Abstract
In a substantial shift in payment policy, the State of Maryland has implemented a global budget program for acute care hospitals. Goals of the program included controlling hospital utilization and spending. Eight rural hospitals entered the program in 2010, while urban and suburban hospitals joined in 2014. Prior studies evaluated impacts of Maryland’s policy up to two years after its implementation, but yielded null or inconclusive results. We used a difference-in-differences analysis to assess whether acute hospital use and price-standardized hospital spending (a summary measure of utilization) changed differentially among Medicare beneficiaries served by rural hospitals versus an in-state control population. By 2013 – three years after the rural program began – we found no differential changes in acute hospital use or price-standardized spending among beneficiaries served by the affected hospitals. Our results suggest that, among Medicare beneficiaries, global budgets in rural Maryland hospitals did not reduce hospital utilization as policymakers had anticipated.
Policymakers and health care payers are implementing alternative payment models in an effort to control the growth of health care spending and to encourage providers to deliver high-value care.1-6 One payment model being tested by the Centers for Medicare and Medicaid Services (CMS), and implemented through a partnership with the State of Maryland, establishes global budgets for hospitals.7-9
Under this payment model, each acute care hospital in Maryland is provided with an annual all-payer budget, which specifies the total amount of revenue it can receive for inpatient, emergency department, and on-campus outpatient department services. By severing the link between volume and revenue, policymakers hoped to limit hospital spending growth and to encourage the provision of care outside of the hospital.8,10-12 Among alternative payment models, Maryland’s program is unique because it encompasses all health care payers – including Medicare, Medicaid, commercial insurers, and self-paying patients – and because it places care in each hospital under a budget.8
Maryland implemented this program in phases: eight rural hospitals received global budgets in 2010, followed by 36 larger, predominately urban and suburban hospitals in 2014. Prior analyses have investigated short-term impacts of Maryland’s program, examining outcomes up to two years after its implementation. One study, which focused on rural Maryland hospitals, found no change in readmissions attributable to the program, but only examined trends over an 18-month post-intervention period.13 Other evaluations assessed changes in utilization after Maryland’s statewide expansion of hospital global budgets in 2014.14,15 However, differences in pre-reform trends between Maryland and these studies’ control groups made it difficult to attribute subsequent changes in utilization to global budgets.
Because it may take time for providers to adjust to new payment incentives, it is important to examine longer-term trends in care as hospitals gain experience operating under global budgets. In this study, we examined changes in acute hospital use and price-standardized hospital spending (a summary measure of utilization) over a 3-year period following the introduction of global budgets in rural Maryland hospitals. To assess effects of this program, we used a difference-in-differences design that compared fee-for-service Medicare beneficiaries whose local hospitals first received global budgets in 2010 to an in-state control group. Our findings can help inform other efforts to use global budgets as an alternative to traditional fee-for-service payment in hospitals.16 For example, CMS has announced plans to introduce global budgets in several rural Pennsylvania hospitals.17
Methods
Maryland’s Hospital Global Budget Program
Since the 1970s, Maryland has operated a unique “rate-setting” system that regulates hospital prices for all health care payers. Prior to the introduction of global budgets, Maryland’s system constrained revenue per admission (for inpatient care) or per service (for outpatient care), without limiting total hospital revenue. Similar to Medicare’s national hospital prospective payment system, which reimburses hospitals at fixed rates without constraining aggregate spending, Maryland’s prior payment system enabled hospitals to increase their revenues by providing more care.18,19
Maryland’s global budget program counteracts incentives to provide more hospital care by establishing a “global” revenue constraint (i.e., a budget) for each of the state’s non-federal acute care hospitals. Each hospital’s budget is calculated from its historical utilization, forecasted changes in use, and prices, which Maryland continues to regulate. Hospitals bill payers per admission (for inpatient care) or per service (for outpatient care), but are now expected to raise or lower their prices to remain on budget. For example, if a hospital reduced its rate of admissions, it would increase its prices and presumably its operating margin. Conversely, a hospital with greater-than-expected utilization must reduce its prices so as not to exceed its budget. Hospitals face financial penalties if they exceed or fall below their budgets by more than 0.5% in any year.15,20 Budgeted revenues do not include payments to physicians for inpatient or outpatient care.
By constraining hospital revenue, policymakers sought to give hospitals a financial incentive to limit unnecessary hospital use, to manage patients’ care in settings not subject to a budget (e.g., community-based primary care practices), and to develop care management programs aimed at reducing potentially avoidable emergency department visits and hospital stays.8,9,12 (Additional details of Maryland’s program are provided in the Appendix.21)
Spending is the product of prices and utilization. It remains unclear whether hospitals in Maryland met their budgets by limiting patient volume or simply by changing their prices. In this study, we examined changes in hospital utilization from before to after the introduction of global budgets in rural Maryland hospitals. The Medicare population is ideal for this analysis, because elderly and disabled individuals have high rates of hospital use,22 and therefore are likely to be impacted by the payment change.
Study Population
We analyzed 2007-2013 enrollment and claims data for 100% of fee-for-service Medicare beneficiaries residing in Maryland. We limited our analyses to beneficiaries with continuous fee-for-service (i.e., Part A and Part B) coverage in the study year (or for decedents, continuous enrollment until death).
Affected Hospitals
Maryland placed 8 rural hospitals under global budgets in July 2010 (Appendix Exhibit 1). (21) Of these 8 hospitals, we excluded 1 (Western Maryland Regional Medical Center) from our analyses. This hospital opened in late 2009, replacing two smaller hospitals in its service area while offering an expanded scope of services that affected the combined hospitals’ budgets. Because this change was concurrent with the implementation of the global budget program, we limited the intervention population to Medicare beneficiaries living in areas primarily served by the 7 remaining hospitals. (Appendix Exhibit 2 plots trends in hospital utilization for Medicare beneficiaries residing in the service area of Western Maryland Regional Medical Center.) (21)
Treatment and Control populations
Because Maryland’s global budget policy is a population-level payment model – providing hospitals with budgets to care for their entire patient population – we determined patient exposure to the program based on where beneficiaries lived, rather than where they received care. Thus, our analyses were conducted on an intention-to-treat basis.
We measured exposure to the global budget program at the ZIP code level. To identify exposed and control populations, we calculated distances from each Maryland ZIP code to the closest affected and unaffected hospitals (see Section 2 of the Appendix for details). (21) We conducted within-Maryland comparisons because the state has a unique hospital payment system, and using an in-state comparison population allowed us to control for changes in the payment and regulatory environment that affected all Maryland hospitals during our study period.18,23
Our intervention population consisted of Medicare beneficiaries living in 117 Maryland ZIP codes located closer to one of the seven hospitals affected by the 2010 payment change than any other hospital. In the pre-intervention period (2007-2009), 74% of admissions from Medicare beneficiaries in these ZIP codes occurred at one of the intervention hospitals (Appendix Exhibit 3).(21)
The control population consisted of Medicare beneficiaries residing in 86 Maryland ZIP codes located at least 15 miles further from one of the affected hospitals compared to any other hospital. We excluded beneficiaries residing in metropolitan areas of Baltimore and Washington, DC because of substantial differences in patient demographics and the types of hospitals serving these areas compared to our intervention group (see Section 2 of the Appendix for details). (21) During the pre-intervention period, approximately 2% of admissions from Medicare beneficiaries residing in the control ZIP codes occurred at one of the intervention hospitals.
We excluded ZIP codes located 0-15 miles closer to a non-intervention hospital versus one of the affected hospitals. Excluding these ZIP codes avoided biasing our difference-in-differences estimates to the null since patients in these areas were partly served by the intervention hospitals. We also excluded ZIP codes within 20 miles of Western Maryland Regional Medical Center, as this hospital opened shortly before the implementation of the global budget program. Appendix Exhibit 4 displays areas of Maryland that encompass the intervention and control populations along with the 7 intervention hospitals, and Appendix Exhibit 5 lists the hospitals serving these populations. (21)
To assess the sensitivity of our estimates to the control population used, we conducted a supplementary analysis that limited the control population to Medicare beneficiaries residing in ZIP codes designated as rural and located least 15 miles further from an intervention hospital vs. any other hospital (see Section 7 of the Appendix for details of this analysis). (21)
Outcome Variables
We assessed changes in acute care utilization and price-standardized hospital spending from before to after the introduction of global budgets in rural Maryland hospitals. All outcomes were measured at the beneficiary-year level.
We measured beneficiaries’ use of acute hospital care as a count of inpatient admissions, observation stays, and emergency department visits that did not lead to admission. In sub-analyses, we separately assessed non-admitted emergency department visits and a composite measure of admissions and observation stays, which we term hospital stays. We assessed a combined measure of hospital stays because hospitals have increasingly classified short hospital stays as observation stays.24
Policymakers also hoped that Maryland’s program would encourage hospitals to develop initiatives aimed at deterring readmissions and returning emergency department visits.9 To assess changes in these outcomes, we measured the proportion of beneficiaries’ acute hospital visits (inpatient admissions, observation stays, emergency department visits) that were followed by a second acute hospital visit within 30 days (we term these 30-day return acute hospital visits).
In supplemental analyses, we assessed 30-day return hospital stays (comprising admissions and observation stays, but excluding emergency department visits). We also assessed changes in the proportion of emergency department visits that led to an inpatient admission.
We assessed price-standardized hospital spending as a summary measure of utilization, as this allowed us to capture potential changes in the composition of hospital care. (For example, hospitals could substitute higher-cost inpatient admissions with lower-priced emergency department visits, with no net change in the number of acute care visits.) Because prices differed across Maryland hospitals and were subject to change under the state’s global budget model, we calculated standardized prices using Medicare claims from non-Maryland hospitals, and applied these prices to claims for beneficiaries in our intervention and control populations. We measured standardized prices annually at the Diagnosis-Related Group level for inpatient claims, at the revenue code level for observation stays, and at the procedure code level for emergency department visits. In sub-analyses, we separately assessed changes in price-standardized hospital stay and emergency department spending.
Finally, because care in hospital outpatient departments is included in hospitals’ budgets, we assessed price-standardized hospital outpatient department spending, which we measured by applying national average procedure code-level prices to hospital outpatient department claims. We did not include a count of hospital outpatient department use as a study outcome given the wide heterogeneity in services provided in hospital outpatient departments. Section 3 of the Appendix provides additional information about these variables. (21)
Patient Characteristics
We used Medicare enrollment data to determine beneficiaries’ age, sex, race and ethnicity, disability status, receipt of Medicaid benefits, and presence of end-stage renal disease. We incorporated data from the Medicare Chronic Conditions Data Warehouse (CCW), which draws from claims since 1999 to measure beneficiaries’ accumulated burden of chronic disease, to assess the presence of 27 chronic conditions reported prior to each study year. In regression analyses, we controlled for indicators of each of these chronic conditions and counts of CCW conditions (indicators in unit increments for 2-8 versus ≥9 conditions).
Statistical Analyses
We used difference-in-differences analysis to compare changes in acute hospital use and price-standardized hospital spending in the intervention versus control populations from before to after the introduction of global budgets in rural Maryland hospitals. Our main analyses assessed average differential changes from the pre-intervention (2007-2009) to the post-intervention (2011-2013) periods. Because effects of the global budget program may have changed with time, in supplementary analyses, we estimated differential changes from the full pre-intervention period to each post-intervention year (2011, 2012, and 2013). We omitted 2010 because the global budget program was implemented in the middle of that year.
For each outcome, we fit a patient-year-level linear regression model to estimate differential changes, which we adjusted for patients’ clinical and demographic characteristics in addition to year and ZIP code fixed effects. We used propensity score weighting to balance observed characteristics of beneficiaries in the intervention and control areas in each study year.25 Thus, our difference-in-differences estimates represent differential changes among comparable Medicare beneficiaries in the intervention versus control populations. Additional details of our statistical analyses are provided in Sections 4 and 5 of the Appendix. (21)
An assumption of difference-in-differences analysis is that changes in the intervention and control populations would have been identical had the global budget policy not been implemented.26 To test this assumption, for each outcome variable, we assessed whether pre-2010 trends were parallel in the intervention and control populations.
Limitations
Our study had several limitations. First, although we used a within-state control population, our estimates could have been biased by unobserved time-varying factors that differentially affected the intervention and control populations. Second, we lacked claims for physician services for our 100% sample of Medicare beneficiaries. Consequently, we did not assess how the policy affected utilization outside of hospitals. Third, our study assessed changes in hospital use in the fee-for-service Medicare population, although Maryland’s program included all health care payers. To the extent that changes in providers’ financial incentives affected care for all patients served – an assumption supported by prior evidence27,28 – we would expect to see any changes associated with the implementation of hospital global budgets among Medicare beneficiaries. Fourth, our intervention population consisted of approximately 78,000 beneficiaries per year who were served primarily by seven hospitals. The relatively small number of patients and hospitals could have limited our statistical power to detect small differential changes in utilization or spending associated with hospital global budgets.
Results
Sample Characteristics
In the implementation year of Maryland’s global budget program for rural hospitals (2010), the intervention population consisted of 77,756 Medicare beneficiaries and the control population consisted of 68,117 beneficiaries. Before weighting, beneficiaries in the intervention population were more likely to be white, under age 65, and disabled, but had slightly fewer chronic conditions than beneficiaries in the control population (Exhibit 1). After weighting, there were no significant differences between the two populations, on average, on observed clinical or demographic characteristics.
Exhibit 1.
Characteristics of the intervention and control populations in 2010, before and after propensity score weighting
| Patient Characteristic | Before Weighting
|
After Weighting a
|
||
|---|---|---|---|---|
| Intervention population (n=77,756) | Control population (n=68,117) | Intervention population | Control population | |
|
| ||||
| Male (%) | 43.8% | 43.3% | 43.5% | 43.5% |
| Age group (years, %): | ||||
| <65 | 13.6% | 13.0% | 13.2% | 13.2% |
| 65–69 | 25.6% | 25.5% | 25.6% | 25.6% |
| 70–74 | 19.8% | 20.5% | 20.2% | 20.2% |
| 75–79 | 16.2% | 16.6% | 16.4% | 16.4% |
| 80–84 | 12.7% | 12.8% | 12.8% | 12.8% |
| ≥85 | 12.1% | 11.6% | 11.8% | 11.8% |
| Race/ethnicity (%): | ||||
| White | 89.8% | 86.0% | 88.1% | 88.1% |
| Black | 8.4% | 11.7% | 9.9% | 9.9% |
| Hispanic | 0.8% | 0.9% | 0.8% | 0.8% |
| Other | 1.0% | 1.4% | 1.2% | 1.2% |
| Disabled (%) b | 18.2% | 17.6% | 17.8% | 17.8% |
| Enrolled in Medicaid (%) c | 8.6% | 8.4% | 8.4% | 8.4% |
| End-stage renal disease (%) | 0.8% | 1.1% | 0.9% | 0.9% |
| Number of Chronic Conditions d | 5.24 | 5.30 | 5.26 | 5.26 |
Propensity score weights were used to balance the observed characteristics of patients in the intervention and control populations in each study year. Therefore, the effective sample sizes of the intervention and control populations in 2010 were 36,010 patients. After weighting, there were no differential changes on observed characteristics between the intervention and control populations from the pre-intervention to the post-intervention periods (see Appendix Exhibit 6).
Disability was the patient’s original reason for Medicare eligibility.
Dually enrolled in Medicare and Medicaid (excluding recipients of partial Medicaid coverage through the Qualified Medicare Beneficiary, Specified Low-Income Medicare Beneficiary, or Qualified Individual programs).
Assessed from the Medicare Chronic Conditions Data Warehouse (CCW), which includes indicators for the following 27 chronic conditions: Alzheimer’s disease, Alzheimer’s disease and related disorders or senile dementia, anemia, asthma, atrial fibrillation, benign prostatic hyperplasia, breast cancer, cataract, chronic kidney disease, chronic obstructive pulmonary disease, colorectal cancer, depression, diabetes, endometrial cancer, glaucoma, heart failure, hip or pelvic fracture, hyperlipidemia, hypertension, hypothyroidism, ischemic heart disease, lung cancer, osteoporosis, prostate cancer, acute myocardial infarction, rheumatoid arthritis, and stroke or transient ischemic attack. We assessed the presence of chronic conditions reported for each patient prior to the study year. Regression analyses were adjusted for indicators for each of these 27 chronic conditions as well as the patient’s count of chronic conditions (in unit increments from 2-8 conditions versus ≥ 9 conditions).
Source: Authors’ analyses of fee-for-service Medicare claims for 2010.
Comparison of pre-intervention trends
We saw comparable pre-intervention trends in the intervention and control populations for counts of acute hospital utilization, but statistically significant trend differences for price-standardized hospital spending (Appendix Exhibit 7). (21) Prior to the payment change, price-standardized acute hospital spending was initially lower in the intervention population than in the control population, but converged to the level of spending in the control population by 2009 (Exhibit 3). From 2008-2009, price-standardized outpatient spending increased markedly in the control population relative to changes in the intervention group.
Exhibit 3. Trends in price-standardized acute and outpatient hospital spending among Medicare beneficiaries in the intervention and control populations, 2007-2013.
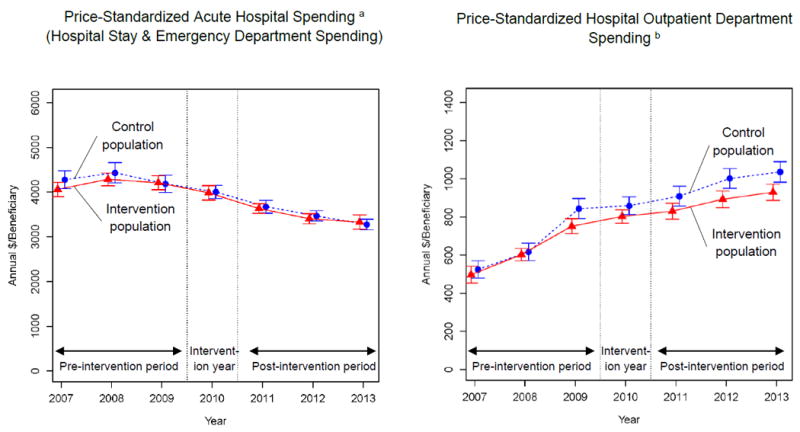
These graphs show unadjusted annual price-standardized spending for acute and outpatient hospital services in the intervention and control populations. The error bars denote 95% confidence intervals and were calculated using standard errors clustered at the ZIP code level. Because Maryland’s global budget program for rural hospitals was implemented in July 2010, we omitted 2010 from our regression analyses. Separate trends for price-standardized spending associated with hospital stays and emergency department visits that did not lead to an admission are plotted in Appendix Exhibit 8.
a Defined as the sum of price-standardized spending associated with hospital stays (inpatient admissions and observation-unit stays) and non-admitted emergency department visits. Because hospital prices were subject to change under Maryland’s global budget program, we price-standardized spending by applying mean national prices (measured annually at the level of Diagnosis-Related Groups for inpatient claims, revenue codes for observation-unit claims, and procedure codes for non-admitted emergency department claims) to claims for the corresponding categories of acute hospital use. Mean prices were calculated annually using Medicare claims from hospitals outside of Maryland. See Section 3 of the Appendix for additional information about the measures’ construction.
b We price-standardized spending for hospital outpatient department services, excluding emergency department visits and observation stays, by applying national average procedure code-level prices to hospital outpatient department claims. Standardized prices were assessed annually from national Medicare claims, excluding hospitals in Maryland.
Source: Authors’ analyses of fee-for-service Medicare claims for the periods 2007–2009 and 2011–2013.
Differential changes in acute hospital use
We observed comparable changes in acute hospital use in the intervention and control populations from before to after 2010. The corresponding differential change of +0.014 annual acute hospital visits per beneficiary in the intervention population (95% CI: -0.007 to 0.036; Exhibits 2 and 4) was equivalent to 1.9% of baseline acute hospital utilization in the intervention population (0.737 annual visits/beneficiary). Underlying these changes, we found a statistically insignificant differential reduction in hospital stays in the intervention population (-0.006 annual stays/beneficiary; 95% CI: -0.020 to 0.007; Appendix Exhibit 8),(21) equivalent to -1.5% of the intervention population’s baseline mean, and a differential increase in non-admitted emergency department visits (+0.020 annual visits/beneficiary; 95% CI: 0.004 to 0.037), or 5.8% of baseline emergency department use in the intervention group. The rate of 30-day return acute hospital visits did not change differentially between the intervention and control populations over the study period (Exhibits 2 and 4).
Exhibit 2. Trends in acute hospital utilization among Medicare beneficiaries in the intervention and control populations, 2007-2013.
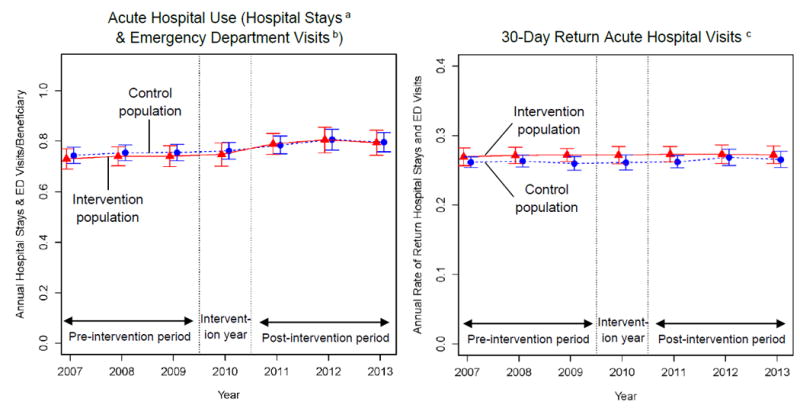
These graphs show unadjusted annual rates of acute hospital utilization for the intervention and control populations. The error bars denote 95% confidence intervals and were calculated using standard errors clustered at the ZIP code level. Because Maryland’s global budget program for rural hospitals was implemented in July 2010, we omitted 2010 from our regression analyses. Separate trends for hospital stays and emergency department visits that did not lead to an admission and are plotted in Appendix Exhibit 8.
a Hospital stays include inpatient admissions and observation stays. See Section 3 of the Appendix and the notes to Exhibit 4 for additional information about the measures’ construction.
b Emergency department visits that did not lead to an inpatient admission.
c Annual proportion of patients’ inpatient admissions, observation stays, and emergency department visits followed within 30 days by a second inpatient, emergency department, or observation visit. Assessed annually among patients with ≥1 inpatient admission, emergency department visit, or observation stay during the study year.
Exhibit 4.
Differential changes in acute hospital utilization and price-standardized hospital spending in the intervention and control populations
| Outcome | Intervention population pre-period mean a | Adjusted changes between the pre- and post-intervention periods b
|
Adjusted differential change c
|
||
|---|---|---|---|---|---|
| Intervention population | Control population | Estimate | 95% CI | ||
|
| |||||
| Acute hospital utilization: | |||||
|
| |||||
| Acute hospital use (Hospital stays d and Emergency Department visits e; Annual Count/Beneficiary) | 0.737 | -0.007 | -0.021 | 0.014 | (-0.007 to 0.036) |
|
| |||||
| Hospital stays (Annual Count/Beneficiary) | 0.391 | -0.078 | -0.072 | -0.006 | (-0.020 to 0.007) |
|
| |||||
| Emergency Department visits (Annual Count/Beneficiary) | 0.346 | 0.071 | 0.051 | 0.020 | (0.004 to 0.036) |
|
| |||||
| 30-day return acute hospital visits (Proportion) f | 0.271 | -0.014 | -0.014 | 0.000 | (-0.007 to 0.007) |
|
| |||||
| Price-standardized hospital spending: | |||||
|
| |||||
| Acute hospital spending g (Hospital stay and Emergency Department spending; Annual $/Beneficiary) | 4185 | -1115 | -1213 | 98 | (-69 to 265) |
|
| |||||
| Hospital Stay spending (Annual $/Beneficiary | 4123 | -1152 | -1246 | 94 | (-72 to 260) |
|
| |||||
| Emergency department spending (Annual $/Beneficiary) | 62 | 37 | 33 | 4 | (-2 to 10) |
|
| |||||
| Hospital Outpatient Department spending (Annual $/Beneficiary) h | 618 | 393 | 450 | -57 | (-99 to -15) |
Unadjusted annual mean in the intervention population over the period 2007-2009.
We defined the pre-intervention period as the years 2007-2009 and the post-intervention period as the years 2011-2013. Because Maryland’s global budget program for rural hospitals was implemented in July 2010, we omitted 2010 from our regression analyses.
Adjusted differential change from the pre-intervention to the post-intervention periods, comparing Medicare beneficiaries in the intervention versus control populations. The differential change was estimated using a weighted patient- and year-level linear regression model, adjusted for patient characteristics as well as year and ZIP code fixed effects. The weights balance the observed characteristics of patients in the intervention and control populations in each study year (see Section 5 of the Appendix for details of our statistical methods).
Hospital stays include inpatient admissions and observation stays.
Emergency department visits that did not lead to an inpatient admission.
Annual proportion of patients’ inpatient admissions, observation stays, and emergency department visits followed within 30 days by a second inpatient, emergency department, or observation visit. Assessed annually among patients with ≥1 inpatient admission, emergency department visit, or observation stay during the study year.
Because hospital prices were subject to change under Maryland’s global budget program, we price-standardized spending by applying mean national prices (measured annually at the level of Diagnosis-Related Groups for inpatient claims, revenue codes for observation-unit claims, and procedure codes for non-admitted emergency department claims) to claims for the corresponding categories of acute hospital use. Mean prices were calculated annually using Medicare claims from hospitals outside of Maryland.
We price-standardized spending for hospital outpatient department services, excluding emergency department visits and observation stays, by applying national average procedure code-level prices to hospital outpatient department claims. Standardized prices were assessed annually from national Medicare claims, excluding hospitals in Maryland.
Source: Authors’ analyses of fee-for-service Medicare claims for the periods 2007-2009 and 2011-2013.
In supplementary analyses, we found no differential change in the annual rate of 30-day return hospital stays (excluding emergency department visits, Appendix Exhibit 10)(21) or evidence of differential declines in acute hospital utilization emerging by the program’s third year (Appendix Exhibit 11).
Differential changes in price-standardized hospital spending
From before to after 2010, we found a non-significant $98 differential increase (95% CI: -69 to 265; Exhibit 4) in annual price-standardized acute hospital spending in the intervention population, which was equivalent to 2.3% of the intervention group’s baseline mean. However, given pre-2010 trend differences between the intervention and control populations (Exhibit 3 and Appendix Exhibit 7),(21) it is unclear whether this differential change can be attributed to the global budget program. We did not find statistically significant differential changes in price-standardized acute hospital spending in any specific post-implementation year (Appendix Exhibit 11). (21)
From before to after the 2010 payment change, we found a differential reduction in annual price-standardized outpatient department spending in the intervention population (-$57; 95% CI: -99 to -15; Exhibit 4). However, these changes reflected a continuation of trend differences that emerged prior the global budget program (Exhibit 3 and Appendix Exhibit 7). (21) Given this pre-reform difference in trends, we cannot reliably attribute subsequent differential changes in outpatient department spending to the introduction of global budgets.
Sensitivity of estimates to the control group used
Our results were generally similar when we compared the intervention group to an alternate control population limited to Medicare beneficiaries in rural ZIP codes (Appendix Exhibit 12).
Discussion
Over a three-year period following the introduction of global budgets in rural Maryland hospitals, we found no changes in acute hospital use (admissions, observation stays, and emergency department visits) or price-standardized hospital spending that could be attributed to the program. Although it may take time for hospitals to gain experience operating under global budgets, we found no evidence of reductions in acute care use or price-standardized spending emerging by the program’s third full year (2013). These results suggest that, among Medicare beneficiaries, Maryland’s introduction of global budgets in rural hospitals was not linked with reductions in hospital utilization that policymakers had hoped to achieve.
Our results are important given the mixed findings of prior analyses of Maryland’s program. While an analysis of the global budget policy in rural hospitals found no differential change in readmissions after 18 months,13 a study of the statewide program reported differential reductions in hospital admissions and increases in emergency department visits among Medicare beneficiaries.14 However, this study’s estimates could have been biased by different pre-intervention trends in its control versus intervention populations. Our study addressed these limitations by using a control group that exhibited more comparable pre-reform trends for acute hospital use, which enhanced our ability to isolate changes in utilization associated with the global budget program. This strength of our study design lends support to our conclusion that global budgets in rural Maryland hospitals had no substantive impact on Medicare beneficiaries’ use of hospital care.
Two important factors may account for these null findings. First, while Maryland’s program requires hospitals to adjust their prices to meet revenue targets, it does not directly affect payments to physicians, who are ultimately responsible for treating patients. This stands in contrast to other alternative payment models, such as Medicare’s Accountable Care Organization (ACO) programs, in which both physicians and hospitals bear risk for patients’ use of care.4,29 Interviews with hospital administrators indicated that some hospitals had difficulty aligning physicians’ incentives with the global budget model.15 The exclusion of physician payments may have limited the policy’s impacts on physician behavior, and ultimately, its effects on patient care.
Second, although Maryland’s program established annual budgets for hospitals, it did not actually pay hospitals on a prospective basis each year. Hospitals continued to bill payers per visit and were expected to adjust their prices to meet their budgets. This payment structure might have limited hospitals’ incentives to lower utilization, since price increases were generally limited to ≤5%.15 (Larger price adjustments were subject to the review and approval of state regulators.) Moreover, incentives to reduce utilization depend on how generously budgets are set. To the extent that hospitals were provided sufficiently large budgets, incentives for hospitals to reduce utilization to maintain their operating margins could have been weak.
Policy Implications
There is widespread interest in shifting from traditional fee-for-service payment to alternative payment models that give providers an economic incentive to efficiently manage their patients’ care.2-6 Unique among alternative payment approaches, Maryland’s global budget program attempts to establish these incentives by providing each hospital in the state with an annual all-payer budget. In contrast to alternative payment models like ACOs, which have demonstrated some success in slowing spending growth (including acute care spending),4,5,29-31 our findings indicate that the current structure of Maryland’s global budget program has not been effective in limiting hospital use.
Maryland has begun to address several limitations of its current payment model. In 2017, the state implemented a Care Redesign Program aimed at further engaging hospitals in care coordination and the management of chronically ill patients.32 In 2019, Maryland plans to expand the scope of its budget model to include inpatient and outpatient spending, and to establish ACOs that will coordinate and bear risk for the care of high-cost patients.33 It remains to be seen whether these reforms will lead to substantial changes in the state’s health care delivery system, and ultimately, patients’ costs and outcomes of care. Ongoing evaluation of Maryland’s program and other payment reforms is needed to identify which alternative payment models are most successful in changing how care is delivered.
Conclusion
In conclusion, we found no changes in hospital use among Medicare beneficiaries over a three-year period following the implementation of global budgets in rural Maryland hospitals. Our results underscore the need for policymakers to consider incentives for behavior change among hospitals and physicians when designing alternative payment models for hospital care.
Supplementary Material
Acknowledgments
Financial support was provided by the Commonwealth Fund, the National Institute on Aging of the National Institutes of Health (Grant No. P01 AG032952), and the Marshall J. Seidman Center for Studies in Health Economics and Health Care Policy at Harvard Medical School. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Eric T. Roberts, University of Pittsburgh Graduate School of Public Health in Pittsburgh, PA.
Laura A. Hatfield, Department of Health Care Policy, Harvard Medical School, in Boston, Massachusetts.
J Michael McWilliams, Department of Health Care Policy, Harvard Medical School.
Michael E. Chernew, Department of Health Care Policy, Harvard Medical School.
Nicolae Done, Boston University School of Medicine.
Sule Gerovich, Mathematica Policy Research in Baltimore, Maryland.
Lauren Gilstrap, Department of Health Care Policy, Harvard Medical School.
Ateev Mehrotra, Department of Health Care Policy, Harvard Medical School.
References
- 1.Anderson GF, Davis K, Guterman S. Medicare Payment Reform: Aligning Incentives for Better Care. New York, NY: Commonwealth Fund; 2015. [PubMed] [Google Scholar]
- 2.Burwell SM. Setting Value-Based Payment Goals – HHS Efforts to Improve U.S. Health Care. New England Journal of Medicine. 2015;372(10):897–899. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 3.Rajkumar R, Conway PH, Tavenner M. CMS-engaging multiple payers in payment reform. Jama. 2014;311(19):1967–1968. doi: 10.1001/jama.2014.3703. [DOI] [PubMed] [Google Scholar]
- 4.Nyweide DJ, Lee W, Cuerdon TT, et al. Association of pioneer accountable care organizations vs traditional medicare fee for service with spending, utilization, and patient experience. Jama. 2015;313(21):2152–2161. doi: 10.1001/jama.2015.4930. [DOI] [PubMed] [Google Scholar]
- 5.Song Z, Rose S, Safran DG, Landon BE, Day MP, Chernew ME. Changes in health care spending and quality 4 years into global payment. N Engl J Med. 2014 Oct 30;371(18):1704–1714. doi: 10.1056/NEJMsa1404026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dale SB, Ghosh A, Peikes DN, et al. Two-Year Costs and Quality in the Comprehensive Primary Care Initiative. New England Journal of Medicine. 2016;374(24):2345–2356. doi: 10.1056/NEJMsa1414953. [DOI] [PubMed] [Google Scholar]
- 7.Maryland All-Payer Model Agreement. [January 5, 2017];Contract. 2014 Available at: http://mhcc.maryland.gov/mhcc/pages/hcfs/hcfs_hospital/documents/chcf_all_payer_model_agreement.pdf.
- 8.Berenson RA. Maryland’s New All-Payer Hospita Demonstration: Interview with John Colmers, Donna Kinzer, and Josh Sharfstein. Washington, DC: Urban Institute; Nov, 2015. [Google Scholar]
- 9.Sharfstein JM, Kinzer D, Colmers JM. An update on Maryland’s all-payer approach to reforming the delivery of health care. JAMA Intern Med. 2015;175(7):1083–1084. doi: 10.1001/jamainternmed.2015.1616. [DOI] [PubMed] [Google Scholar]
- 10.Robeznieks A. Global budgets pushing Maryland hospitals to target population health. Modern Healthcare. 2014 Dec 6; [PubMed] [Google Scholar]
- 11.Rajkumar R, Patel A, Murphy K, et al. Maryland’s All-Payer Approach to Delivery-System Reform. New England Journal of Medicine. 2014;370(6):493–495. doi: 10.1056/NEJMp1314868. [DOI] [PubMed] [Google Scholar]
- 12.Porter E. Lessons in Maryland for Costs at Hospitals. New York Times. 2013 Aug 27; [Google Scholar]
- 13.Mortensen K, Perman C, Chen J. Innovative payment mechanisms in Maryland Hospitals: An empirical analysis of readmissions under total patient revenue. Healthcare. 2014;2(3):177–183. doi: 10.1016/j.hjdsi.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haber S, Beil H, Adamache W, et al. Evaluation of the Maryland All-Payer Model: Second Annual Report. RTI International; Aug, 2017. [Google Scholar]
- 15.Haber S, Beil H, Adamache W, et al. Evaluation of the Maryland All-Payer Model: First Annual Report. RTI International; Oct, 2016. [Google Scholar]
- 16.Sharfstein JM, Gerovich S, Chin D. Global budgets for safety-net hospitals. Jama. 2017 doi: 10.1001/jama.2017.14957. [DOI] [PubMed] [Google Scholar]
- 17.Pennsylvania Rural Health Model. [May 23, 2017];2017 https://innovation.cms.gov/initiatives/pa-rural-health-model/
- 18.Murray R. Setting Hospital Rates To Control Costs And Boost Quality: The Maryland Experience. Health Aff (Millwood) 2009 Sep 1;28(5):1395–1405. doi: 10.1377/hlthaff.28.5.1395. [DOI] [PubMed] [Google Scholar]
- 19.Pauly M, Town R. Maryland Exceptionalism? All-Payers Regulation and Health Care System Efficiency. Journal of Health Politics, Policy and Law. 2012 Aug 1;37(4):697–707. doi: 10.1215/03616878-1597502. [DOI] [PubMed] [Google Scholar]
- 20.An example global budget agreement with Carroll Hospital Center is available via this URL: http://www.hscrc.maryland.gov/documents/global-budgets/tpr/TPR-Agreement-Carroll-1-14-2015.pdf
- 21.To access the Appendix, click on the Appendix link in the box to the right of the article online
- 22.Moore B, Levit K, Elixhauser A. Costs for Hospital Stays in the United States, 2012. Rockville, MD: Agency for Healthcare Research and Quality; Oct, 2014. [PubMed] [Google Scholar]
- 23.Calikoglu S, Murray R, Feeney D. Hospital Pay-For-Performance Programs In Maryland Produced Strong Results, Including Reduced Hospital-Acquired Conditions. Health Aff (Millwood) 2012 Dec 1;31(12):2649–2658. doi: 10.1377/hlthaff.2012.0357. [DOI] [PubMed] [Google Scholar]
- 24.Hospital short-stay policy issues (Ch 7) Washington, DC: Medicare Payment Advisory Commission; Jun, 2015. [Google Scholar]
- 25.Li F, Morgan KL, Zaslavsky AM. Balancing Covariates via Propensity Score Weighting. Journal of the American Statistical Association. 2016:0–0. [Google Scholar]
- 26.Ryan AM, Burgess JF, Dimick JB. Why We Should Not Be Indifferent to Specification Choices for Difference-in-Differences. Health Serv Res. 2015;50(4):1211–1235. doi: 10.1111/1475-6773.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McWilliams JM, Landon BE, Chernew ME. Changes in health care spending and quality for Medicare beneficiaries associated with a commercial ACO contract. Jama. 2013 Aug 28;310(8):829–836. doi: 10.1001/jama.2013.276302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baicker K, Chernew ME, Robbins JA. The spillover effects of Medicare managed care: Medicare Advantage and hospital utilization. Journal of Health Economics. 2013;32(6):1289–1300. doi: 10.1016/j.jhealeco.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early Performance of Accountable Care Organizations in Medicare. N Engl J Med. 2016 Jun 16;374(24):2357–2366. doi: 10.1056/NEJMsa1600142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McWilliams JM. Changes in Medicare Shared Savings Program Savings From 2013 to 2014. Jama. 2016 Oct 25;316(16):1711–1713. doi: 10.1001/jama.2016.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McWilliams J, Gilstrap LG, Stevenson DG, Chernew ME, Huskamp HA, Grabowski DC. Changes in postacute care in the medicare shared savings program. JAMA Intern Med. 2017;177(4):518–526. doi: 10.1001/jamainternmed.2016.9115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Care Redesign and Population Health. 2016 http://www.hscrc.state.md.us/documents/md-maphs/pm/20161021/CPHIT-PMWG-presentation-10-21-16.pdf.
- 33.The Maryland All-Payer Model Progression Plan: Proposal to the Centers for Medicare & Medicaid Services. [2017, March 10];2016 http://dhmh.maryland.gov/Pages/DHMH-HSCRC-Draft-Progression-Plan-for-Public-Comment.aspx.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


