Abstract
Background. The estimated lifetime prevalence of physical or sexual intimate partner violence (IPV) is 30% among women worldwide. Understanding risk and protective factors is essential for designing effective prevention strategies.
Objectives. To quantify the associations between prospective–longitudinal risk and protective factors and IPV and identify evidence gaps.
Search methods. We conducted systematic searches in 16 databases including MEDLINE and PsycINFO from inception to June 2016. The study protocol is registered with PROSPERO (CRD42016039213).
Selection criteria. We included published and unpublished studies available in English that prospectively analyzed any risk or protective factor(s) for self-reported IPV victimization among women and controlled for at least 1 other variable.
Data collection and analysis. Three reviewers were involved in study screening. One reviewer extracted estimates of association and study characteristics from each study and 2 reviewers independently checked a random subset of extractions. We assessed study quality with the Cambridge Quality Checklists. When studies investigated the same risk or protective factor using similar measures, we computed pooled odds ratios (ORs) by using random-effects meta-analyses. We summarized heterogeneity with I2 and τ2. We synthesized all estimates of association, including those not meta-analyzed, by using harvest plots to illustrate evidence gaps and trends toward negative or positive associations.
Main results. Of 18 608 studies identified, 60 were included and 35 meta-analyzed. Most studies were based in the United States. The strongest evidence for modifiable risk factors for IPV against women were unplanned pregnancy (OR = 1.66; 95% confidence interval [CI] = 1.20, 1.31) and having parents with less than a high-school education (OR = 1.55; 95% CI = 1.10, 2.17). Being older (OR = 0.96; 95% CI = 0.93, 0.98) or married (OR = 0.93; 95% CI = 0.87, 0.99) were protective.
Conclusions. To our knowledge, this is the first systematic, meta-analytic review of all risk and protective factors for IPV against women without location, time, or publication restrictions. Unplanned pregnancy and having parents with less than a high-school education, which may indicate lower socioeconomic status, were shown to be risk factors, and being older or married were protective. However, no prospective–longitudinal study investigated the associations between IPV against women and any community or structural factor outside the United States, and more studies investigated risk factors related to women as opposed to their partners.
Public health implications. This review highlights that prospective evidence for perpetrator- and context-related risk and protective factors for women’s experiences of IPV outside of the United States is lacking and urgently needed to inform global policy recommendations. The current evidence base of prospective studies suggests that, at least in the United States, education and sexual health interventions may be effective targets for preventing IPV against women, with young, unmarried women at greatest risk.
PLAIN LANGUAGE SUMMARY
Intimate partner violence (IPV) is the most common form of violence perpetrated against women, yet few interventions exist that effectively prevent IPV in the first instance. Designing effective prevention requires knowing which conditions will, when changed, increase or decrease the risk of women experiencing IPV—also known as risk and protective factors, respectively. To our knowledge, our study is the first to systematically review all available studies of risk and protective factors for IPV against women over time. We identified 60 longitudinal studies, most of which were conducted in the United States. The most important risk factors identified from these studies were unplanned pregnancy and having parents with less than a high-school education, a plausible proxy for lower socioeconomic status. We also found that young, unmarried women were at greatest risk of experiencing IPV, suggesting that these women and their partners may require targeted programming. However, our review revealed that most longitudinal studies focused on how women’s characteristics relate to their own experiences of IPV, with few studies investigating contextual or perpetrator risk factors. More longitudinal research in these priority areas is urgently needed, especially from outside the United States and in low- and middle-income countries, before global policy recommendations can be drawn.
Intimate partner violence (IPV)—actual or threatened physical, psychological, or sexual violence by a current or former partner—is the most common violence perpetrated against women.1 Lifetime prevalence estimates are high for all World Health Organization (WHO) regions, ranging from 23% to 38% among ever-partnered women.2 Intimate partner violence is associated with severe negative health outcomes for women, including death, injury, psychological disorders, sexually transmitted infections, and chronic diseases.
The ecological framework conceptualizing IPV as the result of the interplay among individual, relational, community, and structural factors is widely accepted in public health (Appendix A, Figure 1, available as a supplement to this article at http://www.ajph.org).3,4 Yet there has been no complete, systematic assessment of this model. Previous reviews have conducted nonsystematic searches, pooled mainly cross-sectional studies with longitudinal, and only focused on physical IPV.5,6 Other reviews have included only subsets of risk factors (e.g., alcohol use)7–11 or subpopulations (e.g., high-income countries).12 These reviews have also largely included only peer-reviewed evidence, which tends to overestimate associations.
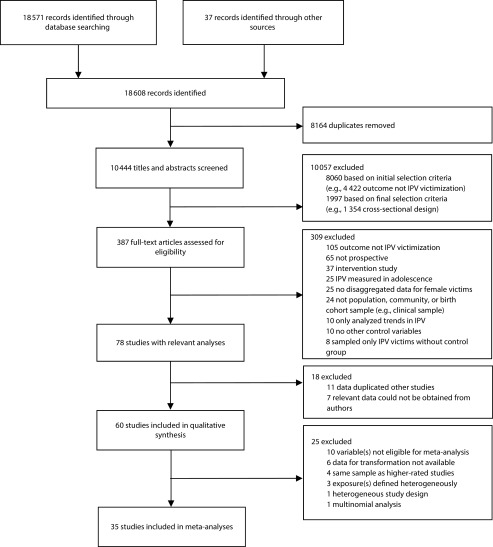
FIGURE 1—
Flow Diagram of Study Selection for Systematic Review and Meta-Analyses of Prospective–Longitudinal Studies of Risk and Protective Factors for Intimate Partner Violence Against Women
Note. IPV = intimate partner violence.
Hundreds of cross-sectional studies have examined factors associated with IPV against women at all ecological levels, including substance misuse (at both the individual and relational levels), childhood exposure to violence (relational), and traditional gender norms (structural).4 Although these studies identified research priorities and population targets for interventions, developing effective interventions for preventing IPV in the first instance requires knowing which conditions will, when changed, increase the risk of IPV (risk factors) or decrease this risk (protective factors)—best evidenced by prospective–longitudinal studies, which measure exposures and outcomes over time.13
We thus conducted, to our knowledge, the first systematic review and meta-analyses of prospective–longitudinal risk and protective factors for different types of IPV against women at all ecological levels. We aimed to estimate the strength of each association, to inform programmatic decisions, and identify evidence gaps across contexts and types of IPV.
METHODS
The review protocol is registered with PROSPERO (CRD42016039213). We undertook a rigorous search strategy, developed in consultation with 2 information specialists (see Appendix A, Tables 1 and 2, available as supplements to this article at http://www.ajph.org, for complete strategy). We searched 16 electronic databases from inception to June 2016: MEDLINE, Embase, Global Health, CINAHL, PsycINFO, Web of Science, Google Scholar, Applied Social Sciences Index and Abstracts, ProQuest Dissertations and Abstracts, OpenGrey, National Criminal Justice Reference Service Abstracts Database, Cochrane Library, Sociological Abstracts, World Bank Open Knowledge Repository, WHO Institutional Repository for Information Sharing, and WHO Prevent Violence Evidence Base and Resources. We screened reference lists of all systematic reviews identified for eligible studies and contacted authors whenever their articles mentioned but did not present eligible data (e.g., gender-disaggregated analyses).
We chose selection criteria iteratively in 2 stages given the extensive literature on IPV.9 In the initial stage, 2 reviewers screened titles and abstracts for studies examining at least 1 risk or protective factor for IPV against women, using any quantitative design. After this initial screening, we limited our focus to prospective studies given that these by design will produce the best evidence for risk and protective factors. Three reviewers screened the remaining studies by using these final selection criteria, first by titles and abstracts followed by full texts as needed.
We included studies that were published or unpublished, available in English, and had quantitatively analyzed at least 1 risk or protective factor for physical, sexual, or psychological IPV in a population, community, or birth cohort sample, with adjustment for at least 1 other variable. Participants had to be at least 19 years old at outcome assessment, according to the WHO definition of adulthood.14 Studies had to include women’s self-reports of IPV victimization (including those that used both partner reports and self-reports or conducted gender-disaggregated analyses). We excluded studies that only measured self-reported perpetration because people tend to self-report experiencing IPV more than their partners self-report perpetrating violence.15 Finally, we included only prospective–longitudinal studies, defined as having at least 2 assessment waves, where exposure to the risk or protective factor was measured before the outcome. We excluded data on risk or protective factor(s) when they were measured at the same time point as the outcome without analyzing change, they were measured retrospectively (e.g., retrospective history of child abuse), or the outcome was lifetime as opposed to current IPV prevalence (e.g., within the past year). In each of these cases, it would not be possible to determine whether the exposure preceded IPV without, for instance, recall bias (see Appendix A, Table 3 for complete selection criteria and rationale).
Data Extraction and Quality Assessment
One reviewer extracted study characteristics and effect estimates for eligible risk or protective factors by using a piloted form. At each stage of screening and extraction, 2 reviewers double-coded a random selection of studies (5%–10%); there were no substantive discrepancies. We appraised study quality by using the Cambridge Quality Checklists,16 which assess the quality of correlational evidence for risk and protective factors (on the basis of sampling, participation rates, sample size, and measurement reliability), temporal evidence (whether data are cross-sectional, retrospective, or prospective), and causal evidence (whether there is variation in the risk or protective factor, change in outcomes is analyzed, and confounding is accounted for; Appendix A, Table 4, available as a supplement to this article at http://www.ajph.org). We computed a percentage score for each study on the basis of the study’s total score across all 3 checklists. Common sources of low scores are discussed.
Data Analysis
When 2 or more studies investigated the same risk or protective factor and used similar measures, we conducted a random-effects meta-analysis in Stata version 13.1 (StataCorp LP, College Station, TX) using the method of moments estimator.17 We selected this model a priori given the expected methodological and contextual differences in studies. We considered studies that did not use similar methods (e.g., diverse variable definitions) to be clinically heterogeneous and did not combine them. We computed odds ratios (ORs) as studies typically reported binary outcomes. We entered log odds and SEs and conducted data transformations wherever necessary and possible (see Appendix A for conventions). When studies did not provide precision estimates or P values, we conducted the meta-analysis twice: once with SE estimated based on a liberal P value (P = .06) and once assuming a conservative P value (P = .50).
We meta-analyzed categorical and continuous measures of the same exposure in different studies separately according to best practice.18 We combined effect estimates from analyses of within-participant change with those from analyses of independent groups wherever unstandardized estimates were provided or could be derived to ensure comparable metrics.19 I2 indicated the total variation among study effects and τ2 indicated between-study variance. We did not quantitatively explore sources of heterogeneity given the small number of studies (usually < 4) per meta-analysis. We summarized meta-analyses by using forest plots (Appendix A, Figures 2–4, available as supplements to this article at http://www.ajph.org), which indicate the number of covariates controlled for in each study; however, after descriptively observing these, we found no systematic relationship between effect direction or significance and the level of covariate control.
To describe all available evidence, regardless of meta-analysis eligibility, we summarized all included studies with harvest plots, which graphically synthesize heterogeneous effect estimates.20 These plots provide a novel summary that illustrates where evidence gaps exist; whether the weight of evidence suggests positive, statistically nonsignificant, or negative effects for each type of IPV (physical, psychological, or sexual); and study quality. When there were multiple effect estimates from the same data, we followed a decision-making algorithm based on previous reviews21 to select the most rigorous and relevant data at greatest maturity (Appendix A, Figure 5, available as a supplement to this article at http://www.ajph.org). We did not use methods for combining multiple effect estimates from a single sample (e.g., robust variance estimation) because of the low number of such cases, which produces inaccurate pooled effect estimates.22
RESULTS
After we screened 18 608 titles and abstracts, 309 studies were eligible for full-text review (Figure 1). Sixty studies satisfied all selection criteria, totaling 35 cohort samples (references for all included studies are in Appendix B, available as a supplement to this article at http://www.ajph.org). We meta-analyzed effect estimates for 35 of the 60 studies.23–57 Reasons for exclusion from meta-analyses included only examining variables not eligible for meta-analysis (e.g., early union, where only 1 study was available; n = 10); not providing data required for transformations (n = 6); using the same sample as higher-ranked studies, as per the algorithm (n = 4); and defining exposures heterogeneously to other studies (n = 3). In addition, 1 study used a 56-day diary design too heterogeneous to combine with other studies and another stratified relevant outcome data across multinomial categories that were not pooled—thus, we excluded both.
The 60 studies included in the qualitative synthesis were largely based in the United States (n = 48), with only 7 other countries represented—3 of which were low- or middle-income countries (LMICs; Table 1). Sample sizes ranged from 118 to 34 653 participants (mean = 3126) and study duration ranged from 56 days to 40 years (mean = 9.3 years), with an average of 5.7 follow-ups. Most studies began with an adult sample and slightly fewer than half (n = 29) followed women until a mean age of 30 years or younger. More than half of the studies (n = 32) used analysis of change when defined liberally; however, this was largely by controlling for baseline IPV (n = 23). When we defined analysis of change more stringently (analysis of within-subject variation), only 9 met this condition. All studies but 1 analyzed physical IPV, whereas only 21 analyzed sexual IPV and 17 psychological; 7 studies measured all 3 types. Most studies measured IPV via women’s self-report only (n = 40). The majority of studies analyzed past-year prevalence of IPV, ranging from 1.5% (criminal incidents of physical or sexual IPV) to 80.0% (any physical, psychological, or sexual IPV). See Table 7 in Appendix A (available as a supplement to this article at http://www.ajph.org) for all study outcomes.
TABLE 1—
Summary Statistics for 60 Included Prospective–Longitudinal Studies of Risk and Protective Factors for Intimate Partner Violence Against Women
| Characteristic | No. Studies (%) |
| Year of publication | |
| 1986–1999 | 8 (13.3) |
| 2000–2010 | 31 (51.7) |
| 2011–June 2016 | 21 (35.0) |
| Country | |
| Canada | 1 (1.7) |
| India | 3 (5.0) |
| New Zealand | 4 (6.7) |
| South Africa | 1 (1.7) |
| South Korea | 1 (1.7) |
| Uganda | 1 (1.7) |
| United Kingdom | 1 (1.7) |
| United States | 48 (80.0) |
| Developmental stage at baseline | |
| Birth | 3 (5.0) |
| Childhood (0–9 y) | 4 (6.7) |
| Adolescence (10–19 y) | 19 (31.7) |
| Adulthood (> 19 y) | 34 (56.7) |
| Demographic area | |
| Urban | 26 (43.3) |
| Rural | 4 (6.7) |
| Both | 30 (50.0) |
| Relationship status at baseline | |
| Currently partnered | 20 (33.3) |
| Currently cohabitated or married | 14 (23.3) |
| Currently married | 13 (21.7) |
| Ever partnered | 8 (13.3) |
| Undefined | 5 (8.3) |
| Analytical method | |
| Generalized estimating equation | 4 (6.7) |
| Multilevel analysis | 4 (6.7) |
| Path analysis/structural equation model | 6 (10.0) |
| Linear regression | 9 (15.0) |
| Binary logistic regression | 22 (36.7) |
| Multinomial logistic regression | 7 (11.7) |
| Ordered regression | 1 (1.7) |
| Poisson regression | 1 (1.7) |
| Probit regression | 1 (1.7) |
| Proportional hazards regression | 1 (1.7) |
| Other | 4 (6.7) |
| Analysis of change | |
| Yes: total | 32 (53.3) |
| Yes: controlled for baseline IPV | 23 (71.9) |
| Yes: analyzed within subject variation (e.g., change scores) | 9 (28.1) |
| No | 28 (46.7) |
| Outcome type | |
| Physical only | 29 (48.3) |
| Sexual only | 1 (1.7) |
| Psychological only | 0 (0.0) |
| Physical or sexual | 13 (21.7) |
| Physical or psychological | 10 (16.7) |
| Physical, sexual, or psychological | 7 (11.7) |
| Outcome reporter | |
| Self-report | 40 (66.7) |
| Couple report | 17 (28.3) |
| Self-report and observation | 1 (1.7) |
| Couple report and observation | 2 (3.3) |
| Outcome measure | |
| Conflict Tactics Scale | 30 (50.0) |
| Inventory of specific behaviors (e.g., pushed or shoved) | 22 (36.7) |
| Other scale (e.g., Severity of Violence Against Women Scale) | 4 (6.7) |
| General items (e.g., experience of “violence” or “assault”) | 4 (6.7) |
Notes. IPV = intimate partner violence. The mean sample size was 3126.2 (SD = 5705.1; median = 634; range = 118–34 653); where relevant, couples are counted as a single unit. The mean length of follow-up was 9.3 years (SD = 8.8; median = 7.0; range = 0.2–40.0). The mean number of time points was 5.7 (SD = 7.9; median = 3.0; range = 2.0–56.0).
Overall, studies scored highly on the quality assessment, largely because of their prospective nature: ranging from 62.5% to 92.4% (mean = 75.5; SD = 7.4; complete scores are in Appendix A, Table 8, available as a supplement to this article at http://www.ajph.org). Common sources of lower scores were poor or inadequately reported participation rates (n = 44) and no analysis of change (n = 28), even when defined liberally as controlling for baseline IPV. Twenty-eight studies did not use random sampling and 19 studies had fewer than 400 participants. Finally, 21 studies used a behavioral inventory to measure IPV with poor or inadequately reported reliability or validity.
Risk and Protective Factors
Seventy-one risk and protective factors were analyzed in the 60 included studies. Most were at the individual (n = 27) or relational level (n = 37); only 7 community-level and no structural-level factors were analyzed. Twenty-eight factors were ineligible for meta-analysis because of clinical heterogeneity among studies (n = 23) or data not being available for transformations to log odds (n = 5). In addition, for 18 factors, only one study provided data appropriate for meta-analysis. All effect estimates, including the operationalization of exposures, and forest plots are in Appendix A.
Meta-analyses showed that few factors were associated with IPV against women with statistical significance (Table 2). Significant protective factors were, at the individual level, being older, and at the community level, living in a disadvantaged neighborhood. At the relational level, being married was protective against women experiencing IPV, but only when we excluded 1 heterogeneous study that examined being married and monogamous compared with single, separated, or married and polygamous42 (Appendix A, Figure 3). At the individual level, experiencing an unplanned pregnancy was a significant risk factor for IPV against women, which remained stable in sensitivity analyses that also included estimates for unwanted pregnancy (Appendix A, Figure 6, available as a supplement to this article at http://www.ajph.org). At the relational level, having parents with less than a high-school education was a risk factor. Sensitivity analysis with a study that instead compared women whose parents had less than a college education to those with more37 showed a nonsignificant pooled association because of heterogeneity (Appendix A, Figure 3).
TABLE 2—
Summary of Meta-Analyses of Prospective-Longitudinal Risk and Protective Factors for Intimate Partner Violence Against Women
| Meta-Analysis |
||||
| Factor | No. Women | No. Studies | OR (95% CI) | I2 (τ2) |
|
Individual level | ||||
| Racial/ethnic identity | ||||
| Black (vs all else) | 30 669 | 8 | 1.15 (0.73, 1.81) | 89.2 (0.38) |
| Latina (vs all else) | 27 137 | 6 | 1.11 (0.73, 1.70) | 80.7 (0.19) |
| White (vs all else) | 3 599 | 2 | 0.72 (0.49, 1.05) | 0.0 (0.00) |
| Women’s education: less than high school | 28 561 | 5 | 1.40 (0.98, 1.99) | 71.1 (0.10) |
| Age (continuous) | 19 623 | 10 | 0.96 (0.93, 0.98) | 68.7 (0.00) |
| Pregnancy status | ||||
| Recent pregnancy | 13 406 | 3 | 0.89 (0.64, 1.24) | 62.1 (0.05) |
| Unwanted pregnancy | 6 874 | 2 | 1.24 (0.91, 1.69) | 0.0 (0.00) |
| Unplanned pregnancy | 3 085 | 2 | 1.66 (1.20, 2.31) | 0.0 (0.00) |
| Youth victimization | 5 572 | 2 | 1.67 (0.59, 4.72) | 81.8 (0.47) |
| Alcohol use | ||||
| Binge drinking (binary) | 4 604 | 3 | 1.20 (0.96, 1.49) | 0.0 (0.00) |
| Greater use (continuous) | 2 633 | 4 | 1.08 (0.91, 1.28) | 67.0 (0.02) |
| Substance use | ||||
| Marijuana use | 4 192 | 3 | 1.23 (0.93, 1.64) | 0.0 (0.00) |
| Other substance use | 4 192 | 3 | 1.43 (0.81, 2.54) | 71.1 (0.18) |
| Experience of child abuse | 1 397 | 4 | 1.30 (0.93, 1.80) | 0.0 (0.00) |
| Antisocial behavior | ||||
| In adolescence | 1 342 | 3 | 1.15 (0.96, 1.37) | 0.0 (0.00) |
| In childhood | 880 | 2 | 1.03 (0.89, 1.19) | 88.1 (0.01) |
| Traditional gender role attitudes | 865 | 2 | 1.16 (0.94, 1.42) | 0.0 (0.00) |
|
Relational level | ||||
| Relationship status | ||||
| Married | 6 410 | 3 | 0.93 (0.87, 0.99) | 0.0 (0.00) |
| Cohabiting | 1 231 | 2 | 1.52 (0.90, 2.55) | 69.1 (0.10) |
| Women’s family structure (single parent) | 3 268 | 4 | 1.57 (0.86, 2.88) | 44.0 (0.16) |
| Women’s higher relationship satisfaction | 2 703 | 3 | 0.79 (0.56, 1.12) | 89.9 (0.09) |
| Positive woman–parent relationship | 2 474 | 2 | 0.96 (0.91, 1.02) | 77.8 (0.00) |
| Women’s parents’ education: less than high school | 2 452 | 3 | 1.55 (1.10, 2.17) | 0.0 (0.00) |
| Greater partner alcohol use | 1 550 | 2 | 1.07 (0.97, 1.17) | 0.0 (0.00) |
| Women’s association with deviant peers | 949 | 2 | 0.86 (0.66, 1.12) | 0.0 (0.00) |
| Women’s family SES (lower) | 813 | 2 | 1.58 (0.78, 3.20) | 0.0 (0.00) |
| Partner’s experience of greater parental monitoring | 365 | 2 | 1.69 (0.65, 4.39) | 76.7 (0.38) |
|
Community level | ||||
| Neighborhood disadvantage | 2 807 | 3 | 0.93 (0.87, 1.00) | 0.0 (0.00) |
| Residential instability | 4 955 | 2 | 0.45 (0.06, 3.33) | 83.7 (1.81) |
| Higher social support | 6 068 | 3 | 0.96 (0.88, 1.04) | 68.9 (0.00) |
Note. CI = confidence interval; OR = odds ratio; SES = socioeconomic status.
Most of our meta-analyses had high heterogeneity or few included studies, which likely contributed to the paucity of statistically significant findings. However, there were several clinically meaningful (based on strength of effect size or confidence interval [CI]), although statistically nonsignificant, associations (Table 2). At the individual level, there was an overall trend between non-White racial/ethnic identity and greater odds of experiencing IPV. However, meta-analyses for Black and Latina identity had substantial heterogeneity, potentially because Huang et al.36 studied a higher-risk sample of unmarried mothers, half of whom were welfare recipients. Nonetheless, women who identified as White had 28% lower odds of experiencing IPV than those who did not (95% CI = 0.49, 1.05). Additional individual-level factors that showed positive but statistically nonsignificant associations were women’s experiences of unwanted pregnancy, binge drinking, marijuana use, experiences of child abuse, and adolescent antisocial behavior. Women with traditional gender role attitudes had higher odds of experiencing IPV, regardless of whether a liberal (OR = 1.11; 95% CI = 1.01, 1.21) or conservative (OR = 1.16; 95% CI = 0.94, 1.42) P value was assumed for the study missing precision estimates,27 although only the former was statistically significant.
At the relational level, factors that showed clinically but not statistically significant risk associations with women’s IPV experiences were cohabiting and partners’ greater alcohol dependence and consumption. There was a statistically nonsignificant, protective association between women’s IPV experiences and positive parent relationships. In addition, each of 2 studies found that women whose partners had experienced less parental monitoring in childhood had significantly greater odds of experiencing IPV in adulthood.40,55 However, the pooled estimate was not statistically significant because of substantial heterogeneity. This may have resulted from measurement differences: Theobald and Farrington measured parental monitoring by child self-report at age 10 only,55 whereas Kerr and Capaldi used both child and parental reports at multiple time points.40 Finally, women who had less than a high-school education had 40% higher odds of experiencing IPV in adulthood (95% CI = 0.98, 1.99). At the community level, there was a statistically nonsignificant, protective association between having more social support and experiencing IPV.
We graphically summarized results for all but 3 of the 71 risk and protective factors, even those not meta-analyzed. The 3 factors too diverse to synthesize were women’s personality characteristics, partners’ personality characteristics, and women’s autonomy. Of these, the following were associated with higher odds of IPV against women: women’s defensiveness51 and partners’ greater problem-solving tendencies, lower withdrawal tendencies, less femininity, and greater impulsivity.26 In addition, in an India-based cohort, women whose financial autonomy remained constant across time and who had constant or improved freedom of movement were at lower risk of experiencing IPV.24
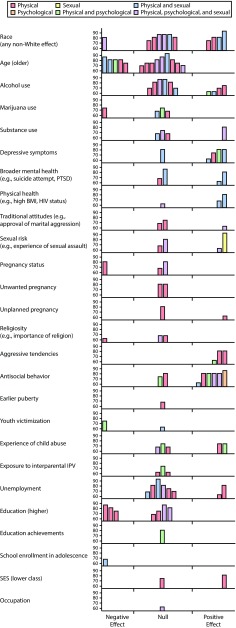
Figure 2 shows the harvest plots for the remaining individual-level factors (for harvest plots for all 68 factors, see Figure A, available as a supplement to this article at http://www.ajph.org). Women’s race, age, alcohol use, and antisocial behavior were the most frequently studied, demonstrating a focus on women’s characteristics in relation to their experiences of IPV as opposed to characteristics of their partners or contexts. Most factors, regardless of ecological level, were studied in 4 or fewer studies: 18 of 26 individual-level factors (69.2%), 28 of 35 relational factors (80.0%), and all 7 community factors (100.0%). For 16 factors, only physical IPV was analyzed as an outcome, including partners’ substance use, women’s life stress, and collective efficacy in women’s communities. Factors not meta-analyzed but that showed evidence for risk associations with IPV across studies (based on effect sizes and interval estimates) were, at the individual level, women’s depressive symptoms and aggressive tendencies and, at the relational level, couples’ lower relationship satisfaction and partners’ identification with non-White races, traditional gender attitudes, antisocial behavior, and unstable employment.
FIGURE 2—
Harvest Plots of Prospective–Longitudinal Risk and Protective Factors for Intimate Partner Violence Against Women at the Individual Level
Note. BMI = body mass index; IPV = intimate partner violence; PTSD = posttraumatic stress disorder; SES = socioeconomic status. Each bar represents an individual study, with the position of the bar indicating whether the findings suggested a negative (risk), null, or positive (protective) effect of the factor on IPV against women. Null (i.e., statistically nonsignificant) results may become statistically significant when pooled together and should not be taken to indicate clinical insignificance. Where necessary, study findings were reinterpreted so that all studies in a single category could be interpreted in the same direction. The height of the bars indicates the quality score limited to the range among included studies (60%–100%). The color of the bar indicates the IPV outcome analyzed in the study. For a harvest plots of all factors at the individual, Relational, community levels, see Figure A (available as a supplement to this article at http://www.ajph.org).
DISCUSSION
To our knowledge, this is the first systematic review of longitudinal evidence for all risk and protective factors for IPV against women. We identified 60 prospective–longitudinal studies that investigated 71 risk and protective factors: 64 were individual or relational-level factors, with only 7 community-level and no structural factors. Most factors were investigated in 4 or fewer, largely US-based studies—illustrating the persisting dearth of prospective evidence in LMICs.
The strongest evidence available for modifiable risk factors for IPV against women was for unplanned pregnancy and parents having less than a high-school education, a plausible proxy for lower socioeconomic status.58 Surprisingly, we found evidence that living in more disadvantaged neighborhoods may be protective; however, this finding could be susceptible to residual confounding or selection bias, with no included study hypothesizing or explaining this relationship.33,34,37 Nevertheless, although the association of neighborhood disadvantage with “public” criminal behaviors (e.g., vandalism) is well-established and theorized (e.g., social disorganization theory), the applicability of these criminological theories to more private forms of violence like IPV is less certain.9,10 This potentially spurious finding highlights the need for further testing of this association prospectively across contexts, with greater attention to the theoretical mechanisms that may link neighborhood disadvantage to IPV, before policy implications are drawn.
Being older or married were also protective against women experiencing IPV. As age and marital status are not amenable to intervention, this informs who should be targeted in preventive efforts—younger women who are single or separated and their partners—rather than which factors should be targeted. Several factors also showed positive but not statistically significant risk associations with IPV and should be further investigated. These include partners’ alcohol use and experiences of low parental monitoring as well as women’s identification as non-White, unwanted pregnancy, binge drinking, marijuana use, experiences of child abuse, antisocial behavior, traditional gender role attitudes, cohabitation with partners, negative parent relationship, low social support, and low education.
This review systematically identified the gaps in the prospective–longitudinal literature on IPV, which ultimately limits the generalizability of these findings. The lack of prospective studies outside the United States means little can be said on contextual differences in the etiology of IPV against women. For instance, parental education may be an important marker for socioeconomic status among women in the United States and other high-income countries,58 but potentially less important in LMICs—a hypothesis that should be tested. The statistically or clinically significant findings in this review indicate priority exposures to measure in future prospective studies of IPV in LMICs and other high-income countries beyond the United States.
In addition to the US bias among the included studies, most of the literature analyzed individual-level risk and protective factors. Twenty-seven factors were related to women’s characteristics or behaviors, whereas only 15 were related to those of their partners. In addition, only 10 studies investigated any community factor. Although this is substantially more than the 3 longitudinal studies identified by previous community-focused systematic reviews,9,10 no community-level factor was investigated outside the United States and most were measured at only 1 time point, limiting conclusions regarding their importance to IPV against women. There were no investigations of structural-level factors, such as alcohol outlet density, societal norms, and gender disparities, despite widespread acknowledgment in public health of the role of social structures in determining outcomes.1 Prospective research on IPV is thus needed that moves beyond women’s characteristics and investigates partner and contextual factors to inform preventive interventions.
Despite the literature’s focus on how women’s characteristics relate to their own victimization, these findings should still not be taken to mean that interventions or the responsibility to change should be targeted to women. The complexity of the risk factors identified and broader socioecological contexts in which they are embedded, including the overall greater social and economic power and status among men compared with women, must be considered when one is designing preventive programs. Although the strongest evidence appeared at the individual and relational levels, the best opportunities to lever change may not be at these levels. Determining the most appropriate intervention strategies requires further qualitative and quantitative appraisals of the nature of each factor and the pathways via which it may causally relate to IPV among women.
An additional gap in the evidence base is the tendency for studies to analyze physical IPV to the exclusion of psychological and sexual IPV. It is consequently unclear how different types of IPV may vary etiologically, which future research should explore. Moreover, most studies began in adulthood and many followed women only until age 30 years or younger; although resource-intensive, more studies are needed that follow women throughout their lifetime to test early life factors and the persistence of the associations identified. Indeed, only 8 of 25 cohorts meta-analyzed (32%) were specifically established to measure women’s intimate relationships or experiences of violence, all of which were based in the United States26,28,33,39,51,52,54,57 except 1 Canadian study.56 This may indicate a lack of funding for these prospective studies that drives the evidence gaps on IPV against women, especially in LMICs.
Finally, the available prospective–longitudinal studies do not allow for issues of reverse causality to be resolved: only 9 measured changes in exposures and outcomes within participants in a repeated-measures design. This means that some included studies did not account for participants’ experiences of IPV before being exposed to risk or protective factors and the hypothesized causal relationships may operate in reverse. For instance, the observed association between unplanned pregnancy and higher odds of IPV could operate causally via feelings of anger and jealousy. Yet sexual IPV and coercive control may directly cause unplanned pregnancy, which has been suggested by cross-sectional studies but analyzed in few, if any, prospective–longitudinal studies.59 Prospective–longitudinal studies that measure first experiences of IPV and changes in violence and exposures over time are thus necessary to clarify our causal understanding of the associations identified in this review.
This review demonstrates that many popular etiological hypotheses for IPV have been understudied prospectively. For instance, few included studies investigated the hypothesis that violence is transmitted across generations and results were inconclusive. We found a statistically nonsignificant, positive relationship between experiencing child abuse and subsequent IPV and little available evidence on exposure to interparental IPV. A recent meta-analysis similarly found only small effects between early domestic violence experiences and subsequent IPV, although this included mainly cross-sectional studies.11 Further limiting conclusions, we identified only US-based studies that prospectively investigated experiencing child abuse or interparental IPV in relation to women’s self-reported victimization. The question thus remains whether these associations exist prospectively and meaningfully across contexts.
Some of this review’s findings differed from those of previous meta-analyses, largely because of our focus on prospective community cohorts and use of modern best practices for meta-analysis. For instance, 1 meta-analysis of women’s alcohol use and subsequent IPV victimization found a significant positive association among 3 studies.7 However, the authors combined categorical46 and continuous54 exposure measures and included a hospital-based study not eligible in the current review. In addition, the authors combined adjusted effect estimates with the unadjusted estimate of Martino et al.,46 which showed a positive association between women’s alcohol use and IPV; whereas we obtained from Martino et al. the adjusted, cross-lagged effect estimate, which was not statistically significant.
Strengths and Limitations
This review had several limitations. First, we only searched and included studies in English, which may have missed some relevant studies. Second, many meta-analyses had high heterogeneity, which we did not have enough statistical power to explore. This is a greater problem when one is meta-analyzing observational studies, which tend to use more diverse methods and adjust for different covariates, as opposed to randomized controlled trials.18 Although we summarized the number of covariates controlled in each study, it was beyond the scope of this review to cover qualitative differences, though we observed no systematic pattern. Longer studies may have been more affected by poor covariate control, given unmeasured time-varying confounders; however, in descriptive checks, we observed no differences in the strength of effect estimates between studies above versus below the median follow-up of 7 years.
Third, by focusing solely on studies in which women self-reported experiencing IPV, we excluded studies that only measured self-reported perpetration of IPV against women. This was necessary to minimize the review’s scope to the most sensitive and rigorous studies15; however, it means that some relevant risk and protective factors may not have been identified. Although there are studies in the field that measure perpetrator characteristics beyond this scope, this review highlights that more prospective–longitudinal studies are needed that measure the characteristics of not just women but their partners as well and include both in measuring IPV against women. This will develop more rigorous evidence for informing preventive interventions that accounts for women’s experiences of IPV but also the critical role of perpetrating partners’ circumstances.
Despite its limitations, to our knowledge, this is the first systematic, meta-analytic review of all risk and protective factors for IPV against women without location, time, or publication restrictions. Accordingly, we retrieved and screened thousands more records than earlier reviews and found more prospective–longitudinal studies than previously identified.5,6,8,12 By only including prospective–longitudinal studies, we located the strongest available evidence for risk and protective factors. We also adopted rigorous methods to ensure maximum but appropriate inclusion of studies in meta-analyses. Finally, by adapting harvest plots, we presented all included evidence, regardless of meta-analysis eligibility, for a novel and complete summary.
Conclusions
Although the burden of IPV against women has been recognized globally, few effective, preventive interventions exist.60 Interventions for improving education and preventing unplanned pregnancies may be beneficial, at least in the United States and other high-income countries. In addition, young and unmarried populations may require targeted interventions. Most conclusively, however, further cross-national, prospective research on the etiological relationships for all types of IPV is needed to inform intervention development worldwide, especially regarding partner and context-related risk and protective factors.
ACKNOWLEDGMENTS
A. R. Yakubovich’s work on this study was supported by The Rhodes Trust and the Canadian Institutes of Health Research (DFS152265). This work was also undertaken with the support of The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UK Clinical Research Collaboration Public Health Research Centre of Excellence. Joint funding (MR/KO232331/1) from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government, and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration is gratefully acknowledged.
The data and analytic procedures used in this study are stored by the first author and may be made available to users upon request.
Note. G. J. Melendez-Torres is on the staff of DECIPHer.
HUMAN PARTICIPANT PROTECTION
Ethical approval by an institutional review board was not required as this study only involved secondary analysis of aggregate data.
Footnotes
See also Allsworth, p. 846.
REFERENCES
- 1.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World Report on Violence and Health. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 2.Garcia-Moreno C, Pallitto C, Devries K, Stockl H, Watts C, Abrahams N, editors. Global and Regional Estimates of Violence Against Women: Prevalence and Health Effects of Intimate Partner Violence and Non-partner Sexual Violence. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 3.Heise LL. Violence against women: an integrated, ecological framework. Violence Against Women. 1998;4(3):262–290. doi: 10.1177/1077801298004003002. [DOI] [PubMed] [Google Scholar]
- 4.Heise L, Fulu E. What works to prevent violence against women and girls? State of the field of violence against women and girls: what do we know and what are the knowledge gaps? London, England: Department for International Development; 2014.
- 5.Stith SM, Smith DB, Penn CE, Ward DB, Tritt D. Intimate partner physical abuse perpetration and victimization risk factors: a meta-analytic review. Aggress Violent Behav. 2004;10(1):65–98. [Google Scholar]
- 6.Mallory AB, Dharnidharka P, Deitz SL et al. A meta-analysis of cross cultural risk markers for intimate partner violence. Aggress Violent Behav. 2016;31:116–126. [Google Scholar]
- 7.Devries KM, Child JC, Bacchus LJ et al. Intimate partner violence victimization and alcohol consumption in women: a systematic review and meta-analysis. Addiction. 2014;109(3):379–391. doi: 10.1111/add.12393. [DOI] [PubMed] [Google Scholar]
- 8.Costa BM, Kaestle CE, Walker A et al. Longitudinal predictors of domestic violence perpetration and victimization: a systematic review. Aggress Violent Behav. 2015;24:261–272. [Google Scholar]
- 9.Vanderende KE, Yount KM, Dynes MM, Sibley LM. Community-level correlates of intimate partner violence against women globally: a systematic review. Soc Sci Med. 2012;75(7):1143–1155. doi: 10.1016/j.socscimed.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 10.Beyer K, Wallis AB, Hamberger LK. Neighborhood environment and intimate partner violence: a systematic review. Trauma Violence Abuse. 2015;16(1):16–47. doi: 10.1177/1524838013515758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith-Marek EN, Cafferky B, Dharnidharka P et al. Effects of childhood experiences of family violence on adult partner violence: a meta-analytic review. J Fam Theory Rev. 2015;7(4):498–519. [Google Scholar]
- 12.Capaldi DM, Knoble NB, Shortt JW, Kim HK. A systematic review of risk factors for intimate partner violence. Partner Abuse. 2012;3(2):231–280. doi: 10.1891/1946-6560.3.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kraemer HC, Kraemer Lowe K, Kupfer DJ. To Your Health: How to Understand What Research Tells Us About Risk. New York, NY: Oxford University Press; 2005. [Google Scholar]
- 14.World Health Organization. Health for the world’s adolescents: a second chance in the second decade. 2015. Available at: http://apps.who.int/adolescent/second-decade. Accessed May 9, 2018.
- 15.Archer J. Assessment of the reliability of the Conflict Tactic Scales: a meta-analytic review. J Interpers Violence. 1999;14(12):1263–1289. [Google Scholar]
- 16.Jolliffe D, Murray J, Farrington D, Vannick C. Testing the Cambridge Quality Checklists on a review of disrupted families and crime. Crim Behav Ment Health. 2012;22(5):303–314. doi: 10.1002/cbm.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 18.Altman DG. Systematic reviews in health care: systematic reviews of evaluations of prognostic variables. BMJ. 2001;323(7306):224–228. doi: 10.1136/bmj.323.7306.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods. 2002;7(1):105–125. doi: 10.1037/1082-989x.7.1.105. [DOI] [PubMed] [Google Scholar]
- 20.Ogilvie D, Fayter D, Petticrew M et al. The harvest plot: a method for synthesising evidence about the differential effects of interventions. BMC Med Res Methodol. 2008;8(1):8. doi: 10.1186/1471-2288-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray J, Farrington DP, Sekol I. Children’s antisocial behavior, mental health, drug use, and educational performance after parental incarceration: a systematic review and meta-analysis. Psychol Bull. 2012;138(2):175–210. doi: 10.1037/a0026407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fisher Z, Tipton E. robumeta: An R-package for robust variance estimation in meta-analysis. arXiv preprint arXiv:150302220. 2015.
- 23.Benson ML, Fox GL, DeMaris A, van Wyk JA. Neighborhood disadvantage, individual economic distress and violence against women in intimate relationships. J Quant Criminol. 2003;19(3):207–235. [Google Scholar]
- 24.Bourey C, Stephenson R, Hindin MJ. Reproduction, functional autonomy and changing experiences of intimate partner violence within marriage in rural India. Int Perspect Sex Reprod Health. 2013;39(4):215–226. doi: 10.1363/3921513. [DOI] [PubMed] [Google Scholar]
- 25.Brown SL, Roebuck Bulanda J. Relationship violence in young adulthood: a comparison of daters, cohabitors, and marrieds. Soc Sci Res. 2008;37(1):73–87. [Google Scholar]
- 26.Caetano R, McGrath C, Ramisetty-Mikler S, Field CA. Drinking, alcohol problems and the five-year recurrence and incidence of male to female and female to male partner violence. Alcohol Clin Exp Res. 2005;29(1):98–106. doi: 10.1097/01.alc.0000150015.84381.63. [DOI] [PubMed] [Google Scholar]
- 27.Chen PH, White HR. Gender differences in adolescent and young adult predictors of later intimate partner violence: a prospective study. Violence Against Women. 2004;10(11):1283–1301. [Google Scholar]
- 28.Cougle JR, Resnick H, Kilpatrick DG. A prospective examination of PTSD symptoms as risk factors for subsequent exposure to potentially traumatic events among women. J Abnorm Psychol. 2009;118(2):405–411. doi: 10.1037/a0015370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Exner-Cortens D, Eckenrode J, Rothman E. Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics. 2013;131(1):71–78. doi: 10.1542/peds.2012-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang X, Corso PS. Child maltreatment, youth violence, and intimate partner violence: developmental relationships. Am J Prev Med. 2007;33(4):281–290. doi: 10.1016/j.amepre.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 31.Fergusson DM, Boden JM, Horwood LJ. Developmental antecedents of interpartner violence in a New Zealand birth cohort. J Fam Violence. 2008;23(8):737–753. [Google Scholar]
- 32.Fergusson DM, Horwood LJ, Kershaw KL, Shannon FT. Factors associated with reports of wife assault in New Zealand. Marriage Fam Living. 1986;48(2):407–412. [Google Scholar]
- 33.Giordano PC, Copp JE, Longmore MA, Manning WD. Anger, control, and intimate partner violence in young adulthood. J Fam Violence. 2016;31(1):1–13. doi: 10.1007/s10896-015-9753-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gomez AM. Testing the cycle of violence hypothesis: child abuse and adolescent dating violence as predictors of intimate partner violence in young adulthood. Youth Soc. 2011;43(1):171–192. [Google Scholar]
- 35.Hahn JW, McCormick MC, Silverman JG, Robinson EB, Koenen KC. Examining the impact of disability status on intimate partner violence victimization in a population sample. J Interpers Violence. 2014;29(17):3063–3085. doi: 10.1177/0886260514534527. [DOI] [PubMed] [Google Scholar]
- 36.Huang C-C, Son E, Wang L-R. Prevalence and factors of domestic violence among unmarried mothers with a young child. Fam Soc. 2010;91(2):171–177. [Google Scholar]
- 37.Jain S, Buka SL, Subramanian SV, Molna BE. Neighborhood predictors of dating violence victimization and perpetration in young adulthood: a multilevel study. Am J Public Health. 2010;100(9):1737–1744. doi: 10.2105/AJPH.2009.169730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jasinski JL. Pregnancy and violence against women. J Interpers Violence. 2001;16(7):712–733. [Google Scholar]
- 39.Kaufman AM. Familial background and relationship-specific correlates of intimate partner violence across the lifecourse. Bowling Green, OH: Dissertation Abstracts International, Bowling Green State University; 2015.
- 40.Kerr DC, Capaldi DM. Young men’s intimate partner violence and relationship functioning: long-term outcomes associated with suicide attempt and aggression in adolescence. Psychol Med. 2011;41(4):759–769. doi: 10.1017/S0033291710001182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim HK, Laurent HK, Capaldi DM, Feingold A. Men’s aggression toward women: a 10-year panel study. Marriage Fam Living. 2008;70(5):1169–1187. doi: 10.1111/j.1741-3737.2008.00558.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kouyoumdjian FG, Calzavara LM, Bondy SJ et al. Risk factors for intimate partner violence in women in the Rakai Community Cohort Study, Uganda, from 2000 to 2009. BMC Public Health. 2013;13:566. doi: 10.1186/1471-2458-13-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koziol-McLain J, Coates CJ, Lowenstein SR. Predictive validity of a screen for partner violence against women. Am J Prev Med. 2001;21(2):93–100. doi: 10.1016/s0749-3797(01)00325-7. [DOI] [PubMed] [Google Scholar]
- 44.Lansford JE, Miller-Johnson S, Berlin LJ, Dodge KA, Bates JE, Pettit GS. Early physical abuse and later violent delinquency: a prospective longitudinal study. Child Maltreat. 2007;12(3):233–245. doi: 10.1177/1077559507301841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lehrer JA, Buka S, Gortmaker S, Shrier LA. Depressive symptomatology as a predictor of exposure to intimate partner violence among US female adolescents and young adults. Arch Pediatr Adolesc Med. 2006;160(3):270–276. doi: 10.1001/archpedi.160.3.270. [DOI] [PubMed] [Google Scholar]
- 46.Martino SC, Collins RL, Ellickson PL. Cross-lagged relationships between substance use and intimate partner violence among a sample of young adult women. J Stud Alcohol. 2005;66(1):139–148. doi: 10.15288/jsa.2005.66.139. [DOI] [PubMed] [Google Scholar]
- 47.McLeod GFH, Fergusson DM, John Horwood L. Childhood physical punishment or maltreatment and partnership outcomes at age 30. Am J Orthopsychiatry. 2014;84(3):307–315. doi: 10.1037/h0099807. [DOI] [PubMed] [Google Scholar]
- 48.Menard S, Weiss AJ, Franzese RJ, Covey HC. Types of adolescent exposure to violence as predictors of adult intimate partner violence. Child Abuse Negl. 2014;38(4):627–639. doi: 10.1016/j.chiabu.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 49.Nowotny KM, Graves JL. Substance use and intimate partner violence victimization among White, African American, and Latina women. J Interpers Violence. 2013;28(17):3301–3318. doi: 10.1177/0886260513496903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Donnell L, Agronick G, Duran R, Myint UA, Stueve A. Intimate partner violence among economically disadvantaged young adult women: associations with adolescent risk-taking and pregnancy experiences. Perspect Sex Reprod Health. 2009;41(2):84–91. doi: 10.1363/4108409. [DOI] [PubMed] [Google Scholar]
- 51.O’Leary KD, Malone J, Tyree A. Physical aggression in early marriage: prerelationship and relationship effects. J Consult Clin Psychol. 1994;62(3):594–602. doi: 10.1037//0022-006x.62.3.594. [DOI] [PubMed] [Google Scholar]
- 52.Quigley BM, Leonard KE. Alcohol and the continuation of early marital aggression. Alcohol Clin Exp Res. 2000;24(7):1003–1010. [PubMed] [Google Scholar]
- 53.Staggs SL, Long SM, Mason GE, Krishnan S, Riger S. Intimate partner violence, social support, and employment in the post-welfare reform era. J Interpers Violence. 2007;22(3):345–367. doi: 10.1177/0886260506295388. [DOI] [PubMed] [Google Scholar]
- 54.Testa M, Livingston JA, Leonard KE. Women’s substance use and experiences of intimate partner violence: a longitudinal investigation among a community sample. Addict Behav. 2003;28(9):1649–1664. doi: 10.1016/j.addbeh.2003.08.040. [DOI] [PubMed] [Google Scholar]
- 55.Theobald D, Farrington DP. Child and adolescent predictors of male intimate partner violence. J Child Psychol Psychiatry. 2012;53(12):1242–1249. doi: 10.1111/j.1469-7610.2012.02577.x. [DOI] [PubMed] [Google Scholar]
- 56.Vézina J, Hebert M, Poulin F, Lavoie F, Vitaro F, Tremblay RE. History of family violence, childhood behavior problems, and adolescent high-risk behaviors as predictors of girls’ repeated patterns of dating victimization. Violence Against Women. 2015;21(4):435–459. doi: 10.1177/1077801215570481. [DOI] [PubMed] [Google Scholar]
- 57.Widom CS, Czaja S, Dutton MA. Child abuse and neglect and intimate partner violence victimization and perpetration: a prospective investigation. Child Abuse Negl. 2014;38(4):650–663. doi: 10.1016/j.chiabu.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Erola J, Jalonen S, Lehti H. Parental education, class and income over early life course and children’s achievement. Res Soc Stratification Mobility. 2016;44:33–43. [Google Scholar]
- 59.Abajobir AA, Alati R, Kisely S, Najman JM. Antecedents and maternal health outcomes of unintended pregnancy: a systematic review. Ethiop Med J. 2017;55(4):325–354. [Google Scholar]
- 60.Ellsberg M, Arango DJ, Morton M et al. Prevention of violence against women and girls: what does the evidence say? Lancet. 2015;385(9977):1555–1566. doi: 10.1016/S0140-6736(14)61703-7. [DOI] [PubMed] [Google Scholar]