Abstract
Temporomandibular joint (TMJ) is one of the most used joint of the body. Moreover, it is common knowledge that TMJ may show degenerative changes 10 years earlier than other joints. Recently, the use of arthroscopic surgery is revolutionizing the classic management of TMJ pathologies. In fact, the minimal invasiveness of this procedure allows faster results and fewer complications than other procedures. In this article, we present our arthroscopic technique. In this line, we would like to emphasize that we used this approach in different temporomandibular disorders such as anchored disk syndrome, habitual dislocation of TMJ, and internal derangement. Furthermore, we wish to underline that our efforts have been rewarded with great results.
Keywords: habitual dislocation of TMJ, anchored disk syndrome, arthroscopic eminoplasty, joint stability, joint overload
The treatment of temporomandibular disorders (TMD) has always been a major challenge to the maxillofacial surgeons. 1 Although nonsurgical approach is frequently the first choice, it often fails in patients with chronic pathology. 2 Thus, numerous types of surgical procedures have been studied with the aim of reducing the symptoms caused by TMD. 2 In this light, most of these surgical techniques are based on an open approach. Nevertheless, the positive results achieved by arthroscopic techniques are changing the management of several temporomandibular joint (TMJ) pathologies. In fact, the minimal invasiveness of arthroscopic procedures associated with a faster postoperative recovery time contributes to the wide dissemination of this approach. 3 Against this backdrop, we present the technique that we used to carry out the arthroscopic eminoplasty of TMJ. We highlight that our method is based on the technique of Segami et al. 2 However, Segami et al applied this technique only in habitual dislocation of TMJ. 2 4 Thus, we introduce certain modifications of this surgical procedure and we extend its use for treating different TMD. In addition, we underline that we performed this technique in more than 70 joints. Particularly, we performed this procedure only in 18 cases. In the remainder cases, we associated the TMJ eminoplasty with other arthroscopic techniques such as myotomy and diskopexy.
Surgical Technique
All surgeries were performed under general anesthesia and nasotracheal intubation. An arthroscope, 2.2 mm and 30 degrees, produced by Dyonics (Smith & Nephew), has been used to carry out the eminoplasty of TMJ.
Surgery begins with the introduction of a 23-gauge needle in the superior joint space. Subsequently, saline solution is introduced into the joint cavity to distend the articular space. Furthermore, the aspiration of synovial fluid confirms that the gauge is correctly located into the TMJ space. At this point, the introduction of a cannula into the posterior joint space is possible due to this expansion. Notably, it is important to highlight that this cannula is approximately inserted 10 mm in front of the tragus through a pointed trocar. Moreover, an Abbocath-T 14 is inserted into the joint space with the aim to facilitate the joint washing and for enhancing the visualization of the surgical field. Once in the joint, a meticulous analysis of TMJ anatomy is mandatory. In this light, the presence of a characteristic bulge facilitates the identification of the articular eminence. Besides, chondromalacia areas are frequently observable in III, IV, and V Wilkes stages. Afterward, with triangulation technique, a second cannula is placed at 25 to 30 mm from the first cannula ( Fig. 1 ). 5 Finally, the surgical instrumentation is introduced into the articular space. Interestingly, through this cannula, a surgical debridement of chondromalacia areas of TMJ apex and eminence is performed. This debridement could be performed with surgical files or with surgical drills (2.0 Full Radius Mini Blade, Smith & Nephew). With the chondromalacia areas removed, we replace the previous instruments with an arthroscopic mill (1.9 Abrader Mini Blade, Smith & Nephew). This is an important step. In fact, with this surgical mill, we perform the eminoplasty of TMJ apex. Importantly, we would like to stress that we draw an identification mark at a depth of 2 mm (in the center of eminence and in proximity to TMJ apex) before beginning surgery. This marking serves as an anatomic reference to guide the milling of TMJ eminence ( Video 1 ). Specifically, we perform the eminoplasty with mediolateral direction. Thus, the eminoplasty is specially performed on the central and lateral zone of TMJ eminence. In light of the above, we would like to stress that the surgical milling of TMJ eminence is typically more aggressive in its lateral zone (4–5 mm). In fact, the remodelling of the medial zone should be more conservative (2–3 mm). Importantly, no studies have described a large remodelling of the medial area using arthroscopic techniques. In fact, according to Segami et al, only a minimally osteotomy should be performed in this zone of eminence to prevent intracranial perforation. 2 4 In this context, we underline that the surgical aggressiveness depends on the specific TMD and anatomical characteristics of each joint. Especially, we perform a more aggressive eminence remodelling for treating habitual dislocation of TMJ. In contrast, the eminoplasty is more conservative in the event of pathologies affecting the joint disk. Moreover, we stress that it is imperative to respect the medial and lateral wall of the eminence. The main reason for this is to try to limit external or internal displacement of mandibular condyle with the aim to improve the joint stability ( Video 2 ). In addition, it is mandatory to avoid surgical trauma of the glenoid fossa. In this line, it is important to underline that the visualization of a softer bone suggests that we are approaching the anatomical limits of the middle cranial fossa. Thus, in this context, the arthroscopic milling of the medial zone should be stopped. Indeed, iatrogenic lesions of this anatomical area could provoke an intracranial drilling. In this regard, Undt also affirmed that special care has to be taken during the surgical manipulation of the TMJ medial zone. 6 Furthermore, the arthroscopic milling should also be avoided in the upper posterosuperior portion of the eminence. The reasoning behind this statement is that surgical trauma of this area could provoke postoperative occlusal disorders. Finally, the surgical mill is removed from the anterolateral via and a synovectomy rongeur is inserted into the joint space. In fact, we also carry out a partial synovectomy of the synovial tissues presenting severe inflammatory signs. Importantly, we are quite conservative during the synovectomy. In fact, we want to prevent postoperative complications such as iatrogenic disk perforations. Moreover, before completing surgery, we remove the residues of TMJ fibrocartilage using arthroscopic files or arthroscopic forceps. Finally, a subsynovial infiltration (with dexamethasone and bupivacaine) in the posterior joint space is performed. After the surgery is finished, a dressing is applied.
Fig. 1.
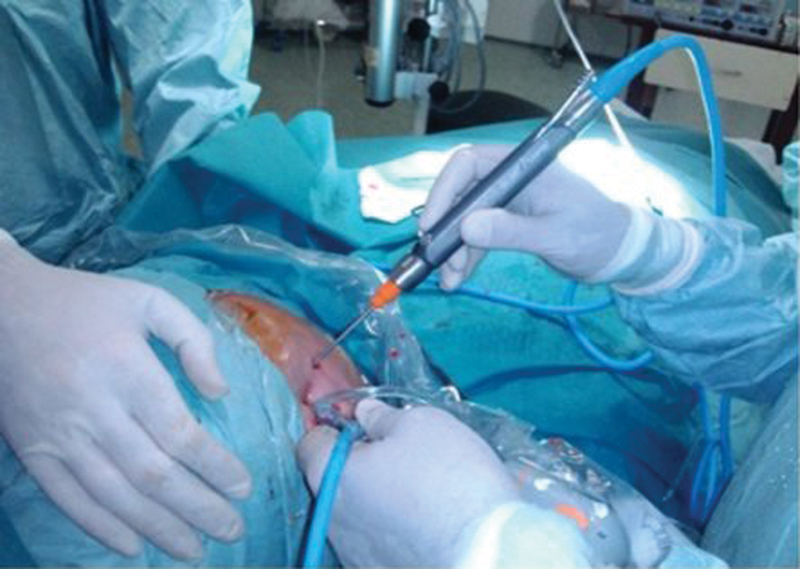
Triangulation technique used for approaching temporomandibular joint space.
Video 1
Surgical scraping of chondromalacia areas. Online content including video sequences viewable at: www.thieme-connect.com/products/ejournals/html/10.1055/s-0038-1639349 .
Video 2
Surgical milling of temporomandibular joint. Online content including video sequences viewable at: www.thieme-connect.com/products/ejournals/html/10.1055/s-0038-1639349 .
Discussion
The main goal of this article is to describe the technique that we used to perform the arthroscopic eminoplasty of TMJ. Furthermore, we want to point out that the choice of using this approach is based on some biomechanical characteristics of TMJ. In fact, we firmly believe that arthroscopic eminoplasty might improve not only the symptoms caused by some TMD but also the joint stability. Moreover, we are deeply convinced that this surgical technique could reduce the joint overload as evidenced by the following formula:
W = σ • A • ( a / h ) • Δ D ,
where σ represents the average stress, A represents the average area of the stress field (mm 2 ), a represents the average radius of the stress field (mm), h represents the average minimum condyle–fossa distance (mm), and Δ D represents the average mediolateral translation of the stress field (mm). 7
Specifically, h represents the mean condyle–fossa distance (mm). In this line, we want to show (with graphic evidence) that our technique is able to modify this specific parameter ( Figs. 2 and 3 ). In fact, the analysis of this formula shows that a decrease in h might reduce the joint overload. In addition, the integrity of the TMJ capsule-ligament system is respected with this approach. This is a very important assertion in terms of joint stability. Another key benefit of arthroscopic eminoplasty is the minimal postoperative morbidity. In fact, Sato et al reported that arthroscopic eminoplasty guarantees postsurgical recovery times faster than open surgery. Specifically, in our patients the average hospital stay was 1 day. Moreover, several authors reported the positive results that arthroscopic procedures provide in terms of TMJ pain and mouth opening. 4 In consideration of all the aforementioned points, we strongly believe that arthroscopic eminoplasty should be considered as the treatment of choice for several TMD. This is especially true when the TMJ disk or the articular eminence is actively involved in the pathology. Thus, although numerous studies showed successful outcomes with open surgery, 8 9 we believe that the open approach should be reserved for cases where arthroscopic approach failed.
Fig. 2.
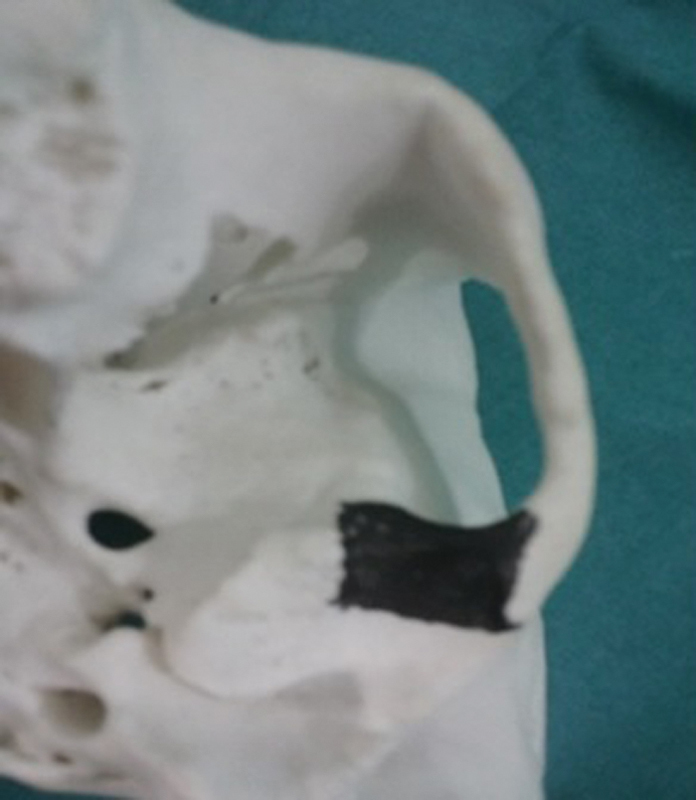
Schematic representation of arthroscopic eminoplasty.
Fig. 3.

Schematic representation of arthroscopic eminoplasty result.
With this idea in mind, we extended the use of arthroscopic eminoplasty for treating some TMD such as anchored disk syndrome, TMJ habitual dislocation, and internal derangement. Interestingly, we would like to stress that this procedure showed brilliant results in patients with TMJ internal derangement. Specifically, our data showed that TMJ pain (measured 6 months before surgery) was higher ( p < 0.01) than the pain registered 18 months after surgery. Moreover, postoperative mouth opening was also greater than preoperative mouth opening ( p < 0.01). 10 In conclusion, we emphasize that this report contains three points that are central to us: first, arthroscopic eminoplasty could reduce the joint overload and the stress acting on TMJ disk. Second, this procedure allows to maintain joint stability. In fact, it is able to increase the joint amplitude without detaching the capsule-ligament system of the joint ( Fig. 4 ). Third, we want to point out that this technique is characterized by extremely low levels of postoperative morbidity. Despite all that have been previously discussed, we want to stress that the realization of an arthroscopic procedure is not a simple task. In many cases, the learning curve is long. However, this long learning period which is considered as an obstacle must be understood as a challenge for all maxillofacial surgeons. Only in this way we will achieve a change in the diffusion of arthroscopic procedures.
Fig. 4.
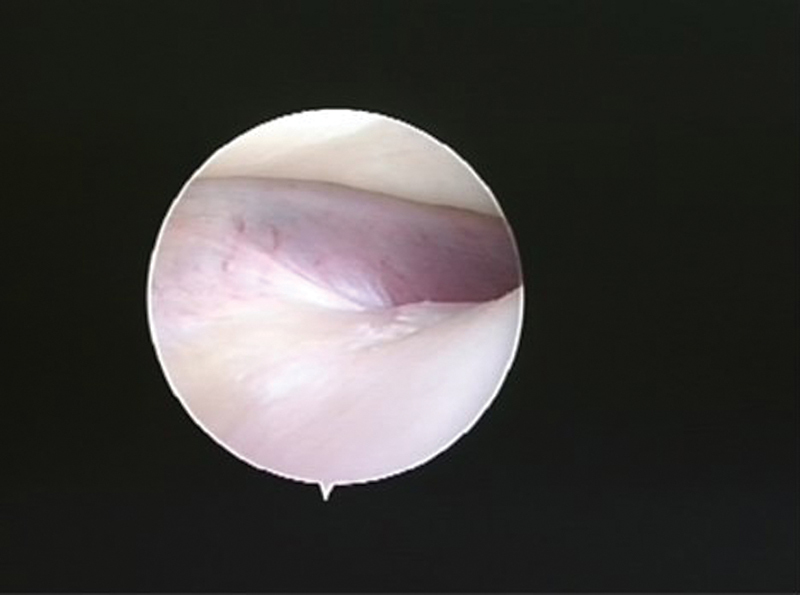
arthroscopic vision of temporomandibular joint space. This image shows temporomandibular joint disk and eminence.
Funding Statement
Funding The authors did not receive any financial assistance.
Conflict of Interest The authors declare that they have no conflict of interests.
Ethical Standards
The authors declare that they have taken into account the ethical responsibilities.
Authors' Contributions
All the authors participated in the creation of the manuscript.
Informed Consent
All patients agreed to participate in the study, and all of the participants signed the informed consent.
References
- 1.Ingawalé S, Goswami T. Temporomandibular joint: disorders, treatments, and biomechanics. Ann Biomed Eng. 2009;37(05):976–996. doi: 10.1007/s10439-009-9659-4. [DOI] [PubMed] [Google Scholar]
- 2.Segami N, Kaneyama K, Tsurusako S, Suzuki T. Arthroscopic eminoplasty for habitual dislocation of the temporomandibular joint: preliminary study. J Craniomaxillofac Surg. 1999;27(06):390–397. doi: 10.1054/jcms.2000.0086. [DOI] [PubMed] [Google Scholar]
- 3.Moses J J. Current concepts, rationale and techniques in TMJ arthroscopic surgery. J Oral Maxillofac Surg. 2007;65(09):96. [Google Scholar]
- 4.Sato J, Segami N, Nishimura M, Suzuki T, Kaneyama K, Fujimura K. Clinical evaluation of arthroscopic eminoplasty for habitual dislocation of the temporomandibular joint: comparative study with conventional open eminectomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(04):390–395. doi: 10.1067/moe.2003.128. [DOI] [PubMed] [Google Scholar]
- 5.Tsuyama M, Kondoh T, Seto K, Fukuda J.Complications of temporomandibular joint arthroscopy: a retrospective analysis of 301 lysis and lavage procedures performed using the triangulation technique J Oral Maxillofac Surg 20005805500–505., discussion 505–506 [DOI] [PubMed] [Google Scholar]
- 6.Undt G. Temporomandibular joint eminectomy for recurrent dislocation. Atlas Oral Maxillofac Surg Clin North Am. 2011;19(02):189–206. doi: 10.1016/j.cxom.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Gallo L M, Chiaravalloti G, Iwasaki L R, Nickel J C, Palla S. Mechanical work during stress-field translation in the human TMJ. J Dent Res. 2006;85(11):1006–1010. doi: 10.1177/154405910608501106. [DOI] [PubMed] [Google Scholar]
- 8.Cascone P, Ungari C, Paparo F, Marianetti T M, Ramieri V, Fatone M. A new surgical approach for the treatment of chronic recurrent temporomandibular joint dislocation. J Craniofac Surg. 2008;19(02):510–512. doi: 10.1097/SCS.0b013e318163e42f. [DOI] [PubMed] [Google Scholar]
- 9.Wolford L M. Clinical indications for simultaneous TMJ and orthognathic surgery. Cranio. 2007;25(04):273–282. doi: 10.1179/crn.2007.041. [DOI] [PubMed] [Google Scholar]
- 10.Garcia Medina B, Cariati P, Galvez P, Cabello Serrano A, Garcia Martin M. Arthroscopic eminoplasty: a new choice of treatment for TMJ internal derangement. Minerva Stomatol. 2017;66(04):141–147. doi: 10.23736/S0026-4970.17.04065-1. [DOI] [PubMed] [Google Scholar]


