Abstract
Objective
In a randomized clinical trial, to investigate the role of sleep-related cognitive variables in the long-term efficacy of an online, fully automated cognitive behavioral therapy intervention for insomnia (Sleep Healthy Using the Internet [SHUTi]).
Method
303 participants (Mage=43.3; SD=11.6) were randomly assigned to SHUTi or an online patient education condition and assessed at baseline, post intervention (9 weeks after baseline), 6- and 12-months after the intervention period. Cognitive variables were self-reported internal and chance sleep locus of control, dysfunctional beliefs and attitudes about sleep, sleep specific self-efficacy, and insomnia knowledge. Primary outcomes were self-reported online ratings of insomnia severity (Insomnia Severity Index), as well as sleep onset latency and wake after sleep onset from online sleep diaries, collected 12-months after the intervention period.
Results
Those who received SHUTi had, at post-assessment, higher levels of insomnia knowledge (95% CI=.10-.16) and internal sleep locus of control (95% CI=.04-.55), and lower dysfunctional beliefs and attitudes about sleep (95% CI=1.52-2.39) and sleep locus of control attributed to chance (95% CI=.15-.71). Insomnia knowledge, chance sleep locus of control, and dysfunctional beliefs and attitudes about sleep mediated the relationship between condition and at least one post 12-month sleep outcome. Within the SHUTi condition, changes in each cognitive variable (with the exception of internal sleep locus of control) predicted improvement in at least one sleep outcome one year later.
Conclusion
Online CBT-I may reduce the enormous public health burden of insomnia by changing underlying cognitive variables that lead to long-term changes in sleep outcomes.
Keywords: eHealth, Internet interventions, insomnia, cognitive behavioral therapy, cognitive mediators
1. Introduction
Insomnia is a massive public health concern (Ohayon, 2002), as well as a robust predictor of both mental and physical health problems (e.g., Baglioni et al., 2011; Fernandez-Mendoza & Vgontzas, 2013; Mallon, Broman, & Hetta, 2005; Taylor, Lichstein, Durrence, Reidel, & Bush, 2005). A growing area of research supports the efficacy of online interventions for insomnia (Christensen et al., 2016; Espie et al., 2012; Ritterband et al., 2009, 2017; Vincent, Walsh, & Lewycky, 2010; Zachariae, Lyby, Ritterband, & O’Toole, 2016), based on cognitive behavioral therapy for insomnia (CBT-I). However, the putative mechanisms of CBT-I, and in particular online CBT-I, have received relatively little attention (for a review see Schwartz & Carney, 2012). Importantly, recent work examining components of CBT-I has found that cognitive therapy is more predictive of lasting, long-term gains in sleep outcomes than is behavior therapy (Harvey et al., 2014). Thus, CBT-I programs that target cognitive mechanisms most relevant to a patient’s needs may optimize the opportunity for sustained success long after the active intervention. The present investigation examined the role of various cognitive mechanisms in mediating post-intervention 12-month sleep outcomes by comparing an online CBT-I program (Sleep Healthy Using the Internet [SHUTi]; Ritterband et al., 2009, 2017) with an online patient education condition.
Cognitive models of insomnia (e.g., Espie, Broomfield, MacMahon, Macphee, & Taylor, 2006; Harvey, 2002, 2005; Kaplan, Talbot, & Harvey, 2009) postulate that sleep difficulties are maintained and worsened when the automatic process of sleep is disrupted by thoughts of trying to will oneself to sleep and/or perseverating on maladaptive sleep beliefs. Individuals with insomnia often dwell on their sleep difficulty and the impact it has on their lives, leading to maladaptive thoughts and beliefs that can reinforce or exacerbate the insomnia. Importantly, CBT-I is designed, in part, to change underlying cognitive factors that impede the normal sleep process, such as cognitive restructuring exercises that help people identify and challenge distorted thoughts about sleep. For example, past research has found that dysfunctional beliefs and attitudes about sleep are strongly associated with objective sleep disturbance (Edinger et al., 2000), and one study of seventy-eight adults found that CBT led to great improvements in dysfunctional beliefs and attitudes about sleep, which in turn predicted better sleep outcomes and maintenance at follow-up sessions (Morin, Blais, & Savard, 2002).
A call has been made for more research to test whether the efficacy of CBT-I is, in fact, due to changes in theorized mechanisms (Schwartz & Carney, 2012). Recent work indicates that cognitive mechanisms are particularly important factors that contribute to long-term improvements in sleep. Specifically, Harvey and colleagues (2014) examined the comparative efficacy of behavioral therapy and cognitive therapy, relative to their combination (CBT). They found that while those who received CBT had the greatest improvements and those who received behavioral therapy had rapid gains, those who received cognitive therapy had a relatively slower yet sustained trajectory of gains six months after treatment. This suggests that cognitive therapy is a critical component that leads to sustained change by altering cognitive factors associated with sleep. Therefore, a primary aim of the present study was to examine the precise cognitive mechanisms associated with insomnia gains in an online CBT-I intervention one year later.
A few studies have examined whether the effects of online CBT-I on sleep outcomes are mediated by cognitive factors, but published research examining mediators of post 12-month sleep outcomes is virtually nonexistent. For example, in a study of one hundred adults with chronic insomnia, Vincent and colleagues (2010) examined the cognitive construct of internal sleep locus of control. A well-researched psychological variable, locus of control is the degree to which one believes they influence what happens to them (Rotter, 1966). Internal sleep locus of control is the belief that sleep is under one’s control, whereas external sleep locus of control is the belief that sleep is the result of external factors. Vincent and colleagues found that internal sleep locus of control mediated the influence of a computerized CBT-I condition (vs. a waiting-list control condition) on insomnia severity five weeks later. In another study of sixty-three adults, researchers found that dysfunctional beliefs and sleep safety behaviors mediated the link between an online CBT-I condition (vs. wait-list control condition) and both insomnia severity and sleep efficiency at post-intervention up to 8 weeks after initiating treatment (Lancee et al., 2015). Thus, there is some evidence that when compared to a wait-list control condition, online CBT-I leads to improved sleep outcomes by increasing internal sleep locus of control and decreasing external sleep locus of control and dysfunctional believes and attitudes about sleep.
Two other cognitive variables that may help explain the relationship between treatment condition and sleep outcomes are insomnia knowledge and sleep self-efficacy. Although some studies have found that sleep-related knowledge is linked to sleeping behavior (e.g., Kloss et al., 2015), knowledge acquisition may not always be a robust marker of behavior change. Since CBT-I involves educating patients on sleep (e.g., sleep hygiene), insomnia knowledge may help explain some of the treatment effects. However, this may not be the case when compared to a patient education condition. CBT-I is based on principles proven to help people successfully change maladaptive behaviors, like spending too much time in bed awake or napping. Thus, the belief that one has the ability to change their sleep behaviors (i.e., sleep self-efficacy) may be an important precursor to actually changing sleep patterns. To date, no studies have examined cognitive mechanisms of change when comparing online CBT-I to more active comparison conditions, such as online patient education. This is important since roughly 59% of all adults in the U.S., and 80% of all Internet users, look for health information online (Fox, 2011). In addition, most conclusions from past research are based on small samples with limited power and generalizability, and no studies have looked at these mechanisms over the long-term.
The aim of the current investigation was to test the hypothesis that SHUTi is more successful than online patient education in changing underlying cognitive variables associated with sleep, and that the beneficial impact of SHUTi on long-term primary sleep outcomes one year later is mediated by those cognitive factors. Whereas previous studies have typically included one or two cognitive variables and sleep outcomes, in this study, five sleep-related cognitive variables (i.e., insomnia knowledge, internal sleep locus of control, chance sleep locus of control, sleep self-efficacy, and dysfunctional sleep beliefs and attitudes) are examined to better understand specificity of effects on three sleep outcomes (i.e., insomnia severity, sleep onset latency, wake after sleep onset). Based on previous research, a priori hypotheses were threefold. Hypothesis 1 is that participants in the SHUTi condition, compared to those in online patient education condition, will experience increases in insomnia knowledge and internal sleep locus of control (i.e., sleep-related cognitive variables that promote sleep), and decreases in dysfunctional beliefs and attitudes about sleep and sleep locus of control attributed to chance (i.e., variables that impede healthy sleep patterns). Hypothesis 2 is that the impact of SHUTi on post 12-month sleep outcomes will be mediated by changes in dysfunctional beliefs and attitudes about sleep, as well as changes in sleep locus of control variables. Hypothesis 3 is that those who receive SHUTi will have increased sleep-specific self-efficacy, which will in turn lead to improvement in post 12-month sleep outcomes. Because the control condition also consisted of participants receiving accurate educational information about sleep, a competing hypothesis was that insomnia knowledge would not mediate the impact of condition on post 12-month sleep outcomes.
2. Method
2.1. Study Procedure
Data and analyses were based on a blind (participant) randomized controlled trial. Cognitive and sleep outcome variables were assessed at four time points: baseline, post intervention (i.e., 9 weeks after baseline), 6 months after the intervention period, and 12 months after the intervention period. Because the focus of the current investigation was on long-term sleep outcomes, only results for post 12-month sleep outcomes are presented (results for post and post-6 month sleep outcomes can be found in the online supplemental material and do not contradict 12-month findings).
Primary outcomes and a full description of the trial can be found in Ritterband et al., 2017. Participants were recruited via online advertisements and online posts. Interested individuals completed a brief online screening form and were then contacted by phone to collect further data regarding insomnia symptoms and to obtain online informed consent. Eligible participants were administered the MINI (Sheehan et al., 1998) and components of the Diagnostic Interview for Insomnia (Morin, 1993). Emails containing online login information were sent and participants were instructed to complete an online pre-assessment questionnaire and sleep diaries (10 diaries in a 2-week period). Upon completion of these steps, participants received an email containing information on how to begin using their assigned online intervention. After the 9-week intervention period was completed, participants were asked to complete online post-assessment questionnaires as well as additional online sleep diaries. These steps were repeated for the 6-month and 12-month follow-up assessments (participants received $50 for completing post and 6-month assessments, and $100 for completing the 12-month follow-up assessment). During the intervention period, researchers and staff did not interact with study participants except to respond to queries regarding technology problems. A diagram of the study procedure can be seen in Figure 1.
Figure 1.
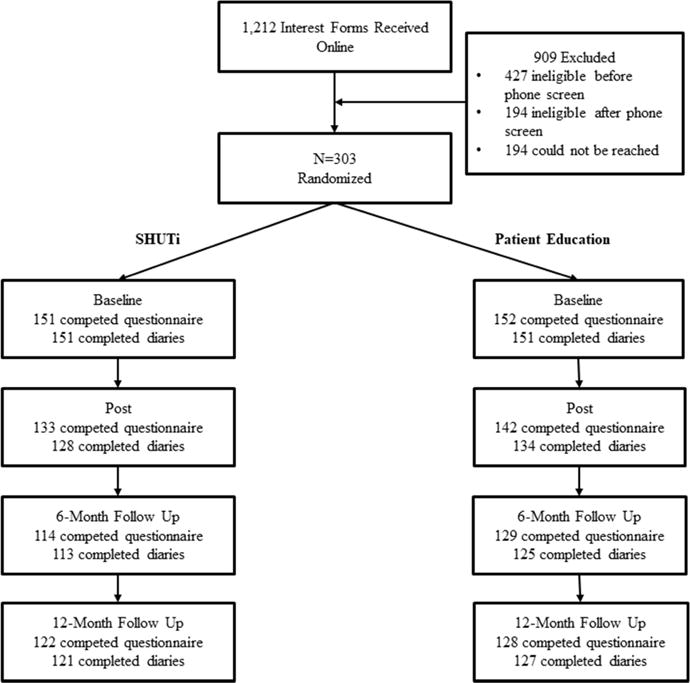
Flow diagram of study procedure.
The study was approved by the Institutional Review Board at the University of Virginia and is registered on clinicaltrials.gov (NCT01438697). Criteria for defining an adverse event was established before the start of the study and approved by the Data and Safety Monitoring Board, however, no participant reported a serious adverse event during the course of the study.
2.2. Participants
Adults with regular Internet access were eligible to participate if they met these inclusion criteria: 1) sleep-onset insomnia and/or sleep maintenance insomnia as defined by > 30 minutes for at least 3 nights/week for at least 6 months; 2) average total sleep time ≤ 6.5 hours, and 3) sleep disturbances (or associated daytime symptoms) causing significant distress or impairment in social, occupational, or other areas of functioning. Exclusion criteria were: 1) presence of another untreated sleep disorder; 2) an irregular schedule which would prevent adoption of intervention strategies (i.e., work schedule resulting in usual bedtime earlier than 8:00 PM or later than 2:00 AM or arising time earlier than 4:00 AM or later than 10:00 AM); 3) pregnancy; 4) current behavioral treatment for insomnia; and 5) initiation of psychological treatment in the previous 3 months. Individuals with severe depression (or with moderate to severe suicidality), bipolar disorder, and/or alcohol or other substance disorder in the last year were excluded from the study. Those with an active, unstable, and/or degenerative health condition (e.g., congestive heart failure) were also excluded. Individuals with comorbid psychiatric and/or physical health conditions were included unless they met one of the exclusionary criteria above. People taking medications (including sleep aids) could participate if the medication regimen had not changed in the previous 3 months. Overall, the study sample consisted of 303 participants (72% female) between the ages of 21 and 65 (Mage=43.3, SD=11.6). Participants were 84% White, 7% Black, 4% Asian, and 5% “other.” Participants were randomly assigned (using a random number generator) to SHUTi or the patient education condition.
2.3. Measures
Insomnia knowledge
A novel self-report measure was developed to assess individuals’ insomnia knowledge for this study. This resulted in a 16-item measure consisting of items about insomnia and general sleep knowledge (e.g., “Sleep is affected by lifestyle factors such as caffeine, nicotine, diet, and exercise”). Items were based on empirical literature and each item had a clear right or wrong response. Participants rated each item as true or false. The number of correct responses was scored in relation to the total number of items to form a proportion (i.e., percentage of accurate insomnia knowledge). Internal consistencies for the insomnia knowledge scale were α=.57 at baseline and .71 at post-assessment.
Sleep Locus of Control
Internal and chance sleep locus of control were assessed with the Sleep Locus of Control Scale (SLOCS; Vincent et al., 2004). Items assess the degree to which insomnia is perceived as due to factors within one’s control (internal sleep locus of control; e.g., “I am directly responsible for my sleep”) or as a result of chance or luck (chance sleep locus of control; e.g., “good sleep is largely a matter of luck”). Internal and external sleep locus of control scales are thought to measure related yet separate constructs. In the current study, zero-order correlations between scales at baseline, post, and 12-month post were r=−.24, −.25, and −.36, respectively, indicating a small to moderate degree of shared variance between these scales (r2=.06-.13). Participants rated each item on a 1 (strongly disagree) to 6 (strongly agree) scale. The SLOCS has good psychometric properties and predictive validity (Vincent et al., 2004).
Sleep Self-Efficacy
A 13-item measure was developed to assess self-efficacy in relation to sleep for this study, based on Bandura’s model and guide for constructing specific self-efficacy measures (Bandura, 1994; 2006). Participants were asked to rate the degree to which they felt confident regularly performing seven different sleep related tasks (e.g., “Follow a prescribed sleep schedule that restricts the amount of time you spend in bed”), as well as the degree to which they felt confident in their ability to regularly follow a sleep program. Participants rated each item on a 1 (not at all confident) to 10 (extremely confident) scale, and responses were aggregated to produce an overall sleep specific self-efficacy score, with higher scores reflecting greater self-efficacy. Internal consistencies for the sleep self-efficacy scale were α=.91 at baseline and .92 at post-assessment.
Dysfunctional Beliefs and Attitudes of Sleep
The 16-item Dysfunctional Belief and Attitudes about Sleep scale (DBAS; Morin, Vallieres, & Ivers, 2007) is widely used to assess distorted sleep related cognitions and beliefs. The DBAS assesses topics such as holding unrealistic expectations about sleep requirements (e.g., I must get 8 hours of sleep to feel refreshed and function well the next day) and misattribution or amplification of the consequences of insomnia (e.g., I am concerned that chronic insomnia may have serious consequences on my physical health). Participants rated each item (e.g., “I believe insomnia is essentially the result of a chemical imbalance”) on a 0 (strongly disagree) to 10 (strongly agree) scale. The DBAS has good psychometric properties with internal consistencies reported as α=.84 at baseline and .92 at post-assessment (Morin et al., 2007).
Sleep Outcomes
Severity of insomnia symptoms was assessed through the Insomnia Severity Index (ISI; Bastien, Vallières, & Morin, 2001), a 7-item measure with scores ranging from 0-28. Participants rated (0=none to 4=very severe) the degree to which they had various insomnia signs and symptoms (e.g., difficulty falling asleep; to what extent sleep problems interfere with daily functioning). Higher scores indicate more severe insomnia severity. Internal consistencies of the ISI were α=.66 and .89 at baseline and post-assessment, respectively. The ISI also has good sensitivity in detecting cases of insomnia and is sensitive to treatment response in clinical patients (Morin, Belleville, Bélanger, & Ivers, 2011).
In addition, sleep diaries were collected online and provided data related to time in bed, length of sleep onset, number and duration of awakenings, perceived sleep quality, and rising time. Data was collected prospectively for 10 days (during a 2-week period) at each of the four assessment periods. Sleep diary questions mirrored those from the Consensus Sleep Diary (Carney et al., 2012). Values for sleep onset latency (SOL) and wake after sleep onset (WASO) were averaged across the 10 days of diaries collection at each assessment period. SOL and WASO have served as primary dependent variables in previous papers examining the efficacy of CBT-I (e.g., Jungquist et al., 2010; Ritterband et al., 2017). Prospective sleep diaries are a well-validated method of assessing and tracking factors associated with insomnia (Buysse, Ancoli-Israel, Edinger, Lichstein, & Morin, 2006).
2.4. Conditions
Online CBT-I
SHUTi is a fully automated web-based program that is based on CBT-I, tailored to individual users (see Thorndike et al., 2008), and designed according to the Model for Internet Interventions (Ritterband, Thorndike, Cox, Kovatchev, & Gonder-Frederick, 2009). SHUTi has been found to be more efficacious than online patient education in changing primary sleep outcomes (insomnia severity, sleep onset latency, wake after sleep onset), with the majority of SHUTi users achieving insomnia remission status one year later (Ritterband et al., 2017). SHUTi is based on the primary principles of face-to-face CBT-I, including sleep restriction, stimulus control, cognitive restructuring, sleep hygiene, and relapse prevention. SHUTi contains six “cores” that are dispensed over time with new cores become available seven days after completion of a previous core. The fourth core focuses on cognitive restructuring. Based on CBT-I, users learn strategies and techniques for identifying and challenging negative thoughts that impede sleep. However, cognitive strategies and techniques are present throughout CBT-I (and SHUTi). This format was meant to mirror traditional CBT-I delivery procedures using a weekly session format. In SHUTi, users examine objectives of the current module, review and receive feedback on progress, learn new material, synthesize main points, and receive updated recommendations and homework assignments. Content and learning was developed to be interactive through the use of graphics, vignettes, personalized goal-setting, interactive exercises, and quizzes. Users also receive automated emails to encourage continued engagement and participation.
Online Patient Education Control
To compare the effects of SHUTi, half of participants received online patient education related to insomnia. The online patient education program provided accurate and relevant information regarding insomnia symptoms, causes and impact/prevalence of insomnia, as well as basic lifestyle and behavioral strategies to improve sleep. Content was based on reviews of insomnia-focused websites at the time of development, and therefore served as a rigorous control condition (relative to typical past research using a wait-list control condition). There was some content overlap between SHUTi and the patient education conditions; however, the patient education website did not personalize or tailor treatment to users, and presented content in a simple, straightforward way that did not leverage web-based technologies (e.g., video vignettes, interactive exercises, etc.). Unlike SHUTi, users in the patient education condition could access all information at once from the website.
2.5. Data Analysis
To examine whether SHUTi was associated with greater changes in cognitive variables versus the patient education condition, 2 condition (SHUTi vs. patient education) × 2 time (baseline vs. post) repeated measures analyses of variance (ANOVA) were conducted, with condition as a between-subject variable, separately for the following variables: insomnia knowledge, sleep locus of control (chance and internal), sleep self-efficacy, and dysfunctional beliefs and attitudes of sleep.
The reliable change index (RCI; Jacobson & Truax, 1991) is a statistic used to infer whether an intervention led to a clinically significant change in scores from before to after the intervention; it incorporates the mean and variance of scaled scores to establish a cutoff value of reliable change. An individual who experiences a meaningful and reliable change would have a pre- to post-intervention change that is greater than or equal to the RCI. To examine the relative impact of SHUTi versus patient education on cognitive variables, RCI values were calculated separately for the five cognitive variables being evaluated: Insomnia Knowledge (RCI=.25), Internal Sleep Locus of Control (RCI=1.34), Chance Sleep Locus of Control (RCI=1.66), Sleep Self-efficacy (RCI=1.13), and Dysfunctional Beliefs and Attitudes about Sleep (RCI=1.67).
For mediational and within-group analyses, residual scores of cognitive variables at post (i.e., scores at post-intervention from which baseline scores were partialed out) were computed to account for baseline levels of cognitive variables1. For mediational analyses, an SPSS macro was used (PROCESS; Hayes, 2013) that employs a bootstrapping procedure to produce an estimate of effects and 95% confidence intervals based on 5,000 resamples, with condition (0=patient education, 1=SHUTi) entered as the independent variable. Bootstrapping, a nonparametric method based on resampling with replacement, is commonly used when testing indirect effects such as in mediation analyses (Bollen & Stine, 1990; Shrout & Bolger, 2002), and has been used in other mediational studies comparing online CBT-I to a control condition (e.g., Lancee et al., 2015; Vincent et al., 2010). To examine the mediating role of individual cognitive variables in the link between condition and post 12-month sleep outcomes, residualized cognitive variables were first entered separately as mediators and sleep outcomes (e.g., insomnia severity) at baseline were entered as a covariate in all models. Then, to examine which of the cognitive variable(s) would most strongly mediate the link between condition and post 12-month sleep outcomes, all residualized cognitive variables were entered simultaneously as mediators in the same models.
To examine whether change in cognitive variables is partially a result of sleeping better, additional analyses were computed to examine the mediating role of sleep outcomes at post-intervention in the link between condition and 12-month post cognitive variables. The same PROCESS macro and bootstrapping method was used, with condition (0=patient education, 1=SHUTi) entered as the independent variable. To examine the mediating role of individual sleep outcomes in the link between condition and post 12-month cognitive variables, residualized sleep outcomes at post were first entered separately as mediators and cognitive variables (e.g., internal sleep locus of control) at baseline were entered as a covariate in all models. To understand the causal link between sleep outcomes and cognitive variables, only variables linked to significant indirect effects in Table 2 were tested (note, insomnia knowledge was not examined because it was not administered at 12-month post intervention).
Table 2.
Standardized coefficients representing the total indirect effects and 95% confidence intervals of Condition (0=Patient Education, 1=SHUTi) predicting sleep outcomes at 12-month post-assessment through cognitive variables at post assessment (bolded cells indicate significant effects at p<.05) for the entire sample.
| Insomnia Severity | Sleep Onset Latency | Wake After Sleep Onset | |
|---|---|---|---|
| Insomnia Knowledge |
−.24 (−.37, −.13) |
.04 (−.07, .16) |
−.04 (−.18, .10) |
| Sleep Locus Internal | −.03 (−.08, .001) |
−.01 (−.06, .01) |
−.01 (−.08, .01) |
| Sleep Locus Chance |
−.09 (−.17, −.03) |
−.07 (−.15, −.02) |
−.07 (−.16, −.02) |
| Sleep Self-Efficacy | .01 (−.01, .07) |
.01 (−.01, .06) |
.02 (−.02, .07) |
| Dysfunctional Beliefs and Attitudes about Sleep |
−.39 (−.56, −.23) |
−.19 (−.34, −.05) |
−.22 (−.44, .01) |
Note. The direct effects of Condition on Insomnia Severity, Sleep Onset Latency, and Wake After Sleep Onset at post-12 assessment were no longer significant when Dysfunctional Beliefs and Attitudes about Sleep post was entered, suggesting full mediation.
For within-group analyses, a series of linear regression analyses were computed. In each analysis, post residual scores for cognitive variables and baseline scores for sleep outcome variables were entered as simultaneous predictors on a single step, testing whether changes in cognitive variables were significantly associated with sleep outcomes at the post 12-month assessment, after taking into account baseline level of sleep outcome variables. Finally, to examine which of the cognitive variables would most strongly predict post 12-month sleep outcomes in each condition, all residualized cognitive variables were entered simultaneously as predictors in the same models, along with baseline scores for sleep outcome variables. For all regression analyses, the Variance Inflation Factor (VIF; a widely used metric to assess multicollinearity) in the current analyses were all less than 5, well below the widely recommended cutoff of 10 (e.g., Hair, Anderson, Tatham, & Black, 1998; O’Brien, 2007). Results for post and post-6 month sleep outcomes can be found in the online supplemental material.
3. Results
3.1. Impact of SHUTi versus Patient Education on Cognitive Variables
Results from ANOVAs revealed significant main effects for Time for Insomnia Knowledge (F(1, 273)=1255.42, p<.01, η2 =.82), Chance Sleep Locus of Control (F(1, 271)=35.20, p<.01, η2 =.12), Internal Sleep Locus of Control (F(1, 271)=68.21, p<.01, η2 =.20), Sleep Self-efficacy (F(1, 272)=12.59, p<.01, η2 =.04), and Dysfunctional Attitudes and Beliefs about Sleep (F(1, 273)=179.54, p<.01, η2 =.40). As seen in Table 1, although there were no significant group differences in these cognitive variables at baseline, there were significant (at p<.05) Group x Time interactions for Insomnia Knowledge, Chance Sleep Locus, and Dysfunctional Beliefs and Attitudes about Sleep. Further, those who received SHUTi had, at post-assessment, significantly higher levels of Insomnia Knowledge (t(273)=7.99, p<.01, 95% CI=.10-.16) and Internal Sleep Locus (t(271)=2.26, p=.03, 95% CI=.04-.55), and significantly lower levels of Chance Sleep Locus (t(271)=3.02, p<.01, 95% CI=.15-.71) and Dysfunctional Beliefs and Attitudes about Sleep (t(273)=8.88, p<.01, 95% CI=1.52-2.39), than did those in the online patient education condition. There was no significant difference between groups in Sleep Self-efficacy at post-assessment (t(272)=.81, p=.39, 95% CI=−.21-.54). Taken together, the pattern of results indicates that those in the SHUTi condition experienced greater changes in sleep-related cognitive variables than did those in the online patient education condition.2
Table 1.
Statistics from Group x Time interactions, descriptive statistics (mean, standard deviation), and percent above RCI threshold, for SHUTi and online patient education groups (shaded cells indicate a significant difference between groups at post, at p<.05).
| Baseline | Post | % above RCI | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| F(1, 273) | η2 | SHUTi | Pt. Ed. | SHUTi | Pt. Ed. | SHUTi | Pt. Ed. | |
| Insomnia Knowledge | 24.75** | .08 | .28 (.13) | .30 (.14) | .88 (.13) | .74 (.15) | 94 | 82 |
| Sleep Locus of Control- Internal | 3.32t | .01 | 3.05 (.99) | 2.98 (1.05) | 3.67 (1.02) | 3.37 (1.14) | 26 | 18 |
| Sleep Locus of Control-Chance | 9.51** | .03 | 3.11 (1.0) | 3.10 (1.19) | 2.53 (1.09) | 2.96 (1.26) | 11 | 4 |
| Sleep Self-Efficacy | .33 | .001 | 8.22 (1.43) | 8.29 (1.34) | 7.86 (1.52) | 8.02 (1.65) | 11 | 8 |
| Dysfunctional Beliefs and | 93.51** | .26 | 6.05 (1.46) | 6.22 (1.56) | 3.89 (1.88) | 5.84 (1.77) | 56 | 15 |
| Attitudes about Sleep | ||||||||
| Insomnia Severity | 60.28** | .18 | 17.03 (4.01) | 17.80 (4.05) | 9.33 (5.48) | 14.68 (5.48) | 62 | 23 |
| Sleep Onset Latency | 15.61** | .06 | 3.52 (.83) | 3.72 (.75) | 2.90 (.83) | 3.41 (.85) | ||
| Wake After Sleep Onset | 30.69** | .11 | 4.20 (.71) | 4.27 (.69) | 3.31 (.96) | 3.95 (.79) | ||
p<.01
p=.07
Note. Pt. Ed.=Patient education condition; % above RCI=Percentage of individuals in each condition who experienced a meaningful and reliable change from pre-intervention to post-intervention, based on the RCI for that measure. RCI’s were not calculated for sleep onset latency and wake after sleep onset because those scores were based a single item scale.
As seen in Table 1, SHUTi (vs. online patient education) had significantly more participants who showed reliable increases in Insomnia Knowledge (z=2.96, p<.01), and reductions in Chance Sleep Locus of Control (z=2.29, p=.02) and Dysfunctional Beliefs and Attitudes about Sleep (z=7.23, p<.01). There were no significant group differences in the reliable change indices for Internal Sleep Locus of Control (z=1.46, p=.15) or Sleep Self-efficacy (z=1.0, p=.32).
3.2. Cognitive Variables Mediating Primary Sleep Outcomes at Post 12-Month Assessment
Indirect effects from all mediational models can be found in Table 2, and standardized regression coefficients are displayed in Figure 2. As seen in Table 2, with the exception of Sleep Self-efficacy and Internal Sleep Locus of Control, each cognitive variable mediated the link between condition and at least one post 12-month sleep outcome. Dysfunctional Beliefs and Attitudes about Sleep mediated the links between Condition and Insomnia Severity and Sleep Onset Latency. Chance Sleep Locus of Control was the only variable to mediate the link between Condition and each of the three post 12-month sleep outcomes. As seen in Figure 2, with the exceptions of Sleep Self-Efficacy and Internal Sleep Locus of Control, Condition predicted changes in at least one post 12-month sleep outcome through every cognitive factor. Combined with results from Table 1, compared to the patient education condition, the pattern of results indicate that SHUTi led to sustained changes in sleep outcomes through significant increases in Insomnia Knowledge, and significant decreases in Chance Sleep Locus and Dysfunctional Beliefs and Attitudes about Sleep.
Figure 2.
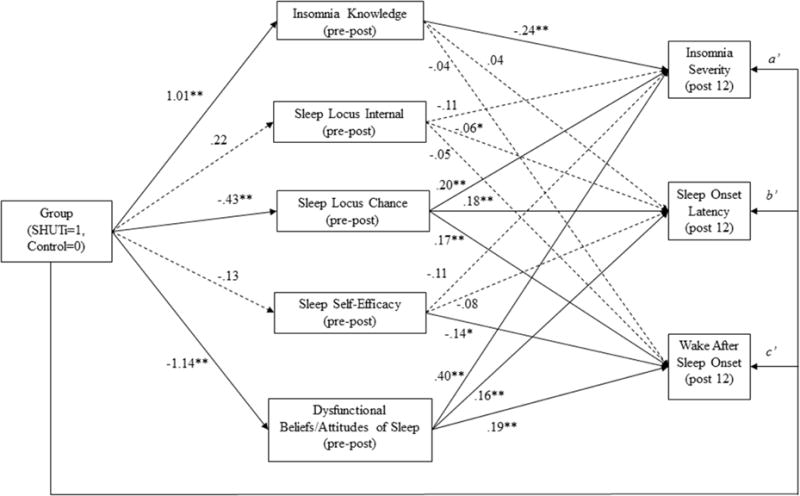
Standardized coefficients from separate mediation models (sleep outcome at baseline was entered as a covariate in all models tested).
**p<.01, *p<.05
Note: In all models, the direct effect of group on sleep outcomes were significant (p<.05), except when dysfunctional beliefs and attitudes about sleep was entered as the mediator.
Because the results above are based on separate analyses examining individual mediators, residual post scores for all cognitive variables were simultaneously entered into a single model for each post 12-month sleep outcome to examine their comparative strength. This allowed for examination of which cognitive variable(s) might be the strongest mediators between condition and long-term sleep outcomes. Insomnia Knowledge (standardized coefficient of indirect effect=−.15, 95% CI=−.29 to −.02), Chance Sleep Locus of Control (indirect effect=−.05, 95% CI=−.13 to −.004), and Dysfunctional Beliefs and Attitudes about Sleep (indirect effect=−.27, 95% CI=−.46 to −.10) all significantly mediated the link between Condition and Insomnia Severity. Chance Sleep Locus of Control (indirect effect=−.05, 95% CI=−.13 to −.01), and Dysfunctional Beliefs and Attitudes about Sleep (indirect effect=−.16, 95% CI=−.31 to −.02) significantly mediated the link between Condition and Sleep Onset Latency. Lastly, Chance Sleep Locus of Control (indirect effect=−.05, 95% CI=−.15 to −.001) significantly mediated the link between Condition and Wake After Sleep Onset. Taken together, these results indicate that Chance Sleep Locus of Control and Dysfunctional Beliefs and Attitudes about Sleep are the strongest mediators of sleep outcome among the five cognitive variables examined in the current study.
The link between Condition and 12-month post Chance Sleep Locus of Control was significantly mediated by Insomnia Severity at post (indirect effect=−.16, 95% CI=−.30 to −.05), but not Sleep Onset Latency (indirect effect=−.06, 95% CI=−.15 to .02) or Wake After Sleep Onset (indirect effect=−.06, 95% CI=−.17 to .05). Further, the link between Condition and 12-month post Dysfunctional Beliefs and Attitudes about Sleep was significantly mediated by Insomnia Severity at post (indirect effect=−.31, 95% CI=−.47 to −.20) and Sleep Onset Latency (indirect effect=−.08, 95% CI=−.20 to −.01), but not Wake After Sleep Onset (indirect effect=−.10, 95% CI=−.24 to .03). Overall, these results indicate that better sleep, and in particular reduced insomnia severity, leads to lower levels of Chance Sleep Locus of Control and Dysfunctional Beliefs and Attitudes about Sleep 1 year later. When taking into account results of cognitive variables as mediators, these results provide some evidence that the relationship between better sleep and decreases in maladaptive attitudes and beliefs about sleep may be bidirectional.
3.3. Impact of Cognitive Variables in Predicting Post 12-Month Sleep Outcomes within Condition
Analyses also focused on determining whether changes in cognitive factors predicted long-term changes to sleep outcomes, separately within each condition. As seen in Table 3, Chance Sleep Locus of Control, Sleep Self-Efficacy and Dysfunctional Beliefs and Attitudes about Sleep significantly predicted all sleep outcomes, whereas this was not the case for the patient education group. Further, changes in all cognitive variables significantly predicted Insomnia Severity within the SHUTi condition (with the exception of Internal Sleep Locus of Control). In the patient education condition, no cognitive variables were a consistent predictor of sleep outcomes. Taken together, results indicate that changes in cognitive variables played an important role in sustained sleep outcomes in the SHUTi condition.
Table 3.
Standardized regression coefficients (with 95% confidence intervals) of residualized cognitive variables predicting sleep variables at post 12-month assessment for the SHUTi and patient education groups.
| SHUTi | Patient Education | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Insomnia Severity | Sleep Onset Latency | Wake After Sleep Onset | Insomnia Severity | Sleep Onset Latency | Wake After Sleep Onset | ||||||
| Insomnia Knowledge | −.31** (−.48, −.15) |
−.04 (−.18, .10) |
−.14 (−.33, −.03) |
−.13 (−.34, .03) |
.12 (−.04, .32) |
.07 (−.10, .25) |
|||||
| Sleep Locus Internal | −.04 (−.20, −.12) |
−.02 (−.15, .12) |
.09 (−.09, .25) |
−.18* (−.32, −.01) |
−.10 (−.25, .05) |
−.16* (−.30, −.01) |
|||||
| Sleep Locus Chance | .28** (.11, .42) |
.20** (.06, .33) |
.25** (.09, .42) |
.14 (−.02, .29) |
.16* (.02, .32) |
.11 (−.04, .26) |
|||||
| Sleep Self-Efficacy | −.21* (−.35, −.04) |
−.16* (−.28, −.02) |
−.26** (−.41, −.09) |
−.04 (−.20, .13) |
−.02 (−.17, .13) |
−.06 (−.20, .09) |
|||||
| Dysfunctional Beliefs and Attitudes about Sleep | .45** (.29, .58) |
.19** (.05, .32) |
.28** (.11, .45) |
.17 (−.002, .31) |
.10 (−.04, .25) |
.01 (−.13, .15) |
|||||
p<.01
p<.05
Note. Residualized post-assessment scores reflected post-assessment cognitive variable scores of which baseline scores were partialed out.
All cognitive variables were entered into a single regression model for each post 12-month sleep outcome. When all cognitive variables were simultaneously entered into the same model, Dysfunctional Beliefs and Attitudes about Sleep predicted Insomnia Severity at post-assessment for the SHUTi condition only (β=.36, p<.01, 95% CI=.17 to .56), whereas Internal Sleep Locus of Control predicted Insomnia Severity in the online patient education condition (β=−.21, p=.01, 95% CI=−.34 to −.04). No cognitive variables significantly predicted the post 12-month outcome of Sleep Onset Latency for either condition. Finally, no cognitive variables were significant predictors for the outcome of post 12-month Wake After Sleep Onset in the patient education condition, whereas Dysfunctional Beliefs and Attitudes about Sleep significantly predicted Wake After Sleep Onset in the SHUTi condition (β=.22, p=.03, 95% CI=.02 to .45).
4. Discussion
Overall, this investigation found evidence that the efficacy of SHUTi on long-term sleep outcomes is related to changing underlying cognitive variables. Specifically, SHUTi was more effective than patient education in increasing insomnia knowledge and decreasing chance sleep locus of control and dysfunctional beliefs and attitudes about sleep, a pattern supported by the RCI analyses. Further, changes in insomnia knowledge, chance sleep locus of control, and dysfunctional beliefs and attitudes about sleep were all significant mediators between condition (SHUTi vs. patient education) and changes in at least one post 12-month sleep outcome. Finally, within the SHUTi condition, changes in each cognitive variable predicted change in at least one sleep outcome at post 12-month intervention (except internal sleep locus of control). Taken together, the present research indicates that the impact of SHUTi in sustaining attenuated insomnia symptoms is, at least partially, due to changing underlying cognitive factors associated with sleep.
The present study contributes to understanding mechanisms in online CBT-I, as well as CBT-I more generally. Relative to the amount of research demonstrating the efficacy of CBT-I in reducing insomnia symptoms, less research has directly examined the putative mechanisms involved (Schwartz & Carney, 2012), particularly as it relates to long-term sleep outcomes. The current findings indicate that targeting insomnia knowledge, chance sleep locus of control, and dysfunctional beliefs and attitudes about sleep may be particularly important in changing insomnia severity over the long-term, whereas decreasing chance sleep locus of control and dysfunctional beliefs and attitudes about sleep may be most relevant to addressing sleep onset latency and wake after sleep onset. For example, results for chance sleep locus of control indicate the importance of discussing personal sense of control over sleep and correcting the misconception that healthy sleep is out of one’s control. This is consistent with many behavioral medicine interventions that highlight the importance of sense of control in achieving better health (Mystakidou, Tsilika, Parpa, & Galanos, 2015; Nuccitelli et al., 2017). Further, there is very little knowledge regarding what components of CBT-I are best delivered in-person or via an Internet intervention. For example, anecdotal accounts from behavioral sleep clinicians may cast doubt on delivering cognitive components of CBT-I via the Internet, due to the potential nuances of cognitive restructuring. Findings from the current study suggest that online CBT-I can be used to change sleep-related cognitions, although future work should deconstruct online CBT-I by examining the independent effects of its treatment components.
When all cognitive variables were entered in the same model, evidence supported the importance of chance sleep locus of control and dysfunctional beliefs and attitudes about sleep in mediating the link between condition and sleep outcomes, and dysfunctional beliefs and attitudes about sleep seemed particularly important in the SHUTi condition at post 12-month assessment. These findings are consistent with previous research finding that CBT-I has a particularly strong effect on beliefs about sleep (Eidelman et al., 2016). Sleep-related beliefs are a core component of many insomnia models (e.g., Harvey, 2002, 2005), and the current investigation extends existing work (Harvey et al., 2014) by identifying those cognitive variables most relevant to sustained sleep improvements, which may assist in developing treatments that are best suited to addressing a client’s needs. For chance sleep locus of control and dysfunctional beliefs and attitudes about sleep, it may be that being high in these variables generally translates into having maladaptive beliefs and attitudes that obstruct healthy sleep patterns. In contrast, being high in insomnia knowledge, internal sleep locus of control, and sleep self-efficacy generally translates into a strong sense of agency, although none of these variables was a consistent mediator between condition and sleep outcomes. Thus, one way to interpret these findings is that it may be more important to decrease people’s negative beliefs and attitudes about sleep, than it is to increase their sense of agency. This interpretation is consistent with cognitive models of insomnia that highlight the role of unhelpful thoughts and beliefs in perpetuating unhealthy sleep behaviors (e.g., Espie et al., 2006; Harvey, 2005). Finally, there was some evidence that CBT-I decreased insomnia severity, which in turn decreased chance sleep locus of control and dysfunctional beliefs and attitudes about sleep. Given the importance of sleep to cognitive processes, this finding was not surprising although future work may wish to continue to investigate the impact of sleep quality on beliefs and attitudes.
Insomnia is a worldwide epidemic that leads to both occupational and health impairment (e.g., Daley et al., 2009; Mallon et al., 2005), and online CBT-I is ideally suited to addressing this issue on a population level. The robust pattern of findings demonstrating the long-term utility of SHUTi supports the notion that, if scaled for mass consumption, online CBT-I programs can provide long-term benefit to those suffering from insomnia by restructuring preexisting thinking patterns about sleep. One advantage of online CBT-I programs is that they can be tailored to a patient’s individual needs, and one component of tailored care may be to assess underlying cognitive factors that impede healthy sleep patterns. For example, knowing that a particular patient has a high level of chance sleep locus of control may lead to a higher dose of cognitive restructuring exercises that target the belief that overcoming insomnia is out of one’s control.
In addition to those already mentioned, there were some limitations of the present investigation. Because the present investigation did not differentiate between cognitive and behavioral components of CBT-I (e.g., Harvey et al., 2014), it is difficult to know which precise components were responsible for changes in cognitive variables associated with sleep. Future work may wish to randomly assign participants to receive either cognitive or behavioral aspects of CBT-I, which could enhance efforts to tailor interventions to a patient’s unique symptoms. Another limitation is that changes in cognitive variables and sleep outcomes were based on patient self-report, allowing for the possibility of common method variance in influencing findings. Future work should demonstrate that changes in underlying cognitive variables are associated with changes in actual behavior to corroborate self-report data, perhaps determined from passive data collection using mobile devices (that can be used to assess sleep quality, movement in bed, etc.) as well as ecological momentary assessments (e.g., assessing fatigue throughout the day and readiness for sleep during evening hours). Future work should also examine whether changes in sleep-related cognitions are an epiphenomenon of sleeping better, by including more assessments during the intervention phase. Finally, given that insomnia is associated with multiple mental health issues such as anxiety disorders, it is possible that psychiatric comorbidity influenced the current findings. For example, individuals high in anxiety may be more resistant to cognitive restructuring of sleep variables although not much is known about this topic. Because participants were assigned randomly to SHUTi versus patient education conditions, this is less of a concern. A topic for future research to examine is the efficacy of online CBT-I in reducing symptoms among comorbid psychiatric populations.
5. Conclusion
In sum, the present research demonstrates the long-term efficacy of an online CBT-I program in reducing insomnia by changing underlying cognitive variables. Findings from the present research enhance understanding of mechanisms in online CBT-I, with potential implications for broader models of internet interventions. Together, the findings suggest valuable directions for future research to determine whether interventions that target specific underlying cognitive factors may be needed to address sustained sleep outcomes.
Supplementary Material
Highlights.
Examined cognitive variables in the long-term efficacy of online CBT for insomnia
Compared online CBT-I to an online patient education condition
Those who received online CBT-I had greater changes to cognitive factors in sleep
Cognitive variables mediated the link between Condition and 12-month sleep outcomes
In CBT-I condition, changes in cognitive variables predicted 12-month sleep outcomes
Acknowledgments
This research was supported by a grant (R01MH86758) from the National Institute of Mental Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Pattern of results is identical when not using residual scores, and baseline cognitive variables are entered as a covariate in the ANOVA models.
Primary sleep outcomes are reported in Ritterband et al. (2017). Raw values and effects from ANOVA can be found in Table 1. RCI for insomnia severity was 6.53 and significantly more participants in the SHUTi condition showed a reliable decrease in insomnia severity than in the patient education condition (z=6.60, p<.01).
References
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, Riemann D. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy. John Wiley & Sons, Inc; 1994. [Google Scholar]
- Bandura A. Guide for constructing self-efficacy scales. Self-efficacy Beliefs of Adolescents. 2006;5:307–337. [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Stine R. Direct and indirect effects: Classical and bootstrap estimates of variability. Sociological Methodology. 1990;20:15–140. [Google Scholar]
- Buysse DJ, Ancoli-lsrael S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep: Journal of Sleep and Sleep Disorders Research. 2006;29:1155–1173. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, Morin CM. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35:287–302. doi: 10.5665/sleep.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Batterham PJ, Gosling JA, Ritterband LM, Griffiths KM, Thorndike FP, Glozier N, O'Dea B, Hickie IB, Mackinnon AJ. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): A randomised controlled trial. The Lancet Psychiatry. 2016;3:333–341. doi: 10.1016/S2215-0366(15)00536-2. [DOI] [PubMed] [Google Scholar]
- Daley M, Morin CM, LeBlanc M, Gregoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32:55–64. [PMC free article] [PubMed] [Google Scholar]
- Edinger JD, Fins AI, Glenn DM, Sullivan RJ, Jr, Bastian LA, Marsh GR, Daily D, Shaw E, Vasilas D. Insomnia and the eye of the beholder: are there clinical markers of objective sleep disturbances among adults with and without insomnia complaints? Journal of Consulting and Clinical Psychology. 2000;68:586–593. [PubMed] [Google Scholar]
- Eidelman P, Talbot L, Ivers H, Bélanger L, Morin CM, Harvey AG. Change in Dysfunctional Beliefs About Sleep in Behavior Therapy, Cognitive Therapy, and Cognitive-Behavioral Therapy for Insomnia. Behavior Therapy. 2016;47:102–115. doi: 10.1016/j.beth.2015.10.002. [DOI] [PubMed] [Google Scholar]
- Espie CA, Broomfield NM, MacMahon KM, Macphee LM, Taylor LM. The attention–intention–effort pathway in the development of psychophysiologic insomnia: a theoretical review. Sleep Medicine Reviews. 2006;10:215–245. doi: 10.1016/j.smrv.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Espie CA, Kyle SD, Williams C, Ong JC, Douglas NJ, Hames P, Brown JS. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35:769–781. doi: 10.5665/sleep.1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Mendoza J, Vgontzas AN. Insomnia and its impact on physical and mental health. Current Psychiatry Reports. 2013;15:418. doi: 10.1007/s11920-013-0418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S. Health Information is a Popular Pursuit Online. 2011 Feb; Retrieved from http://www.pewinternet.org/2011/02/01/health-information-is-a-popular-pursuit-online/
- Hair J, Anderson R, Tatham R, Black W. Multivariate data analysis. Upper Saddle River, NJ: Prentice Hall; 1998. [Google Scholar]
- Harvey AG. A cognitive model of insomnia. Behaviour Research and Therapy. 2002;40:869–893. doi: 10.1016/s0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- Harvey AG. A cognitive theory and therapy for chronic insomnia. Journal of Cognitive Psychotherapy. 2005;19:41–59. [Google Scholar]
- Harvey AG, Bélanger L, Talbot L, Eidelman P, Beaulieu-Bonneau S, Fortier-Brochu É, Ivers H, Lamy M, Hein K, Soehner AM, Mérette C. Comparative efficacy of behavior therapy, cognitive therapy, and cognitive behavior therapy for chronic insomnia: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82:670–683. doi: 10.1037/a0036606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jungquist CR, O’Brien C, Matteson-Rusby S, Smith MT, Pigeon WR, Xia Y, Lu N, Perlis ML. The efficacy of cognitive-behavioral therapy for insomnia in patients with chronic pain. Sleep Medicine. 2010;11:302–309. doi: 10.1016/j.sleep.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan KA, Talbot LS, Harvey AG. Cognitive mechanisms in chronic insomnia: Processes and prospects. Sleep Medicine Clinics. 2009;4:541–548. [Google Scholar]
- Lancee J, Eisma MC, van Straten A, Kamphuis JH. Sleep-related safety behaviors and dysfunctional beliefs mediate the efficacy of online CBT for insomnia: A randomized controlled trial. Cognitive Behaviour Therapy. 2015;44:406–422. doi: 10.1080/16506073.2015.1026386. [DOI] [PubMed] [Google Scholar]
- Mallon L, Broman JE, Hetta J. High Incidence of Diabetes in Men with Sleep Complaints or Short Sleep Duration: A 12-year follow-up study of a middle-aged population. Diabetes Care. 2005;28:2762–2767. doi: 10.2337/diacare.28.11.2762. [DOI] [PubMed] [Google Scholar]
- Morin CM. Insomnia: Psychological assessment and management. New York: The Guilford Press; 1993. [Google Scholar]
- Morin CM, Blais F, Savard J. Are changes in beliefs and attitudes about sleep related to sleep improvements in the treatment of insomnia? Behaviour Research and Therapy. 2002;40:741–752. doi: 10.1016/s0005-7967(01)00055-9. [DOI] [PubMed] [Google Scholar]
- Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin CM, Vallières A, Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS-16): Validation of a brief version (DBAS-16) Sleep. 2007;30:1547–1554. doi: 10.1093/sleep/30.11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mystakidou K, Tsilika E, Parpa E, Galanos A. The influence of sense of control and cognitive functioning in older cancer patients' depression. Psycho-Oncology. 2015;24:311–317. doi: 10.1002/pon.3642. [DOI] [PubMed] [Google Scholar]
- Nuccitelli C, Valentini A, Caletti MT, Caselli C, Mazzella N, Forlani G, Marchesini G. Sense of coherence, self-esteem, and health locus of control in subjects with type 1 diabetes mellitus with/without satisfactory metabolic control. Journal of Endocrinological Investigation. 2017:1–8. doi: 10.1007/s40618-017-0741-8. [DOI] [PubMed] [Google Scholar]
- O’brien RM. A caution regarding rules of thumb for variance inflation factors. Quality & Quantity. 2007;41:673–690. [Google Scholar]
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Medicine Reviews. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, Gonder-Frederick LA. A behavior change model for internet interventions. Annals of Behavioral Medicine. 2009;38:18–27. doi: 10.1007/s12160-009-9133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Thorndike FP, Gonder-Frederick LA, Magee JC, Bailey ET, Saylor DK, Morin CM. Efficacy of an Internet-based behavioral intervention for adults with insomnia. Archives of General Psychiatry. 2009;66:692–698. doi: 10.1001/archgenpsychiatry.2009.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Thorndike FP, Ingersoll KS, Lord HR, Gonder-Frederick L, Frederick C, Quigg MS, Cohn WF, Morin CM. Effect of a Web-Based Cognitive Behavior Therapy for Insomnia Intervention With 1-Year Follow-up: A Randomized Clinical Trial. Jama Psychiatry. 2017;74:68–75. doi: 10.1001/jamapsychiatry.2016.3249. [DOI] [PubMed] [Google Scholar]
- Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General & Applied. 1966;80:1–28. [PubMed] [Google Scholar]
- Schwartz DR, Carney CE. Mediators of cognitive-behavioral therapy for insomnia: a review of randomized controlled trials and secondary analysis studies. Clinical Psychology Review. 2012;32:664–675. doi: 10.1016/j.cpr.2012.06.006. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–1464. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- Thorndike FP, Saylor DK, Bailey ET, Gonder-Frederick L, Morin CM, Ritterband LM. Development and perceived utility and impact of an Internet intervention for insomnia. E-journal of Applied Psychology: Clinical and Social Issues. 2008;4:32–42. doi: 10.7790/ejap.v4i2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent N, Sande G, Read C, Giannuzzi T. Sleep locus of control: Report on a new scale. Behavioral Sleep Medicine. 2004;2:79–93. doi: 10.1207/s15402010bsm0202_1. [DOI] [PubMed] [Google Scholar]
- Vincent N, Walsh K, Lewycky S. Sleep locus of control and computerized cognitive-behavioral therapy (cCBT) Behaviour Research and Therapy. 2010;48:779–783. doi: 10.1016/j.brat.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia–A systematic review and meta-analysis of randomized controlled trials. Sleep Medicine Reviews. 2016;30:1–10. doi: 10.1016/j.smrv.2015.10.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


