Abstract
The purpose of this study was to examine the efficacy of cognitive behavioral therapy (CBT) for anxiety-related disorders based on randomized placebo-controlled trials. We included 41 studies that randomly assigned patients (N = 2,835) with acute stress disorder, generalized anxiety disorder (GAD), obsessive compulsive disorder (OCD), panic disorder (PD), posttraumatic stress disorder (PTSD) or social anxiety disorder (SAD) to CBT or a psychological or pill placebo condition. Findings demonstrated moderate placebo-controlled effects of CBT on target disorder symptoms (Hedges’ g = 0.56), and small to moderate effects on other anxiety symptoms (Hedges’ g = 0.38), depression (Hedges’ g = 0.31) and quality of life (Hedges’ g = 0.30). Response rates in CBT compared to placebo were associated with an odds ratio of 2.97. Effects on the target disorder were significantly stronger for completer samples than intent-to-treat samples, and for individual compared to group CBT in SAD and PTSD studies. Large effect sizes were found for OCD, GAD and acute stress disorder, and small to moderate effect sizes were found for PTSD, SAD and PD. In PTSD studies, dropout rates were greater in CBT (29.0%) compared to placebo (17.2%), but no difference in dropout was found across other disorders. Interventions primarily using exposure strategies had larger effect sizes than those using cognitive or cognitive and behavioral techniques, though this difference did not reach significance. Findings demonstrate that CBT is a moderately efficacious treatment for anxiety disorders when compared to placebo. More effective treatments are especially needed for PTSD, SAD and PD.
Keywords: Anxiety, Anxiety Disorders, Behavior Therapy, Cognitive Therapy, Meta-analysis, Treatment Outcome
Introduction
Anxiety disorders are the most prevalent class of mental disorders, with 12-month prevalence rates of 21.3% in the United States (Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012) and 11.6% worldwide (Baxter, Scott, Vos, & Whiteford, 2013). These disorders are associated with high societal costs (Kessler & Greenberg, 2002; Laynard, Clark, Knapp, & Mayraz, 2007), as well as significant decrements in psychosocial functioning and quality of life (Comer et al., 2011; Hendriks et al., 2016; Olatunji, Cisler, & Tolin, 2007). Fortunately, a sizable body of research has developed over the last several decades demonstrating cognitive behavioral therapy (CBT) to be an effective treatment for anxiety disorders (Hans & Hiller, 2013; Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012).
CBT refers to a class of scientifically-informed interventions that seek to directly manipulate dysfunctional ways of thinking and patterns of behavior in order to reduce psychological suffering (Hofmann, Asmundson, & Beck, 2013). For anxiety disorders specifically, cognitive models posit that exaggerated appraisal of threat is a core element underlying pathological anxiety (Beck & Haigh, 2014; Clark & Beck, 2010). While differences exist in the content and triggers of anxiety across different disorders, research has increasingly supported the idea that anxiety disorders share core underlying features that make them more similar than different (e.g. Barlow, Sauer-Zavala, Carl, Bullis, & Ellard, 2014; Cisler, Olatunji, Feldner, & Forsyth, 2010; Rosellini, Boettcher, Brown, & Barlow, 2015). CBT interventions for anxiety thus share a focus on changing maladaptive beliefs about the likelihood and true cost of anticipated harms by using various cognitive (e.g., cognitive restructuring) and behavioral (e.g., exposure) techniques (Hofmann, 2008; Smits, Julian, Rosenfield, & Powers, 2012).
Evidence for the efficacy of CBT for anxiety disorders comes from a large number of meta-analytic reviews that have shown CBT to result in substantial symptom improvement among individuals with posttraumatic stress disorder (PTSD; Bisson, Roberts, Andrew, Cooper, & Lewis, 2013), generalized anxiety disorder (GAD; Cuijpers et al., 2014), social anxiety disorder (SAD; Mayo-Wilson et al., 2014), obsessive-compulsive disorder (OCD; Öst, Havnen, Hansen, & Kvale, 2015), panic disorder (PD; Pompoli et al., 2016) as well as anxiety disorders globally (Bandelow et al., 2015; Cuijpers, Gentili et al., 2016; Watts, Turnell, Kladnitski, Newby, & Andrews, 2015). However, these meta-analyses examined the effect of CBT relative to a heterogeneous set of control conditions, most frequently consisting of a waitlist control or treatment-as-usual (TAU). Such comparisons are sub-optimal because waitlist control conditions do not control for the effect of patient expectations on treatment outcome (e.g., Greenberg, Constantino, & Bruce, 2006), and TAU conditions are highly varied and not closely monitored (Watts et al., 2015).
The gold-standard study design to best estimate the effect of a treatment is a randomized controlled trial using a psychological or pill placebo as a comparison, as such a control can be standardized within a study and better accounts for the effect of patient expectations on symptom improvement. Comparing CBT to placebo also provides a more useful estimate of the effect of CBT for providers who may be considering medication as a treatment option, as it is standard practice in medication trials to use a placebo comparator to examine treatment efficacy. In fact, the US Food and Drug Administration (FDA) will not accept noninferiority studies with active comparators for approval of new drugs, still considering placebo controlled RCTs as the only effective method for determining efficacy (Feifel, 2009; Laughren, 2001).
In 2008, some of us (Hofmann & Smits, 2008) published the only meta-analysis of exclusively randomized placebo-controlled trials of CBT for anxiety and related disorders. We identified 27 studies showing moderate to large effects (Hedges’ g = 0.73) of CBT for anxiety symptoms and moderate effects (Hedges’ g = 0.45) for depressive symptoms in completer samples. Effects varied across disorder type, with the strongest effect sizes found in OCD and acute stress disorder, and the weakest in PD. Of note, a meta-analysis by Cuijpers, Cristea, Karyotake, Reijnders and Huibers (2016) examined the effects of CBT for PD, OCD and SAD compared to pill placebo in addition to wait list and TAU. However, this analysis did not include studies that compared CBT to a psychological placebo (e.g. supportive counseling), which is an important comparison condition because it can serve as a control for so-called common factors that can impact treatment outcome, such as the therapeutic alliance (Horvath, Del Re, Flückiger, & Symonds, 2011; Smits & Hofmann, 2009).
The present study sought to update the analysis by Hofmann and Smits (2008) with data from randomized placebo-controlled trials of CBT for anxiety related disorders published since 2008. Such an up-to-date analysis of the efficacy of CBT is necessary to further inform ongoing debate about the efficacy of different treatment modalities (e.g., Hofmann & Curtiss, 2015; Wampold & Imel, 2015), and to provide evidence for researchers and policy makers about the potential utility of disseminating CBT interventions. This update to Hofmann and Smits (2008) also provides a more comprehensive assessment of the scope by CBT’s impact on anxiety by including additional moderator analyses, outcome variables, and an examination of follow-up data. Although OCD, acute stress disorder and PTSD are no longer classified as anxiety disorders in DSM-5, we included them in the present study to be consistent with the prior analysis, and because of the high degree of overlap in the etiology and treatment of these disorders when compared to DSM-5 anxiety disorders (Stein et al., 2010; Zoellner, Rothbaum, & Feeny, 2011).
Similar to Hofmann and Smits (2008), we investigated between-group effect sizes for continuous measures of anxiety symptoms and depression symptoms at post-treatment, as well as categorical indices of response rates and dropout rates. We also examined the effects of CBT on target disorder symptom measures (as opposed to general indices of anxiety) and quality of life measures at post-treatment, as well as long-term follow-up outcomes. In addition to study year, placebo type, number of treatment sessions, and use of a completer vs. intent-to-treat (ITT) analyses (moderators tested in Hofmann and Smits, 2008), we examined sample characteristics (race, sex, sample size, inclusion of patients on medication), risk of bias, and treatment type (behavioral, cognitive or both; group vs. individual) as moderators of treatment outcome.
Method
Following the guidelines set forth in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement, the protocol for this meta-analysis was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (registration number CRD42016050841).
Selection of Studies
To identify eligible studies, we searched PubMed and PsycINFO, for articles published from the first available date to January 4, 2017. The following search terms were used: ((random*)) AND (((cognitive behavior*therap*) OR (cognitive therap*) OR (behavior*therap*))) AND ((GAD) OR (generalized anxiety disorder) OR (OCD) OR (obsessive compulsive disorder) OR (social phobia) OR (social anxiety disorder) OR (specific phobia) OR (simple phobia) OR (PTSD) OR (post-traumatic stress disorder) OR (acute stress disorder))). In addition, we conducted manual searches of reference lists from recently published meta-analyses and review articles. Our search produced 3,215 unique studies, the first 1,165 of which were reviewed for eligibility in Hofmann and Smits (2008) using the same eligibility criteria.
Studies were selected by the first, second and third authors and a team of independent trained assessors. Studies were included in the present meta-analysis if: 1) patients were between ages 18 and 65 and met DSM-III-R, DSM-IV, or DSM-5 diagnostic criteria for acute stress disorder, GAD, OCD, PTSD, SAD or specific phobia as determined by a psychometrically sound and structured diagnostic instrument; 2) patients were randomly assigned to either CBT or placebo (pill or psychological). A psychological placebo was defined as a condition involving interventions to control for nonspecific factors (e.g., contact with a therapist equivalent to the active treatment, reasonable rationale for the intervention, discussion of the psychological problem), and not including any treatment elements with demonstrated efficacy for the condition being treated (e.g. relaxation for OCD or PTSD; Smits & Hofmann, 2009); 3) the clinical severity of the anxiety disorder was assessed by means of psychometrically sound measures; and 4) studies provided sufficient data to calculate effect sizes.
Studies were excluded if: 1) they consisted of secondary analyses of a larger, more complete, or earlier study; 2) placebo interventions included active treatment ingredients for the target problem (e.g., self-guided exposures); 3) the CBT intervention was deemed to be ‘third-wave’ (Acceptance and Commitment Therapy, mindfulness-based interventions, etc.); 4) the entire study sample had a particular comorbidity (e.g., substance abuse or a medical condition); or 5) the intervention took place remotely (over the phone or computer; see Olthuis, Watt, Bailey, Hayden, and Stewart (2015) for a meta-analysis on internet-based CBT for anxiety).
Data Extraction
For each study, the first, second and third authors independently identified the outcome measures to be used for the analysis. This included continuous measures of disorder specific symptoms, other anxiety symptoms, depression, and quality of life, as well as dichotomous outcomes of treatment response and dropout percentage. For those studies that reported multiple indices of treatment response, we selected the most conservative measure. Data was then extracted for the CBT and placebo treatment arms at pre-treatment, post-treatment, and if reported 6-month follow-up (or closest available). If data necessary for calculating effect sizes was not available in the published manuscript, we contacted the authors. We also extracted data on sample and study characteristics, including sample size, demographics, placebo type, CBT treatment type (exposure, cognitive or both; group vs. individual), number of sessions, type of analysis (completer vs. ITT), and year of publication. Data were extracted on two separate occasions by independent raters and compared to ensure accuracy, with discrepancies resolved by the first and second authors.
Risk of Bias Assessment
We assessed study quality with the Cochrane Collaboration’s tool for assessing risk of bias (Higgins & Altman, 2008). This tool involves assessing each study as containing a high, low or unclear level of bias risk in a number of domains: 1) Sequence Generation: Was allocation of participants to treatment condition adequately generated in a random manner? 2) Allocation Concealment: Was treatment assignment adequately concealed from investigators and participants prior to randomization? 3) Blinding: Were outcome assessors, therapists, and patients (when possible) blind to the treatment patients were receiving? 4) Incomplete Outcome Data: Were outcome data missing at random and imputed using appropriate methods? 5) Selective Outcome Reporting: Were pre-specified outcome variables of interest adequately and completely reported? A total bias assessment was created for each study by assigning a value of 0 (low bias risk), 1 (unclear bias risk), or 2 (high bias risk), and summing the score of each category. The first and second authors independently rated each study and then met to resolve any discrepancies. Inter-rater reliability for the total bias assessment was strong (Cronbach’s α = .81).
Quantitative Data Synthesis
We examined heterogeneity in our data using the Chi-squared test and the I2 statistic, which is an indicator of the strength of the heterogeneity. Guidelines for I2 suggest that 25%, 50% and 75% values represent low, moderate, and high heterogeneity, respectively (Higgins, Thompson, Deeks & Altman, 2003). Regardless of statistical heterogeneity, we used a random effects model because of the variability within patient and methodological characteristics of the included studies. For continuous outcomes, between-groups effect sizes and their 95% confidence intervals (CI) were calculated using Hedges’ g (Hedges & Olkin, 1985). When a study used multiple measures in a given outcome category, effect sizes were averaged across all outcome measures in the category. Effect sizes were calculated using either pre- and post-treatment means and standard deviations or the mean and standard deviation of pre-post change scores. For follow-up effect sizes, 6-month (or closest available) follow-up means and standard deviations were used in place of post-treatment data. For categorical outcomes (i.e., response rates and attrition), we calculated the odds ratio (OR) and confidence intervals using the Cox-Hinkley-Miettinen-Nurminen method (Miettinen & Nurminen, 1985). To calculate ORs, we used the number of treatment responders and patients randomized to each condition, or if necessary we calculated number of responders based on the response rate reported. To investigate potential moderator effects on outcome, we used the between-group heterogeneity statistic (QB) recommended by Hedges and Olkin (1985) for categorical moderators, and meta-regression procedures for continuous moderators.
To examine the potential influence of publication bias, we inspected the funnel plot to evaluate asymmetry of effect size estimates as a function of their precision. We used Egger’s regression intercept as a formal test of funnel plot asymmetry (Egger, Smith, Schneider, & Minder, 1997). In addition, the Trim and Fill method (Duval & Tweedie, 2000) was used, which estimates the number of studies that would have to be removed from the funnel plot to make it symmetrical, and then imputes an estimated effect size that accounts for funnel plot asymmetry. All meta-analytic procedures were conducted in Comprehensive Meta-Analysis, Version 3.
Results
Study Flow and Characteristics
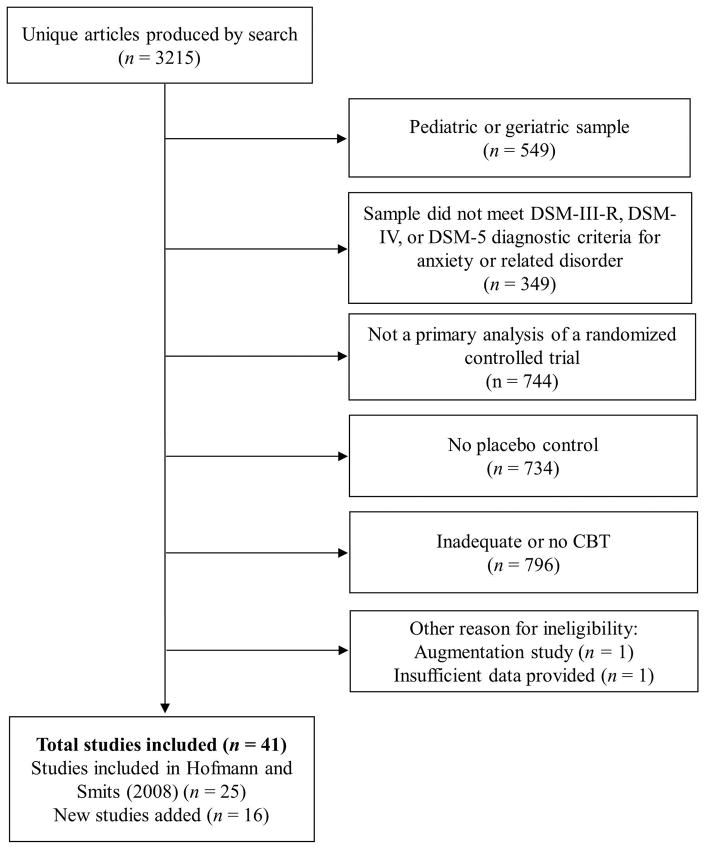
The flow diagram in Figure 1 shows the number of studies excluded and the reasons for exclusion at each stage of study selection. The final analysis included 41 studies, 16 of which were not included in the Hofmann and Smits (2008) paper. Together these studies examined a total of 2,835 patients randomized to either CBT or placebo.
Figure 1.
Flow diagram of study selection process
Of the 41 studies included in the analysis, 40 reported continuous outcome data for target disorder symptoms, and 33 reported categorical outcome data on response rates. PTSD was the most commonly represented disorder (14 studies comprising 1,252 patients), followed by SAD (12 studies, 753 patients), PD (5 studies, 328 patients), OCD (4 studies, 313 patients), acute stress disorder (4 studies, 132 patients) and GAD (2 studies, 57 patients). Most studies (n = 29) compared CBT to a psychological placebo, with supportive counseling being the most common comparison treatment. The majority of CBT treatments used both formal therapist-guided exposure and cognitive techniques (n = 24), though some treatments consisted of primarily exposure techniques (n = 10), or primarily cognitive strategies (n = 7). Thirty-four studies examined individual CBT, while 7 studies examined group CBT. Mean treatment duration across studies was 11.0 sessions (SD = 4.72). The average study sample had a mean age of 36.0 years (SD = 6.53), was 58.9% female (SD = 21.21) and was 73.0% white (SD = 21.87). Of the 35 studies that included information about psychiatric medication use, 18 studies excluded patients receiving psychiatric medication, 15 studies included patients who were on stable doses, and two studies excluded only specific medications (e.g., benzodiazepines, SSRIs). From the latter two groups, nine studies reported data on the number of patients taking psychiatric medication. On average, 34.2% of those samples (SD = 17.4) received psychiatric medication. In terms of risk of bias, all but one study had a rating of unclear risk of bias in at least one of the five categories, and 14 of the 40 studies had at least one category of high risk. The number of studies with low, unclear and high risk of bias in each of the categories was as follows: sequence generation (15 low, 26 unclear, 0 high); allocation concealment (14 low, 27 unclear, 0 high); blinding (27 low, 11 unclear, 3 high); incomplete outcome data (9 low, 19 unclear, 13 high); selective outcome reporting (37 low, 4 unclear, 0 high). Sixteen studies used intent-to-treat analyses for the continuous outcomes, while 25 only presented completer data. Information about characteristics of each study can be seen in the Supplementary Materials Table 1.
Data Synthesis
Dropout Rates
Examination of dropout rates showed a significantly greater likelihood of dropout in CBT compared to placebo (OR = 1.35, 95% CI = 1.05 to 1.77, p < .05). The weighted mean dropout rate across all studies was 24.0% in CBT and 17.2% in placebo. This difference in dropout rates was largely due to a greater attrition rate in the 14 studies examining PTSD (29.0% in CBT vs. 17.2% in placebo), which had an OR of 1.82 (95% CI = 1.32 to 2.52, p < .01). With PTSD studies removed, the difference in dropout between CBT (19.6%) and placebo (17.2%) reduced to non-significance (OR = 1.10, 95% CI = .78 to 1.55, p = n.s.).
Outcomes after Acute Treatment
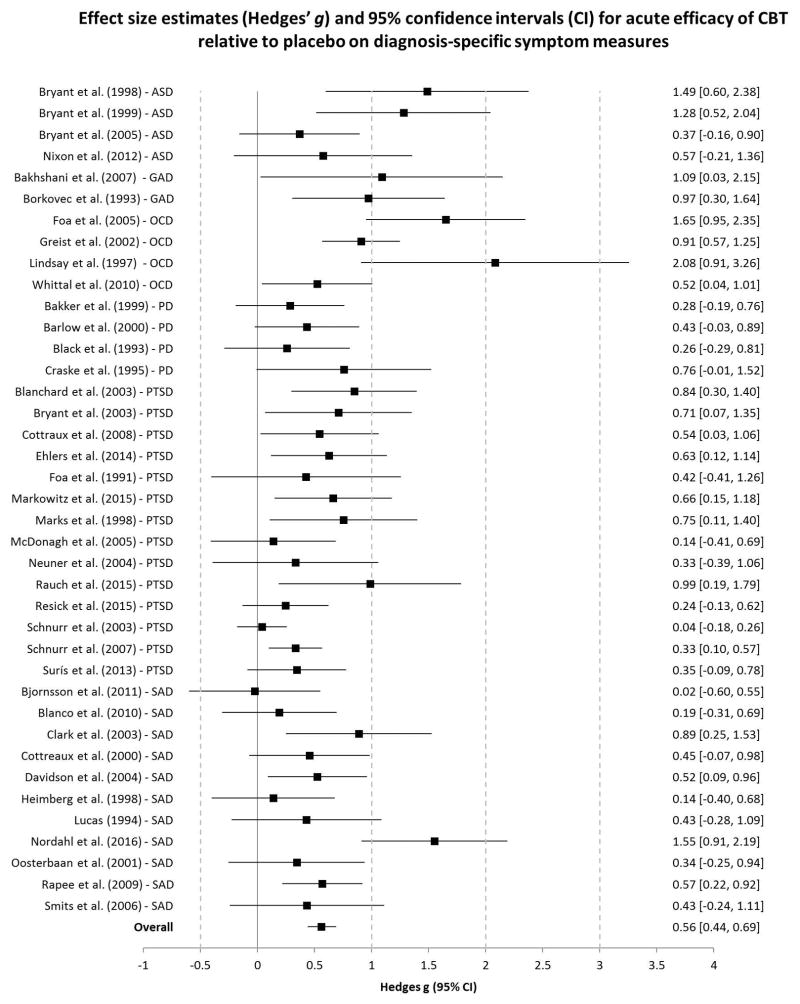
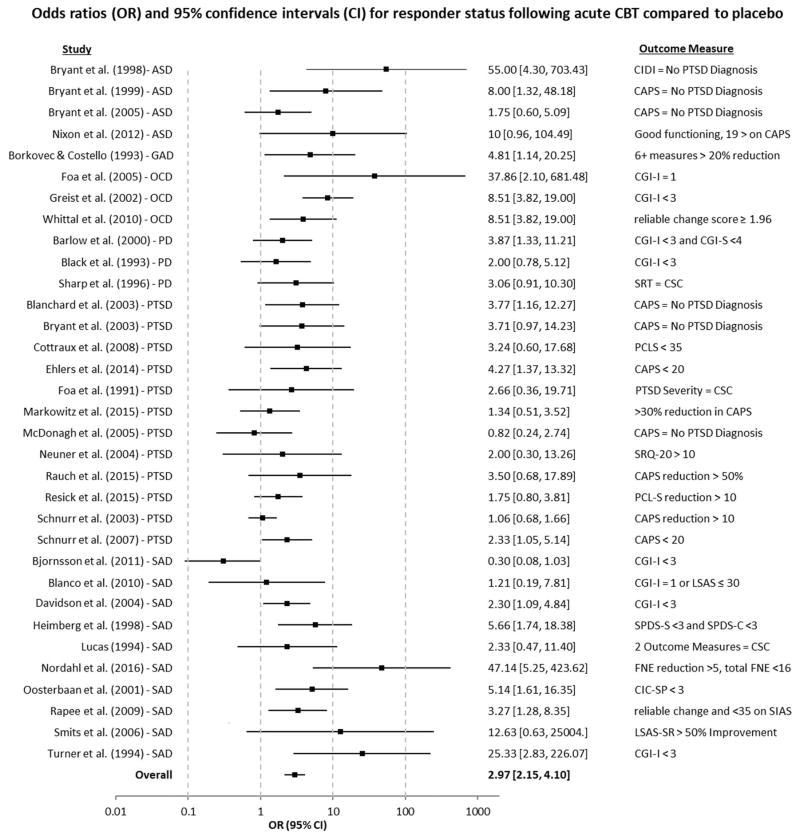
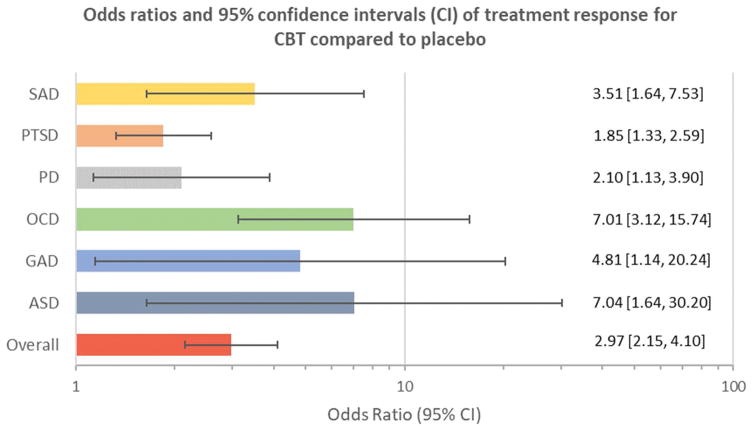
Between-group effect sizes for continuous measures of target disorder symptoms from pre to post-treatment were in the medium range (Hedges’ g = 0.56, 95% CI = 0.44 to 0.69, p < .0001), indicating superior improvement in individuals randomized to CBT over placebo. Effect sizes were significantly smaller for ITT samples (Hedges’ g = 0.40, 95% CI = 0.25 to 0.56, p < .0001) compared to completer samples (Hedges’ g = 0.70, 95% CI = 0.54 to 0.86, p < .0001; QB = 6.85, df = 1, p < .01). The OR for categorical measures of treatment response of CBT compared to placebo condition was 2.97 (95% CI = 2.15 to 4.10, p < .0001). ORs were again larger for completer samples (OR = 3.69, 95% CI = 2.59 to 5.26, p < .0001) than ITT (OR = 2.42, 95% CI = 1.65 to 3.54, p < .0001), however this difference was not significant (QB = 2.56, df = 1, p = n.s.). See Figure 2 and Figure 3 for a forest plot of effect sizes and odds ratios of each individual study included in the analysis.
Figure 2.
Effect size estimates (Hedges’ g) and 95% confidence intervals (CI) for acute efficacy of CBT relative to placebo on diagnosis-specific symptom measures.
ASD = Acute Stress Disorder; GAD = Generalized Anxiety Disorder; OCD = Obsessive- Compulsive Disorder; PD = Panic Disorder; PTSD = Post Traumatic Stress Disorder; SAD = Social Anxiety Disorder.
Figure 3.
Odds ratios (OR) and 95% confidence intervals (CI) for responder status following acute CBT compared to placebo.
ASD = Acute Stress Disorder; GAD = Generalized Anxiety Disorder; OCD = Obsessive- Compulsive Disorder; PD = Panic Disorder; PTSD = Post Traumatic Stress Disorder; SAD = Social Anxiety Disorder. CIDI = Composite International Diagnostic Interview PTSD Module; CAPS = Clinician Administered PTSD Scale; CGI - S = Clinical Global Impressions Scale – Severity; CGI - I = Clinical Global Impressions Scale – Improvement; SRT = Symptom Rating Test; CSC = Clinically Significant Change (See Sharp et al., 1996, Foa et al., 1991, or Lucas, 1994); PCLS = PTSD Checklist; SRQ-20 = Self-Reporting Questionnaire; SPDS-S = Social Phobic Disorder Severity; SPDS-C = Social Phobic Disorder Change Form; FNE = Fear of Negative Evaluation Scale; SIAS = Social Interaction Anxiety Scale; CIC-SP = Clinical Impression of Change — Social Phobia Scale; LSAS-SR = Liebowitz Social Anxiety Scale.
Twenty-six studies reported continuous measures of other anxiety symptoms, producing a Hedges’ g of 0.38 (95% CI = 0.25 to 0.51, p < .0001). Effects of CBT compared to placebo on depression in the 26 studies reporting depression outcomes were in the small range (Hedges’ g = 0.31, 95% CI = 0.21 to 0.41, p < .0001). A minority of studies (n =15) reported data on quality of life, producing a Hedges’ g estimate of 0.30 (95% CI = 0.13 to 0.48, p < .001).
Heterogeneity was in moderate range for disorder-specific outcomes (Q = 83.39, df(Q) = 38, p < .001; I2 = 54.43%) and QOL (Q = 30.81, df(Q) = 15, p < .05; I2 = 51.31%), small for other anxiety symptoms (Q = 34.63, df(Q) = 25, p < 0.10; I2 = 27.80%), and non-significant for depression symptoms (Q = 19.31, df(Q) = 25, p = n.s.; I2 = 0.00%). For categorical outcomes, heterogeneity was also in the moderate range (Q = 73.25, df(Q) = 32, p < .01; I2 = 56.32%).
Long-Term Follow-up
Twenty-two of the 41 studies included in the analysis reported on follow-up outcomes. The mean follow-up assessment period was 5.55 months (SD = 2.37). The effect size for target disorder symptoms at follow-up was in the moderate range (Hedges’ g = 0.47, 95% CI = 0.30 to 0.64, p < .0001), as was the effect size for other anxiety symptoms (Hedges’ g = 0.42, 95% CI = 0.23 to 0.62, p < .0001). Fourteen studies reported follow-up data for depression, producing a Hedges’ g of 0.29 (95% CI = 0.16 to 0.42, p < .0001). Only eight studies reported QOL data at follow-up (all but one of which were PTSD studies), producing a statistically significant but minimal effect (Hedges’ g = 0.15, 95% CI = 0.01 to 0.28, p < .05).
Publication Bias
Based on the funnel plot for the disorder-specific symptom measures, Egger’s regression intercept was 2.25 (p < .001), suggesting asymmetry in the funnel plot. Using the Trim and Fill method, 14 studies would have to be trimmed from the right side of the mean to make the plot symmetrical, leading to an adjusted effect size of 0.33 (95% CI = 0.19 to 0.48).
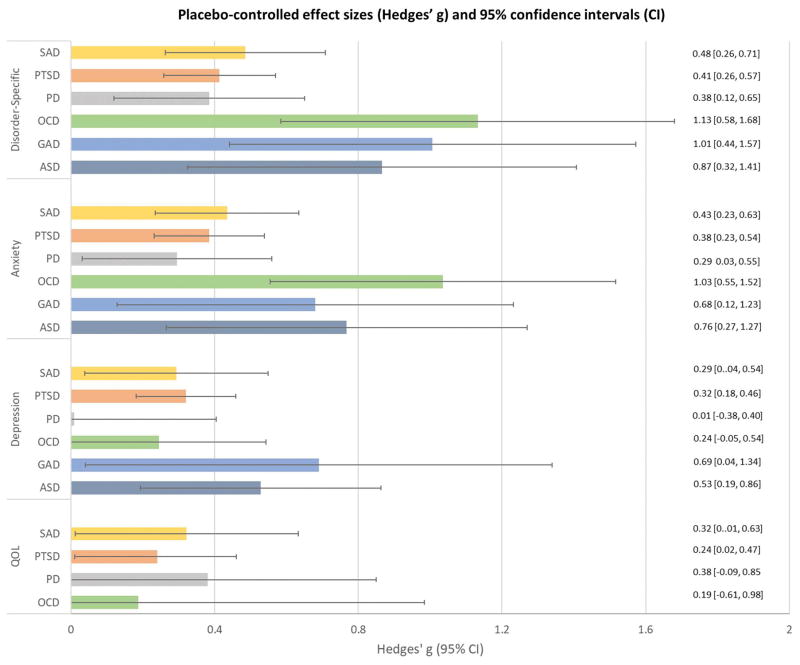
Comparisons between diagnostic groups
Effect sizes and 95% confidence intervals for diagnosis-specific symptoms, anxiety, depression and quality of life for different diagnostic groups are presented in Figure 4. Results revealed significant differences in controlled effect sizes for target disorder symptom measures across disorder type (QB = 12.52, df = 5, p < .05). Greatest effects were seen in OCD (Hedges’ g = 1.13, 95% CI = 0.58 to 1.68, p < .001), followed by GAD (Hedges’ g = 1.01, 95% CI = 0.44 to 1.57, p < .001) and acute stress disorder (Hedges’ g = 0.87, 95% CI = 0.32 to 1.41, p < .01). SAD (Hedges’ g = 0.41, 95% CI = 0.25 to 0.57, p < .0001), PTSD (Hedges’ g = 0.48, 95% CI = 0.26 to 0.71, p < .0001), and PD (Hedges’ g = 0.39, 95% CI = 0.12 to 0.65, p < .0001) each produced effect sizes in the small to medium range (see Figure 4). Pairwise comparisons showed OCD studies to be associated with significantly greater effects sizes than PTSD, SAD and PD studies (all p values < .05). GAD studies exhibited significantly greater effect sizes than PTSD studies (p < .05). To examine whether differential effect sizes across disorders may have been related to varying strength of placebo conditions for different conditions, we examined uncontrolled pre-post effect sizes of just placebo conditions. Results showed no difference in within-group effect sizes across different disorders during placebo treatment (QB = 3.34, df = 5, p = n.s.; range of Hedges’ g = 0.38 to 0.55), a finding that did not change when examining pill (QB = 4..79, df = 3, p = n.s.) and psychological placebos (QB = 3.34, df = 5, p = n.s.) separately.
Figure 4.
Placebo-controlled effect sizes and 95% confidence intervals (CI) for disorder-specific, anxiety, depression and quality of life measures
QOL = Quality of Life. ASD = Acute Stress Disorder; GAD = Generalized Anxiety Disorder; OCD = Obsessive- Compulsive Disorder; PD = Panic Disorder; PTSD = Post Traumatic Stress Disorder; SAD = Social Anxiety Disorder.
When examining categorical outcomes, results similarly showed significant differences across disorder type (QB =13.16, df = 5, p < .05). Odds ratios and 95% confidence intervals by disorder type are presented in Figure 5. Pairwise comparisons showed greater ORs in OCD compared to PTSD (QB = 8.90, df = 1, p < .01) and PD (QB = 5.39, df = 1, p < .05).
Figure 5.
Odds ratios and 95% confidence intervals (CI) of treatment response for CBT compared by target disorder
QOL = Quality of Life. ASD = Acute Stress Disorder; GAD = Generalized Anxiety Disorder; OCD = Obsessive- Compulsive Disorder; PD = Panic Disorder; PTSD = Post Traumatic Stress Disorder; SAD = Social Anxiety Disorder.
Moderator Analyses
Moderator analyses are reported for target disorder symptom outcomes only, though analyses of categorical outcomes mirrored those of the continuous target disorder symptom measures. In analyzing group vs. individual treatment as a moderator, sufficient data were only available for studies on SAD and PTSD. Studies utilizing individual CBT (Hedges’ g = 0.54, 95% CI = 0.40 to 0.68, p < .0001) produced greater effect sizes than group CBT (Hedges’ g = 0.16, 95% CI = 0.01 to 0.31, p < .05; QB = 13.30, df = 1, p < .001). Studies using treatments primarily consisting of exposure techniques (Hedges’ g = 0.78, 95% CI = 0.45 to 1.10, p < .0001) produced larger effect sizes than those including both cognitive and exposure techniques (Hedges’ g = 0.53, 95% CI = 0.36 to 0.70, p < .0001) and only cognitive techniques (Hedges’ g = 0.38, 95% CI = 0.18 to 0.57, p < .001), but these differences did not reach significance (QB = 4.39, df = 2, p = n.s.). No difference in effect size was found between studies comparing CBT to psychological (Hedges’ g = 0.52, 95% CI = 0.38 to 0.66, p < .0001) versus pill placebo (Hedges’ g = 0.66, 95% CI = 0.36 to 0.97, p < .0001; QB = 0.71, df = 1, p = n.s.). Furthermore, no difference in pre-post effect sizes for placebo groups was found between psychological (Hedges’ g = 0.53, 95% CI = 0.44 to .63) and pill placebos (Hedges’ g = 0.45, 95% CI = 0.35 to 0.55; QB = 1.47, df = 1, p = n.s.). Finally, no difference was found between effect sizes of self-report measures (Hedges’ g = 0.53, 95% CI = 0.40 to 0.67, p < .0001) and clinician-administered measures (Hedges’ g = 0.50, 95% CI = 0.36 to 0.64, p < .0001; QB = 0.13, df = 1, p = n.s.).
Sample characteristics, including race (B = 0.01, SE = 0.00, p = n.s.), sex (B = 0.00, SE = 0.00, p = n.s.), sample size (B = 0.00, SE = 0.00, p = n.s.), and inclusion of patients receiving medication (QB = 0.25, df = 1, p = n.s.) did not moderate effect sizes. In addition, study characteristics such as number of sessions (B = −0.01, SE = 0.02, p = n.s.), study year (B = −0.00, SE = 0.01, p = n.s.) and risk of bias (B = −0.05, SE = 0.05, p = n.s.) were not found to relate to effect sizes.
Discussion
Given that patient expectations for improvement alone can lead to significant symptom change (Greenberg et al., 2006; Wampold, Minami, Tierney, Baskin, & Bhati, 2005), the most rigorous method to estimate the effect of an intervention such as CBT is to compare it to a placebo condition. Accordingly, the present study sought to assess the state of the evidence for CBT for anxiety and related disorders by conducting a meta-analysis specifically on randomized placebo-controlled trials. Building on a previous meta-analysis by our group (Hofmann & Smits, 2008), this review yielded 16 additional studies (a 59% increase), examining a total of 41 trials with 2,835 patients who were randomly assigned to CBT or placebo for acute stress disorder, GAD, OCD, PD, PTSD or SAD. Results yielded significant but moderate effect sizes at post-treatment and follow-up for target disorder symptoms, and significantly greater odds of treatment response for CBT than placebo. In addition, CBT was associated with significant effects on other anxiety measures, depression and quality of life. These findings show that CBT is associated with significantly greater benefit for anxiety-related disorders than placebo conditions, and that the superior effects of CBT extend beyond symptoms of the disorder being treated.
The present meta-analytic review extends the work of Hofmann and Smits (2008) and other previous meta-analyses in several important ways. For one, the present study included sufficient studies with follow-up data to examine whether gains during CBT were maintained after treatment concluded. Results showed follow-up effect sizes equivalent to post-treatment for disorder-specific symptoms, anxiety and depression. This maintenance of gains in response to CBT compared to placebo is of great importance given that the goal of psychological treatment is not just to provide immediate relief of symptoms, but to produce long-lasting change in patients’ lives. This finding is also important because meta-analyses relying on wait-list controlled trials are not able to examine controlled followed-up data, since treatment cannot be ethically withheld past the active treatment period for patients assigned to a waitlist.
The larger sample size in the present study also allowed us to conduct more robust moderator analyses on a wider array of variables. Effect size was not found to relate to risk of bias, publication year, or the majority of sample characteristics (race, age, sex, sample size, medication use) and treatment characteristics (number of sessions, placebo type), but the effect of group versus individual treatment was significant. Although group CBT was only tested in PTSD and SAD studies, effect sizes were smaller for group treatment compared to individual CBT for those disorders. This finding is consistent with direct comparisons between group and individual treatments in SAD (e.g., Hedman et al., 2013). Moreover, treatments that primarily focused on exposure techniques produced larger effect sizes (Hedges’ g = 0.78) than those that included both cognitive and behavioral techniques (Hedges’ g = 0.53) and cognitive techniques alone (Hedges’ g = 0.38), though these differences were not statistically significant. This is inconsistent with an earlier head to head comparison that led the author to conclude that exposure and cognitive treatments tend to be equally effective (Ougrin, 2011); however, this interpretation was based on comparisons of relatively small numbers of trials and therefore may be biased.
A number of our results mirror those found in the previous analysis by Hofmann and Smits (2008) and other prior research. Specifically, the strength of the effect of CBT depended on whether the analysis was conducted on completer or ITT samples, with completer samples producing significantly larger effect sizes, though not odds ratios, compared to ITT samples. Such a discrepancy between ITT and completer samples is particularly important given that CBT was associated with significantly greater dropout rates than placebo in the present analysis, a result not found in Hofmann and Smits (2008). Notably, this result appeared to be driven by greater dropout rates among CBT patients in PTSD studies, which has also been found in previous meta-analytic research (Imel, Laska, Jakupcak, & Simpson, 2013). Such a finding suggests that for PTSD studies, the superior effect of CBT compared to placebo may be inflated by lack of data from dropouts.
Dropout rates in CBT for non-PTSD studies (19.6%), on the other hand, were not significantly different from placebo, which is consistent with prior research comparing dropout rates between CBT and other treatments (e.g., Ong, Clyde, Bluett, Levin, & Twohig, 2016). Furthermore, our analysis of dropout in non-PTSD studies produced an identical dropout rate as another meta-analysis examining CBT for anxiety disorders in a different set of studies (Fernandez, Salem, Swift, & Ramtahal, 2015). We can also compare our effect size results with a study by Mayo-Wilson and colleagues (2014) that used network meta-analysis to indirectly compare effect sizes of CBT conditions to placebo in SAD. Results of that study produced controlled effect sizes of 0.72 (individual CBT vs. pill placebo), 0.45 (group CBT vs. pill placebo), 0.56 (individual CBT vs. psychological placebo) and 0.29 (group CBT vs. psychological placebo). Across the groups these effect sizes of CBT for SAD are similar to what we found (0.41).
Also similar to the findings of Hofmann and Smits (2008), CBT effect sizes varied across disorders, with large effect sizes for OCD and acute stress disorder studies and small to moderate effect sizes for PTSD, SAD and PD. In contrast to previous results, GAD studies were associated with large effect sizes, which were significantly greater than PTSD and SAD studies. Effects for OCD studies were also significantly greater than PTSD, SAD and PD. Previous studies have reported a relatively small effect of pill placebo in OCD, and a large placebo response for PD, PTSD and GAD (Khan et al., 2005; Sugarman, Kirsch, & Huppert, 2017), which could plausibly account for differential efficacy across disorders. In the present study, however, we did not find any effect of psychological disorder on pre-post effect sizes of placebo, even when examining pill and psychological placebo separately. Nonetheless, given the relatively small number of studies examining each disorder, findings regarding both the absence of differential placebo efficacy and the superior effects of OCD and GAD should be interpreted with caution.
Highlighting the importance of comparing CBT to placebo controls, effect sizes in the present analysis were substantially smaller than previous meta-analyses comparing the effect of CBT to waitlist or other control treatments for disorder-specific symptoms (Bandelow et al., 2015), depression (Cuijpers, Cristea, Weitz, Gentili, & Berking, 2016), and quality of life (Hofmann, Wu, & Boettcher, 2014) in anxiety disorder samples. For instance, the meta-analysis by Bandelow and colleagues (2015) comparing CBT to waitlist produced an overall effect size of 1.23 for anxiety disorder symptoms. In contrast, we observed that CBT was associated with an effect size of 0.56 when compared to placebo. Given that placebo controls are better able to account for non-specific factors of a treatment such as expectancy effects, the more conservative estimates found in the present study are likely to be the more accurate reflection of the specific effect of CBT. Using only placebo-controlled trials also allows for a more meaningful comparison to effect sizes reported in medication trials. The meta-analysis by Bandelow and colleagues (2015), for instance, found pharmacotherapy for GAD, PD and SAD to be associated with pooled placebo-controlled effect sizes ranging from 0.17 to 0.96 (M = 0.58, SD = 0.22) depending on the medication, suggesting similar efficacy.
A number of limitations should be noted regarding the present research. First, only 16 of the 41 studies included used ITT analyses, and the use of completer analyses appeared to lead to greater effect size estimates. Even among studies using ITT analyses, results from our risk of bias assessment indicated that many studies did not account for missing data properly, or did not provide adequate information for why data were missing or how missing data were dealt with. Relatedly, the present results may have been influenced by publication bias. In addition, criteria for treatment response varied between studies, potentially contributed to increased heterogeneity in the effect sizes for categorical outcomes.
Another limitation is that apart from studies examining PTSD, samples were not particularly diverse racially. The mean sample of non-PTSD studies was 82% white, with only two non-PTSD studies using a sample with more than 23% non-whites. Future research is needed to examine the generalizability of the present results to more diverse samples. Finally, it should be noted that there was some degree of heterogeneity in the types of placebo conditions used across studies. Although no difference between studies using psychological vs. pill placebo was found for either controlled or pre-post placebo effect sizes, the lack of complete uniformity in control conditions limits the precision of the comparison. For instance, studies using pill placebo typically do not control for time spent with a clinician, and may attract a unique sample that is open to both pharmacological and psychotherapy treatments. In studies using psychological placebos, on the other hand, providers and even patients may know that they are assigned to a control condition. In addition, there was some variability in the form and content of psychological placebo treatments across studies, and it is possible that this affected the relative effects of CBT seen in different studies. While not considered a true placebo condition for the purposes of this study, future research would also benefit from comparing full treatment to minimally instructed self-guided CBT.
Despite these limitations, the present results provide strong evidence that CBT is an efficacious treatment for anxiety and related disorders in adults, and that its effects meaningfully exceed that of placebo. In addition, the impact of CBT extends beyond the symptoms of the disorder being targeted, and lasts beyond acute treatment. Results also suggest room for improvement, especially for treating PTSD, SAD, and PD. Furthermore, additional trials that include ITT analyses would help to more accurately estimate the effect of CBT.
Supplementary Material
Footnotes
Financial Disclosures: Dr. Hofmann receives support from NIH/NCCIH (R01AT007257), NIH/NIMH (R01MH099021, R34MH099311, R34MH086668, R21MH102646, R21MH101567, K23MH100259), the James S. McDonnell Foundation 21st Century Science Initiative in Understanding Human Cognition – Special Initiative, and the Department of the Army for work unrelated to the studies reported in this article. He receives compensation for his work as an advisor from the Palo Alto Health Sciences and Otsuka Digital Health, Inc., and for his work as a Subject Matter Expert from John Wiley & Sons, Inc. and SilverCloud Health, Inc. He also receives royalties and payments for his editorial work from various publishers for work unrelated to the studies reported in this article. Dr. Powers receives support from NIH/NIDA (K01DA035930). Dr. Smits receives compensation from MicroTransponder, Inc. for his work as consultant and royalties from various publishers for books unrelated to the research reported in this manuscript. He also receives grant support from the National Institutes of Health (R34DA034658, R34MH099318) and the Cancer Prevention and Research Institute of Texas (RP170095).
References
- Bakhshani NM, Lashkaripour K, Sadjadi SA. Effectiveness of short term cognitive behavior therapy in patients with generalized anxiety disorder. Journal of Medical Sciences. 2007;7:1076–1081. [Google Scholar]
- Bakker A, van Dyck R, Spinhoven P, van Balkom AJ. Paroxetine, clomipramine, and cognitive therapy in the treatment of panic disorder. The Journal of Clinical Psychiatry. 1999;60:831–838. doi: 10.4088/jcp.v60n1205. [DOI] [PubMed] [Google Scholar]
- Bandelow B, Reitt M, Röver C, Michaelis S, Görlich Y, Wedekind D. Efficacy of treatments for anxiety disorders: A meta-analysis. International Clinical Psychopharmacology. 2015;30:183–192. doi: 10.1097/YIC.0000000000000078. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA. 2000;283:2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, Ellard KK. The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science. 2014;2:344–365. [Google Scholar]
- Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychological Medicine. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Beck AT, Haigh EA. Advances in cognitive theory and therapy: The generic cognitive model. Annual Review of Clinical Psychology. 2014;10:1–24. doi: 10.1146/annurev-clinpsy-032813-153734. [DOI] [PubMed] [Google Scholar]
- Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. The Cochrane Library. 2013;12:CD003388. doi: 10.1002/14651858.CD003388.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjornsson AS, Bidwell LC, Brosse AL, Carey G, Hauser M, Mackiewicz Seghete KL, … Craighead WE. Cognitive–behavioral group therapy versus group psychotherapy for social anxiety disorder among college students: A randomized controlled trial. Depression and Anxiety. 2011;28:1034–1042. doi: 10.1002/da.20877. [DOI] [PubMed] [Google Scholar]
- Black DW, Wesner R, Bowers W, Gabel J. A comparison of fluvoxamine, cognitive therapy, and placebo in the treatment of panic disorder. Archives of General Psychiatry. 1993;50:44–50. doi: 10.1001/archpsyc.1993.01820130046008. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Devineni T, Veazey CH, Galovski TE, Mundy E, … Buckley TC. A controlled evaluation of cognitive behaviorial therapy for posttraumatic stress in motor vehicle accident survivors. Behaviour Research and Therapy. 2003;41:79–96. doi: 10.1016/s0005-7967(01)00131-0. [DOI] [PubMed] [Google Scholar]
- Blanco C, Heimberg RG, Schneier FR, Fresco DM, Chen H, Turk CL, … Liebowitz MR. A placebo-controlled trial of phenelzine, cognitive behavioral group therapy, and their combination for social anxiety disorder. Archives of General Psychiatry. 2010;67:286–295. doi: 10.1001/archgenpsychiatry.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG, Dang ST, Sackville T, Basten C. Treatment of acute stress disorder: A comparison of cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology. 1998;66:862–866. doi: 10.1037//0022-006x.66.5.862. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Sackville T, Dang ST, Moulds M, Guthrie R. Treating acute stress disorder: An evaluation of cognitive behavior therapy and supportive counseling techniques. American Journal of Psychiatry. 1999;156:1780–1786. doi: 10.1176/ajp.156.11.1780. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds ML, Guthrie RM, Nixon RD. The additive benefit of hypnosis and cognitive-behavioral therapy in treating acute stress disorder. Journal of Consulting and Clinical Psychology. 2005;73:334–340. doi: 10.1037/0022-006X.73.2.334. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds ML, Guthrie RM, Dang ST, Nixon RD. Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2003;71:706–712. doi: 10.1037/0022-006x.71.4.706. [DOI] [PubMed] [Google Scholar]
- Clark DA, Beck AT. Cognitive theory and therapy of anxiety and depression: convergence with neurobiological findings. Trends in Cognitive Sciences. 2010;14:418–424. doi: 10.1016/j.tics.2010.06.007. [DOI] [PubMed] [Google Scholar]
- Clark DM, Ehlers A, McManus F, Hackmann A, Fennell M, Campbell H, … Louis B. Cognitive therapy versus fluoxetine in generalized social phobia: a randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology. 2003;71:1058–1067. doi: 10.1037/0022-006X.71.6.1058. [DOI] [PubMed] [Google Scholar]
- Cisler JM, Olatunji BO, Feldner MT, Forsyth JP. Emotion regulation and the anxiety disorders: An integrative review. Journal of Psychopathology and Behavioral Assessment. 2010;32:68–82. doi: 10.1007/s10862-009-9161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Maidenberg E, Bystritsky A. Brief cognitive-behavioral versus nondirective therapy for panic disorder. Journal of Behavior Therapy and Experimental Psychiatry. 1995;26:113–120. doi: 10.1016/0005-7916(95)00003-i. [DOI] [PubMed] [Google Scholar]
- Comer JS, Blanco C, Hasin DS, Liu SM, Grant BF, Turner JB, Olfson M. Health-related quality of life across the anxiety disorders. The Journal of Clinical Psychiatry. 2011;72:43–50. doi: 10.4088/JCP.09m05094blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottraux J, Note I, Albuisson E, Yao SN, Note B, Mollard E, … Coudert AJ. Cognitive behavior therapy versus supportive therapy in social phobia: A randomized controlled trial. Psychotherapy and Psychosomatics. 2000;69:137–146. doi: 10.1159/000012382. [DOI] [PubMed] [Google Scholar]
- Cottraux J, Note I, Yao SN, de Mey-Guillard C, Bonasse F, Djamoussian D, … Chen Y. Randomized controlled comparison of cognitive behavior therapy with Rogerian supportive therapy in chronic post-traumatic stress disorder: A 2-year follow-up. Psychotherapy and Psychosomatics. 2008;77:101–110. doi: 10.1159/000112887. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, Huibers MJ. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta-analytic update of the evidence. World Psychiatry. 2016;15:245–258. doi: 10.1002/wps.20346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Cristea IA, Weitz E, Gentili C, Berking M. The effects of cognitive and behavioural therapies for anxiety disorders on depression: A meta-analysis. Psychological Medicine. 2016;46:3451–3462. doi: 10.1017/S0033291716002348. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Gentili C, Banos RM, Garcia-Campayo J, Botella C, Cristea IA. Relative effects of cognitive and behavioral therapies on generalized anxiety disorder, social anxiety disorder and panic disorder: A meta-analysis. Journal of Anxiety Disorders. 2016;43:79–89. doi: 10.1016/j.janxdis.2016.09.003. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G. Psychological treatment of generalized anxiety disorder: A meta-analysis. Clinical Psychology Review. 2014;34:130–140. doi: 10.1016/j.cpr.2014.01.002. [DOI] [PubMed] [Google Scholar]
- Davidson JT, Foa EB, Huppert JD, Keefe FJ, Franklin ME, Compton JS, … Gadde KM. Fluoxetine, comprehensive cognitive behavioral therapy, and placebo in generalized social phobia. Archives of General Psychiatry. 2004;61:1005–1013. doi: 10.1001/archpsyc.61.10.1005. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, Hackmann A, Grey N, Wild J, Liness S, Albert I, … Clark DM. A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry. 2014;171:294–304. doi: 10.1176/appi.ajp.2013.13040552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feifel D. The use of placebo-controlled clinical trials for the approval of psychiatric drugs. Psychiatry (Edgmont) 2009;6:41–43. [PMC free article] [PubMed] [Google Scholar]
- Fernandez E, Salem D, Swift JK, Ramtahal N. Meta-analysis of dropout from cognitive behavioral therapy: Magnitude, timing, and moderators. Journal of Consulting and Clinical Psychology. 2015;83:1108–1122. doi: 10.1037/ccp0000044. [DOI] [PubMed] [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, … Simpson HB. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162:151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ, … Clary CM. Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. Journal of Clinical Psychiatry. 2002;63:138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- Greenberg RP, Constantino MJ, Bruce N. Are patient expectations still relevant for psychotherapy process and outcome? Clinical Psychology Review. 2006;26:657–678. doi: 10.1016/j.cpr.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Hans E, Hiller W. A meta-analysis of nonrandomized effectiveness studies on outpatient cognitive behavioral therapy for adult anxiety disorders. Clinical Psychology Review. 2013;33:954–964. doi: 10.1016/j.cpr.2013.07.003. [DOI] [PubMed] [Google Scholar]
- Hedges L, Olkin I. Statistical Methods for Meta-analysis. Amsterdam: The Netherlands: Academic Press; 1985. [Google Scholar]
- Hedman E, Mörtberg E, Hesser H, Clark DM, Lekander M, Andersson E, Ljótsson B. Mediators in psychological treatment of social anxiety disorder: Individual cognitive therapy compared to cognitive behavioral group therapy. Behaviour Research and Therapy. 2013;51:696–705. doi: 10.1016/j.brat.2013.07.006. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, Holt CS, Welkowitz LA, … Klein DF. Cognitive behavioral group therapy vs phenelzine therapy for social phobia: 12-week outcome. Archives of General Psychiatry. 1998;55:1133–1141. doi: 10.1001/archpsyc.55.12.1133. [DOI] [PubMed] [Google Scholar]
- Hendriks SM, Spijker J, Licht CM, Hardeveld F, de Graaf R, Batelaan NM, … Beekman AT. Long-term disability in anxiety disorders. BMC Psychiatry. 2016;16:248. doi: 10.1186/s12888-016-0946-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J, Altman DG. Chapter 8: Assessing risk of bias in included studies. Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0. 2008 Retrieved from http://www.cochrane-handbook.org.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ: British Medical Journal. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive processes during fear acquisition and extinction in animals and humans: Implications for exposure therapy of anxiety disorders. Clinical Psychology Review. 2008;28:199–210. doi: 10.1016/j.cpr.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Asmundson GJ, Beck AT. The science of cognitive therapy. Behavior Therapy. 2013;44:199–212. doi: 10.1016/j.beth.2009.01.007. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research. 2012;36:427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J. PsycCRITIQUES—Contemporary Psychology: APA Review of Books. 2. Vol. 60. New York, NY: Routledge; 2015. The strawman debate continues. Review of B. E. Wampold and Z. E. Imel’s book The Great Psychotherapy Debate: The Evidence for What Makes Psychotherapy Work; p. 8. [Google Scholar]
- Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. The Journal of Clinical Psychiatry. 2008;69:621–632. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Wu JQ, Boettcher H. Effect of cognitive-behavioral therapy for anxiety disorders on quality of life: A meta-analysis. Journal of Consulting and Clinical Psychology. 2014;82:375–391. doi: 10.1037/a0035491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48:9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, Simpson TL. Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81:394–404. doi: 10.1037/a0031474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21:169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Greenberg PE. The economic burden of anxiety and stress disorders. In: Davis KL, Charney D, Coyle JT, Nemeroff C, editors. Neuropsychopharmacology: The Fifth Generation of Progress. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2002. pp. 981–992. [Google Scholar]
- Khan A, Kolts RL, Rapaport MH, Krishnan KRR, Brodhead AE, Brown WA. Magnitude of placebo response and drug–placebo differences across psychiatric disorders. Psychological Medicine. 2005;35:743–749. doi: 10.1017/s0033291704003873. [DOI] [PubMed] [Google Scholar]
- Laughren TP. The scientific and ethical basis for placebo-controlled trials in depression and schizophrenia: an FDA perspective. European Psychiatry: The Journal of the Association of European Psychiatrists. 2001;16:418–423. doi: 10.1016/s0924-9338(01)00600-9. [DOI] [PubMed] [Google Scholar]
- Lindsay M, Crino R, Andrews G. Controlled trial of exposure and response prevention in obsessive-compulsive disorder. The British Journal of Psychiatry. 1997;171:135–139. doi: 10.1192/bjp.171.2.135. [DOI] [PubMed] [Google Scholar]
- Lucas RA. A comparative treatment outcome study of social phobia. Dissertation Abstracts International. 1994;54:6465. [Google Scholar]
- Laynard R, Clark D, Knapp M, Mayraz G. Cost-benefit analysis of psychological therapy. National Institute Economic Review. 2007;202:90–98. [Google Scholar]
- Markowitz JC, Petkova E, Neria Y, Van Meter PE, Zhao Y, Hembree E, … Marshall RD. Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry. 2015;172:430–440. doi: 10.1176/appi.ajp.2014.14070908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: A controlled study. Archives of General Psychiatry. 1998;55:317–325. doi: 10.1001/archpsyc.55.4.317. [DOI] [PubMed] [Google Scholar]
- McDonagh A, Friedman M, McHugo G, Ford J, Sengupta A, Mueser K, … Descamps M. Randomized trial of cognitive-behavioral therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73:515–524. doi: 10.1037/0022-006X.73.3.515. [DOI] [PubMed] [Google Scholar]
- Mayo-Wilson E, Dias S, Mavranezouli I, Kew K, Clark DM, Ades AE, Pilling S. Psychological and pharmacological interventions for social anxiety disorder in adults: a systematic review and network meta-analysis. The Lancet Psychiatry. 2014;1:368–376. doi: 10.1016/S2215-0366(14)70329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miettinen O, Nurminen M. Comparative analysis of two rates. Statistics in Medicine. 1985;4:213–226. doi: 10.1002/sim.4780040211. [DOI] [PubMed] [Google Scholar]
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an african refugee settlement. Journal of Consulting and Clinical Psychology. 2004;72:579–587. doi: 10.1037/0022-006X.72.4.579. [DOI] [PubMed] [Google Scholar]
- Nixon RD. Cognitive processing therapy versus supportive counseling for acute stress disorder following assault: A randomized pilot trial. Behavior Therapy. 2012;43:825–836. doi: 10.1016/j.beth.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Nordahl HM, Vogel PA, Morken G, Stiles TC, Sandvik P, Wells A. Paroxetine, cognitive therapy or their combination in the treatment of social anxiety disorder with and without avoidant personality disorder: A randomized clinical trial. Psychotherapy and Psychosomatics. 2016;85:346–356. doi: 10.1159/000447013. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review. 2007;27:572–581. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Olthuis JV, Watt MC, Bailey K, Hayden JA, Stewart SH. Therapist-supported internet cognitive–behavioural therapy for anxiety disorders in adults. Cochrane Database of Systematic Reviews. 2015 doi: 10.1002/14651858.CD011565. Art. No.: CD011565. [DOI] [PubMed] [Google Scholar]
- Ong CW, Clyde JW, Bluett EJ, Levin ME, Twohig MP. Dropout rates in exposure with response prevention for obsessive-compulsive disorder: What do the data really say? Journal of Anxiety Disorders. 2016;40:8–17. doi: 10.1016/j.janxdis.2016.03.006. [DOI] [PubMed] [Google Scholar]
- Oosterbaan DB, van Balkom AM, Spinhoven P, van Oppen P, van Dyck R. Cognitive therapy versus moclobemide in social phobia: A controlled study. Clinical Psychology & Psychotherapy. 2001;8:263–273. [Google Scholar]
- Öst LG, Havnen A, Hansen B, Kvale G. Cognitive behavioral treatments of obsessive–compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clinical Psychology Review. 2015;40:156–169. doi: 10.1016/j.cpr.2015.06.003. [DOI] [PubMed] [Google Scholar]
- Ougrin D. Efficacy of exposure versus cognitive therapy in anxiety disorders: systematic review and meta-analysis. BMC Psychiatry. 2011;11:200. doi: 10.1186/1471-244X-11-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompoli A, Furukawa TA, Imai H, Tajika A, Efthimiou O, Salanti G. Psychological therapies for panic disorder with or without agoraphobia in adults: A network meta-analysis. The Cochrane Library. 2016;4:CD011004. doi: 10.1002/14651858.CD011004.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch SM, King AP, Abelson J, Tuerk PW, Smith E, Rothbaum BO, … Liberzon I. Biological and symptom changes in posttraumatic stress disorder treatment: A randomized clinical trial. Depression and Anxiety. 2015;32:204–212. doi: 10.1002/da.22331. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Gaston JE, Abbott MJ. Testing the efficacy of theoretically derived improvements in the treatment of social phobia. Journal of Consulting and Clinical Psychology. 2009;77:317–327. doi: 10.1037/a0014800. [DOI] [PubMed] [Google Scholar]
- Resick PA, Wachen JS, Mintz J, Young-McCaughan S, Roache JD, Borah AM, … Peterson AL. A randomized clinical trial of group cognitive processing therapy compared with group present-centered therapy for PTSD among active duty military personnel. Journal of Consulting and Clinical Psychology. 2015;83:1058–1068. doi: 10.1037/ccp0000016. [DOI] [PubMed] [Google Scholar]
- Rosellini A, Boettcher H, Brown T, Barlow DH. A transdiagnostic temperament-phenotype profile approach to emotional disorder classification. An update. Psychopathology Review. 2015;2:110–128. doi: 10.5127/pr.036014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, … Bernardy NC. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a Department of Veterans Affairs cooperative study. Archives of General Psychiatry. 2003;60:481–489. doi: 10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, … Bernardy N. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. JAMA. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Sharp DM, Power KG, Simpson RJ, Swanson V, Moodie E, Anstee JA, Ashford JJ. Fluvoxamine, placebo, and cognitive behaviour therapy used alone and in combination in the treatment of panic disorder and agoraphobia. Journal of Anxiety Disorders. 1996;10:219–242. [Google Scholar]
- Smits JAJ, Hofmann SG. A meta-analytic review of the effects of psychotherapy control conditions for anxiety disorders. Psychological Medicine. 2009;39:229–239. doi: 10.1017/S0033291708003498. [DOI] [PubMed] [Google Scholar]
- Smits JA, Julian K, Rosenfield D, Powers MB. Threat reappraisal as a mediator of symptom change in cognitive-behavioral treatment of anxiety disorders: A systematic review. Journal of Consulting and Clinical Psychology. 2012;80:624–635. doi: 10.1037/a0028957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JJ, Powers MB, Buxkamper R, Telch MJ. The efficacy of videotape feedback for enhancing the effects of exposure-based treatment for social anxiety disorder: A controlled investigation. Behaviour Research and Therapy. 2006;44:1773–1785. doi: 10.1016/j.brat.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Stein DJ, Fineberg NA, Bienvenu OJ, Denys D, Lochner C, Nestadt G, … Phillips KA. Should OCD be classified as an anxiety disorder in DSM-V? Depression and Anxiety. 2010;27:495–506. doi: 10.1002/da.20699. [DOI] [PubMed] [Google Scholar]
- Sugarman MA, Kirsch I, Huppert JD. Obsessive-compulsive disorder has a reduced placebo (and antidepressant) response compared to other anxiety disorders: A meta-analysis. Journal of Affective Disorders. 2017;218:217–226. doi: 10.1016/j.jad.2017.04.068. [DOI] [PubMed] [Google Scholar]
- Surís A, Link-Malcolm J, Chard K, Ahn C, North C. A randomized clinical trial of cognitive processing therapy for veterans with PTSD related to military sexual trauma. Journal of Traumatic Stress. 2013;26:28–37. doi: 10.1002/jts.21765. [DOI] [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Jacob RG. Social phobia: A comparison of behavior therapy and atenolol. Journal of Consulting and Clinical Psychology. 1994;62:350–358. doi: 10.1037//0022-006x.62.2.350. [DOI] [PubMed] [Google Scholar]
- Wampold BE, Minami T, Tierney SC, Baskin TW, Bhati KS. The placebo is powerful: Estimating placebo effects in medicine and psychotherapy from randomized clinical trials. Journal of Clinical Psychology. 2005;61:835–854. doi: 10.1002/jclp.20129. [DOI] [PubMed] [Google Scholar]
- Wampold BE, Imel ZE. The great psychotherapy debate: The evidence for what makes psychotherapy work. New York, NY: Routledge; 2015. [Google Scholar]
- Watts SE, Turnell A, Kladnitski N, Newby JM, Andrews G. Treatment-as-usual (TAU) is anything but usual: A meta-analysis of CBT versus TAU for anxiety and depression. Journal of Affective Disorders. 2015;175:152–167. doi: 10.1016/j.jad.2014.12.025. [DOI] [PubMed] [Google Scholar]
- Whittal ML, Woody SR, McLean PD, Rachman SJ, Robichaud M. Treatment of obsessions: A randomized controlled trial. Behaviour Research and Therapy. 2010;48:295–303. doi: 10.1016/j.brat.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Rothbaum BO, Feeny NC. PTSD not an anxiety disorder? DSM committee proposal turns back the hands of time. Depression and Anxiety. 2011;28:853–856. doi: 10.1002/da.20899. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.