Abstract
Background
Anxiety and depression are commonly comorbid with each other, with anxiety often temporally preceding the development of depression. Although increasingly research has begun to investigate the role of sleep problems in depression, no study has examined insomnia as a mediator in the longitudinal relationship between anxiety and subsequent depression.
Methods
The current study utilizes data from Waves I, II, and IV of the National Longitudinal Study of Adolescent to Adult Health, a nationally representative prospective study conducted over a 14-year period (n = 20,745, 50.5% female, M age at Wave I = 16.20). Participants completed portions of the Center for Epidemiologic Studies Depression Scale (CES-D) at Waves I and IV to assess depressive symptoms, a six-item anxiety measure at Wave I, and three items assessing insomnia, sleep quality, and sleep duration at Wave II.
Results
Structural equation modeling indicated that insomnia and unrestful sleep significantly mediated the relationship between anxiety and subsequent depression. The relationship between anxiety and depression was not significantly mediated by sleep duration.
Conclusions
Findings suggest that anxiety may increase risk for the development of later depression through insomnia.
Keywords: Anxiety/Anxiety Disorders, Depression, Sleep Disorders, Child/Adolescent, Mood Disorders
Introduction
Depression and anxiety disorders are commonly comorbid with each other, with estimates of current and lifetime comorbidity often among the highest of any disorders (Avenevoli, Stolar, Li, Dierker, & Merikangas, 2001; Brown, Campbell, Lehman, Grisham, & Mancill, 2001; Yorbik, Birmaher, Axelson, Williamson, & Ryan, 2004). Between 27% and 77% of individuals with a principal diagnosis of an anxiety disorder meet lifetime criteria for depression (Brown et al., 2001). There is reason to believe that anxiety functions as a direct risk factor for the development of later depression. Anxiety often temporally precedes depression (Kaufman & Charney, 2000; Starr, Hammen, Connolly, & Brennan, 2014) and predicts later depression both longitudinally and within daily patterns (Cole, Peeke, Martin, Truglio, & Seroczynski, 1998; Starr & Davila, 2012b). Most anxiety disorders have average ages of onset in childhood, with rates of anxiety-depression comorbidity substantially increasing during later adolescence and young adulthood (Merikangas et al., 2010; Wittchen, Kessler, Pfister, Höfler, & Lieb, 2000). Although the association between anxiety and depression is likely bidirectional (Jacobson & Newman, 2017), converging evidence suggests that for a substantial portion of comorbid youth, anxiety increases risk for depression under a likely “direct causation” model (Cummings, Caporino, & Kendall, 2014; Mathew, Pettit, Lewinsohn, Seeley, & Roberts, 2011). However, little is known about processes that may underlie this transition. A small emerging literature has begun to pinpoint factors such as interpersonal dysfunction, negative anxiety response styles, rumination, attentional biases, and behavioral avoidance (Jacobson & Newman, 2014; Jacobson & Newman, 2016; Price et al., 2016; Starr et al., 2014; Starr, Stroud, & Li, 2016) as processes that may bridge anxiety with depression during adolescence, but more work is needed to identify other potential mechanisms.
Strong evidence suggests that sleep problems may play a critical role in both depression and anxiety (Baglioni et al., 2011; Benca, Obermeyer, Thisted, & Gillin, 1992; Dahl & Harvey, 2007). Sleep disturbances are present in high rates in individuals with anxiety and depressive disorders in both adults and children (Johnson, Chilcoat, & Breslau, 2000; van Mill, Hoogendijk, Vogelzangs, van Dyck, & Penninx, 2010). Although research has more recently begun to examine sleep in the context of both anxiety and depression, none have specifically examined the role of insomnia in the temporal relationship between the two. Research on the directionality of sleep and anxiety has been somewhat mixed, although evidence suggests that anxiety may precede sleep problems. Data from a large-scale longitudinal study suggest that generalized anxiety may predict increases in sleep problems over time (Shanahan, Copeland, Angold, Bondy, & Costello, 2014). Consistent with a view of insomnia as an intervening link in the temporal relationship between anxiety and depression, Ohayon and Roth (2003) found that while insomnia primarily preceded a diagnosis of mood disorder or appeared concurrently, in the case of anxiety disorders, insomnia appeared mostly either following anxiety or concurrently rather than before. Another study found similar results, with anxiety disorders preceding insomnia in the majority of cases among adolescents with comorbid disorders; further, although prior anxiety disorder was associated with increased risk of insomnia, prior insomnia was not significantly associated with anxiety onset (Johnson, Roth, & Breslau, 2006). Anxious individuals have been found to engage in worry about sources of their anxiety as well as about sleep, which may contribute to sleep difficulties (Kelly, 2002; McCann & Stewin, 1988). Generalized anxiety is associated with disrupted sleep, including longer sleep latency and decreased percentage of deep sleep (Alfano, Reynolds, Scott, Dahl, & Mellman, 2013; Fuller, Waters, Binks, & Anderson, 1997). Anxious individuals are more likely to engage in repetitive, ruminative thinking regarding anxiety symptoms, which may be particularly disruptive to sleep (Starr & Davila, 2012a).
Although sleep disturbance is a criterion for depression, insomnia is also increasingly being conceptualized as a mechanism in depression etiology (Baglioni et al., 2011; Buysse, Germain, Hall, Monk, & Nofzinger, 2012). A large body of literature has consistently supported insomnia and sleep problems as risk factors for later depression in both children and adults (Baglioni et al., 2011; Gregory, Rijsdijk, Lau, Dahl, & Eley, 2009; Roane & Taylor, 2008). In a systematic review, Alvaro and colleagues (2013) found evidence for bidirectionality of sleep disturbances with depression, although insomnia appeared to be a stronger and more consistent predictor of subsequent depression than depression is of subsequent insomnia. A meta-analysis found that sleep disturbance significantly predicted development of depression in adolescents, providing further support for sleep disturbance as a risk factor (Lovato & Gradisar, 2014). Individuals with major depression and insomnia symptoms report greater risk of depression recurrence and higher rates of comorbid anxiety than those without insomnia (Soehner & Harvey, 2012). Several theories have been proposed to explain why insomnia may lead to increased risk for depression, including disrupted emotion regulation and impaired reward processing (Harvey, Murray, Chandler, & Soehner, 2011; Luking, Pagliaccio, Luby, & Barch, 2016).
Thus, insomnia appears to play a role in the transition from anxiety to depression. However, limitations of existing studies include employment of cross-sectional and retrospective designs that limit both interpretability as well as strength of conclusions. Longitudinal studies may be especially important in increasing understanding of these processes. Most anxiety disorders typically develop by late childhood and early adolescence, whereas depressive symptoms increase in frequency during adolescence into adulthood (Nolen-Hoeksema & Girgus, 1994; Wittchen et al., 2000). Sleep patterns also alter dramatically during adolescence, driven by physiological as well as environmental changes (Dahl & Harvey, 2007; Dahl & Lewin, 2002). Thus, an examination of longitudinal associations between anxiety and depression may be particularly useful in understanding how this transition occurs.
In the current study, we investigated the relationship between anxiety and depressive symptoms, focusing on insomnia as a potential mediator in this association, utilizing a nationally representative longitudinal sample of adolescents followed for over a decade. As symptoms of insomnia can include both difficulty initiating or maintaining sleep and poor sleep quality (unrestful sleep) (American Psychiatric Association, 2013), we examined both in the present study. Additionally, as evidence suggests that sleep quality and duration may have differential associations with psychological outcomes (Pilcher, Ginter, & Sadowsky, 1997), we also examined sleep duration separately. We hypothesized that the relationship between anxiety and subsequent depressive symptoms would be mediated by sleep problems (insomnia, unrestful sleep, and decreased sleep duration).
Material and Methods
Participants
Data came from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative prospective study (Harris et al., 2009). The study used a clustered sampling design based on a stratified sample of 80 high schools and 52 paired middle schools. Clusters were sampled with unequal probability of selection. This study used data from in-home questionnaires, which were collected in four waves. As we were interested in examining the long-term effect of anxiety on depressive symptoms in adulthood, the current study uses Waves I (W1), II (W2), and IV (W4) of Add Health’s restricted-access dataset: W1 was collected during 1994-1995; W2 occurred during 1995-1996; W4 was collected during 2007-2008. Of the full sample of 20,745 adolescents who participated in W1, 28.9% (n = 6009) were missing in W2 and 24.3% (n = 5046) participants were non-responders in W4. Table 1 displays demographic information of the sample at baseline.
Table 1.
Demographics Information at Wave I
| Female | 50.5% |
| Male | 49.5% |
| Ethnicity | |
| Caucasian | 62% |
| African American | 23% |
| American Indian | 4% |
| Asian/Pacific Islander | 8% |
| Other | 9% |
| M (SD) | |
| Age | 16.2 (1.7) |
| SES | .06 (.8) |
Measures
Anxiety Symptoms
Anxiety was assessed at W1 with six items constituting a physiological symptom-based measure, as in prior research (see Jacobson & Newman, 2014; Jacobson & Newman, 2016; Noel, Groenewald, Beals-Erickson, Gebert, & Palermo, 2016). Table 1 lists study items. Internal consistency for the items in the current sample was α = .61. Internal consistency is comparable to previous studies that have grouped the same items together into a single anxiety factor (Jacobson & Newman, 2016; Noel et al., 2016).
Depressive Symptoms
Depressive symptoms at W1 and W4 were measured using portions of the adapted Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), a brief self-report questionnaire designed to measure depressive symptoms in the general population. As unequal numbers of items from the CES-D were administered across waves, in the current study we used only items that were administered in both W1 and W4. We also excluded items that conceptually overlap with sleep [“You felt that you were too tired to do things”] and anxiety [“You were bothered by things that usually don’t bother you”]. Previous examinations of the reduced scale supported a single factor structure with good internal consistency (Catrett & Gaultney, 2009; Jacobson & Newman, 2014). Additionally, combining the reduced scale with anxiety items yielded two distinct depression and anxiety factors (Jacobson & Newman, 2014). Internal consistency in this sample was good for W1 and W4 (α = .87 and .84, respectively).
Sleep Variables
Sleep variables were measured at W2 with one item each assessing difficulty with sleep initiation or maintenance (insomnia) and unrestful sleep. An additional item assessed typical total sleep time (TST) [Table 2]. Previous studies with the Add Health dataset have used both the single insomnia item and TST item to operationalize insomnia and sleep duration, respectively (see Asarnow, McGlinchey, & Harvey, 2014; Roane & Taylor, 2008; Wong, Robertson, & Dyson, 2015).
Table 2.
Relevant study variables
| Measure | Time Frame | Item | Scale | Waves |
|---|---|---|---|---|
| CES-D | Past week | You were happy. | 0 (never) - 3 (most or all of the time) | 1, 2, 4 |
| You could not shake the blues. | 1, 2, 4 | |||
| You enjoyed life. | 1, 2, 4 | |||
| You felt depressed. | 1, 2, 4 | |||
| You felt that you were just as good as other people. | 1, 2, 4 | |||
| You felt sad. | 1, 2, 4 | |||
| You had trouble keeping your mind on what you were doing. | 1, 2, 4 | |||
| You felt that people disliked you. | 1, 2, 4 | |||
|
| ||||
| Anxiety | Past 12 months | Feeling hot all over suddenly, for no reason | 0 (never) - 4 (every day) | 1, 2 |
| Cold sweats | 1, 2 | |||
| Chest pains | 1, 2 | |||
| Fearfulness | 1, 2 | |||
| A stomach ache or an upset stomach | 1, 2 | |||
| Trouble relaxing | 1, 2 | |||
|
| ||||
| Sleep | Past 12 months | Trouble falling asleep or staying asleep | 0 (never) - 4 (every day) | 1, 2, 4a |
| Waking up feeling tired | 1, 2 | |||
| How many hours of sleep do you usually get? | 1, 2 | |||
|
| ||||
| General Health | Past 12 months | In general, how is your health? | 1 (excellent) – 5 (poor) | 1 |
Time frame for the item administered in Wave IV is past four weeks
Covariates
As the anxiety scale is comprised of physiological symptom-based items that could feasibly be indicative of physical health problems, to partial out the effects of this potential confound, a single item assessing self-perceived general health at W1 was also included as a covariate. W1 depressive symptoms, gender (1 = male, 2 = female), age, and socioeconomic status (SES) were also entered as controls. SES was a composite of mother and father education and family income.
Statistical Analysis
We conducted structural equation modeling in Mplus 7.4. Prior to each analysis, the model’s assumptions were tested. The data met statistical assumptions for multivariate normality, linearity, and non-multicollinearity. Table 3 displays Pearson’s product moment correlations, means, and standard deviations for study variables. We first conducted a confirmatory factor analysis (CFA) to test the model fit of the anxiety and depression latent variables. A structural model was then examined that included the three sleep items as mediators, insomnia, unrestful sleep, and TST. The model included paths from anxiety at W1 predicting insomnia, unrestful sleep, and TST at W2, to depressive symptoms at W4 as the outcome variable. Anxiety was modeled as both a direct and indirect predictor of depressive symptoms through insomnia, unrestful sleep, and TST. W1 Depression was included as a predictor of W4 depression to control for the influence of prior depression. Gender, SES, age, and health were also included as controls. Robust maximum likelihood (MLR) estimation method was used as it provides standard errors robust to unmodeled nonnormality of data (Muthén & Muthén, 2007). Full-information maximum-likelihood (FIML) estimation was used to estimate missing values (Arbuckle, Marcoulides, & Schumacker, 1996).
Table 3.
Pearson’s product moment correlations, means, and standard deviations for relevant study variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | M | SD | |
|---|---|---|---|---|---|---|---|---|---|
| 1. W1 Depressive Symptoms | 12.61 | 8.35 | |||||||
| 2. W1 Anxiety Symptoms | .47* | 2.78 | 2.11 | ||||||
| 3. W2 Insomnia | .27* | .28* | 0.97 | 0.96 | |||||
| 4. W2 TST | −.11* | −.06* | −.14* | 7.58 | 1.41 | ||||
| 5. W2 Unrestful Sleep | .23* | .22* | .29* | −.12* | 1.49 | 1.11 | |||
| 6. W4 Depressive Symptoms | .38* | .19* | .17* | −.05* | .16* | 5.73 | 5.37 | ||
| 7. W4 Insomnia | .14* | .11* | .18* | −.05* | .10* | .35* | 1.15 | 1.34 |
p < .01
Practical indices of goodness of fit were evaluated in place of the chi-square statistic, as chi-square values are highly influenced by large sample sizes. Model fit was evaluated based on the following criteria (Kline, 2015): Tucker-Lewis Index (TLI) ≥ .90, with > .95 preferred, Root Mean Squared Error of Approximation (RMSEA) and Standardized Root Mean Square Residual (SRMR) < .05. If model fit was less than acceptable, modification indices were examined for correlated error terms that were conceptually justified and would enhance model fit.
Results
A CFA was conducted to examine the factor structure of the W1 depression and anxiety indicators. Results showed adequate fit to the data (χ2 (102) = 5147.26, p < .001, TLI = .917, RMSEA = .049, SRMR = .037), with all factor loadings significant at p < .001. After examination of modification indices, the residuals of select items on the CES-D were correlated to improve model fit.
We then tested the structural model, examining whether insomnia, unrestful sleep, and TST at W2 significantly mediated the relationship between W1 anxiety and W4 depressive symptoms, controlling for W1 depression, general health, gender, age, and SES [Figure 1]. The resulting model showed adequate fit to the data: χ2(350) = 8905.44, p < .001, TLI = .90, RMSEA = .03, SRMR = .03. Supporting our hypothesis, the indirect effect of W1 anxiety to W4 depressive symptoms through insomnia at W2 was significant and positive (indirect effect = .020, SE = .006, p < .001, 95% CI [.009, .031]). Unrestful sleep also significantly mediated the relationship between W1 anxiety and W4 depressive symptoms (indirect effect = .019, SE = .004, p < .001, 95% CI [.010, .027]). The residual direct effect showed that anxiety was not significant in predicting later depressive symptoms (β = .004, SE = .022, p = .844), suggesting that insomnia and unrestful sleep significantly mediated the relationship between anxiety and subsequent depressive symptoms. W1 anxiety predicted TST at W2, but TST did not predict depressive symptoms at W4. TST was not significant in mediating the relationship between anxiety and depressive symptoms (indirect effect = .00, SE= .002, p = .790, 95% CI [-.004, .003]).
Figure 1.
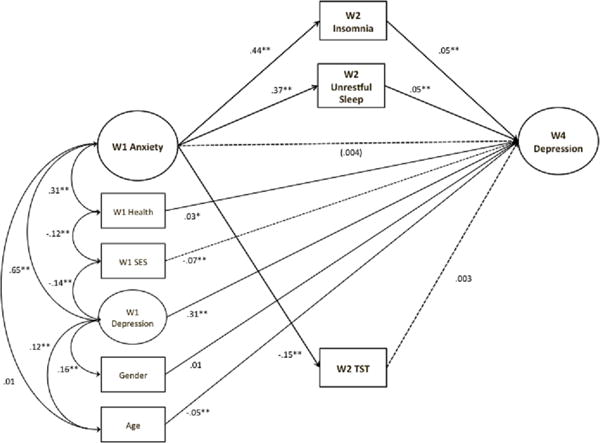
Structural equation modeling examining insomnia, unrestful sleep, and TST as mediators of the relationship between anxiety and later depression. Unstandardized coefficients are presented. χ2(350) = 8905.44, p < .001, TLI = .90, RMSEA = .03, SRMR = .03.
*p < .01, **p < .001
Note. Manifest indicators and error terms are excluded from the model to enhance ease of interpretation.
As both insomnia and hypersomnia are associated with depression (Liu et al., 2007), we also examined potential non-linear effects of TST. We conducted a separate model, entering both linear and quadratic terms for TST. The resulting model showed adequate fit to the data (χ2(325) = 8329.15, p < .001, TLI = .90, RMSEA = .03, SRMR = .04). Neither the linear term (indirect effect = .001, SE = .001, p = .273, 95% CI [-.001, .004]) nor quadratic term (indirect effect = .002, SE = .001, p = .059, 95% CI [.000, .005]) was significant in mediating the anxiety—depressive symptoms relationship.
Discussion
Using a nationally representative sample, we sought to examine the role of insomnia and TST in mediating the relationship between anxiety in adolescence and depression in adulthood. Consistent with our hypothesis, results provided evidence in support of insomnia as a mediator in the relationship between anxiety and subsequent depressive symptoms. To our knowledge, this is the first study to examine a mediational role of insomnia in the sequential comorbidity of anxiety and later depression. Worrying and catastrophic thinking characteristic of anxiety disorders may contribute to sleep related problems, such as delays in sleep onset (Harvey, 2000; Kelly, 2002). Individuals who are more anxious may be more sensitive to normal disruptions in sleep. The three-factor model of insomnia suggest that over time as sleep problems persist, anxiety over insomnia itself becomes a perpetuating factor (Spielman, Caruso, & Glovinsky, 1987); anxiety may thus increase risk for both emergence and maintenance of insomnia.
In turn, individuals with sleep problems are at greater risk for developing subsequent depression (Baglioni et al., 2011; Roane & Taylor, 2008). Depression has been hypothesized to be a disorder of impaired emotion regulation (Joormann & Gotlib, 2010), with maladaptive emotion regulation more likely to result in increased mood instability and vulnerability to depressed mood (Ehring, Tuschen-Caffier, Schnülle, Fischer, & Gross, 2010; Erk et al., 2010). Sleep plays a crucial role in emotion regulation, with sleep deprivation and restriction associated with subjective reports of increased negative emotionality and affective instability (Dinges et al., 1997; Horne, 1985). Additionally, sleep loss blunts positive benefits associated with rewarding experiences (Zohar, Tzischinsky, Epstein, & Lavie, 2005). Sleep also plays a role in maintaining regulation of physiological reactivity to stress (Buckley & Schatzberg, 2005; Meerlo, Sgoifo, & Suchecki, 2008). Elevated cortisol levels have been found in individuals after partial sleep deprivation, suggesting that disturbances in sleep may increase physiological stress reactivity (Meerlo et al., 2008), potentially impacting individuals’ abilities to successfully cope with stress. It appears that insomnia may decrease adaptive responding to stress and increase emotional dysregulation.
Poor sleep may also negatively influence cognitive processes such as attention, impulse control, and memory. Children experiencing sleep loss or disruptions report difficulties with focused attention and modulating impulses (Dahl, 1996; Dahl, 1999; Wolfson & Carskadon, 1998). Sleep also plays an important role in emotional memory encoding and consolidation (Hu, Stylos-Allan, & Walker, 2006). Although sleep deprivation impairs memory formation generally, encoding of negative memory appears to be more resistant to sleep loss (Yoo, Gujar, Hu, Jolesz, & Walker, 2007), potentially contributing to the decreased recall specificity of positive autobiographical memories compared to negative memories seen in depression (van Vreeswijk & de Wilde, 2004). It is possible that for individuals with anxiety, insomnia further contributes to the predominance of memory encoding and recall for negative events, contributing to greater depressive symptoms over time.
In addition to self-reported insomnia, we also found support for the role of subjective sleep quality as a mediator in the anxiety-depression relationship. Studies using neuroimaging techniques have shown that subjective reports of sleep quality are significantly related to amygdala reactivity as well as to reports of negative affect and stress, suggesting that self-perceived sleep quality may be an indicator of emotional processing efficacy during sleep (Goldstein & Walker, 2014; Prather, Bogdan, & Hariri, 2013). Indeed, subjective poor sleep quality has been found to be associated with increased risk for depression as well as emotion dyregulation (Franzen, Buysse, Rabinovitz, Pollock, & Lotrich, 2010; Mauss, Troy, & LeBourgeois, 2013; Park, Meltzer-Brody, & Stickgold, 2013), independent of disrupted sleep initiation and maintenance. As subjective sleep quality appears to reflect sleep depth and continuity (Argyropoulos et al., 2003), our findings suggest a unique role of perceived sleep quality in the relationship between anxiety and depression.
We did not find evidence for the role of sleep duration in mediating the relationship between anxiety and later depression. This is not entirely surprising as previous research has often failed to find effects of shorter sleep duration, suggesting that self-perceived sleep problems may be more strongly associated with negative outcomes than sleep duration (Asarnow et al., 2014; Pilcher et al., 1997). Individuals suffering from insomnia commonly both under- and over-estimate their own sleep duration, with some evidence suggesting that sleep misperception may occur to a greater degree in individuals with depression (Fernandez-Mendoza et al., 2011; Tsuchiyama, Nagayama, Kudo, Kojima, & Yamada, 2003). Estimates of sleep duration may be influenced by other factors such as mood and impaired cognitive function (Bastien et al., 2003). Further, estimates of one’s typical sleep amount (as in the present study) may be more likely to be influenced by retrospective bias and perception of one’s own sleep difficulties, particularly as sleep problems persist. In contrast, objective shortened sleep duration is associated with greater severity of insomnia as well as risk for depression and poorer treatment outcomes (Fernandez-Mendoza et al., 2015; Troxel et al., 2012; Vgontzas, Fernandez-Mendoza, Liao, & Bixler, 2013). Thus, future studies should examine objective sleep duration in anxiety and depression comorbidity.
Our findings should be considered in context of several limitations. First, despite the heterogeneity of sleep related problems, insomnia and sleep quality were assessed using a single self-report item. Although previous studies using Add Health data have similarly used the same item to measure insomnia (e.g., Jacobson & Newman, 2016; Wong & Brower, 2012), future studies should examine the effect of other forms of sleep difficulties on anxiety and depression using objective measures. Additionally, anxiety and depression symptoms were assessed via self-report. In particular, anxiety was assessed using reported physiological symptoms, which excludes cognitive components of anxiety that may contribute to sleep disruptions. Physiological symptoms may also be indicative of other problems associated with depression, although this is somewhat mitigated in this study by the inclusion of a general health item. Further research should explore potential differential relationships between insomnia and various forms of anxiety. However, despite these limitations in measurement, our findings were robust given the use of a large nationally representative sample.
Although we did not examine whether sleep problems mediate the bidirectional relationships between depression and later anxiety, it is possible that insomnia is a potential mechanism through which this process occurs. Depression has been shown to increase risk for insomnia in adults and adolescents (Roberts & Duong, 2013; Sivertsen et al., 2012). In turn, insomnia and sleep disturbances could feasibly increase anxiety (Gillin, 1998; Jansson-Fröjmark & Lindblom, 2008). Adolescents with sleep disruptions experience more self-reported anxiety as well as greater likelihood of engaging in catastrophizing and rate their worries as more threatening (Talbot, McGlinchey, Kaplan, Dahl, & Harvey, 2010). Although we were not able to examine insomnia as a mediator of the bidirectional relationship due to lack of anxiety data at Wave IV, future studies should seek to clarify and disentangle these potentially bidirectional relationships.
Conclusions
The current study has theoretical and clinical implications for the study and treatment of comorbid anxiety and depression. First, it adds to emerging research on the role of anxiety as a risk factor for later depression, and highlights insomnia as a potential process through which this temporal relationship unfolds. We found significant associations over a decade later, suggesting a continued impact of anxiety on depression that extends from adolescence into adulthood. In addition, our findings build on existing studies on sleep as a transdiagnostic factor for anxiety and depression (Harvey et al., 2011), and further suggest that treatments targeting anxiety may benefit from incorporation of interventions for insomnia and sleep related problems, in order to ameliorate risk for the development of subsequent depression and future impairment.
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Footnotes
Portions of these findings were presented at the 2016 Society for Research on Adolescence Biennial Meeting at Baltimore, MD, USA.
Conflict of Interest: Y. Irina Li, Lisa R. Starr, and Laura Wray-Lake declare that they have no conflict of interest.
Compliance with Ethical Standards
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- Alfano CA, Reynolds K, Scott N, Dahl RE, Mellman TA. Polysomnographic sleep patterns of non-depressed, non-medicated children with generalized anxiety disorder. Journal of affective disorders. 2013;147(1):379–384. doi: 10.1016/j.jad.2012.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- Arbuckle JL, Marcoulides GA, Schumacker RE. Full information estimation in the presence of incomplete data. Advanced structural equation modeling: Issues and techniques. 1996;243:277. [Google Scholar]
- Argyropoulos SV, Hicks JA, Nash JR, Bell CJ, Rich AS, Nutt DJ, Wilson SJ. Correlation of subjective and objective sleep measurements at different stages of the treatment of depression. Psychiatry research. 2003;120(2):179–190. doi: 10.1016/s0165-1781(03)00187-2. [DOI] [PubMed] [Google Scholar]
- Asarnow LD, McGlinchey E, Harvey AG. The effects of bedtime and sleep duration on academic and emotional outcomes in a nationally representative sample of adolescents. Journal of Adolescent Health. 2014;54(3):350–356. doi: 10.1016/j.jadohealth.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avenevoli S, Stolar M, Li J, Dierker L, Merikangas KR. Comorbidity of depression in children and adolescents: Models and evidence from a prospective high-risk family study. Biological psychiatry. 2001;49(12):1071–1081. doi: 10.1016/s0006-3223(01)01142-8. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Riemann D. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. Journal of affective disorders. 2011;135(1):10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Fortier-Brochu É, Rioux I, LeBlanc M, Daley M, Morin CM. Cognitive performance and sleep quality in the elderly suffering from chronic insomnia: relationship between objective and subjective measures. Journal of Psychosomatic Research. 2003;54(1):39–49. doi: 10.1016/s0022-3999(02)00544-5. [DOI] [PubMed] [Google Scholar]
- Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders: a meta-analysis. Archives of General Psychiatry. 1992;49(8):651–668. doi: 10.1001/archpsyc.1992.01820080059010. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of abnormal psychology. 2001;110(4):585. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. The Journal of Clinical Endocrinology & Metabolism. 2005;90(5):3106–3114. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Germain A, Hall M, Monk TH, Nofzinger EA. A neurobiological model of insomnia. Drug Discovery Today: Disease Models. 2012;8(4):129–137. doi: 10.1016/j.ddmod.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catrett CD, Gaultney JF. Possible insomnia predicts some risky behaviors among adolescents when controlling for depressive symptoms. The Journal of genetic psychology. 2009;170(4):287–309. doi: 10.1080/00221320903218331. [DOI] [PubMed] [Google Scholar]
- Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski A. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of consulting and clinical psychology. 1998;66(3):451. doi: 10.1037//0022-006x.66.3.451. [DOI] [PubMed] [Google Scholar]
- Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological bulletin. 2014;140(3):816. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl RE. The impact of inadequate sleep on children’s daytime cognitive function. Paper presented at the Seminars in Pediatric Neurology. 1996 doi: 10.1016/s1071-9091(96)80028-3. [DOI] [PubMed] [Google Scholar]
- Dahl RE. The consequences of insufficient sleep for adolescents: Links between sleep and emotional regulation. Phi Delta Kappan. 1999;80(5):354. [Google Scholar]
- Dahl RE, Harvey AG. Sleep in children and adolescents with behavioral and emotional disorders. Sleep medicine clinics. 2007;2(3):501–511. [Google Scholar]
- Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. Journal of Adolescent Health. 2002;31(6):175–184. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, Pack AI. Cumulative sleepiness, mood disturbance and psychomotor vigilance performance decrements during aweek of sleep restricted to 4-5 hours per night. Sleep: Journal of Sleep Research & Sleep Medicine. 1997 [PubMed] [Google Scholar]
- Ehring T, Tuschen-Caffier B, Schnülle J, Fischer S, Gross JJ. Emotion regulation and vulnerability to depression: spontaneous versus instructed use of emotion suppression and reappraisal. Emotion. 2010;10(4):563. doi: 10.1037/a0019010. [DOI] [PubMed] [Google Scholar]
- Erk S, Mikschl A, Stier S, Ciaramidaro A, Gapp V, Weber B, Walter H. Acute and sustained effects of cognitive emotion regulation in major depression. The Journal of neuroscience. 2010;30(47):15726–15734. doi: 10.1523/JNEUROSCI.1856-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Mendoza J, Calhoun SL, Bixler EO, Karataraki M, Liao D, Vela-Bueno A, Vgontzas AN. Sleep misperception and chronic insomnia in the general population: the role of objective sleep duration and psychological profiles. Psychosomatic medicine. 2011;73(1):88. doi: 10.1097/PSY.0b013e3181fe365a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Mendoza J, Shea S, Vgontzas AN, Calhoun SL, Liao D, Bixler EO. Insomnia and incident depression: role of objective sleep duration and natural history. Journal of sleep research. 2015;24(4):390–398. doi: 10.1111/jsr.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzen PL, Buysse DJ, Rabinovitz M, Pollock BG, Lotrich FE. Poor sleep quality predicts onset of either major depression or subsyndromal depression with irritability during interferon-alpha treatment. Psychiatry research. 2010;177(1):240–245. doi: 10.1016/j.psychres.2009.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller KH, Waters WF, Binks PG, Anderson T. Generalized anxiety and sleep architecture: a polysomnographic investigation. Sleep: Journal of Sleep Research & Sleep Medicine. 1997 doi: 10.1093/sleep/20.5.370. [DOI] [PubMed] [Google Scholar]
- Gillin J. Are sleep disturbances risk factors for anxiety, depressive and addictive disorders? Acta Psychiatrica Scandinavica. 1998;98(393):39–43. doi: 10.1111/j.1600-0447.1998.tb05965.x. [DOI] [PubMed] [Google Scholar]
- Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annual review of clinical psychology. 2014;10:679. doi: 10.1146/annurev-clinpsy-032813-153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory AM, Rijsdijk FV, Lau JY, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep. 2009;32(2):189. doi: 10.1093/sleep/32.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, Udry JR. The national longitudinal study of adolescent health: Research design. 2009 Available at http://www.cpc.unc.edu/projects/addhealth/design.
- Harvey AG. Pre-sleep cognitive activity: A comparison of sleep-onset insomniacs and good sleepers. British Journal of Clinical Psychology. 2000;39(3):275–286. doi: 10.1348/014466500163284. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Murray G, Chandler RA, Soehner A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin Psychol Rev. 2011;31(2):225–235. doi: 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne JA. Sleep function, with particular reference to sleep deprivation. Annals of clinical research. 1985 [PubMed] [Google Scholar]
- Hu P, Stylos-Allan M, Walker MP. Sleep facilitates consolidation of emotional declarative memory. Psychological Science. 2006;17(10):891–898. doi: 10.1111/j.1467-9280.2006.01799.x. [DOI] [PubMed] [Google Scholar]
- Jacobson N, Newman MG. Avoidance mediates the relationship between anxiety and depression over a decade later. Journal of anxiety disorders. 2014;28(5):437–445. doi: 10.1016/j.janxdis.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N, Newman MG. Perceptions of close and group relationships mediate the relationship between anxiety and depression over a decade later. Depression and anxiety. 2016;33(1):66–74. doi: 10.1002/da.22402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N, Newman MG. Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychological bulletin. 2017;143(11):1155. doi: 10.1037/bul0000111. [DOI] [PubMed] [Google Scholar]
- Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. Journal of Psychosomatic Research. 2008;64(4):443–449. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Chilcoat HD, Breslau N. Trouble sleeping and anxiety/depression in childhood. Psychiatry research. 2000;94(2):93–102. doi: 10.1016/s0165-1781(00)00145-1. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. Journal of psychiatric research. 2006;40(8):700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Joormann J, Gotlib IH. Emotion regulation in depression: Relation to cognitive inhibition. Cognition and Emotion. 2010;24(2):281–298. doi: 10.1080/02699930903407948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Charney D. Comorbidity of mood and anxiety disorders. Depression and anxiety. 2000;12(s1):69–76. doi: 10.1002/1520-6394(2000)12:1+<69::AID-DA9>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Kelly WE. Worry and sleep length revisited: Worry, sleep length, and sleep disturbance ascribed to worry. The Journal of genetic psychology. 2002;163(3):296–304. doi: 10.1080/00221320209598685. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford publications; 2015. [Google Scholar]
- Liu X, Buysse DJ, Gentzler AL, Kiss E, Mayer L, Kapornai K, Kovacs M. Insomnia and hypersomnia associated with depressive phenomenology and comorbidity in childhood depression. Sleep. 2007;30(1):83–90. doi: 10.1093/sleep/30.1.83. [DOI] [PubMed] [Google Scholar]
- Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep medicine reviews. 2014;18(6):521–529. doi: 10.1016/j.smrv.2014.03.006. [DOI] [PubMed] [Google Scholar]
- Luking KR, Pagliaccio D, Luby JL, Barch DM. Reward Processing and Risk for Depression Across Development. Trends in cognitive sciences. 2016;20(6):456–468. doi: 10.1016/j.tics.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew A, Pettit J, Lewinsohn P, Seeley J, Roberts R. Co-morbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychological medicine. 2011;41(10):2023–2034. doi: 10.1017/S0033291711000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauss IB, Troy AS, LeBourgeois MK. Poorer sleep quality is associated with lower emotion-regulation ability in a laboratory paradigm. Cognition & emotion. 2013;27(3):567–576. doi: 10.1080/02699931.2012.727783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann SJ, Stewin LL. Worry, anxiety, and preferred length of sleep. The Journal of genetic psychology. 1988;149(3):413–418. doi: 10.1080/00221325.1988.10532169. [DOI] [PubMed] [Google Scholar]
- Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep medicine reviews. 2008;12(3):197–210. doi: 10.1016/j.smrv.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus. Statistical analysis with latent variables Version, 3 2007 [Google Scholar]
- Noel M, Groenewald CB, Beals-Erickson SE, Gebert JT, Palermo TM. Chronic pain in adolescence and internalizing mental health disorders: a nationally representative study. Pain. 2016;157(6):1333–1338. doi: 10.1097/j.pain.0000000000000522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological bulletin. 1994;115(3):424. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. Journal of psychiatric research. 2003;37(1):9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- Park EM, Meltzer-Brody S, Stickgold R. Poor sleep maintenance and subjective sleep quality are associated with postpartum maternal depression symptom severity. Archives of women’s mental health. 2013;16(6):539–547. doi: 10.1007/s00737-013-0356-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. Journal of Psychosomatic Research. 1997;42(6):583–596. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- Prather AA, Bogdan R, Hariri PAR. Impact of sleep quality on amygdala reactivity, negative affect, and perceived stress. Psychosomatic medicine. 2013;75(4):350. doi: 10.1097/PSY.0b013e31828ef15b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RB, Rosen D, Siegle GJ, Ladouceur CD, Tang K, Allen KB, Silk JS. From anxious youth to depressed adolescents: Prospective prediction of 2-year depression symptoms via attentional bias measures. Journal of abnormal psychology. 2016;125(2):267. doi: 10.1037/abn0000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351. [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Duong HT. Depression and insomnia among adolescents: a prospective perspective. Journal of affective disorders. 2013;148(1):66–71. doi: 10.1016/j.jad.2012.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L, Copeland WE, Angold A, Bondy CL, Costello EJ. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(5):550–558. doi: 10.1016/j.jaac.2013.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen B, Salo P, Mykletun A, Hysing M, Pallesen S, Krokstad S, Øverland S. The bidirectional association between depression and insomnia: the HUNT study. Psychosomatic medicine. 2012;74(7):758–765. doi: 10.1097/PSY.0b013e3182648619. [DOI] [PubMed] [Google Scholar]
- Soehner AM, Harvey AG. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: results from a nationally representative sample. Sleep. 2012;35(10):1367. doi: 10.5665/sleep.2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatric Clinics of North America. 1987 [PubMed] [Google Scholar]
- Starr LR, Davila J. Responding to anxiety with rumination and hopelessness: mechanism of anxiety-depression symptom co-occurrence? Cognitive therapy and research. 2012a;36(4):321–337. doi: 10.1007/s10608-011-9363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr LR, Davila J. Temporal patterns of anxious and depressed mood in generalized anxiety disorder: A daily diary study. Behaviour research and therapy. 2012b;50(2):131–141. doi: 10.1016/j.brat.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr LR, Hammen C, Connolly NP, Brennan PA. Does relational dysfunction mediate the association between anxiety disorders and later depression? Testing an interpersonal model of comorbidity. Depression and anxiety. 2014;31(1):77–86. doi: 10.1002/da.22172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr LR, Stroud CB, Li YI. Predicting the transition from anxiety to depressive symptoms in early adolescence: Negative anxiety response style as a moderator of sequential comorbidity. Journal of affective disorders. 2016;190:757–763. doi: 10.1016/j.jad.2015.10.065. [DOI] [PubMed] [Google Scholar]
- Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10(6):831. doi: 10.1037/a0020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Kupfer DJ, Reynolds CF, Frank E, Thase M, Miewald J, Buysse DJ. Insomnia and objectively measured sleep disturbances predict treatment outcome in depressed patients treated with psychotherapy or psychotherapy-pharmacotherapy combinations. The Journal of clinical psychiatry. 2012;73(4):478. doi: 10.4088/JCP.11m07184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuchiyama K, Nagayama H, Kudo K, Kojima K, Yamada K. Discrepancy between subjective and objective sleep in patients with depression. Psychiatry and clinical neurosciences. 2003;57(3):259–264. doi: 10.1046/j.1440-1819.2003.01114.x. [DOI] [PubMed] [Google Scholar]
- van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. The Journal of clinical psychiatry. 2010;71(3):1,478–246. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- van Vreeswijk MF, de Wilde EJ. Autobiographical memory specificity, psychopathology, depressed mood and the use of the Autobiographical Memory Test: A meta-analysis. Behaviour research and therapy. 2004;42(6):731–743. doi: 10.1016/S0005-7967(03)00194-3. [DOI] [PubMed] [Google Scholar]
- Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep medicine reviews. 2013;17(4):241–254. doi: 10.1016/j.smrv.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen HU, Kessler R, Pfister H, Höfler M, Lieb R. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatrica Scandinavica. 2000;102(s406):14–23. [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child development. 1998;69(4):875–887. [PubMed] [Google Scholar]
- Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. Journal of psychiatric research. 2012;46(7):953–959. doi: 10.1016/j.jpsychires.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Robertson GC, Dyson RB. Prospective Relationship Between Poor Sleep and Substance-Related Problems in a National Sample of Adolescents. Alcoholism: Clinical and Experimental Research. 2015;39(2):355–362. doi: 10.1111/acer.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep—a prefrontal amygdala disconnect. Current Biology. 2007;17(20):R877–R878. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Yorbik O, Birmaher B, Axelson D, Williamson DE, Ryan ND. Clinical characteristics of depressive symptoms in children and adolescents with major depressive disorder. The Journal of clinical psychiatry. 2004;65(12):1654–1659. doi: 10.4088/jcp.v65n1210. quiz 1760-1651. [DOI] [PubMed] [Google Scholar]
- Zohar D, Tzischinsky O, Epstein R, Lavie P. The effects of sleep loss on medical residents’ emotional reactions to work events: a cognitive-energy model. Sleep: Journal of Sleep and Sleep Disorders Research. 2005 doi: 10.1093/sleep/28.1.47. [DOI] [PubMed] [Google Scholar]


