Abstract
Objectives
To evaluate the fracture resistance and mode of failure of maxillary premolars restorations restored with nanohybrid Composite, ORMOCER and Ceramic Inlays.
Materials and method
100 extracted first maxillary premolar were collected. Samples were divided into five groups. Group I – Intact premolars, Group II –MOD cavities without restorations, Group III – MOD cavities restored with composite restoration, GROUP IV – MOD cavities restored with ORMOCER restoration and GROUP V – MOD cavities restored with ceramic inlays. All the samples were sent for the axial compression test under the universal testing machine. Fracture resistance and fracture modes were recorded.
Result
Highest fracture resistance was achieved in Group V (1324.74 ± 336.78) almost comparable to that of natural tooth (1381.07 ± 259.36) (p < 0.05), followed by Group IV (MOD cavities with ORMOCER restorations) (1082.27 ± 351.27) (p < 0.01) and least fracture resistance in Group III (MOD cavities with composite restorations) (778.35 ± 100.25) (p < 0.0001). Mode of fracture in Group IV and Group V are almost similar and In Group III 65% of the cases showed non-restorable fractures.
Conclusion
ORMOCER fracture resistance along with other groups of clinically restorable fracture stand better than Nanohybrid composite.
Clinical Relevance
Based on the present study, the dentist can utilize the ORMOCER material as a restoration material for the cavities of posterior teeth which is better in terms of fracture resistance and durability of the restoration when compare to nanohybrid composite.
Keywords: Ceramic Inlays, Fracture Resistance, Mode of Fracture, Nanohybrid Composite, ORMOCER
1. Introduction
The demand for aesthetic restorations in MOD cavities for posterior dentition has increased during the last few decades.1, 2, 3, 4, 5, 6, 7 Use of adhesive materials to reinforce the weakened tooth structure was suggested in very early phase of dental practice,8 but due to lack of better formulations in aesthetic adhesive materials, amalgam was the gold standard materials for restoration of posterior tooth. Currently, composite resins and ceramic are available choices of for posterior aesthetic restorative material and recently organically modified ceramic (ORMOCER) is introduced.8, 9
Use of resin composite as aesthetic restorative material in posterior stress bearing areas have been increased due to availability of better aesthetics and good bonding.9 But despite of these improvements in the physical properties like polymerisation shrinkage are present within these resins limit their applications as a restorative material.10, 11 Ceramic is one of the basic groups of materials successfully used in dentistry for many years.12, 13, 14 Ceramic is claimed to be most biocompatible and natural appearing.15, 16, 17, 18, 19 But various studies done on restorations like ceramic inlays stated that these restorations are associated with a vast variety of complications.20 Restorative resin material like organically modified ceramic (ORMOCER) claimed to have improved physical and mechanical properties especially, when it was used as a posterior filling material with improved esthetics.9, 21 Thus, it is imperative to test such material against current successful materials.
The main purpose of this in vitro study is to evaluate and compare the fracture resistance of human maxillary premolars with MOD cavities restored with Nanohybrid Composite, Ceramic Inlays and ORMOCER restorations. Study also focuses on suggesting clinicians to select proper posterior aesthetic restorative material for long term clinical success and benefit of the patients.
2. Materials and Method
The present in vitro study was carried out on 100 non carious human maxillary 1st premolar which were schedule for orthodontic extraction with complete root formation and similar dimensions (Buccolingually 9 mm ± 10%, Mesiodistally 7 mm ± 10% and total tooth length 21 mm ± 10%) were collected. They were cleaned, disinfected and stored as per the recommendations and the guidelines lay by CDC (Centre for Disease Control and Prevention).22 Each tooth was examined under stereomicroscope X16 (3D Medical System) to check for cracks, surface defects, external aberrant anatomy or improperly formed roots. The selected teeth were stored in phosphate buffer saline solution. (Severn Biotech Limited Worcestershire, DT11 6TJ).
The root part of each sample was encircled with spacer wax, this acted as spacer to simulate PDL (periodontal ligament). Metallic mould with dimensions of 11 × 11 mm with clear cold cure acrylic resin (DPI, India) was used to mount the sample tooth. After the complete setting of the acrylic resin, tooth was taken out and spacer wax was removed. The space created in the acrylic resin block were filled with light body elastomeric impression material (Aquasil, Dentsply,Caulk Milford,DE) and tooth was again placed back in the block and excess of material was removed. Then the entire block was finished and polished. All the 100 samples prepared were divided into five groups (20 samples in each group).
Group I – Intact premolars (Negative control group)
Group II – MOD cavities with no restorations (Positive control group).
Group III – MOD cavities restored with composite restoration.
GROUP IV – MOD cavities restored with ORMOCER restoration.
GROUP V – MOD cavities restored with ceramic inlays.
MOD cavities were prepared for groups II, III, IV and V using high speed air rotor (Sirona, Germany) under air-water cooling and similar conditions. All internal angles were rounded and the total occlusal divergence of vertical walls was 5°each. The occlusal isthmus was 1/3rd of intercuspal distance i.e. 3 mm wide buccolingually and with 2 mm deep pulpal floor. The buccolingual widths on mesial and distal boxes were 3 mm wide, similar to the occlusal isthmus width. Each box had a gingival floor of 2 mm mesio distally and axial wall height of 2 mm. Margins were prepared with 90-° cavosurface angles. All the surfaces of the tooth were made with calibrated burs and measured with Williams graduated periodontal probe. The entire cavity was subjected to the coral and AutoCAD software for the accurate measurement of the angle of divergence of cavity.
Samples cavities of Group III were etched with 37% phosphoric acid (Tetric N Ceram, Ivoclar Vivadent, Fürstentum, Liechtenstein) for 30 s. Then metal matrices using toffelmire retainer were contoured around the tooth with medium fusing impression material. After this bonding agent was applied and Nanohybrid composite resin (Tetric N Ceram, Ivoclar Vivadent, Fürstentum, Liechtenstein) was placed in oblique increments in the tooth and each increment cured for 40 s. Finishing and polishing of was done using discs and burs (Shofu, Germany). Cavities of group IV was restored in similar way as in group III with ORMOCER restorations (Voco, Admira, Germany).
In Group V, direct wax pattern of the cavity was taken using inlay wax. Fabrication of inlay was done using IPS empress E – max II (Ivoclar Vivadent, Fürstentum Liechtenstein). All the teeth were etched with 37 percent phosphoric acid for 30 s. The inner surfaces of the ceramic restorations were etched with 4% percent hydrofluoric acid (IPS Ceramic Etching Gel, Ivoclar Vivadent, Fürstentum Liechtenstein) for 20 s. After that ceramic inlays were silanized with Monobond S (Ivoclar Vivadent, Fürstentum Liechtenstein). The ceramic inlays were luted and using multilink II dual-polymerizing resin composite and light cured For 40 s. (Ivoclar Vivadent, Fürstentum Liechtenstein) After polymerizing, the excess resin composite was removed with a scalpel (BD Bard-Parker Special Surgeon’s Blades no. 15C scalpel, Becton- Dickinson, Franklin Lakes, N.J.)
All the samples were checked for any kind of defects and then were sending for the axial compression test under universal testing machine (Instron 4467, India). After testing fracture resistance was noted and Fracture modes were recorded and observed by operator and volunteer, based on the degree of tooth structure and restoration damage, using a modified classification system proposed by Burke et al.23
-
•
TYPE I – Isolated fracture of restoration.
-
•
TYPE II – Restoration fracture involving a small tooth portion.
-
•
TYPE III – Fracture involving more than half of tooth, without periodontal involvement; and
-
•
TYPE IV – Fracture with periodontal involvement.
Fracture modes I–III represented restorable, but mode IV – Not restorable situations.
2.1. Statistical analysis
A null hypothesis was proposed that there is no significant difference in the fracture resistance of the three groups,that is, μ1 = μ2 = μ3. Along with alternate hypothesis, it was stated that there is a significant difference in the fracture resistance of the three groups, that is, μ1 ≠ μ2 ≠ μ3. A level of significance of α = 0.05 had been put. To compare the fracture resistance of the three groups, analysis of variance (ANOVA) is used. A p-value is compared with the level of significance. If p < 0.05, alternate hypothesis is considered and concluded that there is a significant difference in the fracture resistance of the groups. Otherwise, the null hypothesis is accepted.
If there is a significant difference between the groups, pair wise comparisons (post hoc tests) using Tukey’s test are performed.
The clinical parameters were assessed and analyzed by using a computer program statistics (SPSS Version 10.0; SPS Inc., Chicago, IL). Moreover, data were analyzed using mean standard deviation and Exact Binomial test.
3. Results
The group wise mean fractural resistance along with standard deviation (SD) and Range are shown in (Table 1). The mean resistance for control group was found maximum (1381.07 N), while group with only MOD cavity showed the least mean resistance (492.92 N). Amongst the restored groups, ceramic inlay showed maximum resistance (1324.74 N), followed by ORMOCER (1082.27N) while composite restoration indicated minimum (778.35 N). The range for ORMOCER group was maximum amongst all groups (770.28–2061.92 N).
Table 1.
Descriptive statistics for fractural resistance for study groups.
| Group name | No. of samples | Mean ± SD (N) | Range (N) |
|---|---|---|---|
| Control | 20 | 1381.07 ± 259.36 | (1079.6–2075.64) |
| MOD cavity | 20 | 492.92 ± 98.91 | (356.72–692.86) |
| Composite restoration | 20 | 778.35 ± 100.25 | (631.12–1024.1) |
| ORMOCER restoration | 20 | 1082.27 ± 351.27 | (770.28–2061.92) |
| Ceramic inlay | 20 | 1324.74 ± 336.78 | (900.23–1963.58) |
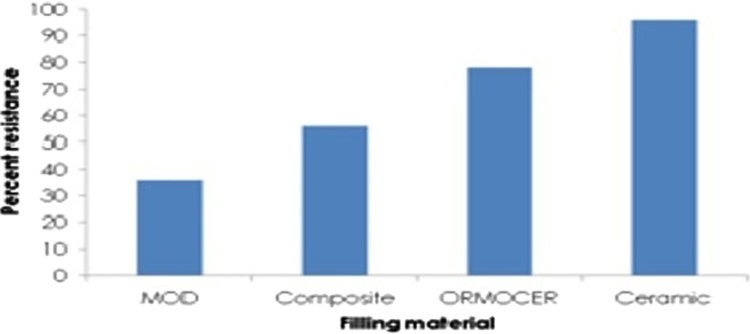
The results revealed that amongst the restored tooth the highest fracture resistance was achieved in Group V (1324.74 ± 336.78) almost comparable to that of the fracture resistance of a natural tooth (1381.07 ± 259.36) (p < 0.05) followed by Group IV (MOD cavities with ORMOCER restorations) (1082.27 ± 351.27) (p < 0.01) and least fracture resistance in Group III (MOD cavities with composite restorations) (778.35 ± 100.25) (p < 0.0001) (Table 2). The mean resistance of each group was used to obtain percent resistance of each group with reference to control group. In case of restored group it was 56%, 78% and 96% in composite, ORMOCER and ceramic groups respectively (Fig. 1).
Table 2.
p-value for difference comparisons.
| Group comparison | Adjusted p-value |
Significance |
|---|---|---|
| Group I Intact tooth negative Control – GROUP II MOD Cavities positive control | 0.0000 | HS |
| Group I Intact tooth negative Control – GROUP III Composite Restorations | 0.0000 | HS |
| Group I Intact tooth negative Control – GROUP IV ORMOCER | 0.0031 | S |
| Group I Intact tooth negative Control – GROUP V Ceramic inlay | 0.9562 | NS |
| GROUP II MOD Cavities positive control – GROUP III Composite Restorations | 0.0074 | S |
| GROUP II MOD Cavities positive control – GROUP IV ORMOCER restorations | 0.0000 | HS |
| GROUP II MOD Cavities positive control – GROUP V Ceramic Inlay | 0.0000 | HS |
| GROUP III Composite Restorations – GROUP IV ORMOCER restorations | 0.0018 | S |
| GROUP III Composite Restorations – Ceramic inlays | 0.0000 | HS |
| GROUP IV ORMOCER restorations – GROUP V Ceramic | 0.0271 | S |
HS: Highly significant (p < 0.0001); S: Significant (p < 0.01); NS: Not significant (p > 0.05).
Fig. 1.
Mean resistance of each filling material expressed as percentage of resistance of control.
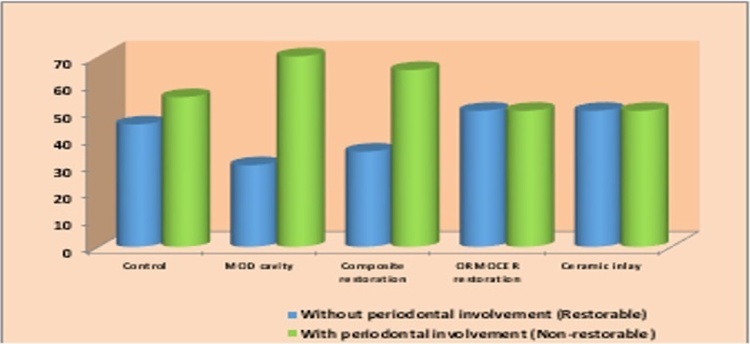
The other parameter observed was the mode of fracture. It was found that mode of fracture in Group IV and Group V are almost similar with 50% teeth showing restorable fracture mode. In Group III it was observed that 65% of the cases showed fracture involving the periodontium i.e. non restorable fractures and only 45% of the fracture were restorable (Fig. 2).
Fig. 2.
Number of restorable and non-restorable samples in each group.
4. Discussion
The main aim of this study is to evaluate the fracture resistance of different restorations in order to determine the durability and their use as posterior aesthetic restorative material.
Goal of restorative dentistry is to restore teeth in their form, function and aesthetic so as to achieve favorable stomatognathic environment. For many years amalgam is one of the most popular restorative materials. It is a well documented fact that by restoring a tooth with amalgam one cannot increase the fracture resistance of prepared tooth.24 The shortcomings of amalgam restorations mainly aesthetics have motivated the clinicians to search for better material formulations which mask the undesirable effects and fulfill the need of better aesthetic posterior restoration.
The results of this study confirm the alternate hypothesis that there is a significant difference exist between the group III, IV, and group V in terms of fracture resistance (p < 0.05) i.e. group V shows maximum fracture resistance (1324.74 ± 336.78 N) followed by ORMOCER group (IV) (1082.27 ± 351.27 N) and least fracture resistance in group III (778.35 ± 100.25 N) (composite group).
Hundred maxillary premolars were selected for the study as their anatomy favors cusp deflection and fracture under masticatory stresses25 and for the standardization. The samples were stored in phosphate-buffered saline not more than 12 weeks; Phosphate-buffered saline shows the best compatibility in maintaining the hydration of the extracted teeth.26
Creating the oral environment in an in vitro study is important as it gives clinical relevance to the study. It is reported that well supported natural tooth can sustain masticatory load up to 725 N and this load exceeded maximal biting forces in some overloading situations for example bruxism or traumatic occlusion.27 Alveolar bone support and the periodontal ligament are important for the mechanisms of stress distribution in natural teeth. This shock absorbing property of supporting tissue appears to be decisive factor in increasing the fracture resistance. Various materials are suggested for the simulation of bone for root embedment which vary from: acrylic resin, die stone or even polystyrene resin.28 In our study, clear cold cure acrylic resin was used for embedment of root 2 mm below cemento-enamel junction as it fulfills the requirement of alternative to bone as well as to have a clear vision to study fractures. In our study PDL was mimicked using light body elastomeric impression material. As this material is able to undergo elastic deformation and reproduce the PDL to accommodate the tooth in the alveolus and provide the non concentration of stresses in the cervical region of the tooth.29
The design of the cavity, width and depth plays a significant role in increasing and decreasing the fracture resistance of the tooth.30 To standardise and reduce the error all the MOD cavities in Group II, III, IV and V were made with 1/3rd of intercuspal distance. A 5° taper was decided and adhered in all cavities of group V and also in group II, III, and IV to standardise the cavities as 5-° taper were significantly more fracture resistant.31 To measure the angle of divergence of the cavities they were subjected to AutoCAD (2012) software.
Proper selection of restorative material results in highly aesthetic and long-lasting restorations. Various composite formulations have been tried in the past with varying degree of success. Nanohybrid composite resin was used to restore group III as the newer combination which contains nanohybrid fillers with the prepolymer technology provides the composites with lower shrinkage values.32 It is reported that nanohybrid composite resins features outstanding optical and mechanical properties.33, 34, 35
ORMOCER (organically modified ceramic) a new packable restorative material which was introduced, as an attempt to overcome some limitations and concerns associated with the traditional composites. ORMOCER materials contain inorganic-organic copolymers in addition to the inorganic silanated filler particles & synthesized through a solution and gelation processes (sol-gel process) from multifunctional urethane and thioether (meth) acrylate alkoxysilanes. ORMOCERS are described as three dimensionally cross-linked copolymers. The abundance of polymerization opportunities in these materials allows ORMOCERS to cure without leaving a residual monomer, thus having greater biocompatibility with the tissues.36 ORMOCER also focuses on overcoming the problems created by the polymerization shrinkage of conventional composites because its coefficient of thermal expansion is very similar to natural tooth structure. As ORMOCER is not much evaluated as posterior restorative material it was selected as one of the materials Samples of Group IV were restored with ORMOCER restorations for the current study.
It was observed that the light cured posterior composites placed in oblique increments helped to match the strength of remaining tooth structure.37 Hence in our study 1 mm (approx) increments of composite resin were placed in oblique manner and were light cured using LED lights for 40 s with soft start protocol with low irradiance and give effective polymerization. This not only helps to reduce heating of composite during curing but possibly permits the flow necessary to minimize the effects of polymerization shrinkage.38
With the introduction of improved ceramic formulations, new bonding procedures and new resin cements has led to an increase in their use. The IPS-Empress system was developed in 1983.39 It contains lithium disilicate glass ceramics which posses the property of thermal expansion mismatch between lithium disilicate crystals and glassy matrix which results in tangential compressive stresses around the crystals leading to crack deflection and strength increase.40 Group V MOD cavities were restored with IPS empress II ceramic inlays using the dual cure resin as conventional etch-and-rinse systems with dual-cured resin composites have been reported to be the gold standard for luting.41
Another important parameter in an in vitro study is artificial aging of tooth sample by thermocycling. In one of the study it was found that maxillary premolars with ceramic MOD inlays without thermocycling reached fracture toughness similar to intact teeth, however, the group that were thermocycled had decreased fracture resistance, by weakening the adhesive bond between restoration and tooth.42 Therefore in our in vitro study thermocycling was not done since it was postulated that it might affect adhesive bond leading to failures.27
All the samples were subjected to Instron Universal Testing Machine using cylinder as a plunger. A sphere plunger was not used as a plunger because it does not adapt to the anatomy of a premolar and it just contacted the tooth surface but not the restorations during loading which may affect the overall fracture resistance of teeth.23, 27, 42
In current vitro study, the control Group I had a mean fracture resistance value in universal testing machine of 1381.07 kN, which was in accordance to the other studies.27, 43 In group II (MOD cavities without restorations) the mean fracture resistance value recorded was 492.92 N and over all range of fracture resistance was 356.72–692.86 N. The fracture resistance was of 36% to that of group I (intact tooth) which is less as compared to other studies.44 This could be attributed to fact that the cavity was maintained with a 5 ° taper; which may have resulted in removal of more tooth structure and subsequent less tooth resistance. Comparison amongst the restored groups, Ceramic inlay (Group V) showed maximum mean fracture resistance while (1324.74 N±) while Composite restoration (Group III) indicated minimum fracture resistance (778.35N). In ORMOCER restorations (group IV) the mean fracture resistance recorded was 1082.27N. These results show statistically highly significant difference between group III of composite restoration and group V ceramic inlays (p < 0.0001). The results were statistically significant in case of group IV ORMOCER restorations and group V ceramic inlays (p < 0.01); it suggests that ORMOCER stands better than composite restorations and comparable to ceramic inlay restorations. The mean resistance of each group was used to obtain percent resistance of each group with reference to control group. In case of restored group it was 56%, 78% and 96% in composite, ORMOCER and ceramic groups respectively. The results of the study were in accordance to other study 27 for group of composite and ceramic inlay.
Fracture modes were recorded and observed by operator and a volunteer, based on the degree of tooth structure and restoration damage, using a modified classification system proposed by Burke et al.23 Fracture patterns in our study tended to involve restorations and cusps fractures.44, 45 However, there were 20% of Group V ceramic inlay samples in which the restorations fractured but not the tooth that was also reported by other study.29 This is probably due to ceramic material being more brittle in nature and it has high elastic modulus and tends to concentrate stresses inside the body of restoration.
Group V showed type I fracture 20% (Isolated fracture of restoration) type II fracture in 10% samples (Restoration fracture involving a small tooth portion), type III fracture in 20% samples (fracture involving more than half of tooth, without periodontal involvement) and type IV fracture in 50% samples (fracture with periodontal involvement). These results shows that restorable fractures in Group V restorations were overall 50% and non restorable fracture were similar to that of natural tooth .These results are in accordance to the studies.43, 45
In our study composite group fractured only as type II fracture in 5% samples (Restoration fracture involving a small tooth portion), type III fracture in 30% samples (fracture involving more than half of tooth, without periodontal involvement) it can be explained by the elastic modulus of composite being similar to the tooth and having good bond strength43 and type IV fracture in 65% samples (fracture with periodontal involvement) or non restorable fracture may be due poor mechanical properties of these resins.
The percentage of fracture i.e. type II fracture was 10% (Restoration fracture involving a small tooth portion), type III fracture 40% (fracture involving more than half of tooth, without periodontal involvement) and type IV fracture 50% (fracture with periodontal involvement) was
much less than that of composite. The percentage of mode of fracture was comparable to that of ceramic. This could be explained on the basis of fact that ORMOCER is basically organically modified ceramic with poly-condensed organic – inorganic network. This new class of material Ormocer combines the surface properties of the silicones, the toughness of the organic polymers and the hardness and thermal stability of ceramics36 ORMOCER formulation allows for a wide range of modification of mechanical parameters.9 Thus Ormocer acts superior to a nanohybrid composite and comparable to that of ceramic inlays.
5. Conclusion
Considering all the factors it can be mentioned that ORMOCER which is organically modified ceramic is a good aesthetic material with promising use as a posterior restorative material to enhance the fracture resistance of tooth as compared to Nanohybrid composite. However further studies should be undertaken to evaluate their clinical performance before it can be advocated as a aesthetic posterior restorative material.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The work was supported by the Department of Conservative Dentistry and Endodontics, Institute of Dental Sciences, Indore, M.P, India.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Acknowledgement
None.
Contributor Information
Mohit. K. Gunwal, Email: dr.mohitgunwal@yahoo.in.
Pratima R. Shenoi, Email: rshenoi@gmail.com.
Sonal Dhote, Email: srsatarkar@gmail.com.
Ravish Tongya, Email: ravishtongya@yahoo.co.in.
Magesh Kumar, Email: drmagesh@yahoo.in.
Sanjay Rastogi, Email: docos79@gmail.com.
References
- 1.Hunter A.R., Treasure E.T., Hunter A.J. Increases in cavity volume associated with the removal of class 2 amalgam and composite restorations. Oper Dent. 1995;20:2–6. [PubMed] [Google Scholar]
- 2.Larson T.D., Douglas W.H., Geistfeld R.E. Effect of prepared cavities on the strength of teeth. Oper Dent. 1981;6:2–5. [PubMed] [Google Scholar]
- 3.Millar B.J., Robinson P.B., Davies B.R. Effects of the removal of composite resin restorations on class II cavities. Br Dent J. 1992;173:210–212. doi: 10.1038/sj.bdj.4808004. [DOI] [PubMed] [Google Scholar]
- 4.Mondelli J., Steagall L., Ishikiriama A., de Lima Navarro M.F., Soares F.B. Fracture strength of human teeth with cavity preparations. J Prosthet Dent. 1980;43:419–422. doi: 10.1016/0022-3913(80)90213-9. [DOI] [PubMed] [Google Scholar]
- 5.Mondelli R.F., Barbosa W.F., Mondelli J., Franco E.B., Carvalho R.M. Fracture strength of weakened human premolars restored with amalgam with and without cusp coverage. Amer J Dent. 1998;11:181–184. [PubMed] [Google Scholar]
- 6.Jagadish S., Yogesh B.G. Fracture resistance of teeth with Class 2 silver amalgam, posterior composite, and glass cermet restorations. Oper Dent. 1990;15:42–47. [PubMed] [Google Scholar]
- 7.Sadowsky S.J. An overview of treatment considerations for aesthetic restorations: a review of the literature. J Prosthet Dent. 2006;96:433–442. doi: 10.1016/j.prosdent.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 8.Deliperi S., Bardwell D.N. Direct cuspal coverage posterior resin composite restoration:a case report. Oper Dent. 2006;30:143–150. doi: 10.2341/04-177. [DOI] [PubMed] [Google Scholar]
- 9.Manhart J., Kunzelmann K.H., Chen H.Y., Mechanical Hickel R. Properties and wear behaviour of light cured packable composite resins. Dent Mater. 2000;16:33–40. doi: 10.1016/s0109-5641(99)00082-2. [DOI] [PubMed] [Google Scholar]
- 10.Nasedkin J.N. Porcelain posterior resin-bonded restorations: current perspectives on aesthetic restorative dentistry; Part II. J Can Dent Assoc. 1988;54(7):499–506. [PubMed] [Google Scholar]
- 11.Christensen G.J. Buonocore memorial lecture. Tooth-colored posterior restorations. Oper Dent. 1997;22(4):146–148. [PubMed] [Google Scholar]
- 12.Banks R.G. Conservative posterior ceramic restorat ions: a literature review. J Prosthet Dent. 1990;63:619–626. doi: 10.1016/0022-3913(90)90316-5. [DOI] [PubMed] [Google Scholar]
- 13.Qualtrough A.J.E., Wilson N.H.F., Smith G.A. The porcelain inlay: a historical view. Oper Dent. 1990;15:61–70. [PubMed] [Google Scholar]
- 14.Kelly J.R., Nishimura I., Campbell S.D. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent. 1996;75:18–32. doi: 10.1016/s0022-3913(96)90413-8. [DOI] [PubMed] [Google Scholar]
- 15.Bergman M. Side-effects of amalgam and its alternatives: local, systemic and environmental. Int Dent J. 1990;40:4–10. [PubMed] [Google Scholar]
- 16.Rykke M. Dental materials for posterior restorations. Endod Dent Traumatol. 1992;8:139–148. doi: 10.1111/j.1600-9657.1992.tb00233.x. [DOI] [PubMed] [Google Scholar]
- 17.Baumann M.A., Heidemann D. Biocompatibility of dental inlay ceramics. In: Mörmann W.H., editor. Proceedings of the international symposium on computer restorations: state of the art of the cerec method. Quintessence Verlag; Berlin: 1991. pp. 373–376. [Google Scholar]
- 18.Rosenblum M.A., Schulman A. A review of all-ceramic restorations. J Am Dent Assoc. 1997;128:297–307. doi: 10.14219/jada.archive.1997.0193. [DOI] [PubMed] [Google Scholar]
- 19.Milleding P., Örtengren U., Karlsson S. Ceramic inlay systems: some clinical aspects. J Oral Rehabil. 1995;22:571–580. doi: 10.1111/j.1365-2842.1995.tb01051.x. [DOI] [PubMed] [Google Scholar]
- 20.Bergman Mark A. The clinical performance of ceramic inlays: a review. Aust Dent J. 1999;44:157–168. doi: 10.1111/j.1834-7819.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 21.Hickel Dasch R.W., Janda R., Tyas M., Anusavice K. New direct restorative materials. FDI Commission Project. Int Dent J. 1998;48(February):3–16. doi: 10.1111/j.1875-595x.1998.tb00688.x. [DOI] [PubMed] [Google Scholar]
- 22.Guidelines for Infection Control in Dental Health-Care Settings—Recommendations and Reports December 19, (2003) 52/No. RR-17. [PubMed]
- 23.Burke F.J., Wilson N.H., Watts D.C. The effect of cavity wall taper on fracture resistance of teeth restored with resin composite inlays. Oper Dent. 1993;18:230–236. [PubMed] [Google Scholar]
- 24.Eakle W.S. Fracture resistance of teeth restored with class II bonded composite resin. J Dent Res. 1986;65:149–153. doi: 10.1177/00220345860650021201. [DOI] [PubMed] [Google Scholar]
- 25.José Mondelli, Fábio Sene, Pereira Ramos Renata, Raquel Benetti Ana. Tooth structure and fracture strength of cavities. Braz Dent J. 2007;18:134–138. doi: 10.1590/s0103-64402007000200009. [DOI] [PubMed] [Google Scholar]
- 26.Jameson M.V., Tidmarsh B.G., Hood J.A. Effect of storage media on subsequent water loss and regain by human and bovine dentine and on mechanical properties of human dentine in vitro. Arch Oral Biol. 1994;39:759–767. doi: 10.1016/0003-9969(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 27.Antra Ragauska, Peteris Apse, Vladimirs Kasjanovs, Berzina Cimdina Liga. Influence of ceramic inlays and composite fillings on fracture resistance of premolars in vitro. Stomatologija Baltic Dent Maxillofacial J. 2008;10:121–126. [PubMed] [Google Scholar]
- 28.Soares Carlos José, Pizi Eliane Cristina Gava, Fonseca Rodrigo Borges, Roberto Luis, Martins Marcondes. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res. 2005;19:11–16. doi: 10.1590/s1806-83242005000100003. [DOI] [PubMed] [Google Scholar]
- 29.Soares C.J., Martins L.R., Fonseca R.B., Correr-Sobrinho L., Fernandes Neto A.J. Influence of cavity preparation design on fracture resistance of posterior leucite-reinforced ceramic restorations. J Prosth Dent. 2006;95:421–429. doi: 10.1016/j.prosdent.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 30.González López S., Sanz Chinesta M.V., Ceballos García L., de Haro Gasquet F., González Rodríguez M.P. Influence of cavity type and size of composite restorations on cuspal flexure. Med Oral Patol Oral Cir Bucal. 2006;11:E536–E540. [PubMed] [Google Scholar]
- 31.Esquivel-Upshaw J.F., Anusavice K.J., Yang M.C., Lee R.B. Fracture resistance of all-ceramic and metal-ceramic inlays. Int J Prosthodont. 2001;14:109–114. [PubMed] [Google Scholar]
- 32.Mahn Eduardo. The renaissance of a classic: tetric-N ceram—a perfect combination of experience and innovation. Cosmet Dent. 2008;2(2) [Google Scholar]
- 33.Yoshida Roberto M. Meeting challenges successfully with aesthetic posterior restorations. Int Dent SA. 2011;12:68–72. [Google Scholar]
- 34.Zorba Y.O., Bayindir Y.Z., Barutcugil C. Direct laminate veneers with resin composites: two case reports with five-year follow-ups. J Contemp Dent Pract. 2010;11:E56–E62. [PubMed] [Google Scholar]
- 35.Jennifer Melander, Link Michael P., Changqi X. Comparison of flexural properties and surface roughness of nanohybrid and microhybrid dental composites. Gen Dent SA. 2011:342–347. [PubMed] [Google Scholar]
- 36.Sivakumar A., Ashima Valiathan. Dental ceramics and ormocer technology – navigating the future. Trends Biomater Artif Organs. 2006;20:40–43. [Google Scholar]
- 37.Priscilla Solomon, Gopi Krishna, Parameswara A., Pradeep Gali, Deivanayagam Kandaswamy. Fracture resistance of premolar teeth with class II preparations restored with light cured composite with beta quartz inserts, light cured’ composite and silver amalgam in comparison with intact unrestored teeth- an in vitro study. J Conserv Dent. 2007;10:122–128. [Google Scholar]
- 38.Musanje L., Darvell B.W. Polymerization of resin composite restorative materials: exposure reciprocity. Dent Mater. 2003;19:531–541. doi: 10.1016/s0109-5641(02)00101-x. [DOI] [PubMed] [Google Scholar]
- 39.Brochu Jean-François, El Mowafy Omar. Longevity and clinical performance of IPS-empress ceramic restorations—a literature review. Can Dent Assoc. 2002;68:233–237. [PubMed] [Google Scholar]
- 40.Guess Petra C., Schultheis Stefan., Bonfante Estevam A., Coelho Paulo G., Ferencz Jonathan L., Silva Nelson R.F.A. All-ceramic systems: laboratory and clinical performance. Dent Clin North Am. 2011;55:333–352. doi: 10.1016/j.cden.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 41.Frankenbergera Roland, Lohbauera U., Schaiblea Rainer B., Nikolaenkob Sergej A., Naumann Michael. Luting of ceramic inlays in vitro: marginal quality of self-etch and etch-and-rinse adhesives versus self-etch cements. Dent Mater. 2008;24:185–191. doi: 10.1016/j.dental.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 42.de Habekost Luciano V., Camacho Guliherme B., Azevedo Eduardo C., Demarco Flavoi F. Fracture resistance of thermal cycled and endodontically treated premolars with adhesive restorations. J Prosth Dent. 2007;98:186–192. doi: 10.1016/S0022-3913(07)60054-7. [DOI] [PubMed] [Google Scholar]
- 43.Soares P.V., Santos-Filho P.C.F., Martins L.R.M., Soares C.J. Influence of restorative technique on the biomechanical behaviour of endodontically treated maxillary premolars. Part I: fracture resistance and fracture mode. J Prost Dent. 2008;99:30–37. doi: 10.1016/S0022-3913(08)60006-2. [DOI] [PubMed] [Google Scholar]
- 44.Blaser P.K., Lund M.R., Cochran M.A., Potter R.H. Effect of designs of class-2-preparations on resistance of teeth to fracture. Oper Dent. 1983;8:6–10. [PubMed] [Google Scholar]
- 45.St-Georges A.J., Sturdevant J.R., Swift E.J., Jr, Thompson J.Y. Fracture resistance of prepared teeth restored with bonded inlay restorations. J Prost Dent. 2003;89:551–557. doi: 10.1016/s0022-3913(03)00173-2. [DOI] [PubMed] [Google Scholar]