Abstract
The treatment of periodontitis primarily consists of mechanical debridement carried out by means of thorough scaling and root planing that might sometimes be a painful procedure which requires the administration of some form of local anesthesia. The present study comparatively evaluates the anesthetic effect of three such forms, viz; eutectic mixture of 25 mg/g lignocaine plus 25 mg/g prilocaine (EMLA) and needleless jet anesthesia during SRP. 30 patients with probing depth of 5 mm or more and visual analog scale (VAS) score of ≥30 mm on probing were selected and asked to assess the pain by VAS and verbal rating scale (VRS) during SRP after application of the two agents. The difference between the visual analogue values of control, EMLA and Madajet XL is highly significant (p < 0.001). According to the VRS scores, 6.7% of the subjects in the EMLA group reported no pain, 80% mild pain, and 13.3% moderate pain. In the Madajet XL group, 46.7% reported no pain and 53.3% mild pain. In the control group 100% of the patients reported moderate pain when none of the anesthetic was administered. None reported severe pain. Thus, the data suggest that both anesthetics are able to produce anesthesia of the tissues. The needleless anesthesia was relatively superior in performance to EMLA.
Keywords: Root planing, EMLA, Jet anesthesia, Periodontal therapy
1. Introduction
Periodontal diseases are a group of inflammatory diseases of microbial etiology. If the disease is left untreated, it may lead to attachment loss, loss of supporting structures of the teeth and eventual tooth loss. Long term studies support the removal of plaque both above and below the margin of the gingiva to promote healing and prevent further progression of inflammation and periodontal tissue destruction.1
Periodontal disease is not considered to be necessarily painful, but a subject may not say the same for the treatment. Periodontal scaling and root planing is an unpleasant and painful process for which local anesthesia is commonly used.
Thus, there is a need for an effective anesthetic preparation that is easy and painless to deliver for procedures involving periodontal tissues.2 The need for painless, noninvasive, fast-acting anesthetics with efficacy only during the procedure has led to the inquisition of the use of anesthetic agents that make the procedure less painful.
Although infiltration and nerve block is regarded gold standard and provide adequate anesthesia, the main drawback is pain associated with needle insertion and a long period of numbness of surrounding tissues such as lips and tongue.3 Another distressing aspect of dentistry for the average dental patient is fear and anxiety caused by the dental environment, particularly the dental injection i.e. syringe and needle also known as “Needle phobia” or “Blenophobia”.4, 5, 6 Fear of needle injections has been prevailing since the development of the conventional syringe in 1853. Epidemiological studies have shown that much of the population do not visit the dentist on regular basis, primarily because of the fear of needles which results in reduction in compliance with treatment.7
A variety of topical and needleless devices have been developed to overcome the drawbacks of conventional local anesthesia. An atypical anesthetic gel (Lidocaine 25 mg/g plus prilocaine 25 mg/g) has been developed to provide pain control during scaling and root planing. Main drawbacks of existing topical products are limited effectiveness and difficulties in regard to administration.3 Many studies have documented that eutectic mixture of local anesthetic agents (EMLA) is more potent than other topical anesthetics. Vickers and Punnia et al in their study found that EMLA 5% cream appeared to be more effective when compared with Xylocaine 5% and NUM (benzocaine 15%, amethocaine 1.7%).8
Needleless devices have also been developed to deliver anesthesia, relying on pressure to force the anesthetic liquid into oral tissues.9 These are self-contained automatic loading, spring-powered syringe devices with a jet nozzle, in which local anesthetic solution is rapidly propelled into tissue by means of mechanical spring pressure without the use of a needle has been developed.
Jet injections, first described in 1866, were originally developed for mass immunization.10 The objective of the needle-less jet injection is to deliver local anesthesia without subjecting the patient to the unpleasant experience of feeling the pain of “the needle”. Thereby, the jet syringe enables the patient to develop a more positive approach towards the dental treatment by eliminating his/her greatest fear.11
Hence, use of anesthetic gel (lidocaine 25 mg/g plus prilocaine 25 mg/g) and jet syringes averts needle stick injuries, produces quick and efficient anesthesia and thus, is a beneficial treatment modality. It banishes the risk of infection at injection site and excludes the risk of side effects due to lower doses.
Hence, the present study was undertaken with the aim to evaluate and compare the effectiveness of anesthetic gel EMLA (lidocaine 25 mg/g and prilocaine 25 mg/g) and needleless jet injection “MADAJET XL” during non-surgical periodontal debridement.
2. Materials and methods
2.1. Study population
The present randomized, controlled, single-center study with 30 chronic periodontitis subjects was approved by our Institutional Ethical Committee and carried out in the Department of Periodontics and Oral Implantology. A split-mouth design was followed and the products were applied in two quadrants, which were chosen randomly, in each subject. The third quadrant was taken as control.
Thirty subjects with age range 18 to 72 years and, with a minimum of five teeth in the selected quadrant having at least three teeth with periodontal pockets of ≥ 5 mm on each mesial, mid-buccal, distal and mid-palatal/lingual sites were included in this study. All subjects also reported a score of ≥3 0 mm on probing on a 100-mm visual analog scale (VAS).
Subjects with a history of allergy to local amide anesthetics were excluded from the study. Additionally, subjects with a significant systemic abnormality that would preclude SRP or the administration of a local anesthesia, pregnancy or lactation were not included.12
2.2. Procedure
EMLA was applied by means of a standard dental-cartridge system with a blunt applicator, left in the periodontal pocket for 5 min, where upon SRP was performed using hand scalers and universal and area specific curettes. The median dose of 5% EMLA was 0.2 g per tooth. If there was an interruption because of pain, the anesthetic was reapplied directly into the pocket of the same tooth, and SRP resumed. No further application of topical anesthetic was allowed. If the tooth was still painful, infiltration as rescue anesthesia was given.13
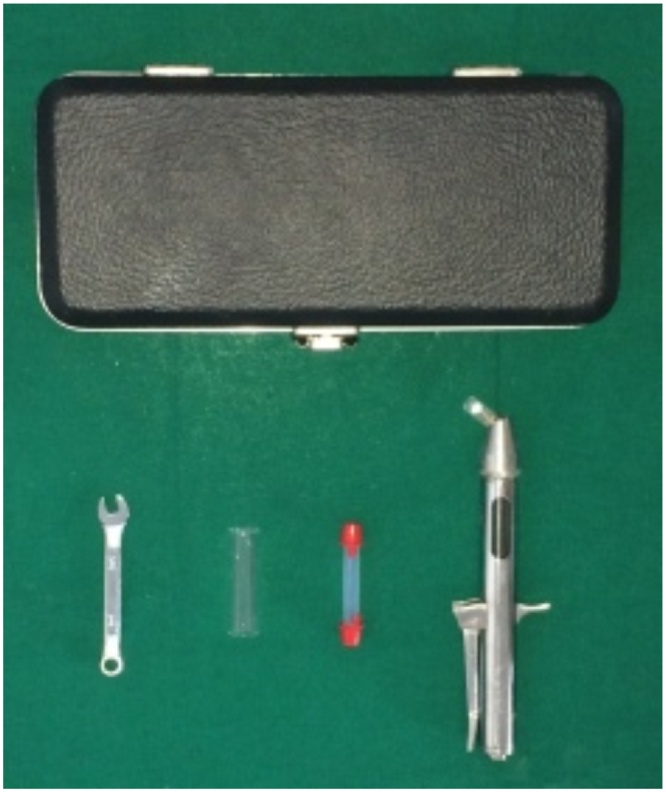
Madajet XL needle free injector manufactured by Advanced Meditech International Inc. (Mumbai) was used in the study. The injector consists of a head assembly with glass fill chamber holding up to 4 ml of local anesthetic solution, the body with a cocking lever and discharge button and Extend a tip and sheath which can be changed between each patient and allows for pinpoint accuracy at the injection site (Fig. 1). For Madajet XL, the pyrax chamber was filled either from regular dental syringe, or from a multiple dose 30cc sterile vial of 2% lidocaine. The head assembly of Madajet XL was primed to remove air and introduce the anesthetic into the head assembly. Madajet XL was held nose down, cocking lever was pulled down until it clicks (90°), the discharge (firing) button was pressed and fired (Fig. 2). Without the use of topical anesthesia the Madajet XL Jet injector was then placed gently against specific area to be injected so that sheath is firmly contacting the mucosa. Each injection of Madajet XL delivered a volume of anesthetic solution 1/10 of an ml at a depth of 2 to 2.5 mm below the epithelium. At the base of each infiltration a wheal approximately 6 mm is formed so that each injection into the tissue forms an inverted cone.14
Fig. 1.
Components of Madajet XL Assembly.
Fig. 2.
Placement of Madajet XL in patient's mouth.
Pain assessment was made at the end of procedures using the VAS and verbal rating scale (VRS). VAS pain scoring was done previous to the VRS pain scores to avoid any influence of an already selected verbal expression. If another anesthetic agent had to be given, the evaluation was made before it was given.
VAS was assessed on a 100-mm scale with the left endpoint marked “no pain” and the right endpoint marked “worst pain imaginable”.15,16 VRS is depicted as a five-point scale: no, mild, moderate, severe, and very severe pain.17
3. Observations and results
3.1. Statistical analysis
The Wilcoxon signed-rank test, Kruskal-Wallis test, and Mann- Whitney test were used.
3.2. Probing depth results
Table 1 shows the mean values of the pocket depth. There was no statistically significant difference among different groups at baseline.
Table 1.
Mean Pocket depth.
| Anesthetics | N | Mean ± std. deviation | p-value |
|---|---|---|---|
| Control | 30 | 5.20 ± 0.17 | 0.419 |
| EMLA | 30 | 5.30 ± 0.29 | |
| Madajet | 30 | 5.28 ± 0.23 |
Using ANOVA, it shows that there was no statistically significant difference among different groups at baseline. (p-value = 0.419) which is P > 0.05.
3.3. VAS results
Table 2 shows the mean values of the VAS of the two groups compared to the control were much lower. The difference from the baseline in two groups was very highly significant. The mean value of the Madajet XL was lowest amongst in three groups (15.00 ± 5.08).
Table 2.
Mean VAS and VRS values.
| Anesthetics | N | Mean VAS value | Mean VRS value | p-value |
|---|---|---|---|---|
| Control | 30 | 34.00 ± 4.98 | 3.00 ± 0.00 | < 0.001 |
| EMLA | 30 | 20.67 ± 4.49 | 2.07 ± 0.45 | |
| Madajet | 30 | 15.00 ± 5.08 | 1.50 ± 0.50 |
Shows the mean value for verbal analogue scale (VAS) values and verbal rating scale (VRS) of two test groups as compared to the control are much lower.
3.4. VRS results
Table 2 shows the mean values of the VRS of the two groups compared to the control were much lower. The difference from the baseline in two groups was very highly significant. The mean value of Madajet was lowest among the three groups (1.50 ± 0.50 mm).
3.5. Second application of anesthetic or rescue anesthetic
Neither the second application not a rescue was required for any of the patients.
4. Discussion
The present study is designed to evaluate the clinical effectiveness of 5% EMLA, and needleless jet injection during SRP. Subjects were asked to assess their pain perception using VAS and VRS during the procedure.
In the present study, a baseline VAS pain score of ≥ 30 mm is included, which was in accordance with the study conducted by Magnusson et al. By including only pain-sensitive subjects, the variations in overall VAS pain scores were eliminated. The operator who performed the probing to screen for pain sensitivity also carried out SRP with the study products. This measure was taken to avoid SRP being experienced as less painful by the subject because some operators have a more gentle technique than others.
The mean pocket depth for Control, EMLA, Madajet XL was 5.20 ± 0.17, 5.30 ± 0.29, 5.28 ± 0.23 respectively. It was found that there was no statistically significant difference among different groups at baseline (Table 1). Similar pocket depths were chosen so as to nullify the effect that different pocket depths can lead to different pain perception during root planing which was in accordance with the study conducted by Pandit N et al.18
Periodontal probing was used at baseline to screen for pain sensitivity, whereas the effect of the topical anesthetics was assessed during SRP. Friskopp et al.19 said that a scaling stroke on the root surface changes the conditions at the place of the stroke. Moving the instrument to another part of the root or to another tooth does not result in identical conditions. For this reason, periodontal probing was used as the indicator of perceived pain for the duration of action measure.
The mean value of visual analogue pain score in control, EMLA and Madajet XL test group was 34.00 ± 4.9, 20.67 ± 4.49, 15.00 ± 5.08 mm respectively (Table 2). The difference between the visual analogue values of control, EMLA and Madajet XL is highly significant (p ˂ 0.001). The Visual analogue pain score of Madajet XL test group was much lower than control and EMLA test groups.
The mean value of verbal rating pain score in Control, EMLA, Madajet XL group was, 3.00 ± 0.000, 2.07 ± 0.450, 1.50 ± 0.509 (Table 2). The difference between the verbal rating values of control, EMLA, local infiltration and Madajet XL were significant (p < 0.001).
The first product used in this study, EMLA, is a 1:1 oil-water emulsion of a eutectic mixture of lignocaine (2.5%) and prilocaine (2.5%) bases. Two double masked investigations have shown an increase in efficacy when lignocaine is used in combination with prilocaine in EMLA. According to Meechan JG 20 it have been shown that there is an increase in efficacy when lidocaine is used in combination with prilocaine. Hassio et al.21 saw that in the dosages used, the absorption of the local anesthetics was more rapid after the eutectic mixture application than after the spray application. Because of the relatively short application time, rapid absorption into the circulation, as well as good regenerative capacity of oral mucosa, tissue toxicity does not impose a risk when local anesthetics are applied topically on mucous membranes. He concluded that only small and relatively short surgical procedures can be performed using EMLA. Antoniazzi et al.22 compared the effects of EMLA 2.5 mg/g, injectable 2% liocaine, topical 2% benzocaine and a placebo substance on reducing pain during scaling and root planing. They concluded that EMLA provided similar effectiveness to injectable lidocaine.22 Franz-Montan et al.23 also found EMLA efficacious during the periodontal therapy.23 Daneskazemi et al. 24 reviewed various previous studies that used EMLA in periodontal treatment and concluded that it is an efficient anesthetic agent to be used for oral application and represents a good anesthetic duration locally for scaling and root planing.24
In a study by Magnusson I et al.17 70% patients reported no pain or mild pain. In present study it was found that in the EMLA test group 6.7% of the patients reported no pain, 80% reported mild pain, and 13.3% reported moderate pain (Table 3).
Table 3.
Mean value percentages of pain according to VRS.
| Anesthetics | No pain | Mild pain | Moderate pain |
|---|---|---|---|
| Control | 0 | 0 | 100 |
| EMLA | 6.7 | 80 | 13.3 |
| Madajet | 46.7 | 53.3 | 0 |
Shows that in the EMLA test group, 6.7% of the patients reported no pain, 80% reported mild pain, and 13.3% reported moderate pain.
The second test group was Madajet XL needleless jet injection. Needle-less local anesthesia with a jet injection device has been proposed by which a high-velocity spray of anesthetic solution is forced under high pressure into the oral mucosa, leading to mechanical infiltration of the compound through the mucosa. Each injection delivers into the tissue a volume of anesthetic of one tenth of an ml at a depth of 2.0 to 2.5 mm below the epithelium.
In the Madajet XL group 46.7% of the patients reported no pain, 53.3% reported mild pain. In the control group 100% of the patients reported moderate pain when none of the anesthetic was administered (Table 3).
When the patients were asked about the form of anesthesia they prefer 17 patients out of 30 (56.7%) preferred EMLA, 10 patients out of 30 (33.3%) preferred Madajet XL which was in accordance with the two different studies conducted by Steenberghe DV 2 and Makade CS et al.22 Steenberghe DV2 when compared anesthetic gel with injection anesthesia, he found that 70% of the patients preferred anesthetic gel while only 22% of the patients preferred injection anesthesia. Makade CS et al.25when compared pressure anesthesia with traditional method of anesthesia, it was concluded that pressure anesthesia was more accepted and preferred by patients (70%) than traditional anesthesia (20%).
In present study the preference of the patient was more towards the EMLA because the application of EMLA was least traumatic as well as because of good anesthetic properties. On the other hand patients showed apprehension to Madajet XL because of its bulky appearance. But it is well accepted that Madajet XL is better in relieving pain than EMLA for routine SRP procedure. None of the subjects required either a second application or a rescue anesthesia. None of the subjects reported with adverse events in the oral cavity on administration of anesthetics. Thus, it can be concluded under the limits of study that needleless jet device (Madajet) and topical anesthetic gel (EMLA) was effective in controlling pain and was well accepted and preferred by the patient.
Conflict of interest
None.
Contribution details
Dr. Rajan Gupta: Concepts, Designs, Definition of intellectual content, Literature search, Experimental studies, Data acquisition, Data analysis, Manuscript editing, Manuscript review.
Dr. Satwinder Kaur: Designs, Definition of intellectual content, Literature search, Data acquisition, Manuscript preparation, Manuscript review.
Dr. Parveen Dahiyad: Concepts, Designs, Literature search, Experimental studies, Data acquisition, Data analysis, Manuscript editing, Manuscript review, Guarantor.
Dr. Mukesh Kumar: Designs, Data acquisition, Statistical analysis, Manuscript editing, Manuscript review.
Contributor Information
Rajan Gupta, Email: info@hids.ac.in.
Satwinder Kaur, Email: info@hids.ac.in.
Parveen Dahiya, Email: info@hids.ac.in.
Mukesh Kumar, Email: info@hids.ac.in.
References
- 1.Perry D.A., Gensky S.A., Loomer P.M. Effectiveness of a transmucosal lidocaine delivery system for local anesthesia during scaling and root planing. J Clin Periodontol. 2005;32:590–594. doi: 10.1111/j.1600-051X.2005.00717.x. [DOI] [PubMed] [Google Scholar]
- 2.Steenberghe D.V., Bercy P., Boever J.D. Patient evaluation of a novel non-injectable anesthetic gel: A multicenter crossover study comparing the gel to infiltration anesthesia during scaling and root planing. J Periodontol. 2004;75:1471–1478. doi: 10.1902/jop.2004.75.11.1471. [DOI] [PubMed] [Google Scholar]
- 3.Milgrom P., Coldwell S., Getz T., Weinstein P., Ramsay D. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–762. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 4.Giangrego E. Controlling anxiey in the dental office. J Am Dent. 1986;113:728–735. doi: 10.14219/jada.archive.1986.0277. [DOI] [PubMed] [Google Scholar]
- 5.Friedson E., Feldman J.J. The public looks at dental office. J Am Dent. 1958;57:325–335. doi: 10.14219/jada.archive.1958.0178. [DOI] [PubMed] [Google Scholar]
- 6.Milgrom P. Increasing access to measure for prevention and treatment of anxiety, fear and phobia, perspective from a dental school based fear clinic. Anaesth Prog. 1986;33:624. [PMC free article] [PubMed] [Google Scholar]
- 7.Gatchel R.J., Ingersoll B.D., Bowman L., Robertson M.C., Walker C. The prevalence of dental fear and avoidance: a recent survey study. J Am Dent Assoc. 1983;107:609–610. doi: 10.14219/jada.archive.1983.0285. [DOI] [PubMed] [Google Scholar]
- 8.Vickers E.R., Moorthy P.A. A clinical evaluation of three topical anesthetics. Aus Den Journal. 1992;37:266–270. [PubMed] [Google Scholar]
- 9.Arapostathis K.N., Dabarakis N.N., Coolidge T., Tsirlis A., Kotsanos N. Comparison of acceptance, preference and efficacy between jet injection injex and local infiltration anesthesia in 6 to 11 year dental patients. Anaesth Prog. 2010;57:1–19. doi: 10.2344/0003-3006-57.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindmayer I., Menassa K., Lambert J. Development of new jet injector for insulin therapy. Diabetes Care. 1986;9:294–297. doi: 10.2337/diacare.9.3.294. [DOI] [PubMed] [Google Scholar]
- 11.Corah N.L., O'hea R.M., Ayer W.A. Dentists' management of patients' fear and anxiety. J Am Dent Assoc. 1985;110:734–736. doi: 10.14219/jada.archive.1985.0427. [DOI] [PubMed] [Google Scholar]
- 12.Carr M.P., Horton J.E. Clinical evaluation and comparison of two topical anesthetics for pain caused by needle sticks and scaling and root planing. J Periodontol. 2001;72:479–484. doi: 10.1902/jop.2001.72.4.479. [DOI] [PubMed] [Google Scholar]
- 13.Donaldson D., Gelskey S.C., Landry R.G., Matthews D.C., Sandhu H.S. Anestheic gel to reduce pain during periodontal scaling and root planing. J Clin Periodontol. 2003;330:171–175. doi: 10.1034/j.1600-051x.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- 14.Munshi A.K., Hegde A., Bashir N. Clinical evaluation of the efficacy of anesthesia and patient preference using the needle-less jet syringe in pediatric dental practice. J Clin Pediatr Dent. 2001;25:131–136. doi: 10.17796/jcpd.25.2.q6426p853266q575. [DOI] [PubMed] [Google Scholar]
- 15.Breivik H., Borchgrevink P.C., Allen S.M. Assessment of pain. Br J Anaesth. 2008;101:17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]
- 16.Collins S.L., Moore R.A., Quay H.J. The visual analogue pain intensity scale: what is moderate pain in millimeters. Pain. 1997;72:95–97. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 17.Magnusson I., Geurs N.C., Harris P.A. Intra pocket anesthesia for scaling and root planing in pain sensitive patients. J Periodontol. 2003;74:597–602. doi: 10.1902/jop.2003.74.5.597. [DOI] [PubMed] [Google Scholar]
- 18.Pandit N., Gupta R., Chandoke U., Gugnani S. Comparative evaluation of topical and electronic anesthesia during scaling and root planing. J Periodontol. 2010;81:1035–1040. doi: 10.1902/jop.2010.090702. [DOI] [PubMed] [Google Scholar]
- 19.Friskopp J., Huledal G. Plasma levels of lidocaine and prilocaine after application of Oraqix, a new intrapocket anesthetic, in patients with advanced periodontitis. J Clin Periodontol. 2001;28:425–429. doi: 10.1034/j.1600-051x.2001.028005425.x. [DOI] [PubMed] [Google Scholar]
- 20.Meechan J.G. Effective topical anesthetic agents and techniques. Dent Clin N Am. 2002;46:759–766. doi: 10.1016/s0011-8532(02)00035-6. [DOI] [PubMed] [Google Scholar]
- 21.Hassio J., Jokinen T., Numminen Rosenberg P.H. Topical anesthesia of gingival mucosa by 5% eutectic mixture of lignocaine and prilocaine or by 10% lignocaine spray. Br J Oral Maxillofac Surg. 1990;28:99–101. doi: 10.1016/0266-4356(90)90131-4. [DOI] [PubMed] [Google Scholar]
- 22.Antoniazzi R.P., Cargnelutti B., Freitas D.N., Guimaraes M.B., Zanatta F.B., Felden C.A. Topical intrapocket anesthesia during scaling and root planing: a randomized clinical trial. Braz Dent J. 2015;26:26–32. doi: 10.1590/0103-6440201300131. [13] [DOI] [PubMed] [Google Scholar]
- 23.Franz-Montan M., Baroni D., Brunetto G. Liposomal lidocaine gel for topical use at the oral mucosa: characterization, in vitro assays and in vivo anesthetic efficacy in humans. J Liposome Res. 2015;25:11–19. doi: 10.3109/08982104.2014.911315. [DOI] [PubMed] [Google Scholar]
- 24.Daneskazemi A., Abrisham S.M., Daneskazemi P., Davoudi A. The efficacy of eutectic mixture of local anesthetics as a topical anesthetic agent used for dental procedures: a brief review. Anesth Essays Res. 2016;10:383–387. doi: 10.4103/0259-1162.172342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Makade C.S., Shenoi P.R., Gunwal M.K. Comparison of acceptance, preference and efficacy between pressure anesthesia and classical needle infiltration anesthesia for dental restorative procedures in adult patients. J Conserv Dent. 2014;17:169–174. doi: 10.4103/0972-0707.128063. [DOI] [PMC free article] [PubMed] [Google Scholar]