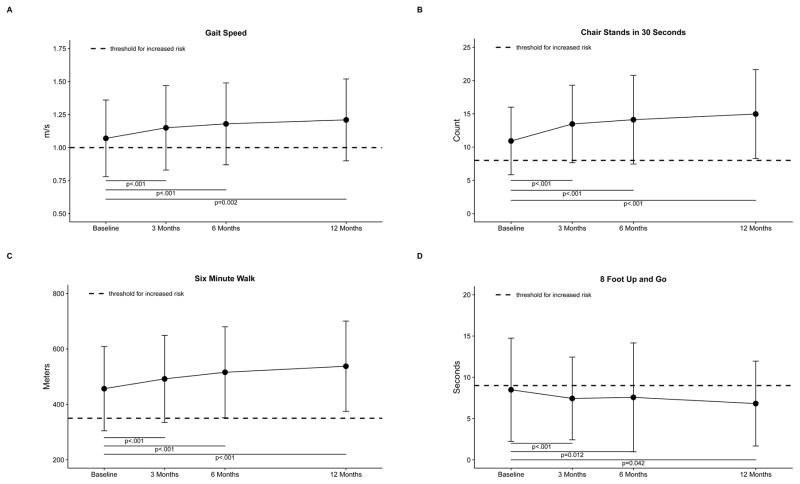
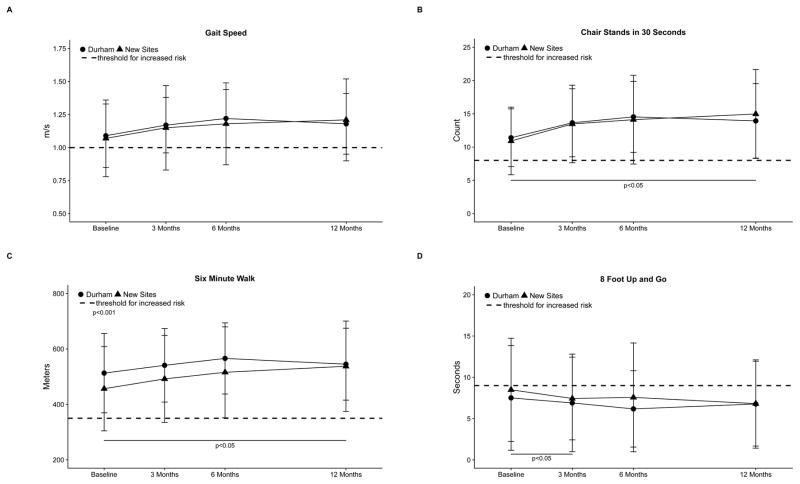
Figure 1 describes change in physical function over time. Because enrollment is ongoing, and each site is at a different stage of implementation, we limited these data to individuals who had a baseline assessment and at least one follow-up score. Change scores from baseline through 1-year follow-up indicated a significant improvement over time for each functional task in newly implemented site participants. Normal gait speed over 10 m had increased 0.08±0.2 m/s at the 3-month follow-up and remained stable over 6 and 12 months of follow-up, whereas 30-second chair stands and 6-minute walk distance showed continued improvement at each testing interval. We also examined overall patterns of change over time and found that, a test for trend was significant for 8-foot up and go (p=.02). Figure 2 highlights the differences between Durham outcomes and those of the new programs. Reported changes over time were largely similar at each wave of testing for each outcome assessed except for the 3-month follow-up for the 8-foot up and go test and the 12-month follow-up for the 30-second chair stand and 6-minute walk, on which new programs performed better than the Durham program. There were no significant differences in tests for change over time between Durham and the new sites for any intervals tested.
Figure 1.
Change from baseline at 3, 6, and 12 months in (A) usual gait speed, (B) number of chair stands completed in 30 seconds, (C) 6-minute walk distance, and (D) 8-foot up and go test. The dotted line indicates a threshold for high risk of loss of independence for the sex and mean age of the study sample. Above the line indicates better function except for the 8-foot up and go test. Models were limited to participants with baseline and at least one follow-up and included control for the baseline value of variable of interest. Sample sizes were n=366 at baseline and n=294, n=213, and n=128 for each successive time point. Some sites did not have time to accrue participants for the 12-month follow-up. P-values are shown for change from baseline.
Figure 2.
Differences between baseline and change from baseline at 3, 6, and 12 months between the Durham Veterans Affairs parent site and the new programs combined for (A) usual gait speed, (B) number of chair stands completed in 30 seconds, (C) 6-minute walk distance, and (D) 8-foot up and go test. The dotted line indicates a threshold for high risk of loss of independence for the sex and mean age of the study sample. Above the line indicates better function except for the 8 foot up and go test. Models were limited to participants with baseline and at least one follow-up and included control for the baseline value of variable of interest. Samples sizes were n=163 at baseline for Durham and n=127, n=106, and n=84 for each successive timepoint and n=336 at baseline for all other sites combined and n=294, n=213, and n=128 for each successive timepoint. Some sites did not have time to accrue participants for 12-month follow-up. P-values are shown for the difference between Durham and all other sites at each timepoint.
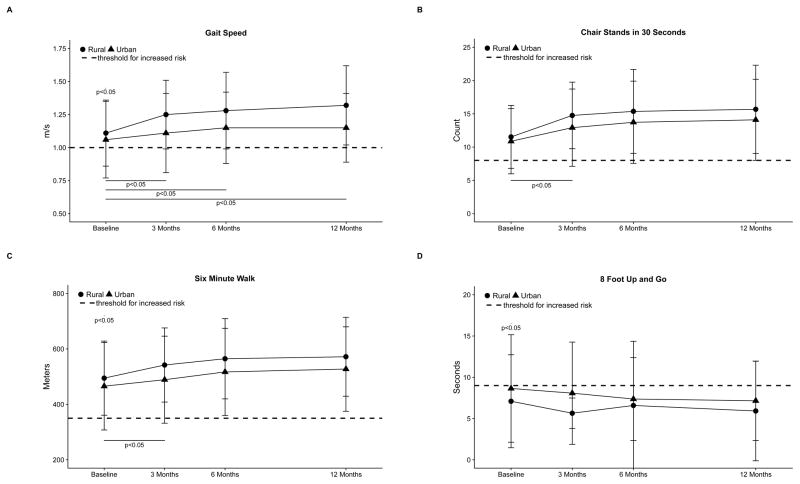
Facility-based implementation in medical centers in counties considered largely rural (Salem, VA; Canandaigua, NY) was equally successful, with programs able to reach or exceed enrollment targets. At baseline (Figure 3), urban-living veterans performed significantly worse than rural-living veterans on gait speed (1.06 vs 1.11 m/s, p=.049), 6-minute walk (438 vs 495 m, p=.03), and 8-foot up and go (8.65 vs 7.04 seconds, p=.005) but not on chair stands. At 3 months, changes from baseline were greater for rural than urban veterans, but observed differences in change from baseline between rural and urban veterans attenuated over time, except for gait speed. Overall, all subgroups experienced changes over time, with no significant differences (interactions in the magnitude of change observed at any wave of testing between rural and urban veterans, controlling for baseline value, baseline value and age, baseline value and body mass index, or baseline value and site).
Figure 3.
Differences between baseline and change from baseline at 3, 6, and 12 months between program participants living in urban and rural sites for (A) usual gait speed, (B) number of chair stands completed in 30 seconds, (C) 6-minute walk distance, and (D) 8-foot up and go test. The dotted line indicates a threshold for high risk of loss of independence for the sex and mean age of the study sample. Above the line indicates better function except for the 8 foot up and go test. Models were limited to participants with baseline and at least one follow-up and included control for the baseline value of variable of interest. Samples sizes were n=348 at baseline and n=283, n=218, and n=150 for each successive timepoint for participants in urban settings and n=151 at baseline n=138, n=102, and n=62 for each successive timepoint for participants in rural settings. Some sites did not have time to accrue participants for 12-month follow-up. P-values are shown for the differences between urban and rural sites.
DISCUSSION
We have described the implementation and dissemination of a successful exercise- and health-promotion program for older veterans. Dissemination and implementation has been largely successful with regard to program replication, fidelity, and outcomes. We have every reason to believe that, over the long term, program participants will have better long-term outcomes such as delayed need for institutional care, compression of morbidity, sustained improved functional profile, lower mortality, and robust psychosocial outcomes documented by the Durham Gerofit program and others who are regularly physically active. 9–14,18 The positive group dynamic that permeates the Gerofit program is difficult to describe in words, and we encourage readers to hear testimonials from the veterans themselves, which can be accessed at http://www.va.gov/geriatrics/gerofit/gerofit_success_stories.asp.
We believe that medical systems largely neglect and underuse exercise as a therapeutic intervention. One problem is that exercise is often promoted for weight management or is equated with physical therapy; with little attention given to its many other benefits, which include preventing premature mortality, coronary heart disease, diabetes mellitus, and certain cancers.19 The Global Burden of Disease Study recently listed physical inactivity as the fifth leading cause of disease burden in North America20 and responsible for 9% of premature death globally, which is comparable with the number of deaths attributed to tobacco use.19, 21 A recent meta-analysis comparing exercise with drug interventions found comparable outcomes in terms of mortality benefits in the secondary prevention of heart disease, stroke rehabilitation, treatment of heart failure, and diabetes mellitus prevention.22 A notable omission in these disease-based reports is the importance of preservation of physical function and mobility as a means of preserving independence in late life. The data collected from these new programs suggest that many veterans aged 65 and older have poor functional mobility and are at high risk of losing independence before age 90. Because VA benefits include payment for institutionalization, it makes good sense for the VA to seek programs that can alter and enhance physical function.
We concur with a commentary on physical inactivity that “it is a mistake to view physical activity only in terms of its disease specific-benefits. The benefits of exercise and physical activity are far-reaching and extend beyond health.”19 Our preliminary analyses have focused on functional benefit. This differs from physical therapy, which focuses on addressing a specific disability rather than overall function and health maintenance. Each newly implemented program has subtle differences. For example, the Greater Los Angeles and Honolulu programs receive their participants from geriatric clinics and geriatric rehabilitation settings. As a consequence, these individuals are older and more functionally impaired at baseline, yet we found that all programs achieved significant improvements in all of the functional measures assessed and observed no differences in outcomes based on program site. This points to the wide-ranging potential for benefit from programs such as Gerofit.
We did not compare the potential benefits that accrued to Gerofit program participants with those of social interactions, well-being, and development of relationships and social connections because we did not measure these factors. Although other types of social programs may confer similar benefits, Gerofit has several components that particularly enhance the psychosocial aspects of the program. Of primary importance is that the program is for veterans who share a strong common bond. Another aspect of Gerofit that we believe to be unique is that there is no time limit on participation. This has allowed us to examine and publish long-term outcomes and contributes to the social interactions.13, 14 The third aspect of the program specific to geriatrics is that some of our older, long-term participants serve as positive role models. Gerofit helps some people realize that, at age 65 to 75, they may still have another 20 years of life expectancy and that being in good physical condition will enhance their own future overall well-being. They also have an opportunity to observe individuals with fairly marked disabilities and chronic conditions successfully engaged in health promotion. Finally, there is great informal therapeutic support for new-onset medical conditions. For any new diagnosis, such as newly diagnosed cancer, stroke, or a condition requiring surgery or complicated therapies, there is always someone in the program who has experienced a similar situation and is happy to share his or her story.
The VA has declared the Gerofit program a Best Practices program. One reason that the program has continued to garner support for dissemination is its cost relative to the 1-year cost of institutionalization for an individual. Sustainment costs of the program vary according to location and scope but are largely equivalent to the 1-year cost of institutionalization of 1 to 2 persons. As we extend our programs, we are developing and testing new programs targeting veterans living in rural areas. Rural veterans score below age-matched norms, report low rates of physical activity, and express interest in exercising to maintain functional health.23
Despite the many successes and positive outcomes, some of the newer programs struggle to obtain local funding to sustain these programs given constrained budgets. Institutional challenges were the most prevalent barriers during the implementation phase, whereas program sustainment is the most prevailing challenge. In addition, one site had a preexisting exercise program, and it was difficult to change the culture of that environment, with individuals reluctant to adopt a new approach to exercise. Although promising, these data must be interpreted with caution because they are purely observational, with no comparison group; nor did we perform a formal cost analysis or analyses comparing dropouts with those who remain in the program. Our drop-out rates are on par with what has been reported in the literature for older adults (~50%) but higher than those reported for randomized trials.24–26 Our sample includes a higher percentage of non-Caucasians and individuals with high functional burden, both of which are typically associated with high attrition, than what is typically found for these types of programs.24 Finally, the majority of program participants were male; we do not know whether these findings would be similar for women.
In conclusion, we have described a highly successful exercise program for older veterans. These findings support the investment of VA-based health promotion programs that promote regular, structured, supported physical activity for older adults. Other integrated systems, for example Kaiser Permanente and health systems in Europe, have found similar population benefits. The implementation of health promotion programs in fee-for-service healthcare markets or regions without universal health care may need a different implementation plan for serving the “third curve” in their efforts for population health improvement.5 Current practice relies heavily on individuals seeking out and committing to an exercise routine despite strong evidence that older adults are less likely to be physically active, less likely to begin an activity program in the later years of life, and even less inclined to do so if living in rural areas. Implementing Gerofit-like programs improves access and provides the necessary support for older adults to begin or re-engage in customized, monitored physical activity that can result in life-altering benefits for individuals and population health improvement that health systems today are aiming for. Older adults are the fastest-growing segment of the population and account for a high percentage of healthcare costs; the benefits of physical activity in this population outweigh barriers to investment in widespread implementation of health promotion.
Acknowledgments
We are indebted to the many veterans who have given us so much through their participation in Gerofit. We are extremely grateful to the VA Offices of Geriatrics and Extended Care, in particular Karen Massey, RN, Kenneth Shay, DDS, Richard Allman, MD, and Susan Lanen, MSN, RN, GNP-BC, BSPH, and the VA Office of Rural Health for their support in the Gerofit dissemination efforts. Many thanks to Katherine Hall, PhD, Joi Deberry, RN, and Matthew Peterson, PhD, from the Durham VA for their contributions to Gerofit dissemination and Lydia Paden, MS, for her contributions to the Baltimore program. We wish to thank Drs. Harvey Jay Cohen and Kenneth Schmader for their long-standing support of the Durham Gerofit program, in addition to the continued support from the executive leadership of the Durham VA Medical Center. We are thankful for the contributions of the many individuals who have worked with the Gerofit program since its initiation in 1986.
Footnotes
Conflict of Interest: None.
Author Contributions: MCM, CCL, SC, WMV, LK, JG, TK, HC, MM, KAO, TW, CJ, MP: implementation and dissemination of Gerofit program; data collection; concept, design, and review of manuscript. KMM, OI, PV, RS, JL: data collection, analysis, preparation and review of manuscript. JPB: review of manuscript. DP: interpretation of data, revision and preparation of materials for resubmission. All authors: final approval of manuscript submitted.
Sponsor’s role: The sponsors had no influence on or participation in the preparation of this manuscript.
Financial Disclosure: Gerofit dissemination has been funded by the VHA Office of Geriatrics and Extended Care Non-Institutional Long Term Care Funding and Mentored Partnership program and the VHA Office of Rural Health. The Gerofit program has been locally supported by the Durham VA Geriatric, Research, Education and Clinical Program. Dr. Morey is supported in part by Duke Older American Independence Center, National Institutes of Health, National Institute on Aging Grant AG028716. Part of the analyses and implementation findings was presented at the American Geriatrics Society Annual Meetings of 2015 and 2016 and at the Gerontological Society of America Annual Meeting of 2015.
References
- 1.Federal Interagency Forum on Aging-Related Statistics. Older Americans Update 2016: Key Indicators of Well-Being. Washington, DC: U.S. Government Printing Office; 2016. [Accessed August 15, 2017]. [on-line]. Available at https://agingstats.gov/docs/LatestReport/Older-Americans-2016-Key-Indicators-of-WellBeing.pdf. [Google Scholar]
- 2.U.S. Department of Health and Human Services. The Surgeon General’s Vision for a Healthy and Fit Nation. Rockville, MD: Office of the Surgeon General; 2010. [PubMed] [Google Scholar]
- 3.Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- 4.Carlson SA, Fulton JE, Pratt M, et al. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis. 2015;57:315–323. doi: 10.1016/j.pcad.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Washington AE, Coye MJ, Boulware LE. Academic health systems’ third curve: Population health improvement. JAMA. 2016;315:459–460. doi: 10.1001/jama.2015.18550. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization Regional Office for Europe. [Accessed August 15, 2017];Health Promotion in Hospitals: Evidence and Quality Management. 2005 May; [on-line]. Available at http://www.euro.who.int/__data/assets/pdf_file/0008/99827/E86220.pdf.
- 7.Boyle PA, Buchman AS, Wilson RS, et al. Physical activity is associated with incident disability in community-based older persons. J Am Geriatr Soc. 2007;55:195–201. doi: 10.1111/j.1532-5415.2007.01038.x. [DOI] [PubMed] [Google Scholar]
- 8.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 9.Cowper PA, Morey MC, Bearon LB, et al. The impact of supervised exercise on psychological well-being and health status in older veterans. J Appl Gerontol. 1991;10:469–485. doi: 10.1177/073346489101000408. [DOI] [PubMed] [Google Scholar]
- 10.Morey M, Crowley G, Robbins M, et al. The Gerofit program: A VA innovation. South Med J. 1994;87:S83–S87. [PubMed] [Google Scholar]
- 11.Morey MC, Cowper PA, Feussner JR, et al. Evaluation of a supervised exercise program in a geriatric population. J Am Geriatr Soc. 1989;37:348–354. doi: 10.1111/j.1532-5415.1989.tb05503.x. [DOI] [PubMed] [Google Scholar]
- 12.Morey MC, Cowper PA, Feussner JR, et al. Two-year trends in physical performance following supervised exercise among community-dwelling older veterans. J Am Geriatr Soc. 1991;39:986–992. doi: 10.1111/j.1532-5415.1991.tb04045.x. [DOI] [PubMed] [Google Scholar]
- 13.Morey MC, Pieper CF, Crowley GM, et al. Exercise adherence and ten year mortality in chronically ill older adults. J Am Geriatr Soc. 2002;50:1929–1933. doi: 10.1046/j.1532-5415.2002.50602.x. [DOI] [PubMed] [Google Scholar]
- 14.Morey MC, Pieper CF, Sullivan RJ, et al. Five-year performance trends for older exercisers: A hierarchical model of endurance, strength, and flexibility. J Am Geriatr Soc. 1996;44:1226–1231. doi: 10.1111/j.1532-5415.1996.tb01374.x. [DOI] [PubMed] [Google Scholar]
- 15.Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881–889. doi: 10.1007/s12603-009-0246-z. [DOI] [PubMed] [Google Scholar]
- 16.Rikli RE, Jones CJ. Functional fitness normative scores for community-residing older adults, ages 60–94. J Aging Phys Act. 1999;7:162–181. [Google Scholar]
- 17.Rikli RE, Jones CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53:255–267. doi: 10.1093/geront/gns071. [DOI] [PubMed] [Google Scholar]
- 18.Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: The evidence. Can Med Assoc J. 2006;174:801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das P, Horton R. Rethinking our approach to physical activity. Lancet. 2012;380:189–190. doi: 10.1016/S0140-6736(12)61024-1. [DOI] [PubMed] [Google Scholar]
- 20.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naci H, Loannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ. 2013;347:f5577. doi: 10.1136/bmj.f5577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valencia W, Coleman N, Iglesias B, et al. Extending the reach of a successful exercise program to improve fitness in older Veterans. Gerontologist. 2015;55:4. [Google Scholar]
- 24.Picorelli AM, Pereira LS, Pereira DS, Felicio D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: A systematic review. J Physiother. 2014;60:151–156. doi: 10.1016/j.jphys.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 25.Linke SE, Gallo LC, Norman GJ. Attrition and adherence rates of sustained versus intermittent exercise interventions. Ann Behav Med. 2011;42:197–209. doi: 10.1007/s12160-011-9279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dishman RK. Overview. In: Dishman RK, editor. Exercise Adherence: Its Impact on Public Health. Champaign, IL: Human Kinetics; 1988. [Google Scholar]