Abstract
The goal of patient-centered outcomes research (PCOR) is to help patients and those who care for them make informed decisions about healthcare. However, the clinical research enterprise has not involved patients, caregivers, and other non-providers routinely in the process of prioritizing, designing and conducting research in hematopoietic cell transplantation (HCT). To address this need, the National Marrow Donor Program (NMDP)/Be The Match® engaged patients, caregivers, researchers and other key stakeholders in a two-year project with the goal of setting a PCOR agenda for the HCT community. Through a collaborative process, we identified six major areas of interest: 1) Patient, Caregiver and Family Education and Support; 2) Emotional, Cognitive and Social Health; 3) Physical Health and Fatigue; 4) Sexual Health and Relationships; 5) Financial Burden; and 6) Models of Survivorship Care Delivery. We then organized into multi-stakeholder Working Groups to identify gaps in knowledge and make priority recommendations for critical research to fill those gaps. Gaps varied by Working Group, but all noted that a historical lack of consistency in measures utilized and patient populations made it difficult to compare outcomes across studies and urged investigators to incorporate uniform measures and homogenous patient groups in future research. Some groups advised that additional pre-emptory work is needed before conducting prospective interventional trials, whereas others felt ready to proceed with comparative clinical effectiveness research studies. This report presents the results of this major initiative, and makes recommendations by Working Group on priority questions for PCOR in HCT.
Keywords: hematopoietic cell transplantation, survivorship, patient-centered outcomes
INTRODUCTION
Mr. WB, a 62-year-old hardware store owner, has acute myeloid leukemia in first clinical remission. His physician referred him for allogeneic hematopoietic cell transplant (HCT) consultation. Mr. WB and his wife prepare a list of questions to ask the transplant team, including: How likely is it that Mr. WB will be cured? How long will it take to feel like himself again? Will he be able to manage his hardware business after the transplant, including stocking shelves and doing the accounting? Will transplant be expensive? What challenges will Mrs. WB face, and how can she best help her husband?
Mr. and Mrs. WB are asking not only about the curative potential of HCT, but also about post-HCT physical and cognitive functioning, quality of life (QOL), financial security and psychosocial wellbeing for him and his caregiver spouse. HCT is a potentially curative treatment modality for many patients with hematologic disorders. Unfortunately, it is also associated with significant morbidity that may adversely impact a patient’s recovery for weeks, months or even years.
Historically, the transplant research community has focused on studies to improve the potential for post-HCT survival. Less attention has been paid to finding the best answers for the other questions posed by Mr. and Mrs. WB, particularly from the perspective of the patient. Furthermore, patients, caregivers, and other non-providers have not been engaged by the research community to assist in the prioritization of research questions. To address this need, the National Marrow Donor Program (NMDP)/Be The Match convened a series of collaborative conferences and established six Working Groups (WGs) to engage patients, caregivers and other key stakeholders as a foundation to develop and to promote a research agenda that incorporates patient perspectives and patient-centered outcomes research (PCOR) in HCT. Here we report project outcomes including the process of engaging patients and caregivers, identification of knowledge gaps, and prioritization of high impact research questions or recommendations by each WG.
METHODS
Work Plan
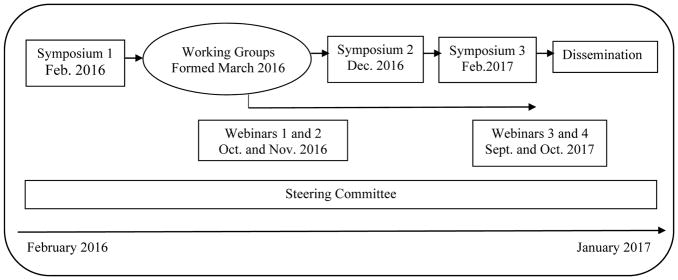
Figure 1 depicts the two-year work plan for this project. The overarching design for this initiative included a series of three symposia with WGs, developed following the initial symposium, conducting their work longitudinally throughout the project. A steering committee (see list of members in Supplemental Table 1) that included patients and caregivers provided input and oversaw all aspects of the project.
Figure 1.
Work plan for the two-year patient engagement project in hematopoietic cell transplantation
Symposia and Formation of Working Groups
The first symposium held in February 2016 focused on setting the stage for the project and included a panel of patients and caregivers who described their personal transplant journeys and what outcomes, other than survival, mattered most to them. Round table discussions centered on what the attendees had learned from the panel, and a subsequent informal “report out” session identified topic areas that merited assignment to a WG. Subsequently, NMDP staff experienced in moderating focus groups conducted three informal focus groups of patients and caregivers. The combined input from the symposium and teleconferences informed the creation of six WGs: 1) Patient, Caregiver and Family Education and Support; 2) Emotional, Cognitive and Social Health; 3) Physical Health and Fatigue; 4) Sexual Health and Relationships; 5) Financial Burden; and 6) Models of Survivorship Care Delivery.
The second and third symposia were held in December 2016 and February 2017, respectively, and focused on presentations by each of the six WGs to obtain attendee feedback for subsequent WG refinement of priority research questions. These two sympoia included patients and caregivers as attendees, panelists and presenters with the WG co-chairs.
Working Group Participants
WGs comprised volunteers representing all stakeholders, including 25 patients and 7 caregivers plus clinicians, researchers, social workers, policy makers, administrators, payers and NMDP staff liaisons (see complete list of members and stakeholder group in Supplemental Table 2). Two members from each WG were designated as co-chairs. Although all WGs were tasked with identifying gaps in knowledge and prioritizing potential research questions with an emphasis, if possible, on questions that would be amenable to addressing through comparative clinical effectiveness research (CER) studies, each WG developed their own process for accomplishing the tasks and hence are described separately by WG in the Results section. WGs met at least once-monthly by teleconference for one hour with any subgroups holding additional meetings as needed.
Webinars
NMDP hosted four webinars as part of the engagement and dissemination efforts (Figure 1). The first webinar highlighted issues in survivorship of importance to patients and caregivers, the second webinar featured three investigators’ PCOR programs, and the final two webinars incorporated the WGs’ final presentations.
WORKING GROUPS
Patient, Caregiver and Family Education and Support Working Group
Process
A literature review using key terms “patient education”, “self-management”, “self-efficacy” and “stem cell transplantation” identified 82 articles published from 1995 – 2016, of which 50 were deemed relevant. WG members worked in dyads to review 8–10 articles. Each dyad included one patient, caregiver or psychosocial health professional and one physician or researcher. Co-chairs reviewed all systematic review articles. Dyads reported their: 1) key learning points; 2) gaps identified; and 3) comparison with personal or clinical experience. Group discussion, including patient and caregiver experiences, further clarified and enhanced the literature. Findings were synthesized into themes and research questions and returned to the group for revision and prioritization.
Knowledge gaps
Gaps in knowledge were in part due to the design of previous research studies (single institution, lack of diverse patient populations, short follow-up times), and were organized into three main categories: 1) Education methodology to optimal format, timing and delivery of education, 2) Tailored assessments of individual learner’s needs, including learning styles, information needs, and cultural/educational backgrounds that impact learning preferences, and 3) Training for health care providers as educators for their patients and caregivers [1–6].
Research Priorities
The WG noted that within their group, providers were most interested in a primary outcome measure of an increase in patient and caregiver health knowledge, whereas patients and caregivers preferred outcome measures of a decrease in distress and an increase in sense of control and self-efficacy. Therefore, the highest priority questions of the WG revolved around comparing models of education within the context of these measures, plus determining the factors that predict these outcomes among patients and caregivers as shown in Table 1.
Table 1.
Priority research questions and recommendations by working group
| Working Group | Priority Research Questions and Recommendations |
|---|---|
| Patient, Caregiver and Family Education and Support |
|
| Emotional, Cognitive and Social Health |
|
| Physical Health and Fatigue |
|
| Sexual Health and Relationships |
|
| Financial Burden |
|
| Models of Survivorship Care Delivery |
|
HCT, hematopoietic cell transplantation; PROMIS, Patient-Reported Outcomes Measurement System
Emotional, Cognitive and Social Health Working Group
Process
This WG conducted a scoping review to identify high-yield review articles focused on emotional, psychological, social, and cognitive well-being as well as health related quality of life (HRQoL) within the adult and pediatric HCT literature. Researchers contributed additional important articles focusing primarily on the intervention literature within HCT as well as oncology at large. The WG then divided into three subgroups to ensure comprehensive coverage of the important topics and ensure good discussion of both adult and pediatric challenges: 1) Adult emotional, psychological, and social health, 2) Pediatric emotional, psychological, and social health, and 3) Adult and Pediatric cognitive function. Researchers were asked to specifically summarize the articles within each subgroup using a specific framework that focused on knowledge, research gaps, and future directions. Subgroup patients and caregivers were asked to read the articles with particular attention to how relevant the content was based on their experience and perspective on the HCT course. Each subgroup had individual meetings to review their findings from the literature review and provide a high-level summary of the current state of the knowledge, research gaps, and areas for future research. Each subgroup then reported their findings back to the entire WG to discuss common themes and make final recommendations.
Knowledge gaps
Major methodological limitations in the current literature of emotional, psychological, and social health for both adult and pediatric HCT recipients were identified, including studies with small sample sizes, high rates of attrition to follow-up with substantial selection biases and utilization of heterogeneous instruments to measure key outcomes [7–12]. Additionally, often autologous and allogeneic HCT patients are grouped together in studies, yet their experiences and recovery courses are drastically different [7–12]. There is a lack of focus on specific psychological, social, and emotional concerns of caregivers [11–14]. Additionally, there is a limited focus on comprehensively understanding the psychological, emotional, and social challenges faced by HCT survivors more than one year post-HCT, in part due to limited access as survivors move away from their HCT centers. There is also a lack of cultural, linguistic, and ethnic diversity in the available studies and very limited intervention studies on both patients and caregivers.
Unique to the pediatric population is a lack of age-appropriate patient-reported outcome measures or instruments further limiting the ability to measure these key outcomes in pediatric populations. Furthermore, there is a significant reliance on parental assessment of patients’ emotional and social well-being, which can be problematic and not always valid. It also remains unclear whether modifying the patients’ experience during HCT (in terms of enhancing their quality of life and distress) can impact post-HCT outcomes and long-term psychological distress.
Studies of cognitive function also have been small in sample size and included heterogeneous populations without good controls [15–18]. There is a lack of data on cognitive outcomes in the special populations of pediatric and older adults. There is also a lack of longitudinal studies with pre-chemotherapy and post-HCT outcomes with long-term follow-up.
Research Priorities
The WG felt this field is not yet mature enough to conduct CER studies. Instead, the WG recommended that multicenter studies, beginning in the adult population, incorporating better methodology to account for missing data, attrition biases and diverse patient populations be conducted that include autologous and allogeneic HCT survivors in separate studies. Longitudinal studies should incorporate measures that are more meaningful to patients and families, including how deficits affect daily living, functioning and return to work. Technology should be leveraged for interventional studies to enhance the potential for dissemination and to reach survivors receiving care remotely. Studies focusing on positive emotional change (resilience) are also needed. Studies to assess the mechanism of cognitive problems are needed, including incorporating functional magnetic resonance imaging, cognitive neuroscience, and event-related potentials. An understanding of the relationship between emotional distress, depression, and psychological well-being and its impact on cognitive dysfunction also requires further exploration. Priority research questions are listed in Table 1.
Physical Health and Fatigue Working Group
Process
To cast a broad net of perspectives, WG members each listed 1) their observations about physical health or fatigue before, during, or after HCT and 2) areas where they felt more research needs to be done (e.g. “gaps” or “unmet needs”). After discussing them together, WG members then worked individually to prioritize them. Based on these priorities, the WG was divided into four subgroups, each including patients and caregivers: 1) Measurement, 2) Mechanism, 3) Engagement, and 4) Intervention. Among all aspects of physical health, fatigue quickly emerged as the highest priority issue.
Knowledge gaps
Inconsistency in instrument choice for measuring physical health and fatigue and application across studies limits our understanding in this area [19–25]. Relatively few studies have attempted to correlate phenotype (self-reported) with biologic measures to identify causative pathways (e.g. inflammatory markers, cells, cytokines, hormones). While fatigue is a common concern across the transplant trajectory, little is known about how HCT patients and providers think about or discuss fatigue and physical health in clinical practice. In the HCT research setting, interventions to improve fatigue and physical health impairments largely have been small-scale efforts [26–28].
Research Priorities
The WG noted that the ideal instrument to measure fatigue in the HCT population would minimize patient, clinician and researcher burden while maximizing comparability. The WG recommended that the HCT community adopt the Patient-Reported Outcomes Measurement System (PROMIS) measures at defined pre- and post-HCT time points. The least burdensome way to develop a correlative infrastructure and biobank for collection of concurrent patient-reported outcomes (e.g. symptoms), objective function/performance measures, and biomarkers to inform our understanding of the mechanisms underlying fatigue should be developed and tested in a cross-sectional study. Priority research recommendations are listed in Table 1.
Sexual Health and Relationships Working Group
Process
The WG began by hearing from their patient and caregiver members on topics of importance to them. From these discussions, five topics for subgroups were identified: 1) Sexual activity, 2) Sexual health, 3) Communication, 4) Body image, and 5) Fertility. Each WG member volunteered to focus on one of the topics with a health professional leading each subgroup. They reviewed the published literature for each topic and assessed knowledge gaps. Each sub-group then shared their findings with the entire WG and discussed how it relates to the patient experience. A list of questions identified during the literature review as well as from the patient experience were developed and prioritized.
Knowledge gaps
There is no information published, and in particular no evidence-based guidelines, to provide guidance as to which sexual activities are safe (or risky) or a time frame as to when survivors may engage in these activities. Some HCT centers have guidelines that are not very specific, and there is no systematic approach to educating survivors. Understanding of the impact of HCT on sexual dysfunction is limited, in large part due to a lack of a well-described “baseline”/pre-HCT/pre-cancer (or general population) incidence of these symptoms. Risk factors for developing these complications are poorly defined, and there is no systematic approach to assessing the sexual health of survivors, nor is there a well-defined network of healthcare providers in any discipline (HCT, gynecology, urology, endocrinology, psychology, others) to provide support, guidance and therapeutic interventions to these patients.
The HCT survivor and their caregiver undergo many role changes throughout the HCT trajectory. The HCT recipient transitions from husband, wife, father, mother, or provider to a patient and the caregiver transitions from spouse to caregiver. There is limited understanding regarding the impact of these role changes and how couples navigate these transitions. Specifically, the change from being a lover to a caregiver or patient and back can be especially challenging.
HCT survivors often struggle with disclosing their health history, particularly their cancer diagnosis and treatment, in new relationships. There are no evidence-based guidelines to describe the best approach to communicating with partners or potential partners about changes in their health in particular sexual functioning and infertility. There is a lack of guidance that can be provided to HCT survivors on how or when to discuss their health history, especially in new relationships.
The literature on body image is limited but the available studies, which are often small in scale and include participants who are predominantly white and middle class, indicate that factors affecting body image can include changes to appearance, sensory changes, and functional impairment [29–31]. In addition, altered body image may disrupt feelings about the self as a sexual being and lead to less sexual satisfaction, poorer body image and increased disruption in sexual relationships. Much of the available research in body image is with patients in committed relationships and/or sexually active patients, but little is known about the sexual functioning, needs or concerns of people who are single and/or sexually inactive [30]. There is a lack of evidence-based guidelines or tested interventions on helping survivors in different stages of life develop a healthy body image post-HCT.
Published literature and the patient experience indicate that issues surrounding fertility and infertility usually arise after the acute phase of HCT [32, 33]. Fertility preservation options are not explored systematically early in the cancer treatment timeline which can limit post-HCT options. Even after chemotherapy and pre-transplant, there may be opportunities to preserve fertility [34, 35]. There has been little research on understanding the psychological impact of infertility nor on interventions to help individuals and couple cope with the loss of fertility. In addition, post-transplant fertility referrals are not well-described in the literature [32, 33, 36–38].
Research Priorities
The WG decided that additional pre-emptory work is needed in all areas to inform comparative clinical effectiveness research. A first step would be to develop expert based clinical guidelines for resuming sexual activity post-HCT and are a priority for this WG. With guidelines in place, interventions could be developed, and ultimately compared, that focus on sexual health education and the treatment of sexual dysfunction. Comparing various interventions such as couples counseling and survivorship workshops delivered at multiple time points pre- and post-HCT could lead to the development of interventions to help patients improve communication in new or existing relationships. A better understanding of the barriers to fertility preservation is needed. Research areas to explore include the emotional response to infertility with longitudinal studies, to understand the impact of infertility on new and established relationships, and to guide the referral of patients for reproductive consultation after HCT. The unique needs regarding sexual health across special populations must be addressed, including adolescents and young adults, culturally and linguistically diverse populations, the lesbian/gay/bisexual and transgender (LGBTQI) population, older (65 years and greater) recipients, pediatric survivors, and single individuals. Priority research questions are listed in Table 1.
Financial Burden Working Group
Process
The WG identified three major areas of concern and divided into three sub-groups to further explore those topics: (1) Describe and determine costs of HCT from the patient’s perspective, (2) Caregiver financial burden, and (3) Information about long-term costs.
Knowledge gaps
The literature provides information about initial post-HCT costs and types of costs [39–41], but little information exists about patient financial health going into HCT or about patient awareness of financial hardship they may face. In fact, one study found that pre-HCT, financial issues and work were the most frequent concerns after symptoms [42]. Patients also express a lack of knowledge about financial resources available to them, as the diagnosis and curative aspect is the focus for both patients and medical providers [43].
Existing literature has attempted to characterize the burden of HCT on caregivers. Available data generally provides descriptions of burden during the short term, within the first three months post-HCT [40, 44, 45]. Caregiver stress and burden has been associated with poorer patient quality of life, impaired patient outcomes, and loss of income including difficulties covering expenses for medical care [41,44, 46]. This suggests that more attention is needed to better understand and mitigate caregiver financial burden.
There is little known about the long-term costs of HCT or about the depth and breadth of this issue across the community, its impact to health systems and patients and families, and ultimately health outcomes. It is also not known how medical professionals can best address cost issues for patients, help reduce costs, or if long-term financial issues could be improved with better pre-HCT planning.
Research Priorities
Recommendations centered on attempting to assess the role of timing in preparation for HCT, better characterize and inform patients of the costs associated with HCT, identify and assess current and new approaches to reducing both patient and caregiver patient financial burden, and identify long-term financial burden across various patient and caregiver populations and what, if any, impact physician involvement has in outcomes. Metrics were suggested, including PROMIS measures, depending on the scope of inquiry. The priority research questions are shown in Table 1.
Models of Survivorship Care Delivery Working Group
Process
The WG first conducted a literature review, including work products from the National Institutes of Health’s Late Effects Initiative Health Care Delivery Working Group [47] and the NMDP Advisory Group on Financial Barriers to Transplantation [48]. The WG engaged their patient and caregiver members in an informal discussion about aspects of survivorship care that were most important to them. Realizing the need for a more focused and detailed assessment of their experiences and needs, a phone-based discussion group was held. Responses were organized into three major themes: 1) Provider access to optimal medical services for their patients, 2) Patient and caregiver education on survivorship issues, and 3) Caregiver and family support services during long-term survivorship care.
Knowledge gaps
Patients and caregivers articulate their preference for a health care delivery model that gives them access to the right physician, for the right indication, at the right time with the right communication among physicians and between physicians and patients. There are a variety of approaches for survivorship care in use globally in HCT programs. These include a shared-care model, care coordination using a nurse-coordinator, and specialty survivorship clinic models. The effectiveness of these and other models in delivering survivorship education and care according to patient and caregiver needs, values, and personal characteristics is unknown. The importance of caregivers in the recovery phase of HCT is crucial, yet there is little knowledge about how to support caregivers in their efforts to promote the health of the patient.
Research Priorities
The WG’s recommendations centered on optimizing long-term care of survivors who may require multiple providers in multiple care settings. The need for increased communication among providers with less reliance on the patient or caregiver to be the sole source of communication among providers was stressed. The most effective delivery method of education to patients and caregivers about survivorship issues that is individually tailored to clinical and personal needs, and is readily accessible for long-term follow-up, should be studied. Measures of patient satisfaction with survivorship care need to be established to improve comparison across studies. Finally, the psychosocial needs of caregivers in supporting the patient throughout the trajectory of recovery should be addressed. The priority research questions are shown in Table 1.
SUMMARY
This project engaged patients and caregivers throughout a reiterative process of literature review, identification of knowledge gaps, dialogue, and prioritization of PCOR questions in HCT. All stakeholders acknowledged the value of engaging patients and caregivers, as their unique insights were informative, drove discussion, and were foundational to prioritizing the research recommendations.
In the early weeks of this project, the first symposium and subsequent teleconferences informed the development of the WGs around topic areas. Education, physical health and fatigue, emotional health and cognitive function, and care delivery were oft repeated themes at the first symposium, but there was minimal mention of a need to focus on the areas of sexual health and financial burden. However, when patients and caregivers were provided with an additional opportunity to discuss topics via teleconferences, sexual health and financial burden emerged as critical focus areas. This suggests that patients and caregivers may not be as comfortable highlighting some sensitive topics in a larger, multi-stakeholder symposium setting as in a smaller setting of those with shared experiences; this concept should inform development of future PCOR initiatives.
The processes followed by the WGs to perform their assigned tasks were similar among the groups in that all members were involved in discussions and prioritization activities, yet two differences were noteworthy. The Patient, Caregiver and Family Education and Support WG demonstrated that patients and caregivers, after having experienced the complexity of HCT, have become so informed about HCT that they were able to be equal partners in the review of research literature. Patients and caregivers in the Models of Survivorship Care Delivery had so much information to share about their experiences navigating healthcare systems for post-HCT care that an additional discussion group was needed for better comprehension of potential research topics. We also engaged patients and caregivers from all the WGs by inviting them to share the podium with clinicians and researchers in presenting the proposed research agenda at the final symposium. Clearly, a variety of effective approaches can be taken to fully engage patients and caregivers in PCOR; groups should explore various methods to identify a process that works optimally for them.
While tasked with identifying questions that could be addressed through CER studies, several WGs, including the Emotional, Cognitive and Social Health, Physical Health and Fatigue, and Sexual Health and Relationships WGs, felt that additional, foundational studies are needed, using consistent measures in homogenous patient populations, in order to interpret outcomes and inform the development of comparative studies. In addition, the Physical Health and Fatigue WG recommended development of an infrastructure to support biobanking of specimens to facilitate future studies of the mechanisms underlying fatigue.
We acknowledge limitations to this project. There were more volunteers for the Working Groups than could be accommodated and, while we offered webinars and notices of how to provide comments via various newsletters and formats, not every stakeholder voice could heard. However, a major strength of the project was that we were able to include representation from domestic and international clinicians/researcher caring for both adult and pediatric populations, caregivers of both adult and pediatric patients, and members from underrepresented groups.
A variety of methods are being used to disseminate the results of this initiative in order to heighten awareness and drive engagement of both the lay and scientific communities. Patients and caregivers have indicated their interest and willingness to participate in the development of research studies to address the priority questions. Now that the PCOR agenda in HCT has been set, it is up to us to move forward and not let the momentum dissipate. We challenge each Working Group to strategize and further develop at least one priority question, invite additional stakeholders’ comments, and hope that the PCOR national and international community will join us in these efforts.
Supplementary Material
Table 1. Steering Committee members, institution and represented stakeholder group(s)
Table 2. Working Group members, institution and represented stakeholder group(s)
Highlights.
Patient engagement is critical to inform patient-centered outcomes research (PCOR)
Multiple methods exist to engage patients in research and should be tailored to fit their preferences
PCOR recommendations in HCT by six Working Groups are presented
Acknowledgments
This project was supported in part by a Patient-Centered Outcomes Research Institute Eugene Washington Engagement Award (PCORI EAIN-2956). We thank the PCORI Program Officer, Yasmeen Long, for her assistance throughout the project. We thank all members of the Working Groups, especially the patients and caregivers, and those who participated in the teleconferences, symposia and webinars for providing their unique perspectives that informed the research agenda. We thank Kate Houg, Christa Meyer, Jaime Preussler, Lin-Win Mau, and Robynn Erdmann for project and symposia planning support, and Edmund Waller for critical review of the manuscript.
Footnotes
Declarations of Interest: none
References
- 1.Cohen MZ, Jenkins D, Holston EC, Carlson ED. Understanding health literacy in patients receiving hematopoietic stem cell transplantation. Oncol Nurs Forum. 2013;40:508–515. doi: 10.1188/13.ONF.508-515. [DOI] [PubMed] [Google Scholar]
- 2.Cooke L, Grant M, Gemmill R. Discharge needs of allogeneic transplantation recipients. Clin J Oncol Nurs. 2012;16:E142–E149. doi: 10.1188/12.CJON.E142-E149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman AJ, Cosby R, Boyko S, Hatton-Bauer J, Turnbull G. Effective teaching strategies and methods of delivery for patient education: A systematic review and practice guideline recommendations. J Cancer Educ. 2011;26:12–21. doi: 10.1007/s13187-010-0183-x. [DOI] [PubMed] [Google Scholar]
- 4.Jim HS, Quinn GP, Gwede CK, et al. Patient education in allogeneic hematopoietic cell transplant: What patients wish they had known about quality of life. Bone Marrow Transplant. 2014;49:299–303. doi: 10.1038/bmt.2013.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 6.Feudtner C. What are the goals of patient education? West J Med. 2001;174:173–174. doi: 10.1136/ewjm.174.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pidala J, Anasetti C, Jim H. Quality of life after allogeneic hematopoietic cell transplantation. Blood. 2009;114:7–19. doi: 10.1182/blood-2008-10-182592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luebbert K, Dahme B, Hasenbring M. The effectiveness of relaxation training in reducing treatment-related symptoms and improving emotional adjustment in acute non-surgical cancer treatment: a meta-analytical review. Psychooncology. 2001;10:490–502. doi: 10.1002/pon.537. [DOI] [PubMed] [Google Scholar]
- 9.Packman W, Weber S, Wallace J, Bugescu N. Psychological effects of hematopoietic SCT on pediatric patients, siblings, and parents: a review. Bone Marrow Transplant. 2010;45:1134–1146. doi: 10.1038/bmt.2010.74. [DOI] [PubMed] [Google Scholar]
- 10.Baliousis M, Rennoldson M, Snowden JA. Psychological interventions for distress in adults undergoing haematopoietic stem cell transplantation: a systematic review with meta-analysis. Psychooncology. 2016;25:400–411. doi: 10.1002/pon.3925. [DOI] [PubMed] [Google Scholar]
- 11.Beattie S, Lebel S. The experience of caregivers of hematologic cancer patients undergoing a hematopoietic stem cell transplant: a comprehensive literature review. Psychooncology. 2011;20:1137–1150. doi: 10.1002/pon.1962. [DOI] [PubMed] [Google Scholar]
- 12.Gemmill R, Cooke L, Williams AC, Grant M. Informal caregivers of hematopoietic cell transplant patients: a review and recommendations for interventions and research. Cancer Nurs. 2011;34:E13–21. doi: 10.1097/NCC.0b013e31820a592d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bevans M, Wehrlen L, Castro K, et al. A problem-solving education intervention in caregivers and patients during allogeneic hematopoietic stem cell transplantation. J Health Psychol. 2014;19:602–617. doi: 10.1177/1359105313475902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laudenslager ML, Simoneau TL, Kilbourn K, et al. A randomized control trial of a psychosocial intervention for caregivers of allogeneic hematopoietic stem cell transplant patients: effects on distress. Bone Marrow Transplant. 2015;50:1110–1118. doi: 10.1038/bmt.2015.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harder H, Cornelissen JJ, Van Gool AR, Duivenvoorden HJ, Eijkenboom WM, van den Bent JM. Cognitive functioning and quality of life in long-term adult survivors of bone marrow transplantation. Cancer. 2002;95:183–192. doi: 10.1002/cncr.10627. [DOI] [PubMed] [Google Scholar]
- 16.Correa DD, Maron L, Harder H, et al. Cognitive functions in primary central nervous system lymphoma: literature review and assessment guidelines. Ann Oncol. 2007;18:1145–1151. doi: 10.1093/annonc/mdl464. [DOI] [PubMed] [Google Scholar]
- 17.Booth-Jones M, Jacobsen PB, Ransom S, Soety E. characteristics and correlates of cognitive functioning following bone marrow transplantation. Bone Marrow Transplant. 2005;36:695–702. doi: 10.1038/sj.bmt.1705108. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs SR, Small BJ, Booth-Jones M, Jacobsen PB, Fields KK. Changes in cognitive functioning in the year after hematopoietic stem cell transplantation. Cancer. 2007;110:1560–1567. doi: 10.1002/cncr.22962. [DOI] [PubMed] [Google Scholar]
- 19.Andrykowski MA, Cordovoa MJ, Hann DM, Jacobsen PE, Fields KK, Phillips G. Patients’ psychosocial concerns following stem cell transplantation. Bone Marrow Transplant. 1999;24:1121–1129. doi: 10.1038/sj.bmt.1702022. [DOI] [PubMed] [Google Scholar]
- 20.Hjernmstad MJ, Knobel H, Brinch L, et al. A prospective study of health-related quality of life, fatigue, anxiety and depression 3–5 years after stem cell transplantation. Bone Marrow Transplant. 2004;34:257–266. doi: 10.1038/sj.bmt.1704561. [DOI] [PubMed] [Google Scholar]
- 21.Jim HS, Sutton SK, Jacobsen PB, Martin PJ, Flowers ME, Lee SJ. Risk factors for depression and fatigue among survivors of hematopoietic cell transplantation. Cancer. 2016;122:1290–1297. doi: 10.1002/cncr.29877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrykowski MA, Bishop MM, Hahn EA, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem cell transplantation. J Clin Oncol. 2005;23:599–608. doi: 10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 23.Gielissen MF, Schattenberg AV, Verhagen CA, Rinkese MJ, Bremmers ME, Bleijenberg G. Experience of severe fatigue in long-term survivors of stem cell transplantation. Bone Marrow Transplant. 2007;39:595–603. doi: 10.1038/sj.bmt.1705624. [DOI] [PubMed] [Google Scholar]
- 24.Graef DM, Phipps S, Parris KR, et al. Sleepiness, fatigue, behavioral functioning, and quality of life in survivors of childhood hematopoietic stem cell transplant. J Ped Psychol. 2016;41:600–609. doi: 10.1093/jpepsy/jsw011. [DOI] [PubMed] [Google Scholar]
- 25.Bevans M, El-Jawahri A, Tierney DK, et al. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: The Patient-Centered Outcomes Working Group Report. Biol Blood Marrow Transplant. 2017;23:538–551. doi: 10.1016/j.bbmt.2016.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobsen PB, Le-Rademacher J, Jim H, et al. Exercise and stress management training prior to hematopoietic cell transplantation: Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0902. Biol Blood Marrow Transplant. 2014;20:1530–1536. doi: 10.1016/j.bbmt.2014.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeFor TE, Burns LJ, Gold EM, Weisdorf DJ. A randomized trial of the effect of a walking regimen on the functional status of 100 adult allogeneic donor hematopoietic cell transplant patients. Biol Blood Marrow Transplant. 13:948–955. doi: 10.1016/j.bbmt.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 28.Shelton ML, Lee JQ, Morris GS, et al. A randomized control trial of a supervised versus a self-directed exercise program for allogeneic stem cell transplant patients. Psychooncology. 2009;18:353–359. doi: 10.1002/pon.1505. [DOI] [PubMed] [Google Scholar]
- 29.Humphreys CT, Tallman G, Altmaier EM, Barnette V. Sexual functioning in patients undergoing bone marrow transplantation: a longitudinal study. Bone Marrow Transplant. 2007;39:491–496. doi: 10.1038/sj.bmt.1705613. [DOI] [PubMed] [Google Scholar]
- 30.Thygesen KH, Schiødt I, Jarden M. The impact of hematopoietic stem cell transplantation on sexuality: a systematic review of the literature. Bone Marrow Transplant. 2012;47:716–724. doi: 10.1038/bmt.2011.169. [DOI] [PubMed] [Google Scholar]
- 31.Tierney DK. Sexuality following hematopoietic cell transplantation. Clinical J Oncol Nurs. 8:43–47. [PubMed] [Google Scholar]
- 32.Loren AW, Chow E, Jacobsohn DA, et al. Pregnancy after hematopoietic cell transplantation: a report from the late effects working committee of the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2011;17:157–166. doi: 10.1016/j.bbmt.2010.07.009. BBMT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joshi S, Savani BN, Chow EJ, et al. Clinical guide to fertility preservation in hematopoietic cell transplant recipients. Bone Marrow Transplant. 2014;49:477–484. doi: 10.1038/bmt.2013.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rossi BV, Ashby RK, Srouji SS. Embryo banking between induction and consolidation chemotherapy in women with leukemia. Fertil Steril. 2011;96:1412–1414. doi: 10.1016/j.fertnstert.2011.09.038. [DOI] [PubMed] [Google Scholar]
- 35.Jahnukainen K, Mitchell RT, Stukenborg JB. Testicular function and fertility preservation after treatment for haematological cancer. Curr Opin Endocrinol Diabetes Obes. 2015;22:217–223. doi: 10.1097/MED.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 36.Curbow B, Baker F, Wingard J, Legro M, Somerfield M. Loss and recovery themes in survivors of bone marrow transplantation. J Psychosocial Oncol. 1993;10:1–20. [Google Scholar]
- 37.Nakajima Y, Kuwabara H, Kishimoto K, et al. Successful pregnancy and delivery via in vitro fertilization with cryopreserved and thawed embryo transfer in an acute myeloid leukemia patient after allogeneic bone marrow transplantation. Int J Hematol. 2015;101:417–420. doi: 10.1007/s12185-014-1709-5. [DOI] [PubMed] [Google Scholar]
- 38.Das M, Shehata F, Son WY, Son WY, Tulandi T, HOlzer H. Ovarian reserve and response to IVF and in vitro maturation treatment following chemotherapy. Hum Reprod. 2012;27:2509–2514. doi: 10.1093/humrep/des143. [DOI] [PubMed] [Google Scholar]
- 39.Abel GA, Albelda R, Khera N, et al. Financial hardship and patient-reported outcomes after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2016;22:1504–1510. doi: 10.1016/j.bbmt.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Majhail NS, Rizzo JD, Hahn T, et al. Pilot study of patient and caregiver out-of-pocket costs of allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2012;18:861–873. doi: 10.1038/bmt.2012.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Denzen EM, Thao V, Hahn T, et al. Financial impact of allogeneic hematopoietic cell transplantation on patients and families over 2 years: results from a multicenter pilot study. Bone Marrow Transplant. 2016;5:1233–1240. doi: 10.1038/bmt.2016.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sheldon LK, Kazmi M, Klein C, Berry DL. Concerns of stem cell transplant patients during routine ambulatory assessment. Patient Prefer Adherence. 2013;7:15–20. doi: 10.2147/PPA.S38567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim W, McNulty J, Chang Y-H, et al. Financial burden after allogeneic hematopoietic cell transplantation: a qualitative analysis from the patient’s perspective. Bone Marrow Transplant. 2015;50:1259–1261. doi: 10.1038/bmt.2015.128. [DOI] [PubMed] [Google Scholar]
- 44.Foxall MJ, Gaston-Johansson F. Burden and health outcomes of family caregivers of hospitalized bone marrow transplant patients. J Adv Nurs. 1996;24:915–923. doi: 10.1111/j.1365-2648.1996.tb02926.x. [DOI] [PubMed] [Google Scholar]
- 45.Akgul N, Ozdemir L. Caregiver burden among primary caregivers of patients undergoing peripheral blood stem cell transplantation: A cross sectional study. Eur J Oncol Nurs. 2014;18:372–377. doi: 10.1016/j.ejon.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 46.Clarke SA, Skinner R, Guest J, et al. Health-related quality of life and financial impact of caring for a child with Thalassaemia Major in the UK. Child Care Health Dev. 2010;36:118–122. doi: 10.1111/j.1365-2214.2009.01043.x. [DOI] [PubMed] [Google Scholar]
- 47.Hashmi SK, Bredeson C, Duarte RF, et al. National Institutes of Health Blood and Marrow Transplant Late Effects Initiative: The Healthcare Delivery Working Group Report. Biol Blood Marrow Transplant. 2017;23:717–725. doi: 10.1016/j.bbmt.2016.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khera N, Martin P, Edsall K, et al. Patient-centered care coordination in hematopoietic cell transplantation. Blood Advances. 2017;1:1617–1627. doi: 10.1182/bloodadvances.2017008789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Committee on Cancer Survivorship: Improving Care and Quality of Life and the National Cancer Policy Board. Delivering cancer survivorship care. In: Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in translation. The National Academies Press; 2006. pp. 187–321. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1. Steering Committee members, institution and represented stakeholder group(s)
Table 2. Working Group members, institution and represented stakeholder group(s)