Abstract
New data reveal significant variation in economic mobility outcomes across U.S. localities. This suggests that social structures, institutions, and public policies—particularly those that influence critical early-life environments—play an important role in shaping mobility processes. Using new county-level estimates of intergenerational economic mobility for children born between 1980 and 1986, we exploit the uneven expansions of Medicaid eligibility across states to isolate the causal effect of this specific policy change on mobility outcomes. Instrumental-variable regression models reveal that increasing the proportion of low-income pregnant women eligible for Medicaid improved the mobility outcomes of their children in adulthood. We find no evidence that Medicaid coverage in later childhood years influences mobility outcomes. This study has implications for the normative evaluation of this policy intervention as well as our understanding of mobility processes in an era of rising inequality.
Keywords: economic mobility, health insurance, inequality, public policy
New estimates of intergenerational economic mobility reveal substantial subnational variation in the degree of economic mobility across U.S. localities (Chetty et al. 2014). These estimates, based on linked administrative tax records for virtually every child born between 1980 and 1993 and their parents, demonstrate that the likelihood a child in the poorest income quintile moves to the richest income quintile in adulthood is strongly conditioned by where he or she grows up. Evidence from families that moved across localities further demonstrates that the local context a child is exposed to early in life has a direct, measureable effect on later-life outcomes, including earnings, college attendance, fertility, and marriage (Chetty and Hendren 2016).
What explains this variation in observed rates of intergenerational economic mobility? In their groundbreaking study, Chetty et al. (2014; hereafter “CHKS”) examine a range of demographic, institutional, and policy correlates of economic mobility across U.S. localities, including government spending, tax policy, and school quality. Notably, variation in population health and health policy were omitted from this analysis, which is surprising given the large and growing literature detailing the central role of health status in shaping economic outcomes both within and between generations (Haas 2006; Haas, Glymour, and Berkman 2011; Kane 2015).
In this paper we argue that health is a key pathway for the transmission of economic status from parents to children and, consequently, that variation in health policy context can help us understand why the economic-mobility outcomes of children vary across localities and between adjacent birth cohorts. We do this by testing whether variation in one targeted health policy intervention—Medicaid public health insurance coverage for low-income pregnant women and their children—has a measurable impact on the economic-mobility outcomes of those children when measured in adulthood. Put another way, we seek to test whether variation in Medicaid eligibility policy across states and over time explains some of the observed variation in the place-based, cohort-specific economic-mobility estimates generated by CHKS.
Previous studies employing rigorous identification strategies and individual-level data consistently find that early-life Medicaid coverage leads to absolute long-run improvements in health, educational attainment, and wages (Black, Devereux, and Salvanes 2007; Cohodes et al. 2014; Levine and Schanzenbach 2009; Miller and Wherry 2017; Smith 2009). Yet demonstrating that a policy intervention improves outcomes for affected individuals does not directly imply that it has an effect on economic-mobility parameters estimated at the population level. For one, the effect of the policy intervention—particularly one targeted to a subset of the population—may be too small to influence the overall level of mobility; expanding early-life Medicaid coverage may improve education and labor market outcomes for kids on the margin without notably impacting the population-level correlation between the income percentile ranks of parents and their children in adulthood. Moreover, the effect of expanding Medicaid coverage to low-income children may be offset by simultaneous shifts in policies or institutional arrangements that benefit children from middle- or upper-income families, resulting in an absolute improvement for all but no net change in relative ranking. At the same time, targeted policy interventions, like Medicaid, can have positive “spillover” effects for individuals not directly impacted by the program—this, too, motivates analyzing the effect of public policies on mobility parameters estimated on the population as whole.
Therefore, in this paper we ask, does state–year variation in early-life Medicaid coverage predict county-by-birth-cohort variation in intergenerational economic mobility? The county-level economic-mobility estimates generated by CHKS are based on cohorts born in the 1980s, a period during which Medicaid eligibility expanded dramatically and unevenly across states as a result of policy changes at the federal and state levels. We exploit this variation to examine whether state–year variation in Medicaid eligibility policy predicts county-by-birth-cohort estimates of intergenerational economic mobility. To identify the causal effect of Medicaid policy on economic mobility, we employ a simulated measure of Medicaid coverage developed by Currie and Gruber (1996) and Cutler and Gruber (1996) (see also Cohodes et al. 2014; Miller and Wherry 2017) that isolates variation in Medicaid coverage driven by real changes in policy and not due to changes in underlying state demographics.
We find that early-life Medicaid coverage across states and over time has a direct, measureable effect on the observed economic-mobility levels of these birth cohorts as measured in adulthood. Our results indicate that county–birth cohorts exposed to higher levels of Medicaid eligibility in utero and during the first year of life experienced greater levels of economic mobility, operationalized as a reduction in the correlation between the income percentile ranks of parents and their children in adulthood. Notably, we find no effect of Medicaid coverage after infancy on economic-mobility levels, suggesting that coverage extensions to children after infancy had no discernable effect on mobility outcomes. Robustness checks demonstrate that the observed relationship between early-life Medicaid coverage and intergenerational economic mobility cannot be accounted for by simultaneous policy shifts at the state or local level.
Economic mobility, the definition of the “American dream,” is a salient and potent construct in American political discourse; identifying which policies successfully increase the level of economic mobility in American society has important implications for our normative evaluation of these interventions. In demonstrating a causal link between Medicaid and intergenerational economic mobility, this study simultaneously highlights the role of health policy context in explaining spatial and temporal variation in mobility levels and underscores how targeted early-life policy interventions can serve to reduce the determinative power of parents' economic position on their child's future economic position. In so doing, this article offers one of the first causal explanations for the observed variation in rates of economic mobility for these cohorts across U.S. localities and has direct implications for ongoing policy debates regarding the size and reach of the Medicaid program and other interventions targeted at improving early-life environments.
Background
Health as a Determinant of Intergenerational Economic Mobility
Health, at the level of both individuals and populations, is a key pathway for the transmission of economic status across generations. Research consistently demonstrates that health status early in life—from the fetal period to infancy to early childhood—has an independent effect on later-life health, educational attainment, and labor market outcomes, which are key determinants of intergenerational economic mobility (Haas 2006; Haas et al. 2011; Smith 2009).
Birth weight—an important measure of health endowment at birth—offers perhaps the clearest illustration of how health can serve to reproduce social inequalities across generations (Kane 2015; Palloni 2006). The incidence of low-weight births, typically defined as less than 2,500 grams, is socially patterned; babies born to low-income and minority mothers are significantly more likely to be underweight than babies born to higher-income parents (Aizer and Currie 2014). Maternal health, exposure to pollution, lack of medical care, poor health behaviors, and greater exposure to sources of stress, such as domestic violence, have all been linked to higher incidence of low-weight births (Aizer 2011; Aizer and Currie 2014; Currie 2009; see also Scharber 2014). Yet beyond individual determinants, birth weight is also strongly conditioned by social and policy context. For example, Walton (2009) found that higher levels of residential segregation are associated with an increased risk of low birth weight for babies born to African American mothers, and Strully, Rehkopf, and Xuan (2010) demonstrated that targeted cash transfers in the form of state-level earned income tax credits (EITCs) reduce the incidence of low-weight births.
In addition to these temporally proximate determinants, recent work by Kane (2015) demonstrated that birth weight is shaped by forces at work long before conception. In a multigenerational analysis using data from the National Longitudinal Survey of Youth 1979 cohort and their children, Kane found that a mother's own early-life conditions impact the likelihood her child will be born underweight. Kane's theoretical model emphasizes health as a key pathway for the transmission of economic status across generations and underscores how disparities in health endowment at birth can serve to perpetuate social and economic inequalities within and between groups.
Infant birth weight has been shown to influence cognitive functioning and school achievement on a variety of measures, including educational attainment and child test scores, even among siblings raised in the same family and social context (Bharadwaj, Eberhard, and Neilson 2018; Black et al. 2007; Conley, Strully, and Bennett 2003; Currie 2009; Figlio et al. 2013; Oreopoulos et al. 2008). In one recent study using merged birth and school administrative records for Florida children born in the 1990s, Figlio et al. (2013) found that low birth weight is associated with lower test scores, a gap that persists over time and is largely unaffected by school quality. Studies using sibling and twin pairs to isolate the unique effect of infant birth weight on life outcomes have found that the impact of low birth weight extends past school age to the labor market, resulting in lower wages, greater reliance on disability programs, and an increased probability of living in a low-income area in adulthood (Black et al. 2007; Oreopoulos et al. 2008).
Beyond infant health, parental socioeconomic status (SES) impacts health status throughout childhood and adolescence on a wide range of measures, from growth stunting to asthma to obesity (Brooks-Gunn and Duncan 1997; Currie 2009; Currie and Lin 2007). Children who grow up in poverty are at greater risk of a range of negative health-related outcomes, from behavioral disorders to chronic disease to premature death (Currie 2009). And, as Case, Lubotsky, and Paxson (2002) demonstrated, the negative health effects of growing up in a poor family accumulate over time. Poor children have less access to healthcare and lower vaccination rates (Klevens and Luman 2001), indicating that expanding access to health insurance could serve to reduce the degree to which economic and health inequalities are mutually reinforcing.
Poor childhood health is associated with lower cognitive and verbal ability in school and the gap in language and cognitive ability between children of high- and low-SES parents (Salm and Schunk 2008). This disadvantage compounds over time, with childhood health having direct implications for later-life educational achievement and labor market outcomes (see, e.g., Smith 2007, 2009). In one recent analysis using data from the Health and Retirement Study, Haas and colleagues (2011) found that adults who report poor health in childhood earn substantially less during prime working years. The authors demonstrate that poor childhood health reduces lifetime earnings through multiple pathways, including lower educational attainment, reduced labor force participation, and higher disease burden in adulthood.
These studies document the long-term consequences of SES on infant and child health and the subsequent effects of child health on educational and labor market outcomes, illustrating the central role of health in mobility processes. They suggest that health policy interventions targeted at improving the health status of low-income children early in life may serve to increase economic mobility by mitigating a key pathway for the transmission of economic disadvantage across generations.
Impact of Early-life Medicaid Coverage: Existing Research
Existing research documents the short- and long-run effects of Medicaid coverage on individual health, educational attainment, and labor market outcomes. The seminal work of Currie and Gruber (1996) demonstrated that expanding Medicaid to low-income pregnant women increased health insurance coverage and reduced infant mortality. Currie (1995) further found that expanding public health insurance coverage for low-income children reduced inequalities in healthcare utilization and health outcomes for children. Lurie (2009) also found that Medicaid coverage increased doctor visits, and Joyce and Racine (2005) found a positive effect of coverage on vaccination rates. More recent work by Miller and Wherry (2017) found that early-life exposure to Medicaid had lasting consequences for health in adulthood, specifically in reducing obesity, diabetes, and some types of hospitalizations.
Beyond health and healthcare utilization, there is a large and growing body of evidence linking early-life Medicaid coverage to improved educational outcomes. Levine and Schanzenbach (2009) found that Medicaid expansions increased children's reading test scores. Cohodes et al. (2014) found that early-life Medicaid coverage improved the high school completion, college attendance, and college completion rates of low-income children. Using Internal Revenue Service administrative data, Brown, Kowalski, and Lurie (2015) found significant impacts of early-life Medicaid exposure on individual labor market outcomes. Specifically, they found that children affected by expanding Medicaid coverage in the 1980s and 1990s were more likely to attend college, collected less in EITC payments, and paid more in cumulative taxes by age 28. They further found a positive effect of early-life Medicaid coverage on wages but only for women (see, however, Boudreaux, Golberstein, and McAlpine 2016).
Given this large and growing body of work documenting the long-run positive effects of expanding public health insurance coverage on individual human capital attainment and labor market performance, we might expect state–year variation in Medicaid eligibility policy to have a measureable impact on population-based estimates of economic mobility. In the next sections, we describe the data used to test this hypothesis.
Data and Methods
Place-based Estimates of Intergenerational Economic Mobility
CHKS generated estimates of intergenerational economic mobility using federal tax records for nearly the total population of 40 million children born between 1980 and 1993 and their parents. CHKS used these data to estimate economic mobility through a multistage process. First, they ranked children within each birth year cohort based on income in adulthood at age 26. They next ranked the parents of these children relative to each other, based on mean family income when the children were young adolescents. The authors then generated an estimate of mobility by comparing the birth cohort–specific income percentile rank of children in adulthood to that of their parents' years earlier; the slope of this rank–rank relationship is the correlation between the child's and parents' positions in the income distribution. CHKS referred to this measure as relative economic mobility. CHKS found that the relationship between mean child income ranks and mean parent income ranks is linear across U.S. localities. Therefore, the overall level of economic mobility for a given county–birth cohort is captured in two key parameters: (1) the slope, which again is the correlation between the income ranks of parents and children, and (2) the intercept, which is the expected mean rank of children at the bottom of the income distribution (i.e., born to families at the zero percentile of income).
In the analyses that follow, we estimated the effect of early-life Medicaid coverage on these two economic mobility parameters. Following CHKS, we also used the slope and intercept to calculate a measure of absolute upward mobility, which is the conditional expectation of a child's rank in adulthood given his or her parents' income rank. Absolute upward mobility provides a more intuitive measure of the prospects of children from each percentile in adulthood and is an important complement to our understanding of relative mobility. We used the slope and intercept to generate measures of absolute upward mobility at given points in the income distribution. Multiplying the rank– rank slope by the specific income percentile in the distribution we wished to examine (10th percentile, 50th percentile, 90th percentile) and adding the county- and birth cohort–specific intercept yielded the county–birth cohort–specific mean income rank of children born to parents at that point in the distribution.
Given the availability of near population-level data, CHKS were able to generate mobility parameters for children in birth year cohorts across U.S. localities. The analyses presented below used mobility estimates generated by Chetty et al. (2014) from a modified sample of “stayers”— parents and children who remained in the same county until the child was 18. These mobility estimates were generated for every birth cohort from 1980 to 1986 for more than 1,400 counties. An alternative measure of intergenerational mobility for all residents (stayers and movers) was estimated for each birth cohort at the commuting-zone level—clusters of counties oriented around a principal city. As commuting zones cross state lines and Medicaid policy is set at the state level, using commuting zones would add noise to our estimates. We therefore used the county-level estimates generated by CHKS from their modified stayers sample in the analyses that follow; we note that our results are substantively robust to the use of commuting zones as well as to generating state-level mobility rates from these county-level estimates.
Medicaid Expansions: 1980s and 1990s
Medicaid eligibility for low-income pregnant women and children expanded dramatically in the 1980s and 1990s (for an overview, see Currie and Gruber 1996; Miller and Wherry 2017). Prior to 1980, Medicaid eligibility was tied closely to eligibility rules governing Aid to Families with Dependent Children (AFDC) cash welfare; as states set eligibility thresholds for AFDC, there was significant cross-state variation in who qualified for Medicaid. Notably, however, prior to 1980, virtually every state had an income limit for AFDC eligibility that was below the federal poverty line—often below 50% of the federal poverty line. Throughout the 1980s, Congress expanded Medicaid coverage for low-income pregnant women and their newborn children in an effort to reduce infant mortality and improve infant health. Initial expansions of the program came from federal mandates that states provide coverage to any pregnant woman meeting eligibility requirements for AFDC, regardless of their participation in the program, as well as their infant children. Later expansions mandated that states provide coverage to pregnant women and infants in households with incomes up to 133% of the federal poverty line and gave states the option to expand coverage further still, up to 185% of the federal poverty line.
These policy changes—at both the federal and state levels—yielded a substantial and significant expansion in Medicaid eligibility for pregnant women and infants over the 1980s and 1990s. However, the degree of variation in the percentage of pregnant women eligible for coverage across states and over time can be attributed to changes in eligibility rules, shifts in underlying state demographics, and the interaction between the two. For example, states with relatively low income cutoffs for AFDC—and thereby Medicaid coverage— before the expansions saw larger increases in the percentage of women eligible than states that covered a greater percentage of women from the start. Therefore, variation within states over time is a function of not only state and federal policy shifts but also changes in the socioeconomic composition of the state. Even absent a change in eligibility policy, increasing the percentage of women in poverty will increase the percentage of pregnant women eligible for Medicaid.
In order to isolate the unique effect of Medicaid policy shifts on eligibility net of shifts in state sociodemographics, the analyses presented below employed a simulated measure of state Medicaid eligibility constructed by Miller and Wherry (2017). First employed by Currie and Gruber (1996) and Cutler and Gruber (1996), this measure was generated by applying state–year-specific Medicaid eligibility rules to a nationally representative sample of women ages 15 to 44 drawn from the Current Population Survey. Using a national sample to generate state–year-specific estimates of the fraction of women who would be eligible for coverage if they became pregnant produces an estimate of “simulated eligibility” that is unaffected by any changes in state demographic or economic characteristics that may influence coverage level over and above changes in actual Medicaid policy (see Miller and Wherry 2017). Following Currie and Gruber (1996) and later studies (e.g., Cohodes et al. 2014), we instrumented for state-level changes in Medicaid eligibility with this measure of simulated eligibility.
Tables A1 and A2 in the appendix display the real and simulated percentages of women ages 15 to 44 who would be eligible for Medicaid coverage if they became pregnant, by state for selected years, as well as the percentage change over this time period. Note that in states with relatively low poverty rates during this time period (e.g., Massachusetts), simulated eligibility is higher than real eligibility, whereas in states with relatively high poverty rates during this time period (e.g., Texas), simulated eligibility is lower than real eligibility. This illustrates that the simulated measure is capturing only variation in eligibility policy and not differences in state sociodemographics.
To examine the effect of increased Medicaid coverage across an individual's childhood, we also employed a state–year measure of Medicaid eligibility coverage for each cohort from ages 1 to 18. This measure was generated by calculating the fraction of children eligible for Medicaid coverage at each age, given a specific birth year and state. The fraction of children eligible was then summed at each age across state and birth cohort, which yielded a measure representing the cumulative average years of public eligibility during childhood. As shifting demographic factors and economic conditions may also influence eligibility across childhood, Miller and Wherry (2017) also constructed a simulated measure of childhood eligibility. The simulated measure of childhood Medicaid eligibility was constructed using a similar method to simulated prenatal eligibility: a nationally representative draw of 1,000 children of a specific age was taken from the American Community Survey, and then the state–year- specific eligibility criteria were applied to this simulated cohort. Then, the fraction of children eligible at each year was summed to generate a simulated measure of cumulative eligibility across childhood.
In the analyses presented below, we used both actual and simulated Medicaid eligibility measures in models estimating the relationship between early-life Medicaid coverage and county–birth cohort observed levels of intergenerational economic mobility.
Analytic Strategy
To estimate the effect of Medicaid coverage on intergenerational economic mobility, we matched the birth cohort–specific county-level mobility estimates to the state-level estimates of Medicaid coverage (both real and simulated) in the same year. Given a gestational period of approximately 40 weeks, matching on birth year is an imperfect measure of coverage: for children born later in the calendar year, this measure captured the entire prenatal period, whereas for children born earlier in the calendar year, this measure captured coverage levels for more of the first year of life. However, given that Medicaid coverage was typically simultaneously extended to pregnant women and their infant children until age 1, in utero coverage and coverage in infancy were highly correlated. We explore the sensitivity of our findings to alternative lag structures in our Robustness Checks section.
To analyze the effect of Medicaid coverage on intergenerational economic mobility, we estimated
where Ycst is the measure of economic mobility at age 26 of children born in year t and county c within state s. Xst is a vector of time-varying state-level covariates: percentage of the population with at least a high school degree, percentage black, percentage Hispanic, percentage single-parent house-holds, percentage below the poverty line, percentage unemployed, and log-transformed total income in the state. These covariates were taken from the Current Population Survey (IPUMS). We additionally included a measure of total state and local non-health spending to net out potential confounding due to simultaneous policy shifts at the state or local level. All models included county fixed effects (αc) to net out all time-invariant characteristics of the county (and state) as well as year fixed effects (γt) to net out trends that affected all counties equally. Standard errors were clustered at the state level to account for correlations between counties within states.
For each outcome we present estimates from three different model specifications: ordinary least squares (OLS) estimates using actual Medicaid eligibility coverage, reduced form estimates using our simulated measure of Medicaid coverage, and two-stage least squares (2SLS) instrumental variable (IV) estimates using simulated coverage to instrument for actual coverage. For the 2SLS model specification, the first stage takes the form
where the simulated eligibility coverage at the state level predicts real eligibility coverage.
We first examined the effect of Medicaid coverage on the two population economic-mobility parameters estimated by CHKS—the rank–rank slope and intercept—and then analyzed absolute upward-mobility outcomes at different points in the income distribution.
Results
Table 1 presents estimates of the effect of Medicaid coverage—operationalized as the fraction of women ages 15 to 44 who would be eligible for Medicaid in the event of a pregnancy—on the county-level rank–rank slope (Models 1 to 3) and intercept (Models 4 to 6), the two mobility parameters generated by CHKS. The estimated coefficient in Model 1—using actual Medicaid coverage levels to predict the county–birth cohort's estimated rank–rank slope—is negative but is not statistically significant. Model 2 substitutes our simulated measure of Medicaid eligibility, which isolates the direct effect of changes in Medicaid eligibility policy on coverage levels, netting out variation in coverage due to shifts in underlying demographics. The estimated coefficient on the simulated measure of Medicaid eligibility is both larger and statistically significant.
Table 1.
Medicaid Coverage in Birth Year and Intergenerational Economic Mobility; County–Birth Cohort Mobility Rank–Rank Slope and Intercept.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
| OLS | Reduced Form | 2SLS | OLS | Reduced Form | 2SLS | |
|
|
|
|
|
|
|
|
| Variable | Rank–Rank Slope | Rank–Rank Slope | Rank–Rank Slope | Intercept | Intercept | Intercept |
| Medicaid coverage (real) | −.033 (.037) | .047* (.023) | ||||
| Medicaid coverage (simulated) | −.101* (.046) | −.100* (.045) | .081* (.038) | .081* (.038) | ||
| First-stage F statistic F(1, 49) | 211.98*** | 211.98*** | ||||
| County–year observations | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 |
| R2 | .014 | .015 | .012 | .025 | .026 | .025 |
Note: OLS = ordinary least squares; 2SLS = two-stage least squares. Robust standard errors in parentheses; standard errors clustered at the state level. All models include state fixed effects, year fixed effects, and a vector of state-level, time-varying covariates. Medicaid coverage refers to percentage of women ages 15 to 44 who would be eligible for Medicaid coverage if pregnant.
p < .10,
p < .05,
p < .01,
p < .001 (two-tailed tests).
Model 3 presents results from the 2SLS where we use the simulated measure of Medicaid coverage to instrument for actual Medicaid coverage. The first-stage F statistic on excluded instruments is over 200, indicating that the instrument is robust and subject to minimal bias. The point estimate indicates that a 10–percentage point increase in Medicaid coverage is associated with a 1-point decrease in the correlation between the income ranks of parents and children; this indicates that state variation in Medicaid coverage levels for cohorts in utero and during the first year of life had a direct, demonstrable impact on the economic-mobility outcomes of those cohorts as measured in adulthood.
Models 4 through 6 present estimates from models analyzing the impact of Medicaid coverage on the county-level intercept. Across all three model specifications we see a positive relationship between Medicaid coverage and the county-level intercept estimated by CHKS. To more readily interpret the effect of Medicaid coverage on mobility outcomes, Table 2 presents estimates from models predicting absolute economic mobility, operationalized as the expected mean income rank in adulthood of children born to parents at a given point in the income distribution. These mobility estimates were calculated using the county-level slope and intercept analyzed above. Here again we present estimated coefficients from three model specifications to examine the effect of Medicaid coverage on the absolute mobility outcomes of children born to parents at the 10th percentile of the national income distribution (Models 1 to 3), the 50th percentile (Models 4 to 6), and 90th percentile (Models 7 to 9).
Table 2.
Medicaid Coverage in Birth Year and Intergenerational Economic Mobility: Expected Income Rank of Children Born at 10th, 50th, and 90th Income Percentiles.
| (1) | (2) | (3) | (4) | (S) | (6) | (7) | (8) | (9) | |
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
| OLS | Reduced Form | 2SLS | OLS | Reduced Form | 2SLS | OLS | Reduced Form | 2SLS | |
|
|
|
|
|
|
|
|
|
|
|
| Variable | 10th Percentile | 10th Percentile | 10th Percentile | 50th Percentile | 50th Percentile | 50th Percentile | 90th Percentile | 90th Percentile | 90th Percentile |
| Medicaid coverage (real) | .044* (.020) | .030† (.016) | .017 (.023) | ||||||
| Medicaid coverage (simulated) | .071* (.035) | .071* (.035) | .031 (.030) | .031 (.030) | −.009 (.035) | −.009 (.034) | |||
| First-stage F statistic F(1, 49) | 21 1.98*** | 21 1.98*** | 21 1.98*** | ||||||
| County-year observations | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 |
| R2 | .030 | .031 | .029 | .058 | .057 | .058 | .029 | .029 | .029 |
Note: OLS = ordinary least squares; 2SLS = two-stage least squares. Robust standard errors in parentheses; standard errors clustered at the state level. All models include state fixed effects, year fixed effects, and a vector of state-level, time-varying covariates. Medicaid coverage refers to percentage of women ages 15 to 44 who would be eligible for Medicaid coverage if pregnant.
p < . 10,
p < .05,
p < .01,
p < .001 (two-tailed tests).
Turning first to the estimated effect of Medicaid coverage on the absolute mobility outcomes of children from low-income families, we see a positive and statistically significant coefficient across all three model specifications. Estimates from the preferred IV model specification indicates a 10–percentage point increase in Medicaid Coverage is associated with .7-point higher expected mean income rank in adulthood. A .7-point increase over the expected mean rank of children born to parents at the 10th percentile translates to approximately $500 higher yearly income in adulthood. Notably, we see no effect of Medicaid coverage on the absolute mobility outcomes of children born to parents at the 50th percentile of the national income distribution (Models 4 to 6) or to children born to parents at the 90th percentile.
Taken together, these estimates reveal that expanding Medicaid coverage to low-income pregnant women and their infant children improved the mobility outcomes of those children as measured in adulthood. This indicates that health policy context very early in life—in utero and during the first year—has direct implications for the mobility outcomes of those children measured decades later. But what about Medicaid coverage levels after infancy? Does variation in Medicaid coverage during childhood years (ages 1 to 18) have a measureable impact on a county–birth cohort's observed economic mobility outcomes?
Table 3 reproduces the main models presented in Table 1, now including a measure of Medicaid eligibility during childhood. Across all three model specifications, we see no effect of increased Medicaid eligibility in childhood on either of the county–birth cohort mobility parameters. These models suggest that while state Medicaid coverage levels in utero and in infancy influence county– cohort economic-mobility outcomes, expansions of coverage in later childhood have no measurable impact on observed mobility levels. This finding runs in line with Miller and Wherry (2017), who also find strong evidence for early-life coverage and no evidence of positive effects for coverage extended in childhood, and runs counter to Cohodes et al. (2014) and Brown et al. (2015), who find significant long-run positive effects of coverage gained in later childhood.
Table 3.
Medicaid Coverage in Birth Year and Exposure in Childhood on County–Birth Cohort Mobility Rank–Rank Slope and Intercept.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
| OLS | Reduced Form | 2SLS | OLS | Reduced Form | 2SLS | |
|
|
|
|
|
|
|
|
| Variable | Rank–Rank Slope | Rank–Rank Slope | Rank–Rank Slope | Intercept | Intercept | Intercept |
| Medicaid coverage: pregnant women (real) | −.031 (.037) | .043† (.022) | ||||
| Medicaid coverage: childhood (real) | −.142 (.218) | .259† (.155) | ||||
| Medicaid coverage: pregnant women (simulated) | −.102* (.043) | −.099* (.044) | .082* (.034) | .080* (.035) | ||
| Medicaid coverage: childhood (simulated) | −.518 (.456) | −.573 (.536) | .525 (.412) | .579 (.477) | ||
| First-stage F statistic F(2, 49) | 107.17*** | 107.17*** | ||||
| County–year observations | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 | 9,429 |
| R2 | .014 | .015 | .011 | .027 | .028 | .023 |
Note: OLS = ordinary least squares; 2SLS = two-stage least squares. Robust standard errors in parentheses; standard errors clustered at the state level. All models include state fixed effects, year fixed effects, and a vector of state-level, time-varying covariates.
p < .10,
p < .05,
p < .01,
p < .001 (two-tailed tests).
Robustness Checks
Employing an IV strategy allowed us to isolate the direct effect of changing Medicaid eligibility policy on economic mobility, net of shifts in state economic conditions and sociodemographics. Yet, it could be argued that simultaneous trends or policy shifts occurring during this same time period may be confounding our analyses. We attempted to account for this in our main models by including a measure of total state and local nongovernment spending; however, this covariate may have been too coarse to pick up policy shifts that are not captured in aggregate spending data. To account for potential co-occurring policy changes at the state and local level, we conducted several additional robustness checks. We first tested the sensitivity of our estimates to different measures of state and local government spending, including total direct spending and total intergovernmental spending; these alternative operationalizations had no effect on the size or significance of our estimates. We then reestimated our models with the inclusion of state-specific linear time trends; here again the effect of Medicaid coverage on mobility outcomes remains large and statistically significant. This provides additional evidence that the observed association between Medicaid policy and mobility outcomes is not being driven by correlated trends at the state level.
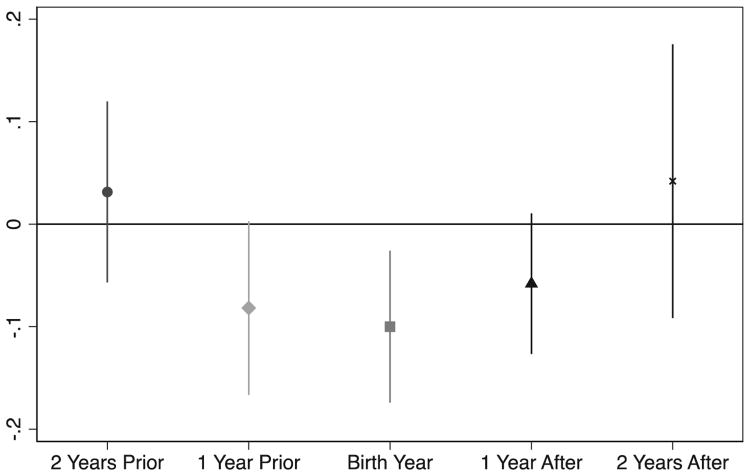
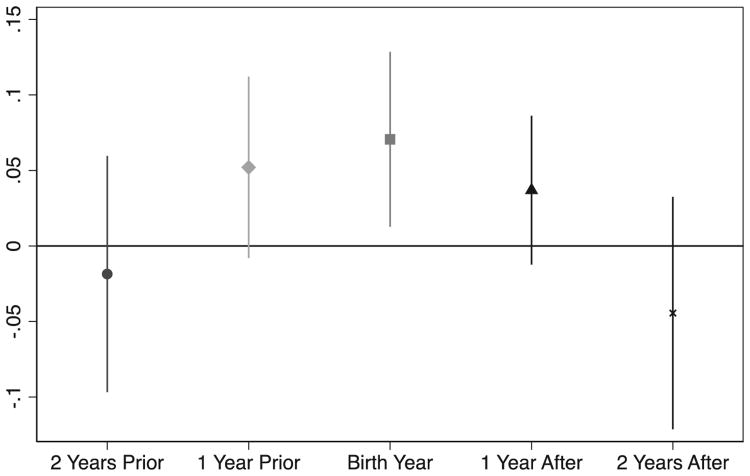
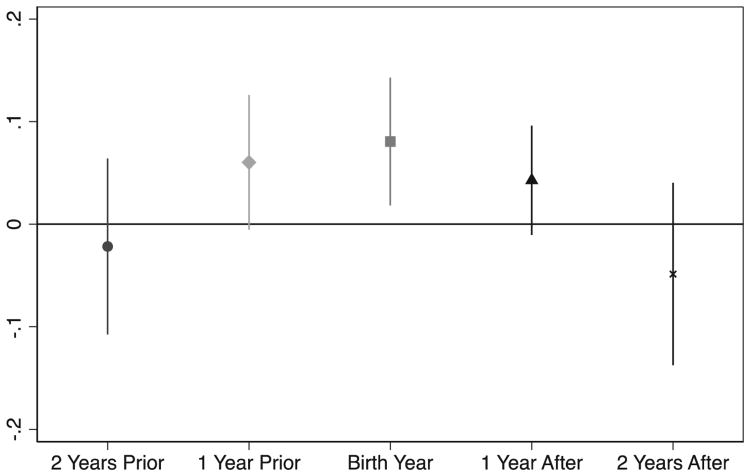
To further test that the observed association between Medicaid eligibility and mobility outcomes is not being driven by contemporaneous policy shifts, we conducted a “placebo test” by estimating the effect of Medicaid coverage on mobility outcomes using simulated Medicaid eligibility one and two years before and one and two years after the focal birth cohort (see Chetty and Hendren 2016). If Medicaid expansions were correlated with other state-level trends or policy interventions that might also affect economic mobility (e.g., investing in education or labor market reforms), we would expect our measures of Medicaid coverage to predict mobility outcomes for adjacent cohorts. Figures 1 through 3 present estimated coefficients from IV models for three different mobility outcomes: rank–rank slope, intercept, and absolute mobility for children born to parents at the 10th percentile. Across all three outcomes, the coefficient on Medicaid coverage two years before and two years after the birth year are not statistically significant. Notably, the coefficient on Medicaid eligibility for one year before and one year after the focal birth cohort approaches statistical significance and is slightly smaller in magnitude relative to the estimate from the focal birth cohort. This is expected given that Medicaid coverage was typically extended simultaneously to low-income pregnant women and infants up to age 1, resulting in an overlapping window of coverage in utero and during the first year of life. This falsification test provides further evidence that the observed association between Medicaid eligibility and economic mobility outcomes is not being driven by other state-level trends or co-occurring policy shifts.
Figure 1.
Estimated Effect of Medicaid Eligibility before and after Focal Cohort's Birth Year on County Rank–Rank Slope.
Note: Coefficients and 90% confidence intervals from fully adjusted instrumental variable models.
Figure 3.
Estimated Effect of Medicaid Eligibility before and after Focal Cohort's Birth Year on Expected Mean Income Rank of Children Born at 10th Percentile.
Note: Coefficients and 90% confidence intervals from fully adjusted instrumental variable models.
Discussion
Analyzing new place-based estimates of intergenerational economic mobility, we find that the Medicaid expansions of the 1980s increased the level of economic mobility experienced by affected cohorts. Increasing the percentage of low-income pregnant women and infant children eligible for this public health insurance program effectively reduced the correlation between the economic position of parents and their children. This finding not only offers additional evidence of the positive, long-run effects of the Medicaid program but also serves to illustrate how subnational policy variation can help account for observed variation in economic-mobility outcomes across localities and between birth cohorts.
Health is a critical pathway for the transmission of economic status across generations; our findings add to a growing body of work demonstrating how targeted early-life interventions that improve infant and maternal health can have lasting positive consequences. Improving maternal and infant health, however, is just one pathway through which expanding health insurance coverage may impact overall economic-mobility levels. Studies have linked insurance coverage, and the Medicaid expansions specifically, to improved outcomes on other measures, including a reduction in bankruptcies from medical debt (Gross and Notowidigo 2011). In reducing out-of-pocket costs and shielding families from potentially devastating debt (see Kalousova and Burgard 2013), increasing insurance coverage may serve to improve mobility outcomes by enabling families to invest more income in mobility-enhancing pathways, such as education. Although our analytic strategy—which isolates exposure to public health insurance in the birth year—suggests Medicaid affects mobility outcomes primarily by improving infant and maternal health and access to healthcare, we cannot rule out the myriad of additional pathways through which expanding insurance coverage leads to improvements in economic mobility.
It is also important to acknowledge the data used in this analysis present several clear limitations. First, the mobility estimates generated by CHKS measure child income only at age 26, whereas previous mobility measures capture child income later in life, during their prime working years. However, CHKS find that mobility estimates stabilize when children reach their late 20s, as opposed to the later ages favored by much of the literature, and demonstrate that using several years of data to measure a child's income has a negligible effect on mobility estimates. A second limitation of our study is that the mobility parameters generated by CHKS are built on the strong assumption that the relationship between the income percentile ranks of children and their parents is linear. As we use the publicly available data from CHKS, we do not have the individual-level data, and we thus cannot confirm the linearity of the relationship independently. However, CHKS provide substantial evidence to support their claim that this operationalization of the mobility relationship is accurate (see Data Appendix in Chetty et al. 2014). As such, we feel confident that, taken together, these parameters offer a useful summary metric of the local economic-mobility contexts.
At the same time, we must caution readers about the generalizability of our findings. This analysis demonstrates that expanding Medicaid coverage to low-income pregnant women in the 1980s and 1990s improved the economic-mobility outcomes of their children in adulthood. In so doing, this study adds to the growing body of evidence documenting the lasting positive consequences of this program expansion for low-income families. Yet these findings do not suggest that further expanding Medicaid eligibility will necessarily result in higher levels of economic mobility. This is because the Medicaid expansions of the 1980s, 1990s, and later extended coverage to very-low-income individuals; further expansions would therefore extend coverage to relatively less disadvantaged persons, who may not benefit from the program in the same way or to the same degree (see, however, Baicker and Finkelstein 2011). Moreover, it should be emphasized that the findings of this particular study—and of any study of economic mobility or other outcomes that span generations—are specific to the cohorts and time period analyzed. Studies of past social processes cannot be readily generalized to predictions of the future.
Nevertheless, this article provides further evidence that targeted interventions early in life can effectively mitigate the deterministic power of parents' social position on child outcomes. Indeed, policies and programs that focus on improving maternal and infant health—for example, through nutrition programs—or improving a child's social and cognitive development—for example, through Head Start and other early-schooling interventions—are also likely to play an important role in explaining variation in economic-mobility outcomes across place and over time. Future work should examine potential complementarities across programs to better understand how variation in the generosity of social safety-net programs and general public spending— on health, education, income assistance, and so on—serve to structure mobility outcomes.
Understanding the effect of public policies and programs on the structure of opportunity is important for our normative evaluation of these interventions. In an era of rising inequality, even public policies and programs that have been found to improve the absolute physical or material well-being of families may not necessarily influence patterns of economic mobility. Fully capturing the effect of policy interventions on mobility processes requires us to consider all of the pathways through which economic status is transmitted across generations. Health—across generations, throughout the life course, and between populations—must be integrated into analyses of economic mobility at both individual and population levels. Doing so will not only improve our understanding of how social inequalities are reproduced across generations but also reveal how policy interventions that improve health serve to affirm the American dream.
Figure 2.
Estimated Effect of Medicaid Eligibility before and after Focal Cohort's Birth Year on County Mobility Intercept.
Note: Coefficients and 90% confidence intervals from fully adjusted instrumental variable models.
Acknowledgments
We gratefully acknowledge seminar participants at Harvard, Wisconsin, Cornell, and Northwestern and the following individuals for their thoughtful feedback on this project: Atheendar Venkataramani, Janet Currie, Amitabh Chandra, Sara McLanahan, Christopher Sandy Jencks, Ichiro Kawachi, Lisa Berkman, Devah Pager, Jason Fletcher, Barbara Wolfe, Timothy Smeeding, Michael Collins, David Pedulla, and Simo Goshez. We also thank Laura Wherry and Sarah Miller for sharing data on Medicaid eligibility, Raj Chetty and colleagues for sharing mobility estimates, and Lillian Schultze for research assistance. This research was supported by the Robert Wood Johnson Foundation Health and Society Scholars program, a core grant to the Center for Demography and Ecology at the University of Wisconsin-Madison (P2C HD047873), and the Doris Duke Fellowship for the Promotion of Child Wellbeing.
Biographies
Rourke L. O'Brien is an assistant professor of public affairs at the University of Wisconsin-Madison. His research focuses on household and consumer finance, tax and budget policy, and the link between health and economic mobility. He previously served as a senior policy advisor at the U.S. Department of the Treasury and as an RWJF Health & Society Scholar at Harvard University.
Cassandra L. Robertson is a doctoral candidate in sociology at Harvard University. Her research focuses on child well-being, intergenerational economic mobility, and family structure, with an emphasis on policy applications and interventions.
Appendix.
Table A1.
Percentage of Women Ages 15 to 44 Eligible for Medicaid Coverage by State.
| Percent age of Women Eligible | Percentage Change in Eligibility | ||||
|---|---|---|---|---|---|
|
|
|
||||
| State | 1980 | 1986 | 1993 | 1980–1986 | 1986–1993 |
| Alabama | 10.16 | 17.00 | 40.86 | 67.30 | 140.29 |
| Alaska | 6.17 | 23.04 | 32.77 | 273.70 | 42.24 |
| Arizona | 1.83 | 12.32 | 38.82 | 572.26 | 215.02 |
| Arkansas | 7.65 | 16.81 | 43.71 | 119.93 | 159.95 |
| California | 25.64 | 29.98 | 61.25 | 16.94 | 104.28 |
| Colorado | 6.55 | 19.20 | 28.12 | 193.27 | 46.49 |
| Connecticut | 11.60 | 17.68 | 34.45 | 52.42 | 94.77 |
| Delaware | 5.64 | 14.71 | 42.25 | 160.91 | 187.23 |
| District of Columbia | 20.65 | 21.37 | 58.06 | 3.51 | 171.62 |
| Florida | 10.56 | 12.06 | 50.88 | 14.13 | 322.03 |
| Georgia | 3.62 | 13.81 | 34.69 | 282.11 | 151.15 |
| Hawaii | 16.78 | 22.75 | 67.84 | 35.55 | 198.21 |
| Idaho | 13.70 | 17.74 | 31.36 | 29.51 | 76.82 |
| Illinois | 14.96 | 18.05 | 32.15 | 20.67 | 78.08 |
| Indiana | 4.40 | 14.34 | 38.92 | 226.06 | 171.49 |
| Iowa | 6.39 | 17.14 | 39.42 | 168.08 | 130.02 |
| Kansas | 12.51 | 16.28 | 37.32 | 30.12 | 129.27 |
| Kentucky | 9.79 | 14.88 | 52.13 | 51.96 | 250.44 |
| Louisiana | 39.23 | 51.94 | 61.34 | 32.41 | 18.10 |
| Maine | 15.22 | 23.51 | 45.71 | 54.49 | 94.46 |
| Maryland | 14.92 | 15.46 | 32.55 | 3.63 | 110.52 |
| Massachusetts | 16.44 | 19.15 | 39.26 | 16.48 | 104.97 |
| Michigan | 18.18 | 24.26 | 42.89 | 33.43 | 76.79 |
| Minnesota | 10.44 | 26.81 | 59.51 | 156.83 | 122.00 |
| Mississippi | 6.05 | 28.42 | 59.49 | 369.94 | 109.33 |
| Missouri | 5.25 | 17.20 | 38.32 | 227.32 | 122.82 |
| Montana | 13.67 | 19.91 | 32.85 | 45.62 | 64.96 |
| Nebraska | 15.21 | 16.96 | 24.42 | 11.53 | 43.96 |
| Nevada | 9.71 | 9.80 | 26.45 | 0.90 | 169.95 |
| New Hampshire | 6.02 | 8.96 | 25.33 | 48.84 | 182.77 |
| New Jersey | 11.66 | 16.88 | 55.32 | 44.76 | 227.67 |
| New Mexico | 9.85 | 18.27 | 52.24 | 85.41 | 185.94 |
| New York | 21.69 | 26.49 | 46.68 | 22.12 | 76.22 |
| North Carolina | 10.16 | 12.60 | 43.99 | 24.07 | 249.09 |
| North Dakota | 13.91 | 16.78 | 31.54 | 20.65 | 87.97 |
| Ohio | 10.47 | 16.94 | 31.31 | 61.83 | 84.81 |
| Oklahoma | 8.00 | 15.42 | 46.61 | 92.88 | 202.28 |
| Oregon | 12.47 | 16.23 | 30.76 | 30.16 | 89.47 |
| Pennsylvania | 13.59 | 16.48 | 39.46 | 21.26 | 139.44 |
| Rhode Island | 21.11 | 17.03 | 47.35 | −19.35 | 178.11 |
| South Carolina | 10.04 | 22.98 | 53.91 | 128.92 | 134.62 |
| South Dakota | 7.32 | 21.74 | 32.20 | 196.95 | 48.10 |
| Tennessee | 8.99 | 13.72 | 44.19 | 52.68 | 221.99 |
| Texas | 3.48 | 12.24 | 49.27 | 251.59 | 302.56 |
| Utah | 9.99 | 29.52 | 26.31 | 195.39 | −10.87 |
| Vermont | 20.35 | 23.39 | 42.95 | 14.95 | 83.62 |
| Virginia | 12.53 | 13.46 | 25.40 | 7.37 | 88.71 |
| Washington | 18.34 | 23.87 | 35.51 | 30.15 | 48.76 |
| West Virginia | 8.54 | 21.45 | 45.98 | 151.17 | 114.42 |
| Wisconsin | 15.41 | 25.41 | 34.23 | 64.90 | 34.68 |
| Wyoming | 3.62 | 18.57 | 30.17 | 412.78 | 62.47 |
Table A2.
Simulated Percentage of Women Ages 15 to 44 Eligible for Medicaid Coverage by State.
| Simulated Percentage of Women Eligible | Percentage Change in Eligibility | ||||
|---|---|---|---|---|---|
|
|
|
||||
| State | 1980 | 1986 | 1993 | 1980–1986 | 1986–1993 |
| Alabama | 7.44 | 10.65 | 34.35 | 43.19 | 222.62 |
| Alaska | 9.54 | 33.94 | 41.05 | 255.58 | 20.97 |
| Arizona | 5.07 | 16.60 | 35.86 | 227.50 | 116.05 |
| Arkansas | 8.37 | 12.44 | 34.35 | 48.54 | 176.20 |
| California | 26.39 | 30.01 | 58.61 | 13.70 | 95.29 |
| Colorado | 10.80 | 21.87 | 34.35 | 102.44 | 57.11 |
| Connecticut | 17.41 | 25.23 | 44.82 | 44.96 | 77.65 |
| Delaware | 7.05 | 16.75 | 43.65 | 137.78 | 160.55 |
| District of Columbia | 14.04 | 19.19 | 44.90 | 36.62 | 134.06 |
| Florida | 8.75 | 14.41 | 44.90 | 64.64 | 211.66 |
| Georgia | 4.61 | 15.00 | 37.11 | 225.58 | 147.33 |
| Hawaii | 18.92 | 23.68 | 73.84 | 25.15 | 211.88 |
| Idaho | 12.93 | 16.40 | 34.46 | 26.79 | 110.13 |
| Illinois | 12.63 | 17.48 | 34.35 | 38.44 | 96.50 |
| Indiana | 6.76 | 15.89 | 37.38 | 135.03 | 135.27 |
| Iowa | 8.94 | 20.44 | 44.90 | 128.48 | 119.72 |
| Kansas | 15.71 | 19.58 | 37.38 | 24.67 | 90.87 |
| Kentucky | 10.43 | 12.51 | 44.82 | 19.97 | 258.18 |
| Louisiana | 34.17 | 46.37 | 48.25 | 35.69 | 4.07 |
| Maine | 13.49 | 27.11 | 42.93 | 100.96 | 58.35 |
| Maryland | 14.99 | 18.38 | 44.82 | 22.63 | 143.92 |
| Massachusetts | 17.50 | 24.57 | 48.17 | 40.42 | 96.03 |
| Michigan | 16.25 | 22.89 | 44.78 | 40.87 | 95.58 |
| Minnesota | 15.75 | 25.74 | 63.47 | 63.40 | 146.56 |
| Mississippi | 5.33 | 19.40 | 44.80 | 264.13 | 130.93 |
| Missouri | 6.68 | 15.89 | 34.35 | 137.96 | 116.23 |
| Montana | 14.79 | 18.69 | 34.35 | 26.34 | 83.82 |
| Nebraska | 14.40 | 18.85 | 34.35 | 30.87 | 82.24 |
| Nevada | 13.07 | 16.26 | 34.35 | 24.41 | 111.28 |
| New Hampshire | 13.04 | 20.77 | 37.54 | 59.34 | 80.72 |
| New Jersey | 13.04 | 20.03 | 67.88 | 53.52 | 238.97 |
| New Mexico | 9.38 | 14.63 | 44.80 | 56.06 | 206.15 |
| New York | 17.82 | 25.32 | 44.82 | 42.05 | 77.06 |
| North Carolina | 9.99 | 14.63 | 44.80 | 46.48 | 206.31 |
| North Dakota | 12.80 | 19.47 | 34.35 | 52.10 | 76.46 |
| Ohio | 11.22 | 17.07 | 34.35 | 52.20 | 101.22 |
| Oklahoma | 12.00 | 17.31 | 37.38 | 44.25 | 115.94 |
| Oregon | 12.13 | 21.42 | 34.35 | 76.62 | 60.38 |
| Pennsylvania | 14.40 | 19.44 | 44.82 | 34.97 | 130.56 |
| Rhode Island | 18.63 | 22.35 | 48.17 | 19.99 | 115.51 |
| South Carolina | 9.90 | 19.71 | 44.80 | 99.09 | 127.35 |
| South Dakota | 9.08 | 19.56 | 34.35 | 115.46 | 75.66 |
| Tennessee | 8.84 | 11.74 | 44.80 | 32.75 | 281.68 |
| Texas | 4.08 | 12.68 | 44.82 | 210.61 | 253.52 |
| Utah | 15.75 | 32.35 | 34.35 | 105.34 | 6.19 |
| Vermont | 21.46 | 26.33 | 48.71 | 22.72 | 84.98 |
| Virginia | 11.17 | 16.45 | 34.35 | 47.29 | 108.81 |
| Washington | 18.42 | 24.89 | 43.46 | 35.09 | 74.60 |
| West Virginia | 10.51 | 14.76 | 37.38 | 40.33 | 153.31 |
| Wisconsin | 17.83 | 26.85 | 38.59 | 50.61 | 43.75 |
| Wyoming | 6.45 | 19.62 | 34.35 | 203.88 | 75.13 |
References
- Aizer Anna. Poverty, Violence, and Health: The Impact of Domestic Violence During Pregnancy on Newborn Health. Journal of Human Resources. 2011;46(3):518–38. doi: 10.1353/jhr.2011.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizer Anna, Currie Janet M. The Intergenerational Transmission of Inequality: Maternal Disadvantage and Health at Birth. Science. 2014;344(6186):856–61. doi: 10.1126/science.1251872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker Katherine, Finkelstein Amy N. The Effects of Medicaid Coverage: Learning from the Oregon Experiment. New England Journal of Medicine. 2011;365(8):683–85. doi: 10.1056/NEJMp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharadwaj Prashant, Eberhard Juan P, Neilson Christopher A. Health at Birth, Parental Investments, and Academic Outcomes. Journal of Labor Economics. 2018;36(2):349–94. [Google Scholar]
- Black Sandra E, Devereux Paul J, Salvanes Kjell G. From the Cradle to the Labor Market? The Effect of Birth Weight on Adult Outcomes. Quarterly Journal of Economics. 2007;122(1):409–39. [Google Scholar]
- Boudreaux Michel H, Golberstein Ezra, McAlpine Donna D. The Long-term Impacts of Medicaid Exposure in Early Childhood: Evidence from the Program's Origin. Journal of Health Economics. 2016;45:161–75. doi: 10.1016/j.jhealeco.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks-Gunn Jeanne, Duncan Greg J. The Effects of Poverty on Children. The Future of Children. 1997;7(2):55–71. [PubMed] [Google Scholar]
- Brown David W, Kowalski Amanda E, Lurie Ithai Z. Working Paper 20835. National Bureau of Economic Research; Cambridge, MA: 2015. Medicaid as an Investment in Children: What Is the Long-term Impact on Tax Receipts? [Google Scholar]
- Case Anne, Lubotsky Darren H, Paxson Christina H. Economic Status and Health in Childhood: The Origins of the Gradient. American Economic Review. 2002;92(5):1308–34. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- Chetty Raj, Hendren Nathaniel. Working Paper 23001. National Bureau of Economic Research; Cambridge, MA: 2016. The Impacts of Neighborhoods on Intergenerational Mobility I: Childhood Exposure Effects. [Google Scholar]
- Chetty Raj, Hendren Nathaniel, Kline Patrick, Saez Emmanuel. Where Is the Land of Opportunity? The Geography of Intergenerational Mobility in the United States. Quarterly Journal of Economics. 2014;129(4):1553–623. [Google Scholar]
- Cohodes Sarah R, Grossman Daniel S, Kleiner Samuel A, Lovenheim Michael F. Working Paper 20178. National Bureau of Economic Research; Cambridge, MA: 2014. The Effect of Child Health Insurance Access on Schooling: Evidence from Public Insurance Expansions. [Google Scholar]
- Conley Dalton, Strully Kate W, Bennett Neil G. The Starting Gate: Birth Weight and Life Chances. Berkeley: University of California Press; 2003. [Google Scholar]
- Currie Janet M. Socio-economic Status and Child Health: Does Public Health Insurance Narrow the Gap? Scandinavian Journal of Economics. 1995;97(4):603–20. [Google Scholar]
- Currie Janet M. Healthy, Wealthy, and Wise? Socioeconomic Status, Poor Health in Childhood, and Human Capital Development. Journal of Economic Literature. 2009;47(1):87–122. [Google Scholar]
- Currie Janet M, Gruber Jonathan H. Saving Babies: The Efficacy and Cost of Recent Expansions of Medicaid Eligibility for Pregnant Women. Journal of Political Economy. 1996;104(6):1263–96. [Google Scholar]
- Currie Janet M, Lin Wanchuan. Chipping Away at Health: More on the Relationship between Income and Child Health. Health Affairs. 2007;26(2):331–44. doi: 10.1377/hlthaff.26.2.331. [DOI] [PubMed] [Google Scholar]
- Cutler David M, Gruber Jonathan H. The Effect of Medicaid Expansions on Public Insurance, Private Insurance, and Redistribution. American Economic Review. 1996;86(2):378–83. [PubMed] [Google Scholar]
- Figlio David N, Guryan Jonathan, Karbownik Krzysztof, Roth Jeffrey. Working Paper 18846. National Bureau of Economic Research; Cambridge, MA: 2013. The Effects of Poor Neonatal Health on Children's Cognitive Development. [DOI] [PubMed] [Google Scholar]
- Gross Tal, Notowidigdo Matthew J. Health Insurance and the Consumer Bankruptcy Decision: Evidence from Expansions of Medicaid. Journal of Public Economics. 2011;95(7):767–78. [Google Scholar]
- Haas Steven A. Health Selection and the Process of Social Stratification: The Effect of Childhood Health on Socioeconomic Attainment. Journal of Health and Social Behavior. 2006;47(4):339–54. doi: 10.1177/002214650604700403. [DOI] [PubMed] [Google Scholar]
- Haas Steven A, Glymour M Maria, Berkman Lisa F. Childhood Health and Labor Market Inequality over the Life Course. Journal of Health and Social Behavior. 2011;52(3):298–313. doi: 10.1177/0022146511410431. [DOI] [PubMed] [Google Scholar]
- Joyce Ted, Racine Andrew. CHIP Shots: Association between the State Children's Health Insurance Program and Immunization Rates. Pediatrics. 2005;115(5):526–34. doi: 10.1542/peds.2004-1533. [DOI] [PubMed] [Google Scholar]
- Kalousova Lucie, Burgard Sarah A. Debt and Foregone Medical Care. Journal of Health and Social Behavior. 2013;54(2):204–20. doi: 10.1177/0022146513483772. [DOI] [PubMed] [Google Scholar]
- Kane Jennifer B. An Integrative Model of Inter-and Intragenerational Preconception Processes Influencing Birthweight in the United States. Journal of Health and Social Behavior. 2015;56(2):246–61. doi: 10.1177/0022146515582043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klevens Monina R, Luman Elizabeth T. US Children Living in and near Poverty: Risk of Vaccine-preventable Diseases. American Journal of Preventive Medicine. 2001;20(4):41–46. doi: 10.1016/s0749-3797(01)00281-1. [DOI] [PubMed] [Google Scholar]
- Levine Phillip B, Schanzenbach Diane W. The Impact of Children's Public Health Insurance Expansions on Educational Outcomes. Forum for Health Economics and Policy. 2009;12(1) doi: 10.2202/1558-9544.1137. [DOI] [Google Scholar]
- Lurie Ithai Z. The Differential Effect of the SCHIP Expansions by Children's Age. Health Services Research. 2009;44(5):1504–20. doi: 10.1111/j.1475-6773.2009.01005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Sarah M, Wherry Laura R. The Long-term Health Effects of Early Life Medicaid Coverage. SSRN Working Paper 2466691. 2017 doi: 10.2139/ssrn.2466691. [DOI] [Google Scholar]
- Oreopoulos Philip, Stabile Mark, Walld Randy, Roos Leslie L. Short-, Medium-, and Long-term Consequences of Poor Infant Health: An Analysis Using Siblings and Twins. Journal of Human Resources. 2008;43(1):88–138. [Google Scholar]
- Palloni Alberto. Reproducing Inequalities: Luck, Wallets, and the Enduring Effects of Childhood Health. Demography. 2006;43(4):587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Salm Martin, Schunk Daniel. The Role of Childhood Health for the Intergenerational Transmission of Human Capital: Evidence from Administrative Data. MEA Discussion Paper 164. 2008 doi: 10.2139/ssrn.1444455. [DOI] [Google Scholar]
- Scharber Helen. Does “Out of Work” Get into the Womb? Exploring the Relationship between Unemployment and Adverse Birth Outcomes. Journal of Health and Social Behavior. 2014;55(2):266–82. doi: 10.1177/0022146514543799. [DOI] [PubMed] [Google Scholar]
- Smith James P. The Impact of Social Economic Status on Health over the Life Course. Journal of Human Resources. 2007;42(4):739–64. [Google Scholar]
- Smith James P. The Impact of Childhood Health on Adult Labor Market Outcomes. Review of Economics and Statistics. 2009;91(3):478–89. doi: 10.1162/rest.91.3.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strully Kate W, Rehkopf David H, Xuan Ziming. Effects of Prenatal Poverty on Infant Health: State Earned Income Tax Credits and Birth Weight. American Sociological Review. 2010;75(4):534–62. doi: 10.1177/0003122410374086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton Emily. Residential Segregation and Birth Weight among Racial and Ethnic Minorities in the United States. Journal of Health and Social Behavior. 2009;50(4):427–42. doi: 10.1177/002214650905000404. [DOI] [PubMed] [Google Scholar]