Abstract
Objective
First, to compare QOL and illness perceptions between patients with a Fontan circulation and patients with anatomically simple defects (i.e., atrial septal defects [ASD] or ventricular septal defects [VSD]). Second, to explore illness perceptions as a mediator of the association between congenital heart disease (CHD) diagnosis and QOL.
Design
Cross-sectional observational study
Setting
24 cardiology centers from 15 countries across five continents
Patients
435 adult patients with congenital heart disease (177 Fontan and 258 ASD/VSD) ages 18-83 years
Outcome Measures
QOL and illness perceptions were assessed by the Satisfaction With Life Scale and the Brief Illness Perceptions Questionnaire, respectively.
Results
Patients with a Fontan circulation reported lower QOL (Wald Z=-3.59, p=<.001) and more negative perceptions of their CHD (Wald Z=-7.66, p<.001) compared to patients with ASD/VSD. After controlling for demographics, anxiety, depressive symptoms, and NYHA functional class, path analyses revealed a significant mediation model, αβ=.15, p=.002, 95% CI=.06-.25, such that CHD diagnosis was indirectly related to QOL through illness perceptions.
Conclusions
The Fontan sample's more negative perceptions of CHD were likely a reflection of life with a more complex defect. Illness perceptions appear to account for unique differences in QOL between groups of varying CHD complexity Psychosocial screening and interventions may be important treatment components for patients with CHD, particularly those with Fontan circulations.
Keywords: congenital heart disease, Fontan circulation, quality of life, illness perceptions
Introduction
The Fontan circulation procedure has provided lifesaving palliation for individuals born with single ventricle physiology, with survival outcomes of 76% at 25 years of age [1]. However, adverse medical outcomes (e.g., liver dysfunction, heart failure, arrhythmia, hemodynamic abnormalities) [2-5] and functional limitations (e.g., exercise intolerance, employment restrictions) [6, 7] have been well documented. In recognition of the potential challenges of living with a Fontan circulation, there has been increasing attention in recent years to patient-reported outcomes, including quality of life (QOL). Research regarding QOL among Fontan patients has produced mixed results (depending on sample characteristics and QOL definitions), with some studies reporting lower levels of QOL relative to healthy controls [4, 8] and others finding no differences [9, 10]. However, most studies suggest that average QOL is relatively high in this population despite the medical outcomes and functional complications of life with a Fontan circulation [6, 7, 9, 11]. Still, it is imperative to recognize the variability in QOL within this population [4, 6, 10]. Approximately 26% of patients in one study reported dissatisfaction with their lives [7], and 42% of young adults in another investigation endorsed total QOL scores in the impaired range [8]. Thus, while Fontan patients on average tend to report relatively good QOL, there is a substantial subset of patients who experience suboptimal outcomes. It is imperative to identify patient characteristics that explain this variability so appropriate treatment can be provided.
Illness perceptions, namely the beliefs patients have about their disease [12], may explain some of the variability in QOL. Illness perceptions provide a framework for managing and coping with chronic health issues; examples include personal control over the illness, perceived treatment benefits, and effect of the illness on emotional functioning [13]. The link between negative illness perception scores and lower QOL has previously been demonstrated in congenital heart disease (CHD) [11, 14, 15], but not specifically within the Fontan population. Illness perceptions may be of particular significance for Fontan patients because individuals with more complex defects, including single ventricle physiology, tend to endorse beliefs of more severe health consequences, have a poorer understanding of their illness, and report more negative emotions [14]. While these perceptions may be considered more “negative” in comparison with those of patients with less complex defects, they likely are an appropriate reflection of the experiences of living with a complex heart defect [14].
Although illness perceptions have been found to mediate the association between condition complexity and QOL outcomes in patients with acquired heart disease [16], there have been no comparable mediational studies in CHD. Identification of mechanisms that affect QOL is necessary to develop and implement interventions that target QOL improvements. Further, it is helpful to understand the Fontan experience relative to patients with other, less complex defects, such as atrial septal defects (ASD) and ventricular septal defects (VSD).
In the present study, we examined QOL and illness perceptions in a multinational sample of Fontan patients relative to patients with simple CHD (ASD or VSD). Patients with isolated ASD/VSD were chosen as a comparison sample in order to limit heterogeneity and provide a clear contrast in complexity between the two samples. In addition, we examined illness perceptions as a mediator between CHD diagnosis (Fontan vs. ASD/VSD) and QOL. We hypothesized the following: (i) Fontan patients would report lower QOL and more negative illness perception scores relative to ASD/VSD patients, and (ii) after controlling for established correlates (e.g., demographics, depressive symptoms, anxiety, and NYHA functional class [11, 17], illness perceptions would mediate the association between CHD diagnosis and QOL.
Methods
Population
Participants were recruited from 24 centers across 15 countries (Argentina, Australia, Belgium, Canada, France, India, Italy, Japan, Malta, Norway, Taiwan, the Netherlands, Sweden, Switzerland, and United States of America) participating in Assessment of Patterns of Patient-Reported Outcomes in Adults with Congenital Heart disease – International Study (APPROACH-IS) [18]. APPROACH-IS is a cross-sectional, multinational study investigating patient-reported outcomes and cultural/geographic differences in adults with CHD. Participants were required to meet the following inclusion criteria: (i) diagnosis of CHD, (ii) 18 years of age or older; (iii) diagnosis established before the age of 10 years, (iv) continued follow-up at a CHD center or included in a national/regional registry; and (v) physical, cognitive, and language capabilities required to complete assessment measures. Exclusion criteria included previous heart transplantation, diagnosis of primary pulmonary hypertension, and significant cognitive impairment. All participants with Fontan circulations, ASD, or VSD were included in the present study.
Procedures
The APPROACH-IS study design and data collection procedures were previously reported by Apers and colleagues [18]. Prior to data collection, APPROACH-IS was approved by the ethics committee of the University Hospitals Leuven/KU Leuven (coordinating center) as well as the ethics review boards of each participating center; therefore, the protocol is in line with ethical guidelines established by the 1975 Declaration of Helsinki. Informed consent was obtained from all participants.
Measures
Demographics
Patient demographic information was obtained by a background questionnaire focused on socio-demographic variables. Additional demographic and medical data (e.g., diagnosis, medical history) were gathered by medical chart review.
Primary study variables
QOL was defined as “the degree of overall life satisfaction that is positively or negatively influenced by individuals' perception of certain aspects of life important to them, including matters both related and unrelated to health” [19]. According to this definition, QOL was measured as a continuous variable using the 5-item Satisfaction With Life Scale (SWLS) [20]. Items capture global life satisfaction and are scored on a 5-point Likert-type scale (e.g., 1 - strongly disagree to 7 - strongly agree). Higher scores indicate greater QOL. Internal consistency in the present study was excellent (Cronbach's α=.87).
Illness perceptions were assessed by the Brief Illness Perception Questionnaire (Brief IPQ) [13]. The nine-item Brief IPQ has demonstrated strong psychometric properties [13]. Items are rated from 0 to 10 and assess illness consequences, experience of symptoms (“identity”), expected duration of illness (“timeline”), personal control, belief of treatment effectiveness (“treatment control”), concern, understanding of one's illness, and experience of distressing emotions (“emotional response”). An item measuring perceived causal factors of illness was not included in the larger study because it is not relevant to CHD. Although the measure was initially validated at the item-level [13] and utilized as such in CHD research [14, 15], cardiac researchers have also used a composite illness perceptions total score [16]. The total score was used to test each hypothesis while exploratory analyses utilized item-level data. Higher values indicate more positive illness perceptions. After reverse-scoring six items, items were averaged to compute a total score (Cronbach's α=.64).
Covariates
Symptoms of depression and anxiety were assessed by the Hospital Anxiety and Depression Scale (HADS) [21]. The questionnaire yields two 7-item subscales for anxiety and depressive symptoms, with each scale ranging from 0 to 21; a score ≥ 8 indicates clinically significant symptoms. Internal consistency for the anxiety and depression subscales in this study were Cronbach's α=.82 and .78, respectively.
Participants provided self-report of their NYHA functional class by answering one item asking them to rate their physical limitations on a 4-point scale ranging from I (no limitations during physical activities) to 4 (unable to be physically active without experiencing physical discomfort).
Statistical Methods
Descriptive statistics and bivariate correlations were conducted to provide additional information about study variables. One-way analyses of covariance (ANCOVAs) examined differences in QOL and illness perceptions between Fontan patients versus those with ASD/VSD. Age, sex, and country of residence were included as covariates due to significant group differences as well as existing evidence-based associations with QOL [17, 19]. Analyses were conducted in Mplus [22] to appropriately manage both missing data and non-normal data. Exploratory analyses included examination of item-level differences in illness perceptions between the two samples. All a priori pairwise comparisons (i.e., comparing samples on each IPQ item) with covariates were run using a multi-group function in Mplus. A false discovery rate (FDR) [23] Type I error control was utilized for all pairwise illness perception comparisons.
Analyses testing whether illness perceptions mediated the association between CHD diagnosis and QOL were also run in MPlus. In addition to demographic covariates, NYHA functional status, and anxiety and depressive symptoms were included as covariates due to previously demonstrated associations with QOL and illness perceptions [11, 17]. Direct and indirect (i.e., mediated) effects were assessed by evaluation of 95% confidence intervals produced by bootstrapping (bootstrapping = 1000). Model fit was assessed using four indicators: χ2, standardized root mean square residual (SRMR), comparative fit index (CFI), and root mean square error of approximation (RMSEA). Following identification of the mediated effect, age and sex were examined as moderators of the mediation model. Country of residence was not examined as a moderator due to small sample sizes within some countries. Missing data was handled using maximum likelihood estimate algorithms (i.e., MLR for ANCOVA and pair-wise comparisons; MLE for mediation analyses) in Mplus.
Results
Baseline Characteristics
Four hundred thirty-five patients (177 Fontan and 258 ASD/VSD) across 15 countries were included in the current study. Of participating patients, ages ranged from 18 to 83 years and 68.5% were White/Caucasian, 23.4% were Asian, 2.8% were Hispanic/Latino, 1.4% were Black/African-origin, 1.4% were Middle-eastern/Arabic, and 0.5% identified with an “other” ethnic background. Fontan patients tended to be younger and were more likely to be male, unmarried, and have a greater NYHA functional class. Additional demographics are listed in Table 1.
Table 1. Demographic and Geographic Information for Fontan patients and ASD/VSD patients.
| Fontan (N=177) | ASD/VSD (N=258) | |
|---|---|---|
| Mean (SD) Age (years) | 27.5 (7.6) | 36.8 (14.7) |
| Sex (%Male) | 52.0% | 39.1% |
| Employment Status (%E) | 61.3% | 69.3% |
| Marital Status (%M) | 21.6% | 34.9% |
| Ethnic Background | ||
| White/Caucasian | 118 (67.8%) | 180 (71.4%) |
| Asian | 41 (23.6%) | 61 (24.2%) |
| Hispanic/Latino | 8 (4.6%) | 4 (1.6%) |
| Black/African-origin | 4 (2.3%) | 2 (0.8%) |
| Middle-eastern/Arabic | 3 (1.7%) | 3 (1.2%) |
| Other | 0 (0.0%) | 2 (0.8%) |
| Country | ||
| Argentina | 8 (4.5%) | 5 (1.9%) |
| Australia | 5 (2.8%) | 4 (1.6%) |
| Belgium | 2 (1.1%) | 25 (9.7%) |
| Canada | 18 (10.2%) | 17 (6.6%) |
| France | 16 (9.0%) | 4 (1.6%) |
| India | 21 (11.9%) | 8 (3.1%) |
| Italy | 1 (0.6%) | 11 (4.3%) |
| Japan | 13 (7.3%) | 19 (7.4%) |
| Malta | 4 (2.3%) | 6 (2.3%) |
| Norway | 16 (9.0%) | 2 (0.8%) |
| Sweden | 22 (12.4%) | 53 (20.5%) |
| Switzerland | 2 (1.1%) | 13 (5.0%) |
| Taiwan | 0 (0.0%) | 31 (12.0%) |
| The Netherlands | 1 (0.6%) | 31 (12.0%) |
| USA | 48 (27.1%) | 29 (11.2%) |
| NYHA Functional Class | ||
| I | 46 (26.7%) | 171 (67.9%) |
| II | 81 (47.1%) | 68 (27.0%) |
| III | 31 (18.0%) | 8 (3.2%) |
| IV | 14 (8.1%) | 5 (2.0%) |
Note: ‡ Employment Status (%E) = percent employed with full-time paid work or part-time paid work; Marital Status (%M) = percent married or remarried.
Correlations
Bivariate Pearson and point-biserial correlations are presented in Table 2. Higher QOL was associated with more positive illness perceptions and lower anxiety symptoms, depressive symptoms, and functional class. Total illness perceptions were also inversely correlated with anxiety and depressive symptoms as well as NYHA functional class. Neither age nor sex were significantly associated with either illness perceptions or QOL, although older age was associated with lower anxiety and lower NYHA functional class for the whole sample.
Table 2. Bivariate correlations of study variables.
| Variable | Age | Sex | HADS Anxiety | HADS Depressive Symptoms | NYHA Functional Class | Illness Perceptions-Total | QOL |
|---|---|---|---|---|---|---|---|
| Age | -- | ||||||
| Sex | .05 p=.35 N=435 |
-- | |||||
| HADS Anxiety |
-.16 p=.001 N=433 |
.08 p=.12 N=433 |
-- | ||||
| HADS Depressive Symptoms | -.00 p=.960 N=433 |
-.01 p=.80 N=433 |
.62 p<.001 N=433 |
-- | |||
| NYHA Functional Class |
-.12 p=.014 N=424 |
.03 p=.48 N=424 |
.35 p<.001 N=422 |
.34 p<.001 N=422 |
-- | ||
| Illness Perceptions-Total | .09 p=.051 N=430 |
.01 p=.81 N=430 |
-.54 p<.001 N=430 |
-.43 p<.001 N=430 |
-.53 p<.001 N=420 |
-- | |
| QOL | .06 p=.26 N=423 |
.07 p=.15 N=423 |
-.45 p<.001 N=423 |
-.55 p<.001 N=423 |
-.33 p<.001 N=414 |
.44 p<.001 N=430 |
-- |
Note: Coefficients related to sex represent point-biserial correlations; all other coefficients represent bivariate Pearson correlations.
HADS=Hospital Anxiety and Depression Scale; NYHA=New York Heart Association; QOL=Quality of Life
Hypothesis 1: Group Differences in QOL and Illness Perceptions
ANCOVA results yielded significantly lower QOL in the Fontan group (Range=1.00-7.00, M=4.73, SD=1.40) relative to the ASD/VSD group (Range=1.20-7.00, M=5.16, SD=1.19), Wald Z=-3.59, p<.001. Similarly, Fontan patients reported more negative illness perception scores (Range=1.25-10.00, M=5.21, SD=1.50) compared to patients with ASD/VSD (Range=1.75-10.00, M=6.47, SD=1.56), Wald Z=-7.66, p<001.
Exploratory Analyses: Group Differences in Illness Perceptions
Results from multi-group analyses with covariates are presented in Fig. 1. Following FDR Type-1 error control, 7 of the 8 pairwise comparisons revealed significant differences between Fontan and ASD/VSD patients, with effect sizes ranging from Cohen's d = 0.17 – 1.03. Fontan patients reported greater effects of CHD on their lives, longer expected duration of CHD, greater expected treatment benefits, more CHD symptoms, greater concern about CHD, greater emotional effects, and less control of CHD. Both groups reported similar levels of perceived understanding of their condition.
Fig. 1. Pairwise comparisons with covariates examining differences in illness perceptions between Fontan and ASD/VSD samples.
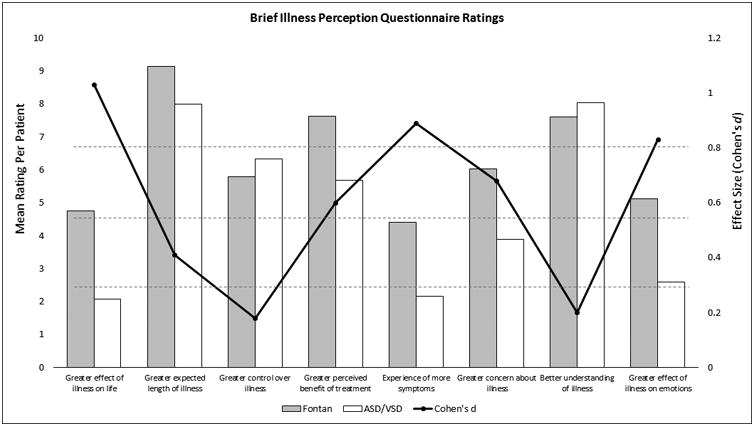
Significant differences were observed for greater effect of illness on life (Wald Z=9.12, p<.001), greater expected length of illness (Wald Z=6.41, p<.001), greater control over illness (Wald Z=-2.03, p=.043), greater perceived benefit of treatment (Wald Z=4.47, p<.001), experience of more symptoms (Wald Z=8.41, p<.001), greater concern about illness (Wald Z=4.53, p<.001) and greater effect of illness on emotions (Wald Z=6.13, p<.001). No significant differences were observed for better understanding of illness (Wald Z=-.75, p=.45).
Note: * indicates p < 0.05; ** indicates p < .01; *** indicates p < .001.
Hypothesis 2: Illness perception mediating the association between CHD group and QOL
For the direct pathways, after controlling for demographics, anxiety and depressive symptoms, and NYHA functional class, CHD diagnosis was significantly associated with illness perceptions (β=.76, p<.001), such that Fontan patients generally endorsed more negative perceptions of their CHD (with the exception of perceived treatment benefits; Fig. 2). In addition, more positive illness perceptions were associated with greater QOL for both groups (β=.19, p<.001). CHD diagnosis did not have a direct effect on QOL when the mediator was included in the model (β=.09, p=.59). However, CHD diagnosis indirectly affected QOL through illness perceptions (αβ=.15, p=.002, 95% CI=.06-.25). Model fit indices suggested that the proposed model fit the data well (χ2[41]=393.27, p<.001, SRMR=0.00, CFI=1.00, RMSEA=0.00). The final model accounted for 30.0% of the variance in QOL and 47.0% of the variance in illness perceptions. Overall, results suggest that CHD diagnosis influences illness perception scores, which are then important contributors to QOL.
Fig. 2.
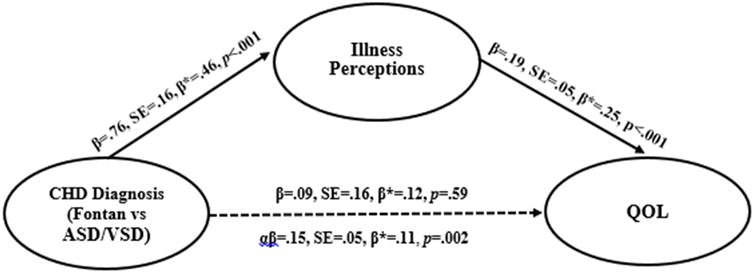
Full Indirect Effects Model with Unstandardized and Standardized Regression Weights Demonstrating that Illness Perceptions Mediate the Association between CHD Diagnosis and QOL with Anxiety and Depressive Symptoms and NYHA functional class Controlled.
Note: β* = standardized regression coefficient
As age and sex differences were present between the Fontan and ASD/VSD samples, these variables were examined as moderators of the mediated associations. Moderated mediation models were tested, such that age and sex were tested as moderators and removed as model covariates. Neither of the moderated mediation models produced significant effects, suggesting that the association between CHD diagnosis, illness perceptions, and QOL does not differ as a function of age or sex.
Discussion
In the present study, we found that patients with a Fontan circulation reported lower QOL and more negative illness perception scores than patients with isolated ASD/VSD. Illness perceptions also mediated the association between CHD diagnosis and QOL. In other words, the patient's defect was associated with his or her perceptions of CHD, which in turn was related to QOL. This finding was consistent regardless of age or sex. Strengths of this study include a large multinational sample, use of a comparison sample, and the use of previous findings to drive study hypotheses.
Consistent with the proposed hypotheses, Fontan patients reported lower QOL relative to patients with less complex defects; this underscores prior studies demonstrating that more complex defects are associated with lower QOL [19, 24, 25]. It is possible that ASD/VSD patients included in APPROACH-IS may have experienced greater CHD severity than the overall ASD/VSD population given the fact that they were followed at a tertiary care center. Thus, the true differences between Fontan and ASD/VSD patients followed in the community may be even larger. Still, similar to prior research [10, 26], Fontan patients in the current study reported relatively high QOL; these high ratings of QOL suggest that many patients with Fontan circulations demonstrate resilience, despite the medical and psychosocial implications of living with complex CHD [2-4, 27]. The chronic illness literature suggests that resilience (i.e., the ability to adapt well despite adversity) results from the dynamic interplay of genetic (e.g., temperament, HPA axis regulation), environmental (e.g., social support), and individual factors (e.g., self-efficacy, spirituality) [28]. Future research may investigate specific contributors to resiliency specific to adults with CHD.
Further, Fontan patients endorsed more negative illness perception scores. Findings are in line with the higher likelihood of complications experienced by Fontan patients [2-5] and research indicating illness perceptions are more pessimistic in patients with more complex CHD [14]. Closer inspection of item-level illness perceptions revealed that Fontan patients perceived a greater effect of CHD on their lives, less perceived control of CHD, a longer duration of CHD, more experienced symptoms, greater concern about CHD, and greater impact of CHD on emotional well-being. Despite these more “negative” or realistic perceptions, patients with a Fontan circulation reported more favorable views regarding treatment benefits compared to the ASD/VSD group; in fact, they endorsed high ratings of confidence in the benefits of medical treatment. Perhaps they realize that their survival to adulthood was drastically increased by having undergone Fontan surgery.
Our results support the hypothesis that the association between CHD diagnosis and QOL is influenced by the patient's illness perceptions. Growing up with a Fontan circulation may be qualitatively different compared to that of a patient with ASD/VSD. Fontan patients, who tend to experience more adverse symptoms, a more intense medical plan, and greater limitations in everyday life (e.g., reduced exercise tolerance, employment restrictions), form illness perceptions that reflect the complexity of their diagnosis. In turn, these perceptions contribute to overall lower QOL. Cognitive theories suggest that thoughts and beliefs have a profound influence on subjective well-being [29]. While adverse medical outcomes and functional status are important determinants of QOL [10, 14, 24], illness perceptions appear to account for unique differences in QOL between groups of varying CHD complexity. In fact, the mediation model was significant even when controlling for NYHA functional class; therefore, we are confident that patients' physical limitations did not confound the associations between CHD diagnosis, illness perceptions, and QOL.
The role of underlying anxiety or depressive symptoms in the development of illness perceptions and assessment of QOL must be acknowledged, especially as internalizing symptoms are frequently elevated among patients with complex CHD [7, 10, 15]. To address this issue, we controlled for anxiety and depressive symptoms in the mediational analyses. Therefore, illness perceptions were less influenced by underlying psychological symptoms and were more likely to reflect independent CHD-related beliefs. Future research may explore how psychological symptoms relate to illness perceptions, QOL, and other psychosocial outcomes in the Fontan population.
Our findings have important implications for clinical practice. Especially in light of findings that psychological difficulties are often missed in patients with CHD [30], patients with Fontan circulations may benefit from ongoing assessment of QOL and perceptions of CHD within the context of comprehensive health care. Patients with diminished QOL or difficulty coping with CHD may be referred for mental health intervention [31, 32], including cognitive behavioural therapy, artistic therapies, spiritual counselling, and peer-to-peer support programs [33]. In fact, a previous study revealed that one third of surveyed patients expressed interest in learning stress management and coping skills related to CHD [27]. It is important to investigate whether the modification of illness perceptions results in improved QOL among Fontan patients. Further, as it is possible that strengthening patients' abilities to manage CHD-related beliefs and improving QOL may have positive effects on their physical health, investing resources into psychological services, including integrated health models [34], should be considered. While treatments targeting illness perceptions have demonstrated promising findings for other cardiac populations [31, 32], there are currently no evidence-based interventions that address psychosocial well-being in CHD.
Limitations
Results must be interpreted in the context of several limitations. First, all data were cross-sectional; the ability to determine whether illness perceptions predicted QOL over time was not possible, although current literature suggests that illness perceptions may predict future QOL in adults with CHD [14, 15]. Second, the internal consistency of the illness perceptions composite was slightly less than the standard 0.70, although the decision was made to retain the variable due to the relative lack of knowledge regarding illness perceptions in CHD. One possibility is that the greater perceived treatment benefits reported by Fontan patients may have lowered the alpha value. Third, shared method variance (i.e., self-report questionnaires) may have increased the likelihood of finding significant associations between illness perceptions and QOL. However, illness perceptions and QOL are purely subjective constructs; assessment by other informants or methods (e.g., direct observation) may not accurately capture the patient's experience of living with CHD. Finally, while the international study sample was relatively diverse, we acknowledge that patients from Asia, Africa, and South America were under-represented relative to world population statistics. Given that countries within these continents are characterized by varying socioeconomic conditions, healthcare infrastructure, and cultural factors that differ markedly from European and North American countries, it is essential for future patient-reported outcomes research to include participants from these under-represented areas.
Conclusions
In summary, patients with a Fontan circulation reported lower QOL and more negative perceptions about their CHD relative to patients with ASD/VSD. After controlling for anxiety and depressive symptoms, and functional status, illness perceptions accounted for an important part of the association between CHD diagnosis (i.e., Fontan vs. ASD/VSD) and lower QOL. This study supports the need for efficient assessment of QOL and illness perceptions and referral to mental health professionals to assist patients, particularly those with Fontan circulations, in acquiring strategies to cope with the physical and emotional challenges associated with their diagnosis.
Acknowledgments
Funding Sources: Research Fund – KU Leuven (OT/11/033), the Swedish Heart-Lung Foundation (20130607), the University of Gothenburg Centre for Person-centred Care, Cardiac Children's Foundation Taiwan (CCF2013_02), and the National Institutes of Health (T32HD068223).
Footnotes
Registration: The study is registered with ClinicalTrials.gov (NCT02150603).
Conflict of interest: No authors have any affiliation or involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the manuscript.
- Christina E. Holbein: Concept/Design; Data analysis/interpretation; Statistics; Drafting article; Critical revision of article; Approval of article
- Nicholas D. Fogleman: Concept/Design; Data analysis/interpretation; Statistics; Drafting article; Critical revision of article; Approval of article
- Kevin Hommel: Critical revision of article; Approval of article
- Silke Apers: Data collection; Critical revision of article; Approval of article
- Jessica Rassart: Data collection; Critical revision of article; Approval of article
- Philip Moons: Concept/Design; Critical revision of article; Funding secured by; Approval of article
- Koen Luyckx: Critical revision of article; Approval of article
- Maayke A. Sluman: Data collection; Approval of article
- Junko Enomoto: Data collection; Approval of article
- Bengt Johansson; Data collection; Critical revision of article; Approval of article
- Hsiao-Ling Yang: Data collection; Approval of article
- Mikael Dellborg: Critical revision of article; Approval of article
- Raghavan Subramanyan: Critical revision of article; Approval of article
- Jamie L. Jackson: Data collection; Critical revision of article; Approval of article
- Werner Budts: Critical revision of article; Approval of article
- Adrienne H. Kovacs: Data collection; Critical revision of article; Approval of article
- Stacey Morrison: Other; Approval of article
- Martha Tomlin: Other; Approval of article
- Kathy Gosney: Other; Approval of article
- Alexandra Soufi: Data collection; Critical revision of article; Approval of article
- Katrine Eriksen: Data collection; Approval of article
- Corina Thomet: Data collection; Critical revision of article; Approval of article
- Malin Berghammer: Data collection; Critical revision of article; Approval of article
- Luis Alday: Data collection; Critical revision of article; Approval of article
- Edward Callus: Data collection; Critical revision of article; Approval of article
- Susan Fernandes: Data collection; Critical revision of article; Approval of article
- Maryanne Caruana: Data collection; Critical revision of article; Approval of article
- Samuel Menahem: Data collection; Critical revision of article; Approval of article
- Stephen C. Cook: Data collection; Approval of article
- Gwen R. Rempel: Data collection; Critical revision of article; Approval of article
- Kamila White: Data collection; Approval of article
- Paul Khairy: Data collection; Critical revision of article; Approval of article
- Shelby Kutty: Data collection; Approval of article
- Gruschen Veldtman: Data collection; Concept/Design; Drafting article; Critical revision of article; Approval of article
References
- 1.d'Udekem Y, Iyengar AJ, Galati JC, et al. Redefining expectations of long-term survival after the Fontan procedure. Circulation. 2014;130(11 suppl 1):S32–S8. doi: 10.1161/CIRCULATIONAHA.113.007764. [DOI] [PubMed] [Google Scholar]
- 2.Kiesewetter CH, Sheron N, Vettukattill JJ, et al. Hepatic changes in the failing Fontan circulation. Heart. 2007;93(5):579–84. doi: 10.1136/hrt.2006.094516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piran S, Veldtman G, Siu S, Webb GD, Liu PP. Heart failure and ventricular dysfunction in patients with single or systemic right ventricles. Circulation. 2002;105(10):1189–94. doi: 10.1161/hc1002.105182. [DOI] [PubMed] [Google Scholar]
- 4.van den Bosch AE, Roos-Hesselink JW, van Domburg R, Bogers AJ, Simoons ML, Meijboom FJ. Long-term outcome and quality of life in adult patients after the Fontan operation. Am J Cardiol. 2004;93(9):1141–5. doi: 10.1016/j.amjcard.2004.01.041. [DOI] [PubMed] [Google Scholar]
- 5.Egbe AC, Connolly HM, Niaz T, et al. Prevalence and outcome of thrombotic and embolic complications in adults after Fontan operation. Am Heart J. 2017;183:10–7. doi: 10.1016/j.ahj.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 6.Overgaard D, Schrader AM, Lisby KH, et al. Patient-reported outcomes in adult survivors with single-ventricle physiology. Cardiology. 2011;120(1):36–42. doi: 10.1159/000333112. [DOI] [PubMed] [Google Scholar]
- 7.Bordin G, Padalino MA, Perentaler S, et al. Clinical profile and quality of life of adult patients after the Fontan procedure. Pediatr Cardiol. 2015;36(6):1261–9. doi: 10.1007/s00246-015-1156-y. [DOI] [PubMed] [Google Scholar]
- 8.Uzark K, Zak V, Shrader P, et al. Assessment of quality of life in young patients with single ventricle after the Fontan operation. J Pediatr. 2016;170:166–72. e1. doi: 10.1016/j.jpeds.2015.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Idorn L, Jensen AS, Juul K, et al. Quality of life and cognitive function in Fontan patients, a population-based study. Int J Cardiol. 2013;168(4):3230–5. doi: 10.1016/j.ijcard.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Pike NA, Evangelista LS, Doering LV, Eastwood JA, Lewis AB, Child JS. Quality of life, health status, and depression: Comparison between adolescents and adults after the Fontan procedure with healthy counterparts. J Cardiovasc Nurs. 2012;27(6):539. doi: 10.1097/JCN.0b013e31822ce5f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rassart J, Apers S, Kovacs AH, et al. Illness perceptions in adult congenital heart disease: A multi-center international study. Int J Cardiol. 2017;244:130–138. doi: 10.1016/j.ijcard.2017.06.072. [DOI] [PubMed] [Google Scholar]
- 12.Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry. 2007;20(2):163–7. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- 13.Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res. 2006;60(6):631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 14.Schoormans D, Mulder BJ, Van Melle JP, et al. Illness perceptions of adults with congenital heart disease and their predictive value for quality of life two years later. Eur J Cardiovasc Nurs. 2014;13(1):86–94. doi: 10.1177/1474515113481908. [DOI] [PubMed] [Google Scholar]
- 15.O'Donovan CE, Painter L, Lowe B, Robinson H, Broadbent E. The impact of illness perceptions and disease severity on quality of life in congenital heart disease. Cardiol Young. 2016;26(01):100–9. doi: 10.1017/S1047951114002728. [DOI] [PubMed] [Google Scholar]
- 16.Steca P, Greco A, Monzani D, et al. How does illness severity influence depression, health satisfaction and life satisfaction in patients with cardiovascular disease? The mediating role of illness perception and self-efficacy beliefs. Psychol Health. 2013;28(7):765–83. doi: 10.1080/08870446.2012.759223. [DOI] [PubMed] [Google Scholar]
- 17.Apers S, Kovacs AH, Luyckx K, et al. Quality of life of adults with congenital heart disease in 15 countries: Evaluating country-specific characteristics. J Am Coll Cardiol. 2016;67(19):2237–45. doi: 10.1016/j.jacc.2016.03.477. [DOI] [PubMed] [Google Scholar]
- 18.Apers S, Kovacs AH, Luyckx K, et al. Assessment of Patterns of Patient-reported Outcomes in Adults with Congenital Heart disease—International Study (APPROACH-IS): Rationale, design, and methods. Int J Cardiol. 2015;179:334–42. doi: 10.1016/j.ijcard.2014.11.084. [DOI] [PubMed] [Google Scholar]
- 19.Moons P, Van Deyk K, De Geest S, Gewillig M, Budts W. Is the severity of congenital heart disease associated with the quality of life and perceived health of adult patients? Heart. 2005;91(9):1193–8. doi: 10.1136/hrt.2004.042234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. J Pers Assess. 1985;49(1):71–5. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 21.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 22.Muthén L, Muthén B. Mplus User's guide 7.0. Los Angeles: Muthen & Muthen; pp. 1998–2015. [Google Scholar]
- 23.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995:289–300. [Google Scholar]
- 24.Jackson JL, Hassen L, Gerardo GM, Vannatta K, Daniels CJ. Medical factors that predict quality of life for young adults with congenital heart disease: What matters most? Int J Cardiol. 2016;202:804–9. doi: 10.1016/j.ijcard.2015.09.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simko LC, McGinnis KA. What is the perceived quality of life of adults with congenital heart disease and does it differ by anomaly? J Cardiovasc Nurs. 2005;20(3):206–14. doi: 10.1097/00005082-200505000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Moons P, Deyk KV, Bleser LD, et al. Quality of life and health status in adults with congenital heart disease: a direct comparison with healthy counterparts. Eur J Cardiovasc Prev Rehab. 2006;13(3):407–13. doi: 10.1097/01.hjr.0000221864.19415.a0. [DOI] [PubMed] [Google Scholar]
- 27.Kovacs AH, Bendell KL, Colman J, Harrison JL, Oechslin E, Silversides C. Adults with congenital heart disease: Psychological needs and treatment preferences. Congenit Heart Dis. 2009;4(3):139–46. doi: 10.1111/j.1747-0803.2009.00280.x. [DOI] [PubMed] [Google Scholar]
- 28.Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics. 2011;52(3):199–209. doi: 10.1016/j.psym.2011.01.036. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT. The current state of cognitive therapy: A 40-year retrospective. Arch Gen Psychiatry. 2005;62(9):953–9. doi: 10.1001/archpsyc.62.9.953. [DOI] [PubMed] [Google Scholar]
- 30.Callus E, Quadri E, Ricci C, et al. Update on psychological functioning in adults with congenital heart disease: A systematic review. Expert Rev Cardiovasc Ther. 2013;11(6):785–91. doi: 10.1586/erc.13.9. [DOI] [PubMed] [Google Scholar]
- 31.Jonsbu E, Martinsen EW, Morken G, Moum T, Dammen T. Change and impact of illness perceptions among patients with non-cardiac chest pain or benign palpitations following three sessions of CBT. Behav Cog Psychother. 2013;41(04):398–407. doi: 10.1017/S1352465813000179. [DOI] [PubMed] [Google Scholar]
- 32.Sararoudi RB, Motmaen M, Maracy MR, Pishghadam E, Kheirabadi GR. Efficacy of illness perception focused intervention on quality of life, anxiety, and depression in patients with myocardial infarction. J Res Med Sci. 2016;21(1):125. doi: 10.4103/1735-1995.196607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Callus E, Quadri E, editors. Clinical Psychology and Congenital Heart Disease. Milan, Italy: Springer; 2015. [Google Scholar]
- 34.Ferguson M, Kovacs AH. An integrated adult congenital heart disease psychology service. Congenit Heart Dis. 2016;11(5):444–51. doi: 10.1111/chd.12331. [DOI] [PubMed] [Google Scholar]


