Abstract
Purpose
Racial variation in the financial impact of cancer may contribute to observed differences in the use of guideline-recommended treatments. We describe racial differences with regard to the financial impact of breast cancer in a large population-based prospective cohort study.
Methods
The Carolina Breast Cancer Study oversampled black women and women younger than age 50 years with incident breast cancer in North Carolina from 2008 to 2013. Participants provided medical records and data regarding demographics, socioeconomic status, and financial impact of cancer at 5 and 25 months postdiagnosis. We report unadjusted and adjusted financial impact at 25 months postdiagnosis by race.
Results
The sample included 2,494 women who completed follow-up surveys (49% black, 51% white). Since diagnosis, 58% of black women reported any adverse financial impact of cancer (v 39% of white women; P < .001). In models adjusted for age, stage at diagnosis, and treatment received, black women were more likely to report adverse financial impact attributable to cancer (adjusted risk difference [aRD], +14 percentage points; P < .001), including income loss (aRD, +10 percentage points; P < .001), health care–related financial barriers (aRD, +10 percentage points; P < .001), health care–related transportation barriers (aRD, +10 percentage points; P < .001), job loss (aRD, 6 percentage points; P < .001), and loss of health insurance (aRD, +3 percentage points; P < .001). The effect of race was attenuated when socioeconomic factors were included but remained significant for job loss, transportation barriers, income loss, and overall financial impact.
Conclusion
Compared with white women, black women with breast cancer experience a significantly worse financial impact. Disproportionate financial strain may contribute to higher stress, lower treatment compliance, and worse outcomes by race. Policies that help to limit the effect of cancer-related financial strain are needed.
INTRODUCTION
With cancer care costs rising rapidly,1 patients often are burdened by the cost of their treatment, yet financial toxicity is rarely discussed in the clinic, and many patients and providers have little guidance about where to turn for assistance with financial burden.2 The rising cost of cancer care not only is an increasingly recognized problem on a societal level but also is a potentially devastating facet of the cancer experience for patients.3 Studies have suggested that patients with cancer carry a high burden of financial distress and are more likely to experience financial crises, such as bankruptcy.4 Financial toxicity has been shown to affect both survival and overall quality of life adversely.5,6
Having health insurance does not necessarily protect against the financial distress associated with cancer. One study found that 42% of insured patients with cancer report significant or catastrophic financial burden,7 and a large majority applied for copayment assistance for medications. Many patients have reported wanting to discuss the costs of cancer treatments with their physicians but not having such conversations,8,9 which may be due to cost-benefit information often being opaque to providers as well as to patients and providers not knowing where to direct patients for financial assistance. As a result, many patients with cancer and their families face difficult decisions on their own and forego, delay, or discontinue treatment in light of competing demands.
An understanding of the effects of financial burden among racial minorities, who shoulder a greater burden of poor cancer outcomes, is important.10 Black patients with breast cancer, in particular, have higher mortality and lower initiation of and adherence to guideline-recommended treatments,11-13 which may be closely related to their inability to pay for care. We leveraged a unique prospective cohort enriched for young and working-age women to quantify the financial impact of breast cancer in racially diverse populations.
METHODS
Data
Women were recruited in 2008 to 2013 across 44 counties at the time of diagnosis by rapid case ascertainment through the North Carolina state cancer registry. The Carolina Breast Cancer Study is purposefully enriched such that one half of all participants are black and one half are younger than age 50 years.14 Participants provided consent for access to medical records and self-reported survey data on demographics, socioeconomic status, health-related quality of life, access to care, treatment experiences, and financial impact of cancer at approximately 5 months (baseline) and 25 months (follow-up) postdiagnosis. Study retention was high, with 89.6% of eligible women completing the follow-up survey. Ongoing data collection within this prospective cohort study continues, with final follow-up data expected approximately 10 years postdiagnosis for all participants. This study was approved by the University of North Carolina at Chapel Hill institutional review board.
Financial Impact Measures
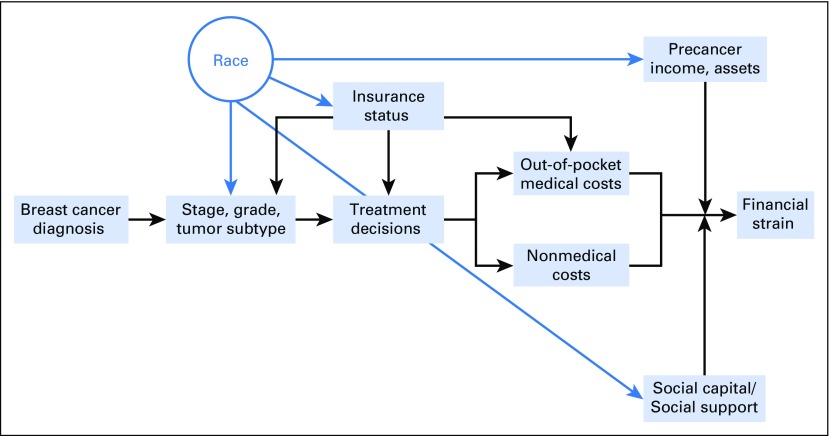
We conceptualized financial impact using a modified model from the National Cancer Institute that describes the direct and indirect contributors to adverse financial impact.15 We modified this model to describe how race is related to multiple factors that directly influence adverse financial impact (Fig 1). Several questions related to financial impact of cancer diagnosis were self-reported by women at 25 months postdiagnosis.
Fig 1.
Conceptual framework. Conceptual model of racial differences in financial impact. Modified from the National Cancer Institute framework on health and financial outcomes.15
Women reported having lost a job and/or income as a result of breast cancer. Those who reported never having worked (n = 15) and who declined to respond about their employment (n = 38) were excluded from the analysis for both of these employment-related outcomes. In addition, women reported whether they had been unable to access any medical care as a result of financial and/or transportation barriers since the time of diagnosis. In a separate question, they were asked whether they refused or delayed any recommended cancer treatment because of cost and/or transportation. These health care access and treatment refusal/delay questions were combined into one indicator each for financial and transportation barriers to care after diagnosis.
We also assessed loss of private insurance during the study period to estimate cancer-attributable financial burden. We focused on insurance changes that were likely to result from cancer treatment that rendered women unable to work or to afford private insurance premiums (as opposed to changes in public insurance primarily driven by entitlement programs on the basis of eligibility). Women’s insurance status and type of insurance were assessed at both time points. Those who self-identified as having private insurance during the 5-month survey but who were uninsured at the 25-month survey were coded as having lost private insurance. Analyses for this variable, therefore, restricted the sample to only women who had private insurance at the time of the first survey (n = 1,834). Finally, we assessed a measure of any adverse financial outcome as a summary indicator that reflected whether an individual reported one or more of the five outcomes studied.
Control Variables
The primary analyses control for clinical differences (eg, tumor stage) that may vary by race and lead to differences in clinical decision making and treatment-related costs. Medical record abstraction was used to determine tumor stage and treatment history and measured using binary indicators for receipt of mastectomy, chemotherapy, radiation therapy, trastuzumab, and adjuvant endocrine therapy. Comorbidity burden also may vary by race and influence the extent of financial burden and was measured from medical records at the time of diagnosis, including obesity, diabetes, chronic obstructive pulmonary disease, hypertension, and heart disease. Age was self-reported at the baseline survey.
In secondary analyses, we added to the models socioeconomic variables that may vary by race and influence one’s ability to cope financially with high medical and nonmedical expenses. Educational attainment, annual household income, and insurance status were self-reported at baseline. Women could report more than one source of insurance, and these were organized into mutually exclusive categories such that dual Medicaid/Medicare beneficiaries were identified as having any Medicaid, and Medicare beneficiaries who also reported supplemental private insurance were classified as having any private coverage. We also included self-reported marital status as one measure of social support because this has been associated with financial vulnerability and cancer outcomes.16,17
Analysis
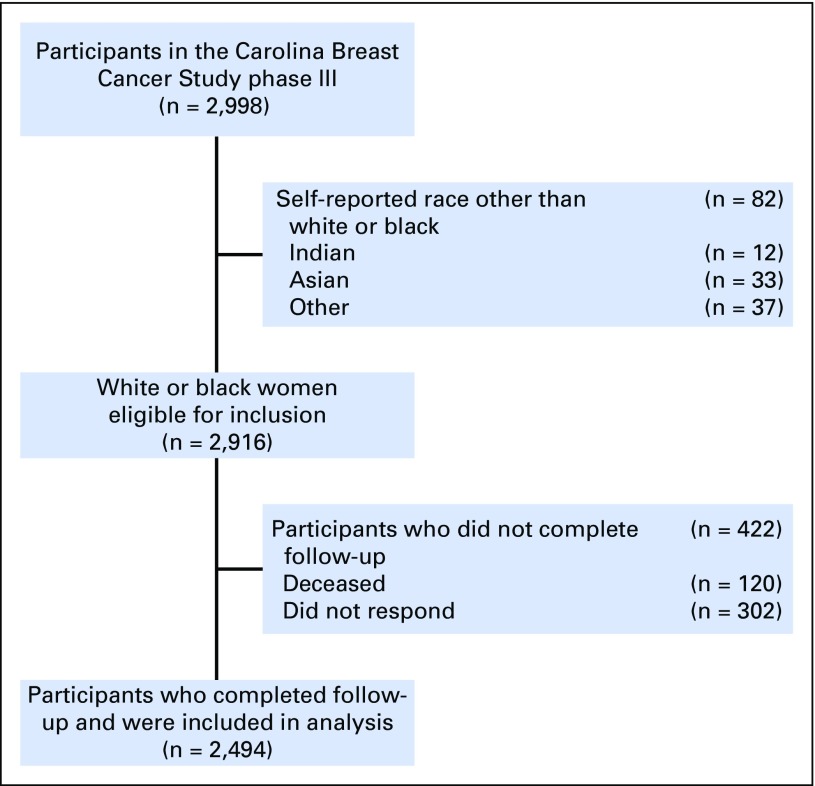
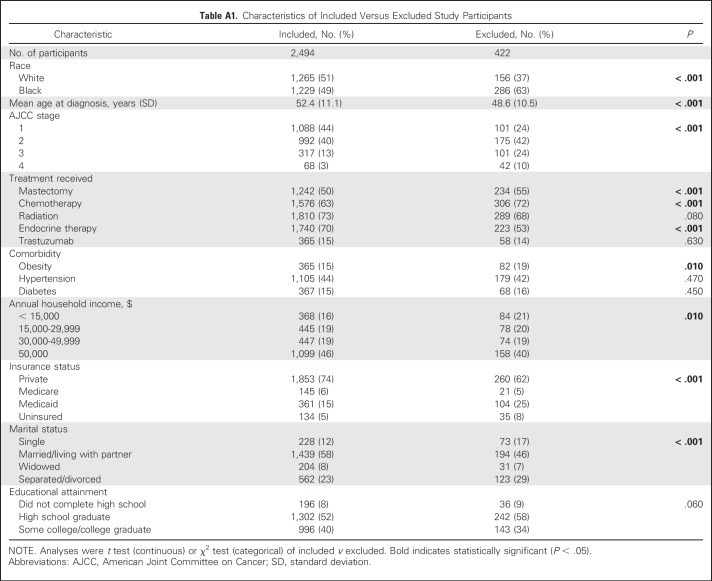
From 2,998 study participants, we excluded women who reported a race other than black or white (n = 82) because it would be inappropriate to analyze these individuals as one group, yet small sample sizes within each category precluded analysis (Appendix Fig A1, online only). We also excluded women who did not complete the follow-up survey (n = 422) because of death (n = 120) or nonresponse (n = 302). Although small in number, we found that those excluded because of death or nonresponse often were, on average, black and younger, had a higher stage at diagnosis, and were of lower socioeconomic status than those who completed the follow-up (Appendix Table A1, online only). Any bias that resulted from exclusion of these more vulnerable groups would likely be small but, if anything, would have shifted the reported findings toward more conservative estimates of financial burden.
We first examined unadjusted racial differences in prevalence of adverse financial impact. To account for a small number of women with missing values for income (5%), tumor stage (2%), or baseline insurance status (< 1%), we performed multiple imputation to estimate values for missing variables. Fifty imputed data sets were created, with results combined as described by Rubin.18 Sensitivity analysis using only complete cases yielded similar findings for all outcomes.
By following recommendations by the Institute of Medicine,19 we first specified multivariable logistic regressions for each of the six dichotomous outcomes of interest and adjusted for race and clinical differences only. To determine the extent to which racial differences in adverse financial impact were explained by differences in underlying socioeconomic status, in secondary analyses, we added to these regressions socioeconomic variables, including self-reported education, income, marital status, and insurance status. We examined model fit because these variables were added sequentially. Among clinical variables, age was associated with the largest improvement in model fit, and among socioeconomic variables, income was associated with the largest increase in model fit, with insurance also explaining a large portion of the variation. Results from the primary, partially adjusted models can be interpreted as the total or joint effect of race,20 whereas results from the secondary, fully adjusted models can be interpreted as the direct residual effect of race.21
We also examined potential interactions between race and treatment indicators for radiation therapy and endocrine therapy to explore whether racial differences in financial burden exist within various treatment subgroups. Because these findings were inconsistent in magnitude, direction, and statistical significance and did not meaningfully improve model fit, we reverted to and present our final models without interactions.
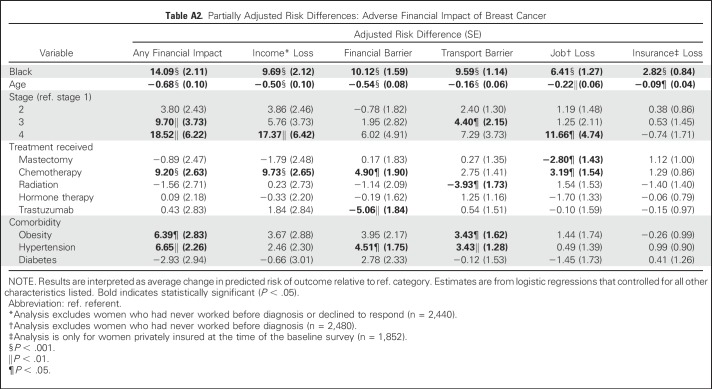
Regression results are presented as adjusted risk differences (aRDs), which describe the absolute difference in the likelihood of each outcome for black (relative to white) women, after controlling for other characteristics.22 We also present adjusted risk ratios in Appendix Table A2 (online only).
Stata 13 software (StataCorp, College Station, TX) was used for the statistical analysis. A significance level of .05 was used for all analyses.
RESULTS
The final sample included 1,265 white women and 1,229 black women (Table 1). On average, women were 52 years of age at the time of diagnosis, and black women were slightly but significantly younger than white women (P = .01). Black women more often presented with higher-stage disease at the time of diagnosis (P < .001) and more often received chemotherapy (69% v 58%; P < .001) and radiation therapy (75% v 70%; P = .003). Black women more often than white women presented with comorbid conditions at diagnosis, including obesity (19% v 10%; P < .001), hypertension (58% v 31%; P < .001), and diabetes (22% v 8%; P < .001). Black women also were more socioeconomically disadvantaged relative to white women, including having lower average household incomes, lower education, and higher rates of both Medicaid and no insurance. Black women were significantly less likely to be married than white women (43% v 72%; P < .001).
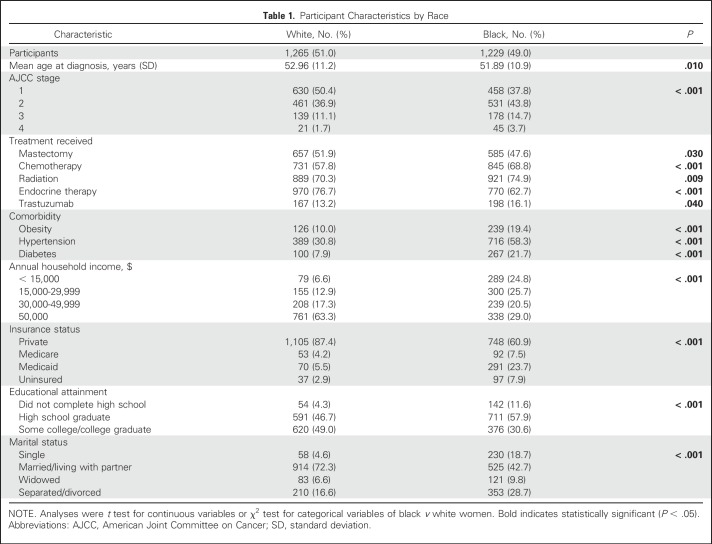
Table 1.
Participant Characteristics by Race
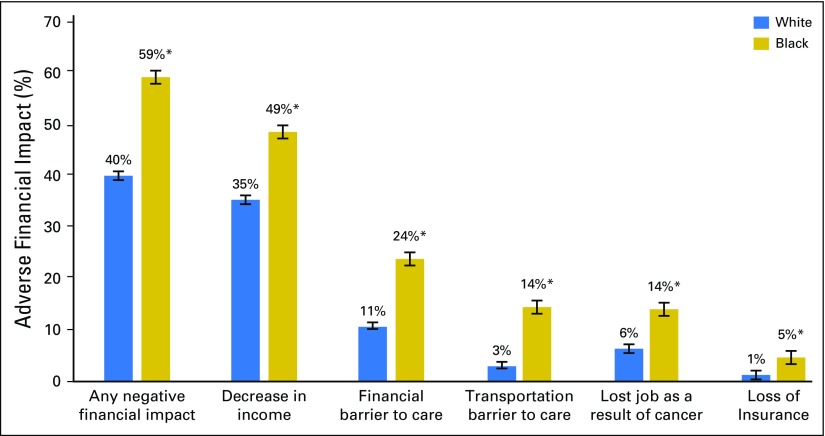
Negative financial impact was common among all breast cancer survivors (48%), but prevalence was strikingly higher among black versus white women (58% v 39%; P < .001). Since diagnosis, black women more often lost private insurance (5% v 1%; P < .001), lost a job (14% v 6%; P < .001), or experienced a financial barrier to health care (24% v 11%; P < .001). Black women also were four times more likely to experience a transportation barrier (14% v 3%; P < .001) than white women (Fig 2).
Fig 2.
Unadjusted probability of adverse financial impact by race. Bars represent SEs. (*)P < .001, black versus white.
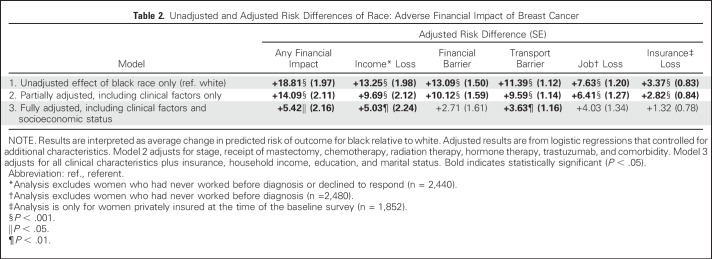
Adjustment for clinical differences explained some of the variation in financial impact, but racial differences remained large and statistically significant (Table 2; Appendix Table A1). Compared with white women, black women were 14.1 percentage points more likely to experience a financial impact (P < .001) and after controlling for clinical differences, were significantly more likely to experience each individual measure of financial impact, including a financial barrier (aRD, +10.1 percentage points; P < .001), loss of income (aRD, +9.7 percentage points; P < .001), transportation barrier (aRD, +9.6 percentage points; P < .001), loss of a job (aRD, +6.4 percentage points; P < .001), and loss of insurance (aRD, +2.8 percentage points; P < .001; Table 2).
Table 2.
Unadjusted and Adjusted Risk Differences of Race: Adverse Financial Impact of Breast Cancer
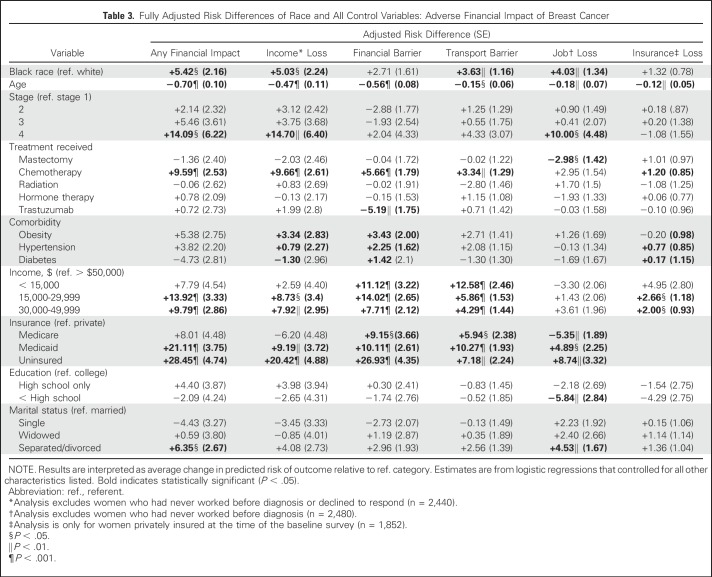
Additional adjustment for socioeconomic characteristics explained much of the racial differences for both income loss and financial barriers to care. However, risk differences in other financial outcomes, although attenuated, remained statistically significant (Table 2). After controlling for income, insurance status, marital status, and education, black women remained 5.4 percentage points more likely to experience any financial impact (P = .01), 5.0 percentage points more likely to lose income (P = .02), 3.6 percentage points more likely to experience transportation barriers (P = .002), and 4.0 percentage points more likely to lose a job (P = .003) than white women.
In fully adjusted models, each additional year of age reduced the risk of experiencing any financial impact by 0.7 percentage points (P < .001; Table 3). Women with stage IV breast cancer at diagnosis were more likely than those with stage I disease at diagnosis to experience any adverse financial impact (aRD, +14.1 percentage points; P = .02). Women who received chemotherapy versus those who did not were 9.6 percentage points more likely to experience an adverse financial impact (P < .001). Of note, receipt of trastuzumab was negatively associated with experiencing a financial barrier to care (aRD, −5.2 percentage points; P = .003) but not with other outcomes.
Table 3.
Fully Adjusted Risk Differences of Race and All Control Variables: Adverse Financial Impact of Breast Cancer
Compared with women with an annual income > $50,000, those with an annual income of $15,000 to $29,999 more often reported any adverse financial impact (aRD, +13.9 percentage points; P < .001) and having experienced a reduction in income (aRD, +8.8 percentage points; P = .02), a financial barrier to care (aRD, +14.0 percentage points; P < .001), and a loss of insurance (aRD, +2.7 percentage points; P = .002; Table 3). Women who earned < $15,000 per year were most likely to report a transportation barrier to care (aRD, +12.6 percentage points; P < .001) compared with those who earned > $50,000 per year.
Insurance also was a strong predictive factor, with uninsured women 28.4 percentage points more likely (P < .001) and Medicaid-insured women 21.1 percentage points more likely (P < .001) than the privately insured to experience any adverse financial impact (Table 3). Medicaid enrollees were more likely than any other group to experience transportation barriers (aRD, +10.3 percentage points; P < .001). Relative to being single, being separated or divorced was associated with an increase of 4.5 percentage points in the probability of losing a job as a result of cancer (P = .007) and a increase of 6.4 percentage points in the probability of any adverse financial impact (P = .02; Table 3).
DISCUSSION
Prevalence of adverse financial impact of cancer is high among all breast cancer survivors, and black women experience a disproportionate share of this burden. Overall, the study found that adverse financial impact is reported by more than one half of black women and more than one third of white women, a large proportion of which is attributable to lost income postdiagnosis. By controlling for only clinical differences,20 we found that black women were at greater risk than white women for all measured adverse financial impacts. The effect of black race was somewhat attenuated when baseline education, income, occupation, and health insurance were also included in models but remained significantly associated with the majority of adverse outcomes. The remaining racial differences in adverse financial impact, once both clinical and socioeconomic variables have been controlled for (the direct residual effect), may reflect unmeasured differences in social capital, household economic dynamics (eg, caregiving burden, single-income households), or asset reserves that vary by race and contribute to greater cancer-related financial strain among black women.
High cancer-related financial burden has been shown to affect treatment choice, treatment compliance, and cancer outcomes.6,23 Although prior studies have drawn attention to the increasing burden of cancer-related financial toxicity,5,24,25 we are aware of no study that has directly measured and reported on the extent of racial and age-related differences in the financial burden of cancer because of insufficient samples of black and young women. Because we oversampled both black and young women in equal proportions, we can report on the experiences of these important subpopulations who shoulder a greater burden of poor cancer outcomes. Of note, racial and age-related disparities in breast cancer outcomes13,26 may be related, at least in part, to cost-related undertreatment.27,28 Prior studies of commercially insured populations have shown that high out-of-pocket costs and younger age are related to nonadherence to aromatase inhibitors but lack detail on racial identification.28 An increased focus on financial strain as a potential driver of outcome disparities may help to reduce differences in recurrence and survival.29
Several limitations should be considered. First, this study reflects racial differences within a single region that may not be representative of experiences elsewhere, particularly in states where additional policy differences, such as Medicaid expansion or out-of-pocket restrictions on oral chemotherapy drug pricing, may reduce overall cost burden for patients with cancer. Nevertheless, North Carolina is an ideal state in which to examine these issues because of its large size and socioeconomic diversity. Of North Carolina’s 9.9 million residents, approximately 30% are minorities, and 22% are African American compared with the national average of 13%.30 Economic conditions are in line with national averages, with slightly more than a quarter being college educated and 18% living below the poverty line. Therefore, we believe that the findings are largely generalizable, particularly for states with few policies to address financial burden. In addition, we do not have information that reflects actual out-of-pocket health care spending for study participants, only a perceived burden as a result of cancer care costs. However, our goal was to measure the differences in patient-perceived rather than objective hardship as a result of high cancer costs; therefore, we believe that our measure is an accurate reflection of the effect of cancer costs on patients. Although we recognize the vital importance of the Affordable Care Act–related health insurance expansions that occurred during the study period, which likely affected financial vulnerability, the study did not capture longitudinal changes in health insurance enrollment with any granularity. Future studies should examine in more detail the role of insurance changes in cancer-related financial vulnerability over time to ensure sufficient samples of public and private insurance plan enrollees. Finally, we were limited to only 2 years of follow-up data, but because Carolina Breast Cancer Study data capture is ongoing, we eventually will examine the longer-term financial burden; cancer-related outcomes such as endocrine therapy adherence, recurrence, and breast cancer–specific mortality; and emotional and physical sequelae associated with this financial burden.
An urgent need exists for research on the financial needs of diverse patients with breast cancer as well as for the development of interventions and support tools that identify and match patients to resources for financial assistance, can be delivered broadly across a variety practice settings, and are user friendly to facilitate discussions between patients and providers about addressing financial barriers to treatment. Policies and programs that help to limit and mitigate the effects of cancer-related financial strain are needed, including ensuring greater price transparency. Finally, providers should recognize and communicate with patients about the potential for cancer-related financial strain and, where possible, offer higher-value treatment alternatives, particularly for minority women who may be more financially vulnerable. In the absence of such interventions, black women will continue to shoulder a disproportionate burden of cancer-related financial strain and downstream disparate cancer outcomes.
ACKNOWLEDGMENT
We thank Robert Millikan, PhD; Melissa Troester, PhD; Mary Beth Bell; Chiu Kit Tse; Jo Anne Earp, ScD; Shelley Earp, MD; Carol Golin, MD; Bryan Weiner, PhD; Michael Pignone, MD MPH; Ethan Basch, MD MSc; all the patients with breast cancer; and the staff who made the Carolina Breast Cancer Study possible.
Appendix
Fig A1.
Inclusion/exclusion of study participants.
Table A1.
Characteristics of Included Versus Excluded Study Participants
Table A2.
Partially Adjusted Risk Differences: Adverse Financial Impact of Breast Cancer
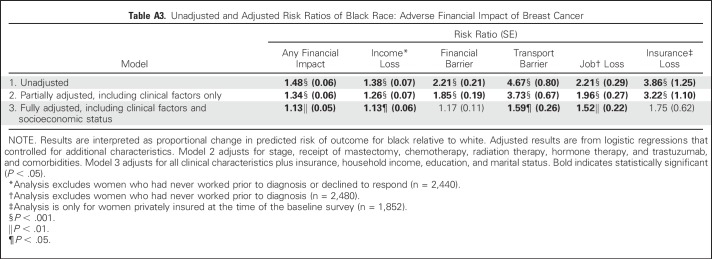
Table A3.
Unadjusted and Adjusted Risk Ratios of Black Race: Adverse Financial Impact of Breast Cancer
Footnotes
Supported by American Cancer Society Mentored Research Scholar grant MRSG-13-157-01-CPPB (to S.B.W., “Improving Endocrine Therapy Utilization in Racially Diverse Populations”), the University Cancer Research Fund of North Carolina and the National Cancer Institute Specialized Program of Research Excellence in Breast Cancer grant P50-CA58223, National Cancer Institute grant P01-CA151135, and the Susan G. Komen Foundation (CCR 15333140).
Presented at the 2017 American Society for Clinical Oncology Annual Meeting, Chicago, IL, June 2-6, 2017.
Listen to the podcast by Dr Yabroff at ascopubs.org/jco/podcasts
AUTHOR CONTRIBUTIONS
Conception and design: Stephanie B. Wheeler, Jennifer C. Spencer, Laura C. Pinheiro, Lisa A. Carey, Katherine E. Reeder-Hayes
Financial support: Stephanie B. Wheeler, Andrew F. Olshan, Katherine E. Reeder-Hayes
Administrative support: Stephanie B. Wheeler, Jennifer C. Spencer
Provision of study materials or patients: Andrew F. Olshan
Collection and assembly of data: Stephanie B. Wheeler, Andrew F. Olshan
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Financial Impact of Breast Cancer in Black Versus White Women
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Stephanie B. Wheeler
Research Funding: Pfizer
Jennifer C. Spencer
Research Funding: Pfizer
Laura C. Pinheiro
Employment: Johnson & Johnson (I)
Lisa A. Carey
Research Funding: GlaxoSmithKline (Inst), Genentech (Inst), Roche (Inst)
Andrew F. Olshan
No relationship to disclose
Katherine E. Reeder-Hayes
Research Funding: Pfizer
REFERENCES
- 1.Howard DH, Bach PB, Berndt ER, et al. : Pricing in the market for anticancer drugs. J Econ Perspect 29:139-162, 2015 [DOI] [PubMed] [Google Scholar]
- 2. doi: 10.1093/jnci/djv370. Zafar SY: Financial toxicity of cancer care: It’s time to intervene. J Natl Cancer Inst 108:djv370, 2016. [DOI] [PubMed] [Google Scholar]
- 3.Schnipper LE, Meropol N: ASCO addresses the rising cost of cancer care. J Oncol Pract 5:214-215, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramsey S, Blough D, Kirchhoff A, et al. : Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 32:1143-1152, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zafar SY, McNeil RB, Thomas CM, et al. : Population-based assessment of cancer survivors’ financial burden and quality of life: A prospective cohort study. J Oncol Pract 11:145-150, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramsey SD, Bansal A, Fedorenko CR, et al. : Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol 34:980-986, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zafar SY, Peppercorn JM, Schrag D, et al. : The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 18:381-390, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irwin B, Kimmick G, Altomare I, et al. : Patient experience and attitudes toward addressing the cost of breast cancer care. Oncologist 19:1135-1140, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bestvina CM, Zullig LL, Yousuf Zafar S: The implications of out-of-pocket cost of cancer treatment in the USA: A critical appraisal of the literature. Future Oncol 10:2189-2199, 2014 [DOI] [PubMed] [Google Scholar]
- 10.Edwards BK, Brown ML, Wingo PA, et al. : Annual report to the nation on the status of cancer, 1975-2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst 97:1407-1427, 2005 [DOI] [PubMed] [Google Scholar]
- 11.Reeder-Hayes KE, Meyer AM, Dusetzina SB, et al. : Racial disparities in initiation of adjuvant endocrine therapy of early breast cancer. Breast Cancer Res Treat 145:743-751, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts MC, Wheeler SB, Reeder-Hayes K: Racial/ethnic and socioeconomic disparities in endocrine therapy adherence in breast cancer: A systematic review. Am J Public Health 105:e4-e15, 2015. (suppl 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wheeler SB, Reeder-Hayes KE, Carey LA: Disparities in breast cancer treatment and outcomes: Biological, social, and health system determinants and opportunities for research. Oncologist 18:986-993, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hair BY, Hayes S, Tse C-K, et al. : Racial differences in physical activity among breast cancer survivors: Implications for breast cancer care. Cancer 120:2174-2182, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National Cancer Institute: Financial Toxicity and Cancer Treatment (PDQ®)–Health Professional Version, 2017. https://www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-hp-pdq. [PubMed]
- 16.Aizer AA, Chen M-H, McCarthy EP, et al. : Marital status and survival in patients with cancer. J Clin Oncol 31:3869-3876, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eskander MF, Schapira EF, Bliss LA, et al. : Keeping it in the family: The impact of marital status and next of kin on cancer treatment and survival. Am J Surg 212:691-699, 2016 [DOI] [PubMed] [Google Scholar]
- 18. Rubin DB: Multiple Imputation for Nonresponse in Surveys, Volume 81. New York, NY, John Wiley & Sons, 2004. [Google Scholar]
- 19.Nelson A: Unequal treatment: Confronting racial and ethnic disparities in health care. J Natl Med Assoc 94:666-668, 2002 [PMC free article] [PubMed] [Google Scholar]
- 20.VanderWeele TJ, Robinson WR: On the causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology 25:473-484, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lê Cook B, McGuire TG, Zuvekas SH: Measuring trends in racial/ ethnic health care disparities. Med Care Res Rev 66:23-48, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Norton EC, Miller MM, Kleinman LC: Computing adjusted risk ratios and risk differences in Stata. Stata J 13:492-509, 2013 [Google Scholar]
- 23.Hendren S, Chin N, Fisher S, et al. : Patients’ barriers to receipt of cancer care, and factors associated with needing more assistance from a patient navigator. J Natl Med Assoc 103:701-710, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Altice CK, Banegas MP, Tucker-Seeley RD, et al. : Financial hardships experienced by cancer survivors: A systematic review. J Natl Cancer Inst 109:djw205, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jagsi R, Pottow JAE, Griffith KA, et al. : Long-term financial burden of breast cancer: Experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol 32:1269-1276, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruddy KJ, Gelber S, Tamimi RM, et al. : Breast cancer presentation and diagnostic delays in young women. Cancer 120:20-25, 2014 [DOI] [PubMed] [Google Scholar]
- 27.Walker HE, Rosenberg SM, Stanton AL, et al. : Perceptions, attributions, and emotions toward endocrine therapy in young women with breast cancer. J Adolesc Young Adult Oncol 5:16-23, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sedjo RL, Devine S: Predictors of non-adherence to aromatase inhibitors among commercially insured women with breast cancer. Breast Cancer Res Treat 125:191-200, 2011 [DOI] [PubMed] [Google Scholar]
- 29.Miller JW, Smith JL, Ryerson AB, et al. : Disparities in breast cancer survival in the United States (2001-2009): Findings from the CONCORD-2 study. Cancer 123:5100-5118, 2017. (suppl 24) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. US Census Bureau: Quick Facts, 2016. https://www.census.gov/quickfacts/fact/table/US/PST045216.