Abstract
Background
Malaria, Dengue and Chikungunya are vector borne diseases with shared endemic profiles and symptoms. Coinfections with any of these diseases could have fatal outcomes if left undiagnosed. Understanding the prevalence and distribution of coinfections is necessary to improve diagnosis and designing therapeutic interventions.
Methods
We have carried out a systematic search of the published literature based on PRISMA guidelines to identify cases of Malaria, Dengue and Chikungunya coinfections. We systematically reviewed the literature to identify eligible studies and extracted data regarding cases of coinfection from cross sectional studies, case reports, retrospective studies, prospective observational studies and surveillance reports.
Results
Care full screening resulted in 104 publications that met the eligibility criteria and reported Malaria/Dengue, Dengue/Chikungunya, Malaria/Chikungunya and Malaria/Dengue/Chikungunya coinfections. These coinfections were spread over six geographical locations and 42 different countries and are reported more frequently in the last 15 years possibly due to expanding epidemiology of Dengue and Chikungunya. Few of these reports have also analysed distinguishing features of coinfections. Malaria/Dengue coinfections were the most common coinfection followed by Dengue/Chikungunya, Malaria/Chikungunya and Malaria/Dengue/Chikungunya coinfections. P. falciparum and P. vivax were the commonest species found in cases of malaria coinfections and Dengue serotype-4 commonest serotype in cases of dengue coinfections. Most studies were reported from India. Nigeria and India were the only two countries from where all possible combinations of coinfections were reported.
Conclusion
We have comprehensively reviewed the literature associated with cases of coinfections of three important vector borne diseases to present a clear picture of their prevalence and distribution across the globe. The frequency of coinfections presented in the study suggests proper diagnosis, surveillance and management of cases of coinfection to avoid poor prognosis of the underlying etiology.
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5626-z) contains supplementary material, which is available to authorized users.
Background
In recent years the spread of vector borne diseases has gained concern worldwide, especially in tropical and subtropical regions because of their recurring outbreaks [1]. Some of these diseases have become endemic in many areas causing millions of cases every year [2]. The most common of these diseases includes Malaria, Dengue and Chikungunya spread by mosquito bites. Malaria has been long recognized as a significant public health threat with around 212 million cases reported in 2015 alone [3]. Malaria is caused by five different species of Protozoal parasite, Plasmodium. These include P. falciparum, P. ovale, P. malariae, P. vivax and P. knowlesi that are carried and spread by Anopheles mosquito [4, 5]. Dengue and Chikungunya are caused by viruses named Dengue virus (DENV) and Chikungunya virus (CHIKV) respectively. Both are spread by common mosquito vectors Aedes s p. Dengue viruses have four serotypes DENV-1, 2,3 and 4 [6]. As many as 400 million people are affected with Dengue every year [7]. Chikungunya follows somewhat unique pattern of spread across the world, it has the potential to emerge and re-emerge, drastically affecting a population and then remaining undetected for years [8]. In recent years many tropical countries have seen an unexpected rise and spread in cases of Dengue and Chikungunya [9].
These three vector borne diseases share an overlapping epidemic pattern with most cases reported from tropical regions of the world. Several studies have been published reporting co-circulation of Malaria, Dengue and Chikungunya [10, 11]. Apart from shared endemicity, the three diseases also share similar clinical presentation with febrility as the most common symptom. There are several distinguishing features also, like periodic increase and decrease of fever in Malaria, hemorrhagic conditions and depletion of platelet count in Dengue and severe arthralgia in case of Chikungunya infection [12, 13]. The cumulative burden of these infections has increased in recent times with frequent outbreak of Dengue and Chikungunya being reported from several parts of the world. Global travel and rapid urbanisation are important factors that have contributed in expansion of disease endemicity by introducing the vector population to exotic surroundings [14].
Simultaneous infections with more than one infectious agent complicate the diagnosis and course of treatment available. Due to the similar nature of initial symptoms for Malaria, Dengue and Chikungunya and overlapping endemicity, misdiagnosis of dual infection as monoinfection is a real possibility. Indeed several reports have been published reporting such scenarios. These arthropod borne diseases affect some of the poorest countries and in resource poor settings; clinician might rely on symptoms and endemicity for diagnosis, which might lead to underdiagnosis of cocirculating pathogens [15]. Despite similar clinical presentation the course of treatment is entirely different for all three diseases. Malaria is treated using antimalarial drugs. In case of Dengue and Chikungunya no vaccine or drug is available and clinicians rely on supportive therapy [13, 16]. Any delay in either diagnosis or start of therapy for any of these infections could have fatal outcomes. Also, there is lack of sufficient information on how concurrent infections affect disease severity and outcome. Several studies have been published that report cases of concurrent infection with two of these pathogens and in rare instances concurrent infection with all three vector borne infections. Such reports have the potential to inform public health officials and clinicians about the prevalence, disease severity and treatment options available for concurrent infections. The purpose of the present review is to assess the prevalence of such infections by thorough search and analysis of published literature.
Methodology
Search strategy
We did a review based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to identify all relevant publications pertaining to the prevalence of Malaria, Dengue and Chikungunya coinfection. We systematically searched PubMed and Web of Knowledge from inception up to April 2018, using the following search terms anywhere in the articles: Malaria AND Dengue or Malaria AND Chikungunya or Dengue AND Chikungunya. We searched without any bar on language, publication or nature of studies. To identify additional studies, reference list of publications were carefully screened.
Eligibility criteria
Initial assessment was based on review of title and abstract of all studies. Full texts of potentially relevant studies were further analysed for coinfection prevalence data. Cross-sectional studies, retrospective analysis and case reports with full text availability and reporting data about any/all of the coinfections were included in the study. We excluded studies carried out in animals, reviews, letters, opinion pieces, grey literature, dissertations and conference abstracts.
Data extraction
The data extracted from the selected publications included first author, date of survey, place where the study was carried out, sample size and age, type of diagnostic testing performed, study design and prevalence of coinfection. All the data was entered in an excel file and double-checked.
Prevalence mapping
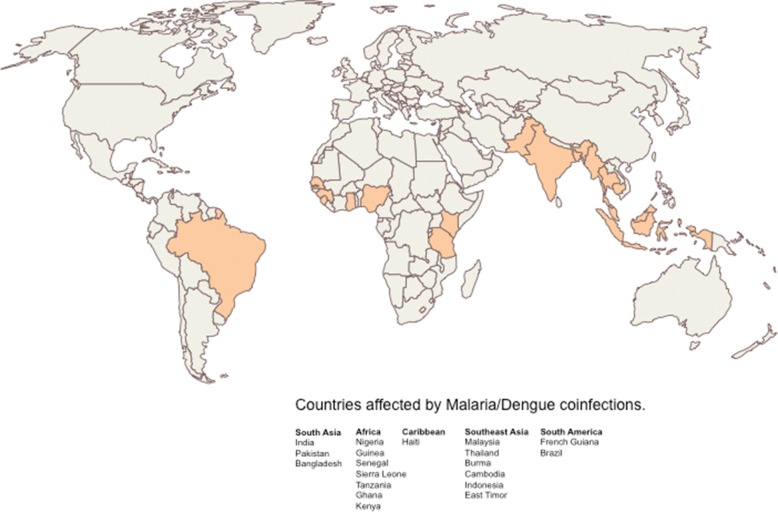
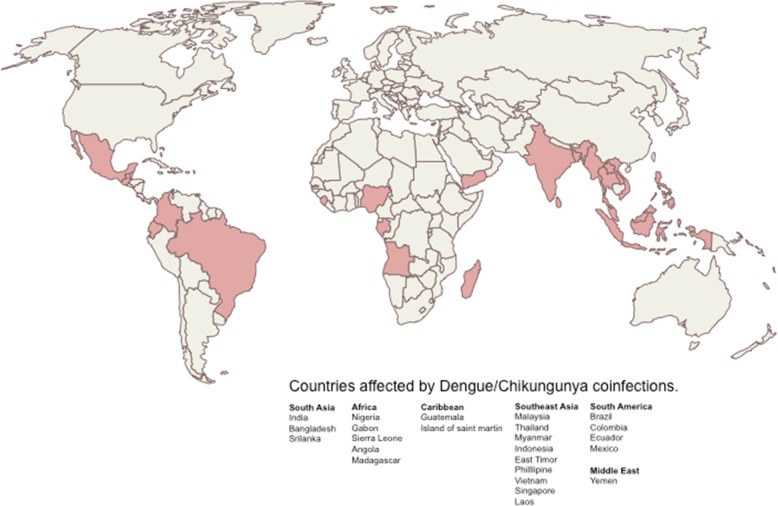
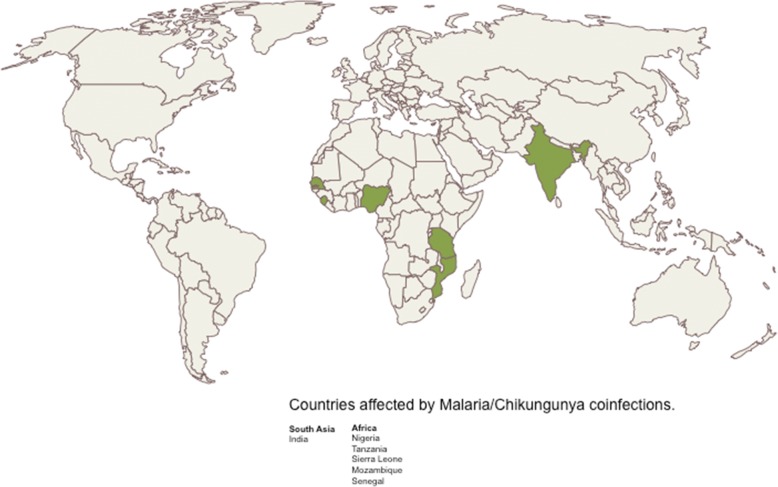
The extracted data was used to create a map of prevalence of coinfection cases. All the cases reported were from seven geographical locations, South Asia, Africa, Southeast Asia, South America, North America, Caribbean and the Middle East. A total of 19 countries reported cases of Malaria/Dengue coinfection; while 24 countries reported coinfection cases of Dengue/Chikungunya. Malaria/Chikungunya cases were reported from 6 countries. Malaria/Dengue/Chikungunya coinfections were reported from only 3 countries. The maps were created using openly available maps (https://www.freeworldmaps.net).
Results
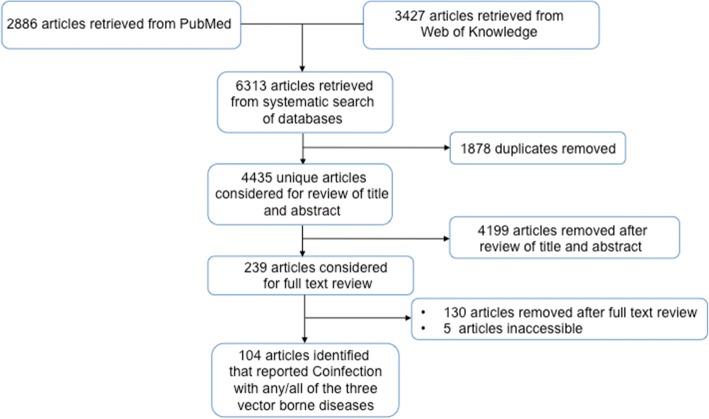
We were able to identify 109 publications that reported the data for any coinfections (Fig. 1, Additional file 1: Table S1). The full text of 104 publications were available out of which 48 were cross sectional studies, 37 were case reports, 13 were retrospective analysis, 5 were prospective studies and 1 surveillance report [17–120]. 49 studies reported only Malaria/Dengue coinfections (Table 1) while 44 studies reported only Dengue/Chikungunya coinfections (Table 2). 1 study reported only Malaria/Chikungunya infection. 3 studies reported both Malaria/Dengue and Malaria/Chikungunya coinfections (Table 3) and 1 study reported Malaria/Dengue, Dengue/Chikungunya and Malaria/Chikungunya coinfections. Malaria/Dengue/Chikungunya coinfections were reported by 4 separate studies (Table 4). 2 studies reported Malaria/Dengue, Dengue/Chikungunya, Malaria/Chikungunya and Malaria/Dengue/Chikungunya coinfections. All of the studies, except two, were published after year 2005. Cases of coinfections were reported from all age groups and two studies from India and Burma reported data from only pregnant females. Blood smear was the most prevalent method for detection of Malaria parasite, while NS1 (Non-structural protein-1) and immunoglobulin ELISA were the most common methods for the detection of Dengue. IgM ELISA was the predominant method for the detection of most cases of Chikungunya. In 14 studies P. falciparum was the cause of Malaria while another 13 reported P. vivax as the infecting species alongside coinfecting arbovirus. 12 studies reported both P. falciparum and P. vivax with Dengue virus in the same population. Another 5 studies reported P. falciparum, P. vivax and Dengue virus in the same individuals. P. knowlesi was reported by two studies and P. ovale was reported by one study.
Fig. 1.
Schematic representation of the study selection process
Table 1.
Coinfection cases of Malaria and Dengue
| S.No. | Citation | Place | Year | Study design | N | Positive for coinfection | Coinfection (%) | Age | Diagnostic test ML/DN | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| South Asia | ||||||||||
| 1 | Abbasi [17] | Karachi, Pakistan |
Sept.2007-Jan. 2008 | Cross sectional | 112 | 26 | 23 | 13–70 | Blood smear / IgM and IgG ELISA | P. vivax- 25, P. falciparum- 1 |
| 2 | Ahmad [18] | Uttarakhand, India | Dec 2012-Dec2013 | Retrospective observational studies | 233 | 9 | 3.8 | 38.6 ± 16 | Blood smear/ IgM ELISA | NM |
| 3 | Alam [19] | Patna, India |
2013 | Case report | 1 | 1 | NA | 42 | Blood smear /NS1, IgM and IgG ELISA | P. falciparum |
| 4 | Ali [20] | Rawalpindi, Pakistan |
Nov. 2003-Oct. 2004 | Cross sectional | 800 | 9 | 1 | 17–50 years | Blood smear /IgM ELISA | P. vivax-8, P. falciparum-1 |
| 5 | Arya [21] | Delhi, India |
2003 | Case report | 2 | 2 | NA | 35 and 63 years | Blood smear /IgM ELISA | P. vivax |
| 6 | Assir [22] | Lahore, Pakistan |
Aug- Nov 2012 | Cross sectional | 856 | 17 | 2 | 12–32 | Blood smear /PCR, NS1 and IgM ELISA | P. vivax - 14, P. falciparum-3 |
| 7 | Barua [23] | Mumbai, India |
June-Nov. 2014, June -Nov. 2015 | Retrospective analysis | 573 | 44 | 8 | NM | Blood smear / NS1 and IgM ELISA | NM |
| 8 | Bhagat [24] | Mumbai, India |
2014 | Case report | 3 | 3 | NA | 8 months −12 year | Blood smear, RDT/NS1, IgM and IgG ELISA | P. vivax |
| 9 | Bhalla [25] | Delhi, India |
2006 | Case report | 1 | 1 | NA | 21 | Blood smear /IgM ELISA | P. falciparum |
| 10 | Chander [26] | Chandigarh, India |
2009 | Case report | 1 | 1 | NA | 28 | Blood smear /IgM ELISA | P. falciparum |
| 11 | Deresinski [27] | USA, infected in India | 2003, Dec | Case report | 1 | 1 | NA | 27 | Blood smear/IgM and IgG ELISA | P. vivax |
| 12 | Faruque [28] | Chittagong, Bangladesh |
Dec. 2008-Nov. 2009 | Cross sectional | 720 | 1 | 0.1 | All ages | RDT/IgM ELISA | P. vivax |
| 13 | Hati [29] | Kolkata, India |
Aug 2005-Dec 2010 | Cross sectional | 2971 | 46 | 1.5 | NM | Blood smear /IgM and IgG ELISA | P. vivax-28, P. falciparum-18 |
| 14 | Kaushik [30] | Dehradun, India |
2006 | Case report | 1 | 1 | NA | 26 | Blood smear/ IgM and IgG ELISA | P. vivax + P. falciparum |
| 15 | Malhotra [31] | Patiala, India |
2012 | Case report | 1 | 1 | NA | 27 | Blood smear /NS1 and IgM ELISA | P. vivax |
| 16 | Mittal [32] | Dehradun, India | Dec 2012- Nov 2013 | Retrospective observational study | 2547 | 8 | 0.3 | Above 18 | Blood film, RDT/IgM, NS1 ELISA | NM |
| 17 | Mohapatra [33] | Odisha, India |
June-Sep 2011 | Prospective observational study | 469 | 27 | 6 | NM | Blood smear /IgM and NS1 ELISA | P. falciparum-24, P. vivax – 2, P. falciparum + P. vivax - 1 |
| 18 | Mørch [34] | Assam, Bihar, Chhattisgarh, Maharashtra, Anantpur Tamilnadu India |
April 2011–November 2012 | Cross sectional | 1564 | 58 | 3.7 | 34 mean age | Blood smear/IgM, NS1 ELISA/ | NM |
| 19 | Mushtaq [35] | Srinagar, infected in Delhi, India |
Oct - 2012 | Case report | 1 | 1 | NA | 25 | Blood smear, RDT/ IgM ELISA | P. falciparum + P. vivax |
| 20 | Pande [36] | Meerut, India |
2013 | Case report | 1 | 1 | NA | 25 | Blood smear /NS1 and IgM ELISA | P. falciparum, P. vivax |
| 21 | Raja [37] | Chennai, India |
May 2013- Jan 2014 | Cross sectional | 100 | 3 | 3 | NM | Blood smear/ELISA | NM |
| 22 | Rani [38] | Hyderabad, India | 2015 | Case report | 1 | 1 | NA | 30s | Blood smear/IgM ELISA | NM |
| 23 | Rao [39] | Odisha (Angul), India | Jan-Dec 2013 | Cross sectional | 1980 | 22 | 1 | All ages | Blood smear, RDT/ IgM and NS1 ELISA, PCR | P. falciparum- 12, P. vivax- 10 |
| 24 | Singh [40] | Dehradun, India | July-Nov 2013 | Retrospective | 1141 | 9 | 0.8 | 12–80 | Blood smear/IgM, NS1 ELISA | NM |
| 25 | Saksena [41] | Delhi, India |
2017 | Case report | 1 | 1 | NA | 17 male | RMAT, PCR/IgM ELISA | P. vivax, P. falciparum |
| 26 | Singla [42] | Chandigarh, India | Jan 2011-Dec 2012 | Cross sectional | 300 | 1 | 0.3 | NM | NM/NS1 and IgM ELISA | P. vivax |
| 27 | Shah [43] | Ahmedabad, India | June 2013-Nov 2014 | Retrospective | 8364 | 27 | 0.3 | NM | Blood smear/NS1, IgM ELISA |
P. vivax + DENV-17, P. falciparum + DENV-9, P. falciparum + P. vivax + DENV-1 |
| 28 | Thangaratham [44] | Alappuzha, Kerala |
2006 | Case report | 1 | 1 | NM | 22 | Blood smear /IgM ELISA | P. vivax, DENV2 |
| 29 | Yasir [45] | Karachi, Pakistan |
April 2013-Jan 2014 | Cross sectional | 159 | 5 | 3 | 15–53 years | Blood smear /IgM ELISA | NM |
| Africa | ||||||||||
| 30 | Ayorinde [46] | Ogun, Nigeria | April-May 2014 | Cross sectional | 60 | 1 | 2 | All ages | Blood smear, RDT, PCR/NS1, IgM and IgG ELISA | P. falciparum |
| 31 | Baba [47] | Nigeria | July-Dec. 2008 | Cross sectional | 310 | 18 | 6 | All ages | Blood smear /PRNT | P. falciparum |
| 32 | Charrel [48] | France, infected in Guinea, Senegal and Sierra Leone | 2004, march | Case report | 1 | 1 | NA | 37 | Blood smear /IgM and IgG ELISA | P. falciparum, DENV3 |
| 33 | Chipwaza [49] | Morogoro, Tanzania | March–May and Aug-Oct. 2013 | Cross sectional | 364 | 31 | 9 | 2–13 | Blood smear /IgM and IgG ELISA, PCR | NM |
| 34 | Dariano [50] | Bo, Sierra Leone | 2012–2013 | Cross sectional | 1260 | 3 | 0.2 | All ages | RDTs/IgM, IgG, NS1 ELISA | NM |
| 35 | Kolawole [51] | Ilorin, Nigeria |
2016 | Cross sectional | 176 | 5 | 3 | All ages | RDT/IgM ELISA, PCR | DENV2, DENV3, DENV4 |
| 36 | Oyeoro [52] | Ibadan, Nigeria | Jan-April 2013 | Cross sectional | 188 | 19 | 10 | All ages | NM/IgG, IgM, NS1 ELISA | NM |
| 37 | Sow [53] | Kedougou, Senegal | July 2009–March 2013 | Cross sectional | 13,845 | 1 | 0.01 | All ages | Blood smear, RDT/ IgM ELISA, PCR | P. falciparum |
| 38 | Stolar [54] | Ghana | 2011–2014 | Retrospective analysis | 218 | 7 | 3 | 2–14 years | RDT/IgM and IgG, ELISA, PCR | P. falciparum |
| 39 | Vu [55] | Kenya | 2016 | Cross sectional | 579 | 33 | 6 | 1–17 years | Blood smear /PCR | NM |
| Caribbean | ||||||||||
| 40 | Serre [56] | Spain, Infected in Haiti |
2011 | Case report | 1 | 1 | NA | 27 | Blood smear, PCR/IgM, IgG and NS1 ELISA, PCR | P. falciparum, DENV4 |
| Southeast Asia | ||||||||||
| 41 | Che rahim [57] | Kelantan, Malaysia | 2017 | Case report | 1 | 1 | NA | 59 | Blood smear, PCR/NS1 ELISA | P. knowlesi |
| 42 | Chong [58] | Malaysia | 2017 | Case report | 1 | 1 | NA | 59 | Blood smear/NS1 and IgM ELISA | P. knowlesi |
| 43 | Issaranggoon [59] | Thailand | 2014 | Case report | 1 | 1 | NA | 11 | Blood smear/ NS1, IgM ELISA | P. falciparum |
| 44 | McGready [60] | Thai-Burmese border | Jan 2004-May 2006 | Cross sectional | 209 | 1 | 0.5 | Pregnant women | Blood smear/IgM ELISA, NS1 ELISA | P. falciparum, P. vivax |
| 45 | Mueller [61] | (Oun Kouma, Ou Chra, Snoul) Rural Cambodia |
Jan 2008- Dec 2010 | Prospective observational study | 1193 | 30 | 2.5 | 7–49 years | RDT/PCR | P. falciparum, P. vivax |
| 46 | Thaha [62] | Surabaya, Indonesia | Nov 2008 | Case report | 1 | 1 | NA | NM | Blood smear/IgM, IgG ELISA | NM |
| 47 | Ward [63] | East Timor | 2006 | Case report | 1 | 1 | NA | 7 | Blood smear /IgM ELISA | P. falciparum |
| 48 | Yong [64] | Riau Island Indonesia | 2012 | Case report | 1 | 1 | NA | 49 | Blood smear/IgM, NS1 ELISA | P. falciparum |
| South America | ||||||||||
| 49 | Carme [65] | French Guiana | July 2004-June 2005 | Retrospective analysis | 1723 | 17 | 1 | NM | Blood smear/PCR, IgM ELISA, virus isolation | P. vivax − 14, P. falciparum- 3, DENV3–5, DENV1–1, NM-11 |
| 50 | Epelboin [66] | French Guiana | 2004–2010 | Retrospective matched pair study | NM | 104 | NA | All ages | Blood smear/PCR, NS1, IgM, IgA ELISA | P. vivax – 80, P. falciparum – 21, P. vivax + P. falciparum – 3, DENV1–3, DENV2–2, DENV3–5, NM-94 |
| 51 | Lupi [67] | Rio de Janeiro, Brazil | Apr 2013 | Case report | 1 | 1 | NA | 52 | Blood smear, RDT, PCR/ IgM and NS1 ELISA, PCR | P. ovale wallikeri |
| 52 | Magalhaes [68] | Brazilian Amazon Manaus Brazil |
March 2009 to April 2010 | Retrospective study | 132 | 11 | 8 | Mean age, 42.7 yrs | Blood smear, PCR/NS1 ELISA, PCR | P. vivax DENV2, DENV3, DENV4 |
| 53 | Magalhaes [69] | Brazilian Amazon Manaus Brazil |
2009–2011 | Cross-sectional | 1578 | 44 | 3 | All ages | Blood smear, PCR/ NS1 ELISA, PCR | P. vivax |
| 54 | Mendonca [70] | Brazilian Amazon Manaus Brazil |
2009–2013 | Prospective observational study | All febrile patients | 30 | NA | 31.11 median age | Blood smear, PCR/ IgM and NS1 ELISA | P. vivax, DENV4–8, DENV3–1, DENV2–18, DENV1–3 |
| 55 | Santana [71] | Novo Repartimento (Pará), Brazil | May 2003 to August 2005 | Cross sectional | 111 | 2 | 2 | > 18 years | Blood smear/PCR | P. vivax, DENV2 |
N – sample size, ML/DN - Malaria/Dengue coinfection, ELISA - Enzyme linked immunosorbent assay, NS1 - Dengue non-structural protein − 1, PCR - Polymerase Chain reaction, RDT - rapid diagnostic test, PRNT - Plaque reduction neutralisation test, RMAT - Rapaid malaria antigen test, NM - not mentioned, NA - not applicable
Table 2.
Coinfection cases of Dengue and Chikungunya
| S.No. | Citations | Place | Year | Study design | N | Positive for coinfection | Coinfection (%) | Age | Diagnostic test DN/CK | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| South Asia | ||||||||||
| 1. | Afreen [72] | Delhi, India |
2014 | Cross sectional | 87 | 9 | 10 | All ages | NS1, IgM, IgG ELISA, PCR/ IgM ELISA, PCR | DENV2 + CHIKV-5, DENV3 + CHIKV -2, DENV1 + CHIKV-1, DENV1 + DENV2+ CHIKV-1 |
| 2. | Carey [73] | Vellore, India |
1964 | Cross sectional | 477 | 8 | 2 | All ages | Virus isolation Serological Complement fixation and Hemagglutination inhibition assay for both infection |
NM |
| 3. | Chahar [74] | Delhi, India |
2006 | Cross sectional | 69 | 6 | 9 | All ages | PCR/PCR | DENV1, DENV3, DENV4 |
| 4. | Galate [75] | Mumbai, Maharashtra | April 2012-Oct. 2013 | Cross sectional | 200 | 19 | 10 | 13–60 | IgM ELISA/IgM ELISA | NM |
| 5. | Hapuarachchi [76] | Sri Lanka | 2006 | Case report | 1 | 1 | NA | 70 | PCR/PCR | NM |
| 6. | Kalawat [77] | Tirupati, India |
2011 | Retrospective analysis | 72 | 2 | 3 | All ages | IgM ELISA / IgM ELISA | NM |
| 7. | Kaur [78] | Delhi, India |
Aug-Dec. 2016 | Cross sectional | 600 | 152 | 25 | 11–68 | IgM ELISA, NS1 ELISA, PCR/IgM ELISA, PCR | NM |
| 8. | Londhey [79] | Mumbai, India |
June 2010–April 2015 | Prospective observational study | 300 | 30 | 10 | All ages | IgM ELISA, PCR/ IgM ELISA, PCR | NM |
| 9. | Mørch [34] | Assam, Bihar, Chhattisgarh, Maharashtra, Anantpur, Tamilnadu India |
April 2011–November 2012 | Cross sectional | 1564 | 25 | 1.6 | 34 mean age | IgM, NS1 ELISA/IgM ELISA | NM |
| 10. | Mukherjee [80] | Kolkata, India |
July 2014-Oct. 2015 | Cross sectional | 326 | 53 | 16 | All ages | IgM and NS1 ELISA, PCR/IgM ELISA, PCR | DENV2, DENV4 |
| 11. | Neeraja [81] | Hyderabad, Telangana | 2007 | Cross sectional | 713 | 8 | 1 | NM | IgG, IgM, PCR/PCR | NM |
| 12. | Paulo [82] | Potugal, Infected in India |
2016 | Case report | 1 | 1 | NA | 65 | PCR/IgM ELISA | DENV3 |
| 13. | Rahim [83] | Dhaka, Bangladesh | 2017 | Case report | 1 | 1 | NA | 23 female | NS1 ELISA/IgM ELISA | NM |
| 14. | Saswat [84] | Khurda, Odisha Aurangabad, Maharashtra India |
July-Dec. 2013 | Cross sectional | 222 | 43 | 19 | All ages | NS1, IgM, IgG ELISA, PCR/IgM ELISA, PCR | DENV2 |
| 15. | Shaikh [85] | Karnataka, India |
July 2010–June 2013 | Cross sectional | 6554 | 532 | 8 | NM | IgM ELISA/IgM ELISA | NM |
| 16. | Schilling [86] | Chennai, India |
September 2008 | Case report | 1 | 1 | NA | 25 | NS1, IgM ELISA and IFA/IgM IFA | NM |
| 17. | Taraphdar [87] | West Bengal, India | 2010 | Cross sectional | 550 | 68 | 12 | All ages | IgM ELISA, PCR / IgM ELISA, PCR | DENV2, DENV3 |
| 18. | Kularatne [88] | Peradeniya, Srilanka | Dec. 2006-March 2007 | Cross sectional | 54 | 3 | 5 | 15–74 | IgM ELISA, Hemagglutination inhibition/ IgM ELISA, Hemagglutination inhibition | NM |
| Africa | ||||||||||
| 19. | Baba [47] | Nigeria | July-Dec. 2008 | Cross sectional | 310 | 63 | 20 | All ages | PRNT/PRNT | NM |
| 20. | Caron [89] | Gabon | Sep 2007-Aug 2010 | Cross sectional | 4287 | 37 | 1 | All ages | PCR of partial E gene/ PCR of partial E1 gene | DENV2 |
| 21. | Dariano [50] | Bo, Sierra Leone | 2012–2013 | Cross sectional | 1260 | 13 | 1 | All ages | IgM, IgG, NS1 ELISA/IgM ELISA | NM |
| 22. | Leroy [90] | Gabon | March–July 2007 | Cross sectional | 773 | 8 | 1 | NM | PCR/ PCR | DENV2 |
| 23. | Nkoghe [91] | Franceville, Gabon | Feb-July 2010 | Cross sectional | 433 | 20 | 4.6 | 1–77 | PCR/PCR | NM |
| 24. | Parreira [92] | Portugal, infected in Luanda, Angola | January 2014 | Case report | 1 | 1 | NA | Early 50s | NS1 IgM, IgG ELISA, PCR/IgM ELISA, PCR | DENV4 |
| 25. | Ratsitorahina [93] | Tomasina, Madagascar |
Jan-March 2006 | Cross sectional | 55 | 10 | 18 | NM | IgM ELISA, PCR/IgM ELISA, PCR | DENV1 |
| Caribbean | ||||||||||
| 26. | Edwards [94] | Guatemala | June 2015 | Surveillance report | 144 | 46 | 32 | All ages | PCR/ PCR | DENV1–4, DENV2–40, DENV4–2 |
| 27. | Omarjee [95] | Island of Saint Martin | Dec. 2013- Jan 2014 |
Cross sectional | 1502 | 16 | 1 | All ages | IgM, IgG ELISA and PCR / IgM, IgG ELISA and PCR | DENV1–10, DENV2–2, DENV4–4 |
| Southeast Asia | ||||||||||
| 28. | Cha [96] | Osong korea Infected (2 in Philllipine, 1 Vietnam, 1 Indonesia, 1 East Timor) | 2009–2010 | Cross sectional | 486 | 5 | 1 | 11–70 | IgM ELISA, PCR/ IgM ELISA, PCR | NM |
| 29. | Chang [97] | Taipei China, infected in Singapore | 2009 April | Case report | 1 | 1 | NA | 12 | IgM and IgG ELISA, PCR/ IgM and IgG ELISA, PCR | DENV2 |
| 30. | Khai Ming [98] | Rangoon, Burma | July 1970-Dec. 1972 | Cross sectional | 2060 | 55 | 2.6 | 0–11 | HI, CF/HI, CF | NM |
| 31. | Laoprasopwattana [99] | Southern Thailand | April–July 2009 | Prospective Cohort study | 50 | 1 | 2 | ≤15 | IgM ELISA and Hemagglutination inhibition/IgM IFA, PCR | NM |
| 32. | Nayar [100] | Kinta, Malaysia |
2006 | Case report | 2 | 2 | NA | 22 and 28 | NS1, IgM ELISA, PCR/PCR | DENV1 |
| 33. | Ooi [101] | Selangor, Malaysia, | 2009 | Case report | 1 | 1 | NA | NM | NM/Complete Genome sequencing of CHIKV | DENV2 |
| 34. | Phommanivong [102] | Champasak Laos | July-Aug 2013 | Cross sectional | 40 | 5 | 12.5 | 5–65 | PCR/PCR | DENV2–3, DENV3–2 |
| 35. | Tun [103] | Mandalay, Myanmar |
July–October 2010 | Cross sectional | 116 | 7 | 6 | ≤12 | IgM ELISA, PCR/IgM ELISA, PCR | NM |
| North America | ||||||||||
| 36. | Kariyawasam [104] | Toronto, Canada | May 2006-April 2007 and Feb 2013-March 2014 | Retrospective analysis | 1304 | 1 | 0.07 | 0–91 | PCR/PCR | DENV-1 |
| 37. | Lindholm [105] | Maryland, USA |
Dec 2013-May 2015 | Cross sectional | 267 | 2 | 0.7 | 25–60 | IgM, IgG ELISA, PCR, PRNT/ IgM, IgG ELISA, PCR, PRNT | NM |
| South America | ||||||||||
| 38. | Bocanegra [106] | Barcelona Spain Infected in south America | April 2014–2015 | Retrospective | 42 | 5 | 12 | 34.6 mean age | IgM ELISA/IgM ELISA, PCR | NM |
| 39. | Brooks [107] | Santos, Brazil |
2017 | Case report | 1 | 1 | NA | 27 | IgM ELISA/IgM ELISA | NM |
| 40. | Calvo [108] | Girardot, Colombia |
Feb 2015 | Cross sectional | 8 | 4 | 50 | 0–10 | IgM ELISA, PCR/PCR | NM |
| 41. | Carrillo-Hernández [109] | Norte de Santander, Colombia | August 2015 – April 2016 | Cross sectional | 157 | 12 | 7.6 | 26.81 | PCR/PCR | NM |
| 42. | Farrell [110] | Machala, Ecuador | 2015 | Case report | 1 | 1 | NA | 35 | IgM, IgG ELISA/PCR | NM |
| 43. | Gomez-Govea [111] | Nuevo leon, Mexico |
Jan-Oct 2015 | Cross sectional | 101 | 5 | 5 | 31 median age | IgM ELISA/IgM ELISA, PCR | NM |
| 44. | Mercado [112] | Bogota, Colombia | Sept 2014-Oct 2015 | Retrospective analysis | 58 | 7 | 12 | NM | IgM ELISA, PCR/PCR | NM |
| 45. | Rosso [113] | Cali, Colombia |
2015 | Case report | 1 | 1 | NA | 72 | PCR/ PCR | DENV3 |
| Middle East | ||||||||||
| 46. | Malik [114] | Al-Hudaydah, Yemen | Oct 2010-March 2011 | Cross sectional | 136 | 1 | 0.7 | NM | IgM ELISA, PCR/IgM ELISA | NM |
| 47. | Rezza [115] | Al-Hudaydah Yemen |
2012 | Cross sectional | 400 | 14 | 3.5 | All ages | IgM, IgG ELISA and PCR/ IgM, IgG ELISA and PCR | DENV2 Predominantly |
N – sample size, DN/CK – Dengue/Chikungunya coinfection, ELISA – Enzyme linked immunosorbent assay, NS1 - Dengue non-structural protein −1, PCR – Polymerase Chain reaction, IFA – immunofluorescence assay, PRNT – Plaque reduction neutralisation test, NM – not mentioned, NA – not applicable
Table 3.
Coinfection cases of Malaria and Chikungunya
| S.No. | Citations | Place | Year | Study design | N | Positive for coinfection | Coinfection(%) | Age | Diagnostic test ML/CK | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| South Asia | ||||||||||
| 1. | Mørch [34] | Assam, Bihar, Chhattisgarh, Maharashtra, Anantpur, Tamilnadu | April 2011–Nov 2012 | Cross sectional | 1564 | 20 | 1.3 | 34 mean age | IgM, NS1 ELISA/IgM ELISA | NM |
| Africa | ||||||||||
| 2. | Ayorinde [46] | Ogun, Nigeria | April-May 2014 | Cross sectional | 60 | 9 | 15 | All ages | Blood smear, RDT, PCR/IgM ELISA | P. falciparum |
| 3. | Baba [47] | Nigeria | July-Dec. 2008 | Cross sectional | 310 | 21 | 6.7 | All ages | Blood smear /PRNT | P. falciparum |
| 4. | Chipwaza [49] | Morogoro, Tanzania | March–May and Aug-Oct. 2013 | Cross sectional | 364 | 2 | 0.6 | 2–13 years | Blood smear / IgM and IgG ELISA, | NM |
| 5. | Dariano [50] | Bo, Sierra Leone | 2012–2013 | Cross sectional | 1260 | 118 | 9 | All ages | RDTs/IgM ELISA | NM |
| 6. | Mugabe [116] | Quelimane Mozambique | Feb-June 2016 | Cross Sectional | 163 | 2 | 1.2 | 28 median age | RDT /IgM ELISA, PCR | NM |
| 7. | Sow [53] | Kedougou, Senegal | July 2009–March 2013 | Cross sectional | 13,845 | 3 | 0.02 | All ages | Blood smear, RDT/ IgM ELISA, PCR | P. falciparum |
N – sample size, ML/CK- Malaria/Chikungunya coinfection, ELISA – Enzyme linked immunosorbent assay, NS1 - Dengue non-structural protein −1, PCR – Polymerase Chain reaction, RDT – rapid diagnostic test, PRNT – Plaque reduction neutralisation test, NM – not mentioned
Table 4.
Coinfection cases of Malaria, Dengue and Chikungunya
| S.No. | Citations | Place | Year | Study design | N | Positive for coinfection | Coinfection (%) | Age | Diagnostic test ML/DN/CK | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| South Asia | ||||||||||
| 1. | Abdullah [117] | Delhi, India |
2016 | Case report | 1 | 1 | NA | 21 | Blood smear, RDT/PCR/IgM ELISA, PCR | P. vivax, DENV3 |
| 2. | Gupta [118] | Delhi, India |
2017 | Case report | 1 | 1 | NA | 55 | RDT/NS1, IgM ELISA/PCR | P. falciparum |
| 3. | Mørch [34] | Assam, Bihar, Chhattisgarh, Maharashtra, Anantpur, Tamilnadu India | April 2011–Nove 2012 | Cross sectional | 1564 | 2 | 0.1 | 34 mean age | Blood smear/IgM, NS1 ELISA/IgM ELISA | NM |
| 4. | Tazeen [119] | Delhi, India |
2016 | Case report | 1 | 1 | NA | 3 | Blood smear /PCR/PCR | P. vivax |
| Africa | ||||||||||
| 5. | Dariano [50] | Bo, Sierra Leone | 2012–2013 | Cross sectional | 1260 | 4 | 0.3 | All ages | RDTs/IgM, IgG, NS1 ELISA/IgM ELISA | NM |
| 6. | Raut [120] | India Infected in Nigeria |
2014 | Case report | 1 | 1 | NA | 21 | Blood smear / NS1 ELISA, PCR/PCR | P. falciparum |
N – sample size, ML/DN/CK – Malaria/Dengue/Chikungunya coinfection, ELISA – Enzyme linked immunosorbent assay, NS1 - Dengue non-structural protein −1, PCR – Polymerase Chain reaction, RDT – rapid diagnostic test, NA – not applicable, NM-not mentioned
Out of the 55 reports about Malaria/Dengue coinfections, only ten have reported the serotype of the Dengue virus. Out of the 47 reports about Dengue/Chikungunya coinfections 20 reports have mentioned the serotype of Dengue virus. Earliest report of Malaria/Dengue coinfection came in 2003 from Brazil, while earliest reported case of Dengue/Chikungunya coinfection came in 1964 from India. Malaria/Chikungunya cases were reported as late as 2008 from Nigeria. A retrospective matched pair study from French Guiana reported most cases (104) of Malaria/Dengue coinfections. Maximum cases of Dengue/Chikungunya coinfections (532) were reported from Karnataka in India and most cases of Malaria/Chikungunya coinfections (118) were reported from Bo, Sierra Leone.
Most cases of coinfections were reported from South Asia (52), primarily from India, followed by Africa (25), South-east Asia (16), South America (15), Caribbean (3) and Middle East (2). Two studies from North America reported coinfections of Dengue/Chikungunya in returning travellers without identifying the location where coinfections occurred. Malaria/Dengue coinfections were reported from 44 unique locations spread across 20 different countries (Fig. 2). Dengue/Chikungunya coinfections were reported from 48 unique locations spread across 26 countries (Fig. 3). 5 countries from African continent and India reported cases of Malaria/Chikungunya coinfections (Fig. 4). Cases of Malaria/Dengue/Chikungunya coinfections were reported from India, Sierra Leone and Nigeria (Fig. 5). Seven countries reported infection in returning travellers(Fig. 6). Based upon cross sectional studies Malaria/ Dengue prevalence varied widely, ranging between 0.1–23% from south Asia, 0.01–9% from Africa, 0.5–2.5% from Southeast Asia and 1–3% from South America. The frequency of Dengue/Chikungunya coinfections ranged from 1 to 25% from South Asia, 1–20% from Africa, 1–32% from Caribbean, 1–12.5% from Southeast Asia, 0.07–0.7% from North America, 5–50% from South America and 0.7–3.5% from Middle east. Malaria/Chikungunya coinfections frequency ranged from 0.02–15% from Africa and a single study reported from India reported 1.3% patients coinfected with both pathogens. Malaria/Dengue/Chikungunya coinfection frequency was reported by two cross sectional studies, one from India with 0.1% prevalence and another from Sierra Leone with 0.3% prevalence.
Fig. 2.
Global distribution of Malaria/Dengue coinfections
Fig. 3.
Global distribution of Dengue/Chikungunya coinfections
Fig. 4.
Global distribution of Malaria/Chikungunya coinfections
Fig. 5.
Global distribution of Malaria/Dengue/Chikungunya coinfections
Fig. 6.
Countries from where coinfection cases were reported in returning travellers
Discussion
Malaria, Dengue and Chikungunya are arthropod borne diseases that have shared endemic profiles. These diseases are spread by mosquito vector, which are found in abundance in tropical regions of the world. Anopheles mosquito, which transmits Malaria parasite, is a night biting mosquito and breed in stagnant water [121]. Aedes that spreads Dengue and Chikungunya, on the other hand bites in daylight and breeds in stored clean water [122]. Expansion of the Aedes vector has lead to introduction of Dengue and Chikungunya to newer locations. Rapid urbanisation without the development of civic infrastructure, constant movement of population for livelihood, monsoon dependent breeding patterns and overlapping habitats have lead to co-circulation and coinfection of these pathogens in the same population [123]. Diagnosis of cases of coinfection is compounded by the fact that initial symptoms of all three diseases are very similar that include febrility as the common factor. Several reports have been published that does not identify the coinfecting pathogen due to lack of distinguishing symptoms at the time, but retrospective analysis later revealed otherwise. In resource poor settings and during outbreaks clinicians might not have the resources or time to rely on detailed investigations.
We have attempted to identify regions of the world from where cases of mixed infection with Malaria, Dengue and Chikungunya have been reported. We searched the databases to identify published reports about any of these coinfections. Most reports of Malaria/Dengue and Dengue/Chikungunya coinfections were reported from India. In recent years there have been many outbreaks of Dengue and Chikungunya in India, not to mention that the first published report of Dengue/Chikungunya coinfection was reported from India in 1967 [72]. However the overall percentage of Malaria/Dengue coinfections was low which, can be explained by different vector species for Malaria verses Dengue and Chikungunya. The highest frequency of Malaria/Dengue coinfections was reported from Pakistan that is endemic for both Malaria and Dengue. Lowest frequency was reported form Senegal with only 0.01%. 41 reports clearly identified the parasite species for Malaria infection but only 10 reported the serotype of Dengue virus. All four serotypes were found to exist with Malaria parasite. Coinfection cases were found in all age groups and gender. Nearly 85% of the reports for Malaria/Dengue coinfections have used microscopic confirmation of the Malaria parasite identifying the parasite load and species. Dengue infections were primarily detected by a combination of immunoglobulin ELISA, NS1 ELISA and PCR.
Dengue/Chikungunya coinfections were reported by 47 studies and an overall higher percentage as compared to Malaria/Dengue coinfection possibly because of similar vector species. The Highest frequency of Dengue/Chikungunya coinfections was reported from Colombia and lowest from Canada in returning travellers. Dengue virus serotype-4 was the predominant serotype found in cases of coinfections. Malaria/Chikungunya coinfections were rare with only 7 published reports. All of them were reported from Africa and India. 6 studies reported Malaria/Dengue/Chikungunya coinfections, four of them were case reports and two cross sectional studies. Three of the case reports were infected in Delhi while another one could have been infected in Nigeria or India. Delhi has become a hub of Industrial and social activities with a burgeoning population. Almost every year during monsoon season the city witnesses Dengue outbreaks with thousands of people getting infected. Due to the lack of distinguishing clinical features, laboratory diagnosis based on endemic patterns and outbreak reports are the only way for adequate clinical management of double or triple coinfections. At least 12 studies reported coinfections in returning travellers underlining the role of travel-based spread of the diseases. This phenomenon has been observed for SARS, MERS-CoV and Dengue [124–126]. Exposing a naïve population to new pathogens might lead to disease outbreak, not to mention viral mutations to adapt its human or mosquito host resulting in more pathogenic strain. Travel advisories and routine surveillance of returning travelers to endemic regions should be implemented stringently to control spread of infections.
Interaction of multiple pathogens within a host may potentially result in several different outcomes. Firstly, if the coinfecting organisms are dependent on similar tissues, the host may have to deal with multiple pathogens at the same time and place. Such interactions are likely to be detrimental to the host as happens in the case of coinfection with Hepatitis B, C and Delta virus coinfections. Hepatitis B, C and Delta virus coinfections results in severe chronic disease that responds poorely to the interferon alpha treatment [127] as compared to single infections. Secondly, the immune effector mechanisms triggered by one pathogen may weaken or divert the host immunity leading to severe outcomes or increased resistance to therapy as exemplified in the case of infection with Mycobacterium tuberculosis and parasite coinfections [128]. Thirdly, the coinfection may not have any serious effect on the prognosis of disease. However, even in such cases the misdiagnosis and mistreatment that may result, can be detrimental to the host. And finally, a coinfection may infact lead to better prognosis. For instance, it has been observed in the decreased mortality rate among the HIV patients coinfected with hepatitis G virus as compared to patients infected with HIV [129]. Plasmodium, Dengue virus and Chikungunya virus all infect different cell types in humans and might influence immune effector mechanism by downregulationg proinflammaotry cytokines like IL-12 and IFN-γ [11, 130]. A proper clinical analysis of Malaria, Dengue and Chikungunya coinfection is necessary to form an informed opinion on following a treatment regimen that best supports the patient and leads to an early resolution of the infection. Out of 104 reports, there are very few reports that have actually looked at the disease severity by establishing proper controls and comparing it with cases of monoinfections systematically. For Malaria/Dengue coinfections, prolonged fever, thrombocytopenia, anemia, renal failure and Jaundice were more pronounced as compared to monoinfections. Dengue/Chikungunya coinfections can result in diarrahea, deep bleeding, hepatomegaly and overall increase in disease severity. High grade fever was the only distinguishing feature of Malaria/Chikungunya coinfection. More such studies are required to create a consensus about disease outcome in cases of coinfections. Animal models that can replicate the coinfection scenario would be very helpful in identifying severity patterns for these diseases.
The distribution of Aedes vector has been reported from Southeast Asia, South Asia, East, Central and West Africa, Caribbean and South America. Aedes aegypti and Aedes albopictus are responsible for the spread of Dengue, Chikungunya, West Nile, Yellow fever and Zika virus [131]. It is difficult to distinguish whether cases of coinfection are due to separate mosquito bites delivering the viruses or single bite by mosquito harboring both viruses. The incubation period of both viruses is nearly same so both diseases are manifested around the same time. Anopheles has also been reported from the above-mentioned regions and also from East and central Asia, Europe and North America [132]. Most cases of Malaria/Dengue and Malaria/Chikungunya coinfections were found from the regions where both vector species are present. In many instances a seasonal pattern of infections is observed with most cases being reported during monsoon season, which coincides with the breeding season of Mosquito vector. Climatic, sociodemographic and environmental factor play a crucial role in survivability and distribution of the mosquito vector thereby influencing cases of coinfections [133]. Vector control continues to be an integral part of reducing disease burden but very few studies reported about the vectors responsible for cases of coinfection. Routine collection of vector surveillance data and thorough analysis of the role of vectors in coinfection cases need to be assessed.
Data collection is prone to bias, to this affect we have made every effort to search and analyze the current literature with broad search queries, nonetheless many relevant studies were unavailable due to lack of full text availability. Also the review relied completely on published literature where grey literature and studies with minimal or negative results may not have been included resulting in publication bias. Furthermore, studies obtained were of variable quality and many did not reported data on disease severity and outcomes in cases of coinfections. Despite these lacunas, the present study attempts to clearly identify regions of the world from where cases of coinfections were reported by thorough search and analysis of published reports. Our analysis indicates that coinfections with Malaria, Dengue and Chikungunya or in rare instances all three is a possibility. Our analysis also indicates that there are higher percentages of people with febrile symptoms, which might have Dengue/Chikungunya coinfections as compared to Malaria/Dengue or Malaria/Chikungunya coinfections. Shared epidemiology, vector distribution and co-circulation of pathogens are some of the reasons for coinfections. We have georeferenced cases of coinfections and identified affected countries of the worlds, establishing co-endemicity of these infections, which might help in proper and complete diagnosis of cases of coinfections with similar initial symptoms.
Conclusion
This systematic review has found evidence of Malaria, Dengue and Chikungunya coinfections in 42 Countries spread across several geographical locations. Malaria/Dengue was the most prevalent coinfection followed by Dengue/Chikungunya. These infections often affect same populations due to share endemicity and can be present simultaneously in the same individual. Similar initial symptoms make it harder for clinicians to identify cases of coinfections. Most coinfections were found from South Asia and Africa. P. falciparum and P. vivax were the most common malaria species found with coinfecting arbovirus and DENV-4 was the most common serotype found in cases of Dengue coinfections. Prolonged and high grade fever, thrombocytopenia, diarrhea, Jaundice and hepatomegaly were some of the signs and symptoms associated with cases of coinfection. We also found evidence of coinfections in returning travellers, which have the potential to introduce the pathogen into new locations with established vector populations. Our study highlights the global prevalence of cases of coinfection and their geographical distribution, which could help in systematic planning, surveillance, diagnosis and health care delivery to the affected population.
Additional file
Table S1. Detailed search strategy. (DOCX 14 kb)
Availability of data and materials
The datasets analysed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- CHIKV
Chikungunya Virus
- DENV
Dengue Virus
- ELISA
Enzyme linked immunosorbent assay
- MERS-CoV
Middle East respiratory syndrome corona virus
- PCR
Polymerase chain reaction
- SARS
Severe Acute Respiratory Syndrome
Authors’ contributions
NS, SM, AH, extracted the data, AAC, FD and SP cross checked and tabulated the data, NS wrote the manuscript. All the authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5626-z) contains supplementary material, which is available to authorized users.
Contributor Information
Nasir Salam, Email: nsalam@imamu.edu.sa.
Shoeb Mustafa, Email: drshoebmustafa@gmail.com.
Abdul Hafiz, Email: aaahafiz@uqu.edu.sa.
Anis Ahmad Chaudhary, Email: anis.chaudhary@gmail.com.
Farah Deeba, Email: farahdeeba19@gmail.com.
Shama Parveen, Email: shamp25@yahoo.com.
References
- 1.Kilpatrick AM, Randolph SE. Drivers, dynamics, and control of emerging vector-borne zoonotic diseases. Lancet. 2012;380:1946–1955. doi: 10.1016/S0140-6736(12)61151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, et al. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.http://www.who.int/mediacentre/factsheets/fs094/en/ Accessed on 19th Oct. 2017.
- 4.Miller LH, Ackerman HC, Su XZ, Wellems TE. Malaria biology and disease pathogenesis: insights for new treatments. Nat Med. 2013;19:156–167. doi: 10.1038/nm.3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barber BE, Rajahram GS, Grigg MJ, William T, Anstey NM. World malaria report: time to acknowledge Plasmodium knowlesi malaria. Malar J. 2017;16:135. doi: 10.1186/s12936-017-1787-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diamond MS, Pierson TC. Molecular insight into dengue virus pathogenesis and its implications for disease control. Cell. 2015;162:488–492. doi: 10.1016/j.cell.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.http://www.who.int/denguecontrol/epidemiology/en/ Accessed on 19th Oct. 2017.
- 8.Deeba F, Islam A, Kazim SN, Naqvi IH, Broor S, et al. Chikungunya virus: recent advances in epidemiology, host pathogen interaction and vaccine strategies. Pathog Dis. 2016;74 [DOI] [PubMed]
- 9.Mayer SV, Tesh RB, Vasilakis N. The emergence of arthropod-borne viral diseases: a global prospective on dengue, chikungunya and zika fevers. Acta Trop. 2017;166:155–163. doi: 10.1016/j.actatropica.2016.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Furuya-Kanamori L, Liang S, Milinovich G, Soares Magalhaes RJ, Clements AC, et al. Co-distribution and co-infection of chikungunya and dengue viruses. BMC Infect Dis. 2016;16:84. doi: 10.1186/s12879-016-1417-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halsey ES, Baldeviano GC, Edgel KA, Vilcarromero S, Sihuincha M, et al. Symptoms and immune markers in Plasmodium/dengue virus co-infection compared with mono-infection with either in Peru. PLoS Negl Trop Dis. 2016;10:e0004646. doi: 10.1371/journal.pntd.0004646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hisam A, Mahmood ur R, Khan MB, Kadir E, Azam N. Frequency of co-existence of dengue and malaria in patients presenting with acute febrile illness. J Pak Med Assoc. 2014;64:247–251. [PubMed] [Google Scholar]
- 13.Weaver SC, Lecuit M. Chikungunya Virus Infections. N Engl J Med. 2015;373:94–95. doi: 10.1056/NEJMc1505501. [DOI] [PubMed] [Google Scholar]
- 14.Randolph SE, Rogers DJ. The arrival, establishment and spread of exotic diseases: patterns and predictions. Nat Rev Microbiol. 2010;8:361–371. doi: 10.1038/nrmicro2336. [DOI] [PubMed] [Google Scholar]
- 15.Waggoner J, Brichard J, Mutuku F, Ndenga B, Heath CJ, et al. Open forum infect dis 4: ofx110. 2017. Malaria and chikungunya detected using molecular diagnostics among febrile Kenyan children. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dondorp AM, MNT H, Mer M. Recommendations for the management of severe malaria and severe dengue in resource-limited settings. In: Sepsis in Resource-Limited Settings-Expert Consensus Recommendations Group of the European Society of Intensive Care M, the Mahidol-Oxford Research Unit in Bangkok T: Intensive care med; 2016. [DOI] [PMC free article] [PubMed]
- 17.Abbasi A, Butt N, Sheikh QH, Bhutto AR, Munir SM, et al. Clinical features, diagnostic techniques and Management of Dual Dengue and Malaria Infection. J Coll Physicians Surg Pak. 2009;19:25–29. [PubMed] [Google Scholar]
- 18.Ahmad S, Dhar M, Mittal G, Bhat NK, Shirazi N, Kalra V, Sati HC, Gupta V. A comparative hospital-based observational study of mono- and co-infections of malaria, dengue virus and scrub typhus causing acute undifferentiated fever. Eur J Clin Microbiol Infect Dis. 2016;35:705–711. doi: 10.1007/s10096-016-2590-3. [DOI] [PubMed] [Google Scholar]
- 19.Alam A, Dm M. A case of cerebral malaria and dengue concurrent infection. Asian Pac J Trop Biomed. 2013;3:416–417. doi: 10.1016/S2221-1691(13)60087-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ali N, Nadeem A, Anwar M, Tariq WU, Chotani RA. Dengue fever in malaria endemic areas. J Coll Physicians Surg Pak. 2006;16:340–342. [PubMed] [Google Scholar]
- 21.Arya AC, Mehta LK, Agarwal N, Agarwal BK, Mathai G, et al. Episodes of concurrent dengue and malaria. Dengue Bulletin. 2005;29:208–209. [Google Scholar]
- 22.Assir MZK, Masood MA, Ahmad HI. Concurrent dengue and malaria infection in Lahore, Pakistan during the 2012 dengue outbreak. Int J Infect Dis. 2014;18:41–46. doi: 10.1016/j.ijid.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Barua A, Yeolekar ME (2016) Concurrent dengue and malaria coinfection: observations from a Central Mumbai hospital. Int J Infect Dis 45: 165–165.
- 24.Bhagat M, Kanhere S, Phadke V, George R. Concurrent malaria and dengue fever: a need for rapid diagnostic methods. J Family Med Prim Care. 2014;3:446–448. doi: 10.4103/2249-4863.148146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhalla A, Sharma N, Sharma A, Suri V. Concurrent infection with dengue and malaria. Indian J Med Sci. 2006;60:330–331. doi: 10.4103/0019-5359.26610. [DOI] [PubMed] [Google Scholar]
- 26.Chander J, Singla N, Singh R. Concurrent presence of dengue and Plasmodium falciparum. Trop Med health. 2009;37:69–70. doi: 10.2149/tmh.2009-07. [DOI] [Google Scholar]
- 27.Deresinski S. Concurrent plasmodium vivax malaria and dengue. Emerg Infect Dis. 2006;12:1802. doi: 10.3201/eid1211.060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Faruque LI, Zaman RU, Alamgir AS, Gurley ES, Haque R, et al. Hospital-based prevalence of malaria and dengue in febrile patients in Bangladesh. Am J Trop Med Hyg. 2012;86:58–64. doi: 10.4269/ajtmh.2012.11-0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hati AK, Bhattacharjee I, Mukherjee H, Bandyopadhayay B, Bandyopadhyay D, et al. Concurrent dengue and malaria in an area in Kolkata. Asian Pac J Trop Med. 2012;5:315–317. doi: 10.1016/S1995-7645(12)60046-7. [DOI] [PubMed] [Google Scholar]
- 30.Kaushik RM, Varma A, Kaushik R, Gaur KJ. Concurrent dengue and malaria due to Plasmodium falciparum and P. Vivax. Trans R Soc Trop Med Hyg. 2007;101:1048–1050. doi: 10.1016/j.trstmh.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 31.Malhotra V. Concurrent malaria and dengue infection. Int Jour Health Allie Sci. 2012;1:181–182. doi: 10.4103/2278-344X.105083. [DOI] [Google Scholar]
- 32.Mittal G, Ahmad S, Agarwal RK, Dhar M, Mittal M, Sharma S. Aetiologies of acute undifferentiated febrile illness in adult patients an experience from a tertiary care hospital in northern India. J Clin Diagn Res. 2015;9:DC22–DC24. doi: 10.1111/crj.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohapatra MK, Patra P, Agrawala R. Manifestation and outcome of concurrent malaria and dengue infection. J Vector Borne Dis. 2012;49:262–265. [PubMed] [Google Scholar]
- 34.Morch K, Manoharan A, Chandy S, Chacko N, Alvarez-Uria G, Patil S, Henry A, Nesaraj J, Kuriakose C, Singh A, et al. Acute undifferentiated fever in India: a multicentre study of aetiology and diagnostic accuracy. BMC Infect Dis. 2017;17:665. doi: 10.1186/s12879-017-2764-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mushtaq MB, Qadri MI, Rashid A. Concurrent infection with dengue and malaria: an unusual presentation. Case Rep Med. 2013;2013:520181. doi: 10.1155/2013/520181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pande A, Guharoy D. A case report of Plasmodium vivax, Plasmodium falciparum and dengue co-infection in a 6 months pregnancy. Ann Med Health Sci Res. 2013;3:S16–S17. doi: 10.4103/2141-9248.121211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raja, J. M., Mary, A., Usha, S. (2016) A Study on Dual Infections in Pyrexia Cases International Journal of Medical Research & Health Sciences 5:150–155.
- 38.Rani PK, Chhablani J, Bhargava A. Frosted branch Angiitis in a patient Coinfected with dengue hemorrhagic fever and malaria. JAMA ophthalmology. 2015;133:e1568. doi: 10.1001/jamaophthalmol.2015.68. [DOI] [PubMed] [Google Scholar]
- 39.Rao MRK, Padhy RN, Das MK. Prevalence of dengue viral and malaria parasitic co-infections in an epidemic district, Angul of Odisha, India: an eco-epidemiological and cross-sectional study for the prospective aspects of public health. Journal of Infection and Public Health. 2016;9:421–428. doi: 10.1016/j.jiph.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 40.Singh R, Singh SP, Ahmad N. A study of etiological pattern in an epidemic of acute febrile illness during monsoon in a tertiary health Care Institute of Uttarakhand, India. Journal of clinical and diagnostic research. 2014; JCDR 8, Mc01–03 [DOI] [PMC free article] [PubMed]
- 41.Saksena R, Matlani M, Singh V, Kumar A, Anveshi A, Kumar D, Gaind R. Early treatment failure in concurrent dengue and mixed malaria species infection with suspected resistance to artemisinin combination therapy from a tertiary care center in Delhi: a case report. International medical case reports journal. 2017;10:289–294. doi: 10.2147/IMCRJ.S139729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singla N, Arora S, Goel P, Chander J, Huria A. Dengue in pregnancy: an under-reported illness, with special reference to other existing co-infections. Asian Pac J Trop Med. 2015;8:206–208. doi: 10.1016/S1995-7645(14)60316-3. [DOI] [PubMed] [Google Scholar]
- 43.Shah PD, Mehta TK. Evaluation of concurrent malaria and dengue infections among febrile patients. Indian J Med Microbiol. 2017;35:402–405. doi: 10.4103/ijmm.IJMM_16_161. [DOI] [PubMed] [Google Scholar]
- 44.Thangaratham PS, Jeevan MK, Rajendran R, Samuel PP, Tyagi BK. Dual infection by dengue virus and Plasmodium vivax in Alappuzha District, Kerala. India Jpn J Infect Dis. 2006;59:211–212. [PubMed] [Google Scholar]
- 45.Yasir S, Rashid MO, Moin F, Owais K. Co-existence of dengue fever & malaria in thrombocytopenic patients presented with acute febrile illness. Pak Jour Med Dent. 2014;3:19–23. [Google Scholar]
- 46.Ayorinde AF, Oyeyiga AM, Nosegbe NO, Folarin OA. A survey of malaria and some arboviral infections among suspected febrile patients visiting a health Centre in Simawa, Ogun state, Nigeria. J Infect Public Health. 2016;9:52–59. doi: 10.1016/j.jiph.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 47.Baba M, Logue CH, Oderinde B, Abdulmaleek H, Williams J, et al. Evidence of arbovirus co-infection in suspected febrile malaria and typhoid patients in Nigeria. J Infect Dev Ctries. 2013;7:51–59. doi: 10.3855/jidc.2411. [DOI] [PubMed] [Google Scholar]
- 48.Charrel RN, Brouqui P, Foucault C, de Lamballerie X. Concurrent dengue and malaria. Emerg Infect Dis. 2005;11:1153–1154. doi: 10.3201/eid1107.041352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chipwaza B, Mugasa JP, Selemani M, Amuri M, Mosha F, et al. Dengue and chikungunya fever among viral diseases in outpatient febrile children in Kilosa District hospital. Tanzania Plos Neglected Tropical Diseases. 2014;8 [DOI] [PMC free article] [PubMed]
- 50.Dariano DF, Taitt CR, Jacobsen KH, Bangura U, Bockarie AS, Bockarie MJ, Lahai J, Lamin JM, Leski TA, Yasuda C, et al. Surveillance of vector-borne infections (chikungunya, dengue, and malaria) in Bo, Sierra Leone, 2012-2013. The American journal of tropical medicine and hygiene. 2017;97:1151–1154. doi: 10.4269/ajtmh.16-0798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kolawole OM, Seriki AA, Irekeola AA, Bello KE, Adeyemi OO. Dengue virus and malaria concurrent infection among febrile subjects within Ilorin metropolis, Nigeria. J Med Virol. 2017;89:1347–1353. doi: 10.1002/jmv.24788. [DOI] [PubMed] [Google Scholar]
- 52.Oyero OG, Ayukekbong JA. High dengue NS1 antigenemia in febrile patients in Ibadan, Nigeria. Virus Res. 2014;191:59–61. doi: 10.1016/j.virusres.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 53.Sow A, Loucoubar C, Diallo D, Faye O, Ndiaye Y, et al. Concurrent malaria and arbovirus infections in Kedougou, southeastern Senegal. Malar J. 2016;15:47. doi: 10.1186/s12936-016-1100-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stoler J, Delimini RK, Bonney JHK, Oduro AR, Owusu-Agyei S, et al. Evidence of recent dengue exposure among malaria parasite-positive children in three urban centers in Ghana. Am J Trop Med Hyg. 2015;92:497–500. doi: 10.4269/ajtmh.14-0678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vu KR, Mutai N, Ndenga BA, Heath C, LaBeaud AD. Dengue virus and malaria co-infection in Kenyan children. Annals of Global Health. 2016;82:397–436. doi: 10.1016/j.aogh.2016.04.209. [DOI] [Google Scholar]
- 56.Serre N, Franco L, Sulleiro E, Rubio JM, Zarzuela F, et al. Concurrent infection with dengue type 4 and Plasmodium falciparum acquired in Haiti. J Travel Med. 2015;22:345–347. doi: 10.1111/jtm.12222. [DOI] [PubMed] [Google Scholar]
- 57.Che Rahim MJ, Mohammad N, Besari AM, Wan Ghazali WS. Severe Plasmodium knowlesi with dengue coinfection. BMJ case reports. 2017;2017 [DOI] [PMC free article] [PubMed]
- 58.Chong SE, Mohamad Zaini RH, Suraiya S, Lee KT, Lim JA. The dangers of accepting a single diagnosis: case report of concurrent Plasmodium knowlesi malaria and dengue infection. Malar J. 2017;16:2. doi: 10.1186/s12936-016-1666-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Issaranggoon na ayuthaya S, Wangjirapan A, Oberdorfer P. An 11-year-old boy with Plasmodium falciparum malaria and dengue co-infection. BMJ Case Rep. 2014:2014. [DOI] [PMC free article] [PubMed]
- 60.McGready R, Ashley EA, Wuthiekanun V, Tan SO, Pimanpanarak M, Viladpai-Nguen SJ, Jesadapanpong W, Blacksell SD, Peacock SJ, Paris DH, et al. Arthropod borne disease: the leading cause of fever in pregnancy on the Thai-Burmese border. PLoS Negl Trop Dis. 2010;4:e888. doi: 10.1371/journal.pntd.0000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mueller TC, Siv S, Khim N, Kim S, Fleischmann E, et al. Acute undifferentiated febrile illness in rural Cambodia: a 3-year prospective observational study. PLoS One. 2014;9:e95868. doi: 10.1371/journal.pone.0095868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thaha M, Pranawa, Yogiantoro M, Tanimoto M, Tomino Y. Acute renal failure in a patient with severe malaria and dengue shock syndrome. Clin Nephrol. 2008;70:427–430. doi: 10.5414/CNP70427. [DOI] [PubMed] [Google Scholar]
- 63.Ward DI. A case of fatal Plasmodium falciparum malaria complicated by acute dengue fever in East Timor. Am J Trop Med Hyg. 2006;75:182–185. [PubMed] [Google Scholar]
- 64.Yong KP, Tan BH, Low CY. Severe falciparum malaria with dengue coinfection complicated by rhabdomyolysis and acute kidney injury: an unusual case with myoglobinemia, myoglobinuria but normal serum creatine kinase. BMC Infect Dis. 2012;12:364. doi: 10.1186/1471-2334-12-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carme B, Matheus S, Donutil G, Raulin O, Nacher M, et al. Concurrent dengue and malaria in cayenne hospital, French Guiana. Emerg Infect Dis. 2009;15:668–671. doi: 10.3201/eid1504.080891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Epelboin L, Hanf M, Dussart P, Ouar-Epelboin S, Djossou F, et al. Is dengue and malaria co-infection more severe than single infections? A retrospective matched-pair study in French Guiana. Malar J. 2012;11:142. doi: 10.1186/1475-2875-11-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lupi O, Ridolfi F, da Silva S, Zanini GM, Lavigne A, et al. Dengue infection as a potential trigger of an imported Plasmodium ovale malaria relapse or a long incubation period in a non-endemic malaria region. Int J Infect Dis. 2016;44:20–24. doi: 10.1016/j.ijid.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 68.Magalhaes BM, Alexandre MA, Siqueira AM, Melo GC, Gimaque JB, et al. Clinical profile of concurrent dengue fever and Plasmodium vivax malaria in the Brazilian Amazon: case series of 11 hospitalized patients. Am J Trop Med Hyg. 2012;87:1119–1124. doi: 10.4269/ajtmh.2012.12-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Magalhaes BML, Siqueira AM, Alexandre MAA, Souza MS, Gimaque JB, et al. P. Vivax malaria and dengue fever co-infection: a cross-sectional study in the Brazilian Amazon. PLoS Negl Trop Dis. 2014;8 [DOI] [PMC free article] [PubMed]
- 70.Mendonca VRR, Andrade BB, Souza LCL, Magalhaes BML, Mourao MPG, et al. Unravelling the patterns of host immune responses in Plasmodium vivax malaria and dengue co-infection. Malar J. 2015;14 [DOI] [PMC free article] [PubMed]
- 71.Santana Vdos S, Lavezzo LC, Mondini A, Terzian AC, Bronzoni RV, et al. Concurrent dengue and malaria in the Amazon region. Rev Soc Bras Med Trop. 2010;43:508–511. doi: 10.1590/S0037-86822010000500007. [DOI] [PubMed] [Google Scholar]
- 72.Afreen N, Deeba F, Khan WH, Haider SH, Kazim SN, et al. Molecular characterization of dengue and chikungunya virus strains circulating in New Delhi, India. Microbiol Immunol. 2014;58:688–696. doi: 10.1111/1348-0421.12209. [DOI] [PubMed] [Google Scholar]
- 73.Carey DE, Myers RM, DeRanitz CM, Jadhav M, Reuben R. The 1964 chikungunya epidemic at Vellore, South India, including observations on concurrent dengue. Trans R Soc Trop Med Hyg. 1969;63:434–445. doi: 10.1016/0035-9203(69)90030-3. [DOI] [PubMed] [Google Scholar]
- 74.Chahar HS, Bharaj P, Dar L, Guleria R, Kabra SK, et al. Co-infections with chikungunya virus and dengue virus in Delhi, India. Emerg Infect Dis. 2009;15:1077–1080. doi: 10.3201/eid1507.080638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Galate LB, Agrawal SR, Shastri JS, Londhey V. Chikungunya fever among patients with acute febrile illness attending a tertiary Care Hospital in Mumbai. Journal of laboratory physicians. 2016;8:85–89. doi: 10.4103/0974-2727.180787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hapuarachchi HA, Bandara KB, Hapugoda MD, Williams S, Abeyewickreme W. Laboratory confirmation of dengue and chikungunya co-infection. Ceylon Med J. 2008;53:104–105. doi: 10.4038/cmj.v53i3.252. [DOI] [PubMed] [Google Scholar]
- 77.Kalawat U, Sharma KK, Reddy SG. Prevalence of dengue and chickungunya fever and their co-infection. Indian J Pathol Microbiol. 2011;54:844–846. doi: 10.4103/0377-4929.91518. [DOI] [PubMed] [Google Scholar]
- 78.Kaur N, Jain J, Kumar A, Narang M, Zakaria MK, Marcello A, Kumar D, Gaind R, Sunil S. Chikungunya outbreak in Delhi, India, 2016: report on coinfection status and comorbid conditions in patients. New microbes and new infections. 2017;20:39–42. doi: 10.1016/j.nmni.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Londhey V, Agrawal S, Vaidya N, Kini S, Shastri JS, et al. Dengue and chikungunya virus co-infections: the inside story. J Assoc Physicians India. 2016;64:36–40. [PubMed] [Google Scholar]
- 80.Mukherjee S, Dutta SK, Sengupta S, Tripathi A. Evidence of dengue and chikungunya virus co-infection and circulation of multiple dengue serotypes in a recent Indian outbreak. Eur J Clin Microbiol Infect Dis. 2017; [DOI] [PubMed]
- 81.Neeraja M, Lakshmi V, Dash PK, Parida MM, Rao PV. The clinical, serological and molecular diagnosis of emerging dengue infection at a tertiary care institute in southern, India. Journal of clinical and diagnostic research: JCDR. 2013;7:457–461. doi: 10.7860/JCDR/2013/4786.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Paulo CO, Ze-Ze L, Jordao S, Pena ER, Neves I, et al. Dengue virus serotype 3 and chikungunya virus co-infection in a traveller returning from India to Portugal. November 2016 IDCases. 2017;9:30–33. doi: 10.1016/j.idcr.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rahim MA, Zaman S, Sultana N, Islam A, Uddin KN. Chikungunya-dengue co-infection during pregnancy requiring preterm caesarean section: first case report from Bangladesh. Trop Dr. 2017;49475517747431 [DOI] [PubMed]
- 84.Saswat T, Kumar A, Kumar S, Mamidi P, Muduli S, et al. High rates of co-infection of dengue and chikungunya virus in Odisha and Maharashtra, India during 2013. Infect Genet Evol. 2015;35:134–141. doi: 10.1016/j.meegid.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 85.Shaikh N, Raut CG, Manjunatha M. Co-infections with chikungunya and dengue viruses: a serological study in Karnataka state, India. Indian J Med Microbiol. 2015;33:459–460. doi: 10.4103/0255-0857.158607. [DOI] [PubMed] [Google Scholar]
- 86.Schilling S, Emmerich P, Gunther S, Schmidt-Chanasit J. Dengue and chikungunya virus co-infection in a German traveller. J Clin Virol. 2009;45:163–164. doi: 10.1016/j.jcv.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 87.Taraphdar D, Sarkar A, Mukhopadhyay BB, Chatterjee S. A comparative study of clinical features between monotypic and dual infection cases with chikungunya virus and dengue virus in West Bengal, India. Am J Trop Med Hyg. 2012;86:720–723. doi: 10.4269/ajtmh.2012.11-0704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kularatne SAM, Gihan MC, Weerasinghe SC, Gunasena S. Concurrent outbreaks of chikungunya and dengue fever in Kandy, Sri Lanka, 2006-07: a comparative analysis of clinical and laboratory features. Postgrad Med J. 2009;85:342–346. doi: 10.1136/pgmj.2007.066746. [DOI] [PubMed] [Google Scholar]
- 89.Caron M, Paupy C, Grard G, Becquart P, Mombo I, et al. Recent introduction and rapid dissemination of chikungunya virus and dengue virus serotype 2 associated with human and mosquito coinfections in Gabon. Central Africa Clinical Infectious Diseases. 2012;55:E45–E53. doi: 10.1093/cid/cis530. [DOI] [PubMed] [Google Scholar]
- 90.Leroy EM, Nkoghe D, Ollomo B, Nze-Nkogue C, Becquart P, et al. Concurrent chikungunya and dengue virus infections during simultaneous outbreaks, Gabon, 2007. Emerg Infect Dis. 2009;15:591–593. doi: 10.3201/eid1504.080664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nkoghe D, Kassa RF, Bisvigou U, Caron M, Grard G, Leroy EM. No clinical or biological difference between chikungunya and dengue fever during the 2010 Gabonese outbreak. Infectious disease reports. 2012;4:e5. doi: 10.4081/idr.2012.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Parreira R, Centeno-Lima S, Lopes A, Portugal-Calisto D, Constantino A, et al. Dengue virus serotype 4 and chikungunya virus coinfection in a traveller returning from Luanda, Angola, January 2014. Euro Surveill. 2014;19 [DOI] [PubMed]
- 93.Ratsitorahina M, Harisoa J, Ratovonjato J, Biacabe S, Reynes JM, et al. Outbreak of dengue and chikungunya fevers, Toamasina, Madagascar, 2006. Emerg Infect Dis. 2008;14:1135–1137. doi: 10.3201/eid1407.071521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Edwards T, Signor LD, Williams C, Donis E, Cuevas LE, et al. Co-infections with chikungunya and dengue viruses, Guatemala, 2015. Emerg Infect Dis. 2016;22:2003–2005. doi: 10.3201/eid2211.161017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Omarjee R, Prat C, Flusin O, Boucau S, Tenebray B, et al. Importance of case definition to monitor ongoing outbreak of chikungunya virus on a background of actively circulating dengue virus, St Martin, December 2013 to January 2014. Euro Surveill. 2014;19 [DOI] [PubMed]
- 96.Cha GW, Cho JE, Lee EJ, Ju YR, Han MG, Park C, Jeong YE. Travel-associated chikungunya cases in South Korea during 2009-2010. Osong public health and research perspectives. 2013;4:170–175. doi: 10.1016/j.phrp.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chang SF, Su CL, Shu PY, Yang CF, Liao TL, Cheng CH, Hu HC, Huang JH. Concurrent isolation of chikungunya virus and dengue virus from a patient with coinfection resulting from a trip to Singapore. J Clin Microbiol. 2010;48:4586–4589. doi: 10.1128/JCM.01228-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Khai Ming C, Thain S, Thaung U, Tin U, Myint KS, Swe T, Halstead SB, Diwan AR. Clinical and laboratory studies on haemorrhagic fever in Burma, 1970–72. Bulletin of the, vol. 51: World Health Organization; 1974. p. 227–35. [PMC free article] [PubMed]
- 99.Laoprasopwattana K, Kaewjungwad L, Jarumanokul R, Geater A. Differential diagnosis of chikungunya, dengue viral infection and other acute febrile illnesses in children. Pediatr Infect Dis J. 2012;31:459–463. doi: 10.1097/INF.0b013e31824bb06d. [DOI] [PubMed] [Google Scholar]
- 100.Nayar SK, Noridah O, Paranthaman V, Ranjit K, Norizah I, et al. Co-infection of dengue virus and chikungunya virus in two patients with acute febrile illness. Med J Malaysia. 2007;62:335–336. [PubMed] [Google Scholar]
- 101.Ooi MK, Gan HM, Rohani A, Syed Hassan S (2016) First Complete Genome Sequence of a Chikungunya Virus Strain Isolated from a Patient Diagnosed with Dengue Virus Infection in Malaysia. 4. [DOI] [PMC free article] [PubMed]
- 102.Phommanivong V, Kanda S, Shimono T, Lamaningao P, Darcy AW, Mishima N, Phaytanavanh B, Nishiyama T. Co-circulation of the dengue with chikungunya virus during the 2013 outbreak in the southern part of Lao PDR. Tropical medicine and health. 2016;44:24. doi: 10.1186/s41182-016-0020-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tun MM, Thant KZ, Inoue S, Nabeshima T, Aoki K, et al. Detection of east/central/south African genotype of chikungunya virus in Myanmar, 2010. Emerg Infect Dis. 2014;20:1378–1381. doi: 10.3201/eid2008.131431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kariyawasam R, Lau R, Eshaghi A, Patel SN, Sider D, Gubbay JB, Boggild AK. Spectrum of viral pathogens in blood of malaria-free ill travelers returning to Canada. Emerg Infect Dis. 2016;22:854–861. doi: 10.3201/eid2205.151875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lindholm DA, Myers T, Widjaja S, Grant EM, Telu K, Lalani T, Fraser J, Fairchok M, Ganesan A, Johnson MD, et al. Mosquito exposure and chikungunya and dengue infection among travelers during the chikungunya outbreak in the Americas. The American journal of tropical medicine and hygiene. 2017;96:903–912. doi: 10.4269/ajtmh.16-0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bocanegra C, Anton A, Sulleiro E, Pou D, Salvador F, Roure S, Gimferrer L, Espasa M, Franco L, Molina I, et al. Imported cases of chikungunya in Barcelona in relation to the current American outbreak. Journal of travel medicine. 2016;23 [DOI] [PubMed]
- 107.Brooks JBB, Ruiz CAC, Fragoso YD. Acute illness with neurological findings caused by coinfection of dengue and chikungunya viruses in a Brazilian patient. Journal of infection and public health. 2017;10:359–360. doi: 10.1016/j.jiph.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 108.Calvo EP, Coronel-Ruiz C, Velazco S, Velandia-Romero M, Castellanos JE. Dengue and chikungunya differential diagnosis in pediatric patients. Biomedica: revista del Instituto Nacional de Salud. 2015;36:35–43. doi: 10.7705/biomedica.v36i0.2982. [DOI] [PubMed] [Google Scholar]
- 109.Carrillo-Hernandez MY, Ruiz-Saenz J, Villamizar LJ, Gomez-Rangel SY, Martinez-Gutierrez M. Co-circulation and simultaneous co-infection of dengue, chikungunya, and zika viruses in patients with febrile syndrome at the Colombian-Venezuelan border. BMC Infect Dis. 2018;18:61. doi: 10.1186/s12879-018-2976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Farrell DF, Lupone CD, Kenneson A, Cueva C, Heydari N, Barzallo Aguilera JH, Polhemus M, Endy TP, Stewart-Ibarra AM. Case report: an acute chikungunya infection and a recent secondary dengue infection in a Peripartum case in Ecuador. The American journal of tropical medicine and hygiene. 2018;98:838–840. doi: 10.4269/ajtmh.17-0781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gomez-Govea MA, Zamudio-Osuna MD, Murillo KDT, Ponce G, Cavazos MED, Tavitas-Aguilar MI, Flores-Suarez AE, Villarreal-Perez JZ, Rodriguez-Sanchez IP. Chikungunya fever in patients from northeastern Mexico. Southwestern Entomologist. 2017;42:143–152. doi: 10.3958/059.042.0114. [DOI] [Google Scholar]
- 112.Mercado M, Acosta-Reyes J, Parra E, Pardo L, Rico A, Campo A, Navarro E, Viasus D. Clinical and histopathological features of fatal cases with dengue and chikungunya virus co-infection in Colombia. 2014 to 2015 Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. 2016;21 [DOI] [PubMed]
- 113.Rosso F, Pacheco R, Rodriguez S, Bautista D. Co-infection by chikungunya virus (CBIK-V) and dengue virus (DEN-V) during a recent outbreak in Cali, Colombia. Report of a fatal case. Revista Chilena De Infectologia. 2016;33:464–467. doi: 10.4067/S0716-10182016000400013. [DOI] [PubMed] [Google Scholar]
- 114.Malik MR, Mnzava A, Mohareb E, Zayed A, Al Kohlani A, Thabet AA, El Bushra H. Chikungunya outbreak in Al-Hudaydah, Yemen, 2011: epidemiological characterization and key lessons learned for early detection and control. Journal of epidemiology and global health. 2014;4:203–211. doi: 10.1016/j.jegh.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rezza G, El-Sawaf G, Faggioni G, Vescio F, Al Ameri R, et al. Co-circulation of dengue and chikungunya viruses, Al Hudaydah, Yemen, 2012. Emerg Infect Dis. 2014;20:1351–1354. doi: 10.3201/eid2008.131615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mugabe VA, Ali S, Chelene I, Monteiro VO, Guiliche O, Muianga AF, Mula F, Antonio V, Chongo I, Oludele J, et al. Evidence for chikungunya and dengue transmission in Quelimane, Mozambique: results from an investigation of a potential outbreak of chikungunya virus. PLoS One. 2018;13:e0192110. doi: 10.1371/journal.pone.0192110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Abdullah M, Tazeen A, Hisamuddin M, Naqvi IH, Verma HN, et al. Virol. 2017. Indian. J. [Google Scholar]
- 118.Gupta N, Gupta C, Gomber A. Concurrent mosquito-borne triple infections of dengue, malaria and chikungunya: a case report. J Vector Borne Dis. 2017;54:191–193. [PubMed] [Google Scholar]
- 119.Tazeen A, Abdullah M, Hisamuddin M, Ali S, Naqvi IH, et al. Concurrent infection with Plasmodium vivax and the dengue and chikungunya viruses in a Paediatric patient from New Delhi, India in 2016. Intervirology. 2017; [DOI] [PubMed]
- 120.Raut CG, Rao NM, Sinha DP, Hanumaiah H, Manjunatha MJ. Chikungunya, dengue, and malaria co-infection after travel to Nigeria, India. Emerg Infect Dis. 2015;21:908–909. doi: 10.3201/eid2105.141804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sinka ME, Bangs MJ, Manguin S, Chareonviriyaphap T, Patil AP, et al. The dominant Anopheles vectors of human malaria in the Asia-Pacific region: occurrence data, distribution maps and bionomic precis. Parasit Vectors. 2011;4:89. doi: 10.1186/1756-3305-4-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Corbel V, Nosten F, Thanispong K, Luxemburger C, Kongmee M, et al. Challenges and prospects for dengue and malaria control in Thailand, Southeast Asia. Trends Parasitol. 2013;29:623–633. doi: 10.1016/j.pt.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 123.Kraemer MU, Sinka ME, Duda KA, Mylne AQ, Shearer FM, et al. The global distribution of the arbovirus vectors Aedes aegypti and ae. albopictus Elife. 2015;4:e08347. doi: 10.7554/eLife.08347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ruan S, Wang W, Levin SA. The effect of global travel on the spread of sars. Math Biosci Eng. 2006;3:205–218. doi: 10.3934/mbe.2006.3.205. [DOI] [PubMed] [Google Scholar]
- 125.Shaqha WM, Fareed M, Chaudhary AA, Azzi A, Shaqha MW, et al. Immunopathogenesis and epidemiology of Middle East respiratory syndrome coronavirus. Journal of Applied Medical Sciences. 2016;5:53–64. [Google Scholar]
- 126.Chen LH, Wilson ME. Dengue and chikungunya infections in travelers. Curr Opin Infect Dis. 2010;23:438–444. doi: 10.1097/QCO.0b013e32833c1d16. [DOI] [PubMed] [Google Scholar]
- 127.Weltman MD, Brotodihardjo A, Crewe EB, Farrell GC, Bilous M, et al. Coinfection with hepatitis B and C or B, C and delta viruses results in severe chronic liver disease and responds poorly to interferon-alpha treatment. J Viral Hepat. 1995;2:39–45. doi: 10.1111/j.1365-2893.1995.tb00070.x. [DOI] [PubMed] [Google Scholar]
- 128.Li XX, Zhou XN. Co-infection of tuberculosis and parasitic diseases in humans: a systematic review. Parasit Vectors. 2013;6:79. doi: 10.1186/1756-3305-6-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Xiang J, Wunschmann S, Diekema DJ, Klinzman D, Patrick KD, et al. Effect of coinfection with GB virus C on survival among patients with HIV infection. N Engl J Med. 2001;345:707–714. doi: 10.1056/NEJMoa003364. [DOI] [PubMed] [Google Scholar]
- 130.Ruiz Silva M, Aguilar Briseno JA, Upasani V, van der Ende-Metselaar H, Smit JM, et al. Suppression of chikungunya virus replication and differential innate responses of human peripheral blood mononuclear cells during co-infection with dengue virus. PLoS Negl Trop Dis. 2017;e0005712:11. doi: 10.1371/journal.pntd.0005712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Patterson J, Sammon M, Garg M. Dengue, Zika and chikungunya: emerging arboviruses in the new world. West J Emerg Med. 2016;17:671–679. doi: 10.5811/westjem.2016.9.30904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sinka ME, Bangs MJ, Manguin S, Rubio-Palis Y, Chareonviriyaphap T, et al. A global map of dominant malaria vectors. Parasit Vectors. 2012;5:69. doi: 10.1186/1756-3305-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Waldock J, Parham PE, Lelieveld J, Christophides GK. Climate and human health: the impact of climate change on vector-borne diseases, Paphos, Cyprus (17-19 October 2012) Pathog Glob Health. 2013;107:387–392. doi: 10.1179/2047772413Z.000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Detailed search strategy. (DOCX 14 kb)