Abstract
Severely atrophic mandible fractures are frequently a challenge to treat. Virtual surgical planning (VSP) uses three-dimensional computed tomographic (CT) scans that can be translated into stereolithographic models to fabricate surgical templates, facilitating intraoperative procedures. The purpose of this article is to describe the reconstruction of two cases of severe atrophic mandible fracture using VSP. Two elderly edentulous/partially dentate patients who presented with fractures of their mandibles and who underwent reconstruction using VSP were included. Both had Class III atrophy at the region of the fracture. While both fractures were complex, the mechanism of injury differed with one being a tractor accident and the other being a pathologic fracture. Both patients presented with critical medical conditions. CT scans were obtained on both. The displaced segments were aligned virtually using mirror images and the midline of the maxilla. Three-dimensional models were fabricated to allow preoperative contouring of 2.5-mm reconstruction plates. Patients were operated under general anesthesia and fractures reduced and stabilized with 2.5-mm reconstruction plates placed at the lateral border of the mandible. Average treatment time for both patients was a little over 2 hours. There was good reduction with both. VSP is a valuable tool to assess and reduce complex fractures with less surgical time and predictable results.
Keywords: facial trauma, mandibular fractures, mandibular atrophy, virtual surgical planning
Virtual surgical planning (VSP) is a tool which uses computed tomographic (CT) scans that can be translated into stereolithographic models facilitating intraoperative management of patients. 1 The implementation of this technology has allowed surgeons to plan and execute complex cases in a more precise fashion with the added benefit of decreasing surgical time. 2
Currently, maxillofacial use of VSP includes orthognathic surgery, mandibular and maxillary defects in need of reconstruction with free flaps, and complex trauma. 2 3 4 5 6 7 8 As this technology is intended to facilitate the reconstruction of bizarre craniomaxillofacial injuries or defects, the native tissues are usually malpositioned, injured, compromised by multiple surgeries, absent, irradiated, or severely atrophied. 9
The repair/reconstruction of severe atrophic mandible fractures (SAMF) in an elderly population presents a significant challenge because the tridimensional loss of bone limits accurate anatomic reduction. Loss of teeth and anatomical references complicate management and in addition, these patients frequently have comorbidities that occur with the aging process. 10
Techniques that have been employed to treat atrophic mandible fractures include splints, external pins, and rigid fixation with and without grafting. 10 11 12 Although VSP has been reported in orthognathic surgery, complex trauma, and reconstructive surgery, currently there is a minimal documentation of its use in elderly patients with SAMF. The purpose of this article is to describe the repair/reconstruction of two patients with SAMF using VSP.
Patients and Methods
Two elderly patients with severely atrophic edentulous/partially dentate mandible fractures which were severely displaced with several co-moieties were included in this review. As a case study of two patients, this review was classified as exempt by the University of Kentucky Institutional Review Board (IRB).
Case 1
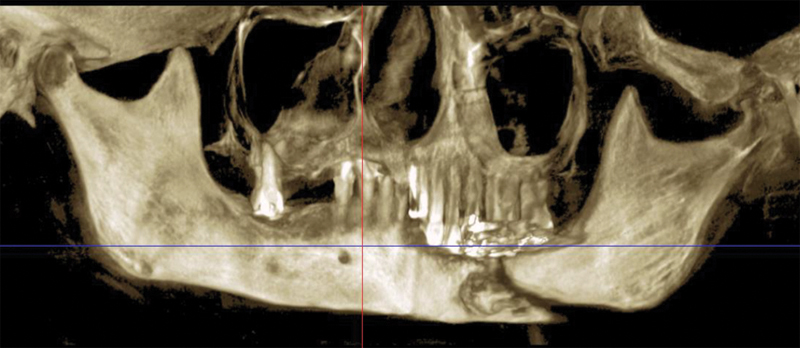
A 72-year-old male patient involved in a roll over tractor accident presented to an outside hospital where he was intubated. Injuries included right upper extremity degloving injury and multiple unstable cervical spine injuries of anterior and posterior columns requiring fusion of C5–T1. It was elected by the spine service not to fuse C2 to allow him rotation of his neck. A CT scan revealed bilateral intracapsular condylar head fractures, a left comminuted mandible fracture, and complex nasal fracture ( Fig. 1a–c ). Additionally, he had a transverse body fracture of C2 and C5 through T1. The patient was transferred to the University of Kentucky for further management.
Fig. 1.
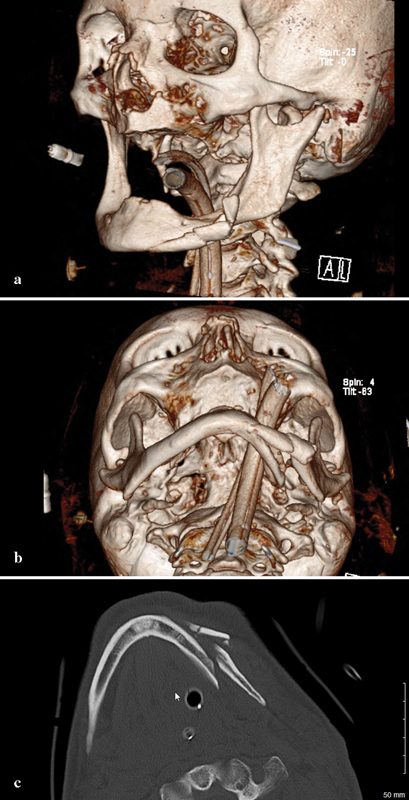
( a ) 3D preoperative CT reconstruction of the injury from a three-fourths view. Note the intracapsular head fracture on the left. ( b ) Submental vertex view showing displacement and comminution. ( c ) Axial CT showing comminution. As the maxillary fracture was minimally displaced, the authors believed that any discrepancies would be resolved with an eventual prosthesis.
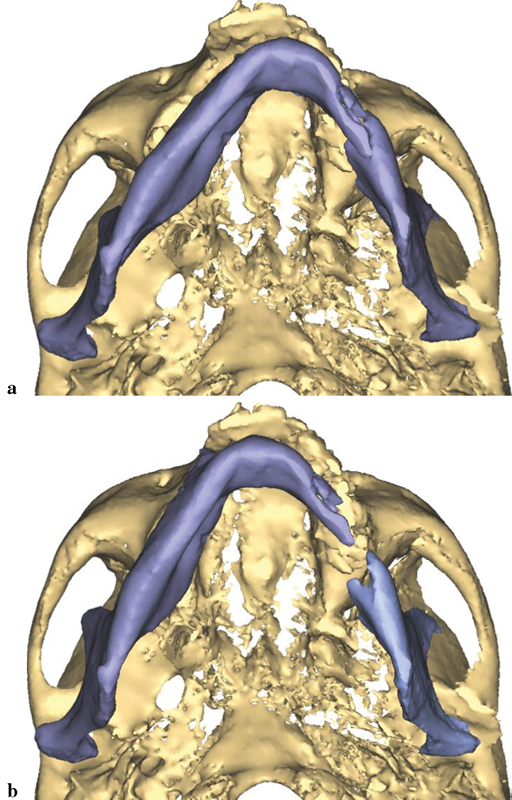
Owing to the significant injury to the anterior and posterior column of the cervical spine, a fusion was performed of C5–T1. Prior to surgery, he was kept in a cervical spine collar. To minimize the time in the operating room (OR) and manipulation of the displaced, atrophic mandible, his initial CT scans were used to fabricate a model to facilitate the correction of the complex mandible fracture. Turnaround time was 5 days. Using three-dimensional (3D) software for VSP (Materialize, Plymouth, MI), the midline of the larger segment of the mandible was aligned with the midline of the maxilla ( Fig. 2a, b ). A mirror image was created using the opposing uninjured mandibular body ( Fig. 3a, b ). A stereolithographic model was fabricated facilitating the preoperative bending of a 2.5-mm reconstruction plate, based on the virtually planned model ( Fig. 4 ). The plate was contoured to the model the evening before surgery.
Fig. 2.
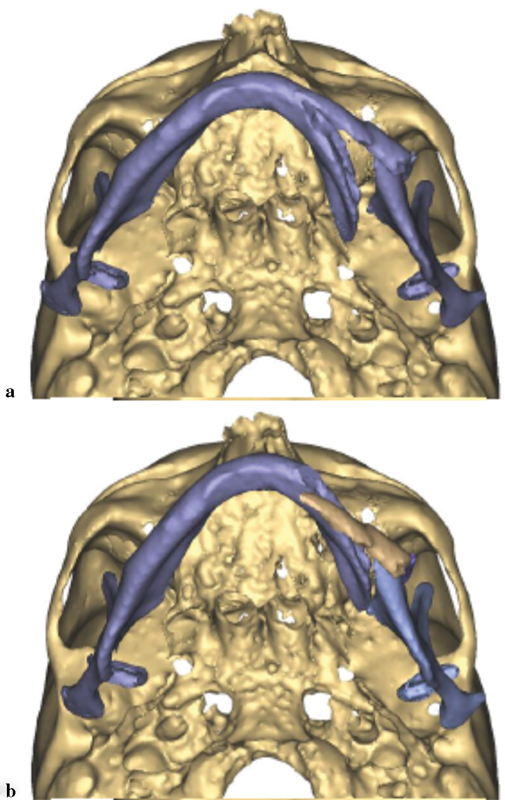
( a ) Preoperative submental image prior to manipulation. ( b ) Midline of mandible aligned with midline of the maxilla.
Fig. 3.
( a ) A mirror image as seen from frontal. ( b ) Mirror image as seen from submental vertex.
Fig. 4.

Plate contoured to mandible.
As both condylar head fractures were very high (at or within the capsule), the most important part of his postsurgical therapy was function. Later, when he was fully alert following surgery, he was kept on a soft mechanical diet and physical therapy with range of motion exercises instituted. He had good mouth opening and range of motion despite the intracapsular fractures.
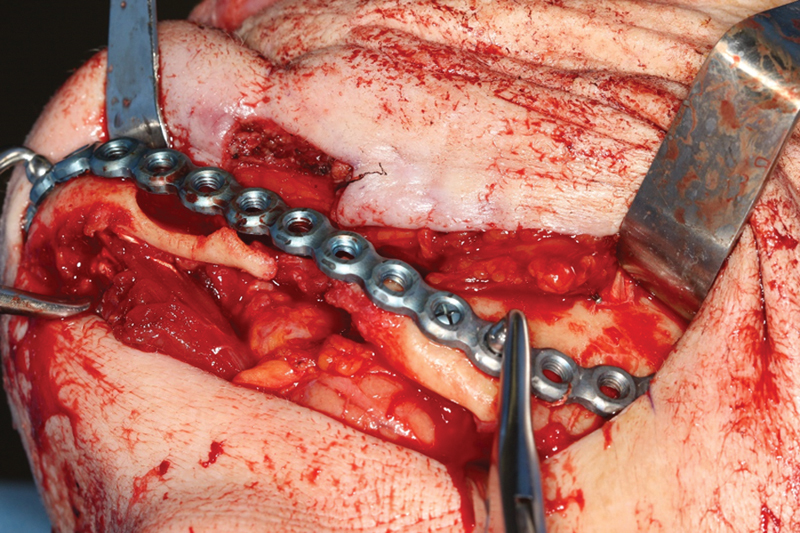
In the OR, the oral endotracheal tube was switched out with a bougie atraumatically. In-line stabilization of his c-spine was completed with tape over the forehead secured to the operating table and 1 L “sand bags” placed on either side of his neck. The mandibular body fracture was exposed using an apron neck incision. Then, a temporary inferior border plate was used to align the segments. The prefabricated reconstruction plate was then placed with four bicortical screws placed in the proximal and distal segments leaving four additional holes over the area of commination ( Fig. 5 ). The temporary plate placed at the inferior border was removed. His function was observed and it was noted that his mandible moved freely. Neurologic checks postoperatively showed no change. The total time from the start of the incision to closure of the wounds was 2 hours and 30 minutes.
Fig. 5.
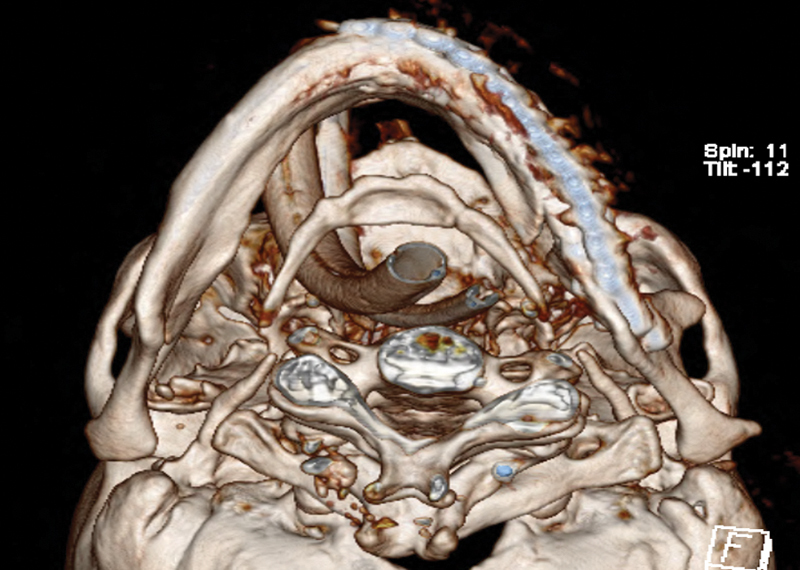
Postoperative 3D submental vertex view with plate in place.
Case 2
A 70-year-old female patient presented as an outpatient for definitive treatment of her pathologic mandibular fracture, orocutaneous fistula, and chronic osteomyelitis. Clinically, she had a draining orocutaneous fistula in the submental region which communicated intraorally at the left lingual border of the mandible. The left mandibular body was mobile and her chin was deviated 2 cm to the left. She had a severely atrophied mandible in the area of the fracture with poor remaining dentition. A cone beam computed tomography (CBCT) was obtained. The approximate defect was measured at 4 to 5 cm in the left body ( Fig. 6 ).
Fig. 6.
Pathologic fracture with displacement of the minor segment.
The patient's medical history includes chronic obstructive pulmonary disease (COPD), mitral valve prolapse, coronary artery disease (CAD), anxiety, depression, gait disturbance, malnutrition, and gastroesophageal reflux disease (GERD). She has a demand pacemaker in place. Her mandible had fractured following removal of a carious infected bicuspid. Her referral was delayed for 6 months while she was treated for osteomyelitis. She had a peripherally inserted central catheter (PICC) line and was undergoing 12 weeks of intravenous (IV) daptomycin and ertapenem. Upon finishing 12 weeks of IV antibiotic therapy, she was placed on oral bactrim and augmentin until surgery.
Owing to the comorbidities and her difficulty ambulation, it was felt that she would be at high risk for an autogenous hip graft and the associated increased time under general anesthesia. It was decided to debride her mandible and simultaneously reconstruct it with a locking reconstruction plate with placement of an alloplastic graft to replace the bone defect.
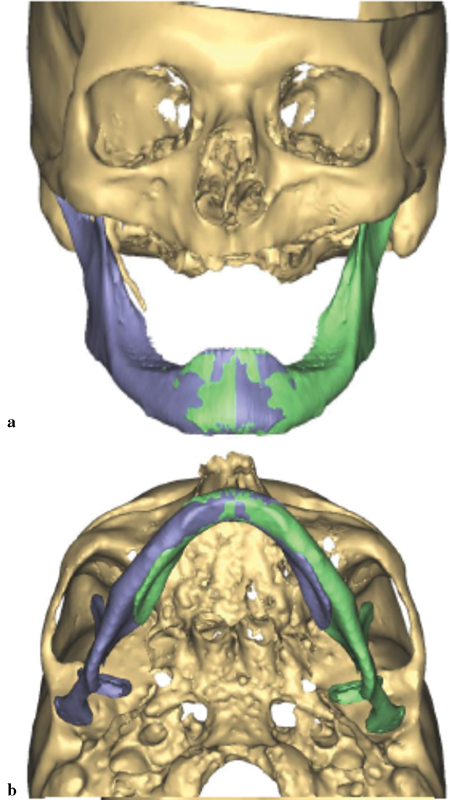
Prior to surgery, VSP was implemented to plan the procedure (Materialize, Plymouth, MI). A CBCT was obtained. Similar to the previous case, the midline of the major segment was aligned with the midline of the maxilla ( Fig. 7a, b ). The displaced smaller segment was placed in the glenoid fossa and the inferior borders were aligned. A mirror image of the unaffected right side of the mandible was then superimposed. The area of lytic bone was outlined and a model was fabricated. A 2.5-mm locking reconstruction plate was prebent according to the 3D model using the mirror image model with enough length to span the area that would be reconstructed ( Fig. 8 ).
Fig. 7.
( a ) Displacement of the jaw prior to manipulation. ( b ) Alignment of the midline of the mandible with the maxilla revealing the large defect on the jaw lateral border.
Fig. 8.

Model made from mirror image with defect filled in.
In the OR, a left-sided transcervical approach was performed to the left mandible with a fistulectomy. The tissue surrounding the fistula was friable probably due to the long time that it has been present. In addition, there were fragments of devitalized bone present when the wound was opened. The fistula was excised and included into the incision.
Debridement of the fibrous callous and a minimal amount of bone was removed. The soft-tissue scars were released and the bony segments were placed near their normal position and the prefabricated 2.5-mm locking reconstruction plate was applied ( Fig. 9 ). The dissection was subperiosteal due to the need to debride the bone. While Luhr's principle of supraperiosteal dissection and its use in atrophic mandible fractures was discussed prior to surgery, it was felt that it would be difficult to achieve it with devitalized bone fragments present and the need to immediately graft the area due to the continuity defect. The bony defect was replaced with an alloplastic material and a mixture of BMP and β-tricalcium phosphate. The tissue was undermined to allow for soft-tissue coverage over the plate. Postoperative images show good restoration of the segments ( Fig. 10a, b ). The total time of the procedure was 2 hours and 26 minutes.
Fig. 9.
Intraoperative initial placement of the plate.
Fig. 10.
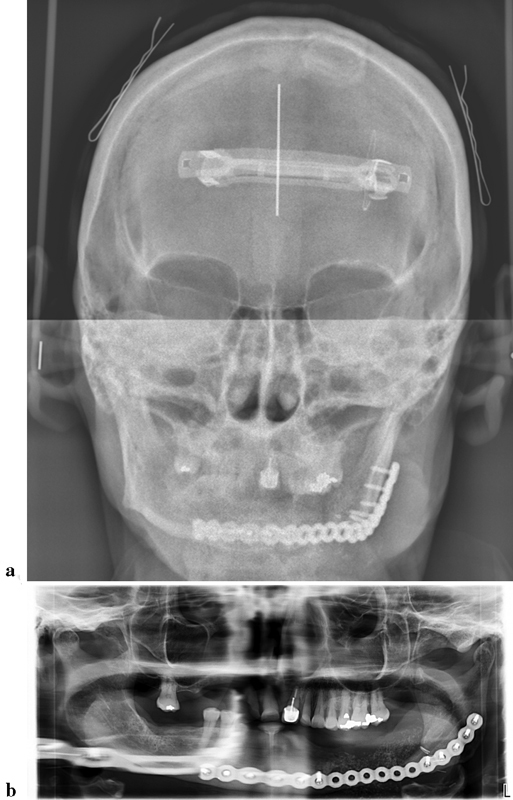
( a ) Frontal radiograph showing alignment of the mandible. ( b ) Panoramic radiograph with plate in place and alloplastic material present.
Discussion
The primary objective of this article was to describe the reconstruction of SAMF using VSP. To accomplish such aim, the authors reviewed and presented two patients seen at the University of Kentucky. They were both treated without intraoperative or postoperative complications. From the operative standpoint, VSP fulfilled the proposed goals of reducing surgical time and guiding the realignment of displaced, atrophic mandibular bone segments with precision and predictability.
Bone resorption in edentulous alveolar processes is a chronic, progressive, and irreversible condition occurring in all individuals following the loss of the dentition. 13 Hence, as the geriatric population continues to increase with a concomitant loss of teeth, surgeons are more likely to see fractures of the atrophic edentulous mandible. 14 15 16 To better understand the biological process taking place in mandibular atrophy and to allow for improved treatment plans, several classification methods have been presented to classify the degree of atrophy of partially or fully edentulous mandibles. 17 18 19 20 21 22 23
In 1996, Luhr et al 24 classified the atrophic mandible in to Class I, Class II, and Class III, according to the degree of atrophy ( Fig. 11 ). Both of our patients were classified as Class III atrophy at the site of the injury. As with previous studies, the group of Luhr et al noted that more severely atrophic mandible fractures had a higher incidence of complications. 24 In 2010, Van Sickels and Cunningham presented their results with Class II and III atrophic mandible fractures using prefabricated reconstruction plates placed at the inferior border of the mandible. 10 Plates were contoured prior to surgery on stock plastic models and modified in the OR to account for differences in anatomy. VSP was not used in their study, but the authors felt that operative time was decreased with having the plates contoured prior to being in the OR.
Fig. 11.
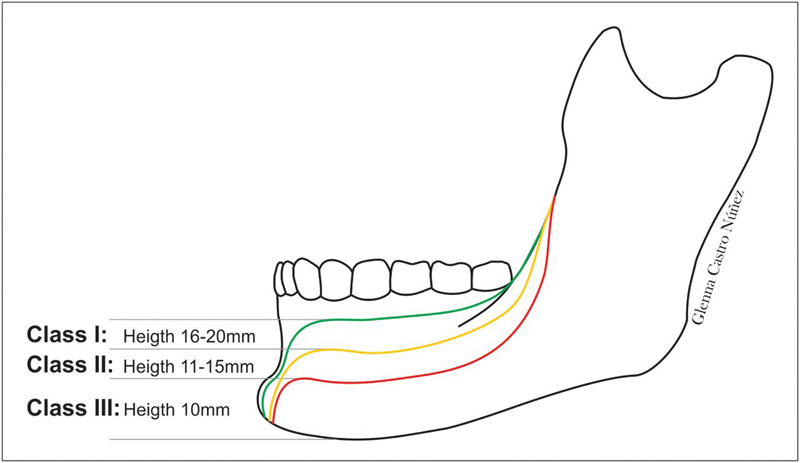
Classification of the atrophic mandible by Luhr et al. 24 Drawing by Glenna Castro.
Using VSP models and contouring the plates on an exact or nearly exact model of the patient was more accurate than our previous research and also greatly decreased operating time. As with our preceding work, we believe that large load-bearing plates are necessary to treat patients with atrophic mandible fractures. 10 12 Decreasing surgical time in patients with concomitant medical concerns should not be ignored. This was, in fact, a major consideration in both of our cases, where there were pulmonary and cardiac issues. Scott felt that a prudent surgical team must put in perspective such systemic conditions to avoid further complications, as undergoing general anesthesia in the geriatric patient is a risk factor by itself, with morbidity occurring four times more often in older patients than in younger patients. 25
Our second patient not only had a prebent plate fabricated off of a mirror image model but an alloplastic material was also used to reconstruct her 4.0-cm defect on the lateral aspect of mandible. While controversial, given her comorbidities, it was considered prudent to avoid the morbidity of a second surgical site and to further compromise her ability to ambulate. While dental implants may be considered in the future, the goal was to reconstruct a continuity fracture defect in a medically compromised patient who had a problem for 9 months.
Mandibular fractures are often associated with trauma and are more frequently seen in young men. They represent 20 to 60% of all facial fractures. Accidents usually account for a higher percentage of the causative factor. 26 27 28 29 This demographic features usually change in an elderly population, where an atrophic mandible predisposed the mandible to fracture with more minor insults. The etiology of the fractures differs in our two patients, one a relatively high-energy roll over tractor injury and the second a delayed fracture secondary to an extraction of a pathologic tooth.
Treatment modalities for atrophic mandible fractures include observation, closed reduction, Gunning splits, external pix fixation, and open reduction and internal fixation (ORIF) with titanium mesh, locking miniplate, or 2.4-reconstruction plate. It has been customary at our institution to use large load-bearing 2.5-mm reconstruction plates to provide primary stability and allow the patient to return to immediate function. 30 In both cases presented in this article, we described the use of 2.5-mm locking reconstruction plates being bent to a prefabricated model.
Conclusion
The management of SAMF is challenging and the literature supports the concept that treatment decisions should continue to be based on the clinician's previous experience. 31 Nevertheless, newer technology, such as VSP, can improve the outcomes and decrease the time in the OR. In SAMF with severe displacement of the segments or large defects, VSP allows mirror imaging, allowing the alignment of segments and the replacement of missing parts. While other research has reported the use of VSP in facial trauma, 2 8 32 there are few studies that describe the use of VSP in SAMF. 9 33 We agree with the results seen by these authors that VSP assists the surgeon to better plan and execute ORIF in SAMF, employing less surgical time with predictable results and reestablishing mandibular alignment, shape, and projection.
References
- 1.Neumann P, Siebert D, Schulz A et al. Using virtual reality techniques in maxillofacial surgery planning. Virtual Real (Walth Cross) 1999;4:213–222. [Google Scholar]
- 2.Saad A, Winters R, Wise M W, Dupin C L, St Hilaire H. Virtual surgical planning in complex composite maxillofacial reconstruction. Plast Reconstr Surg. 2013;132(03):626–633. doi: 10.1097/PRS.0b013e31829ad299. [DOI] [PubMed] [Google Scholar]
- 3.Swennen G R, Mollemans W, Schutyser F. Three-dimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg. 2009;67(10):2080–2092. doi: 10.1016/j.joms.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Hirsch D L, Garfein E S, Christensen A M, Weimer K A, Saddeh P B, Levine J P. Use of computer-aided design and computer-aided manufacturing to produce orthognathically ideal surgical outcomes: a paradigm shift in head and neck reconstruction. J Oral Maxillofac Surg. 2009;67(10):2115–2122. doi: 10.1016/j.joms.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Roser S M, Ramachandra S, Blair H et al. The accuracy of virtual surgical planning in free fibula mandibular reconstruction: comparison of planned and final results. J Oral Maxillofac Surg. 2010;68(11):2824–2832. doi: 10.1016/j.joms.2010.06.177. [DOI] [PubMed] [Google Scholar]
- 6.Antony A K, Chen W F, Kolokythas A, Weimer K A, Cohen M N. Use of virtual surgery and stereolithography-guided osteotomy for mandibular reconstruction with the free fibula. Plast Reconstr Surg. 2011;128(05):1080–1084. doi: 10.1097/PRS.0b013e31822b6723. [DOI] [PubMed] [Google Scholar]
- 7.Tepper O M, Sorice S, Hershman G N, Saadeh P, Levine J P, Hirsch D. Use of virtual 3-dimensional surgery in post-traumatic craniomaxillofacial reconstruction. J Oral Maxillofac Surg. 2011;69(03):733–741. doi: 10.1016/j.joms.2010.11.028. [DOI] [PubMed] [Google Scholar]
- 8.Zheng G S, Su Y X, Liao G Q et al. Mandible reconstruction assisted by preoperative virtual surgical simulation. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(05):604–611. doi: 10.1016/j.tripleo.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Kupfer P, Saadad N, Hughes P J. Open reduction and internal fixation of bilateral atrophic mandible fractures utilizing virtual surgical planning, custom cutting guides and reconstruction plate. A case report. J Oral Maxillofac Surg. 2016;74:e89. [Google Scholar]
- 10.Van Sickels J E, Cunningham L L. Management of atrophic mandible fractures: are bone grafts necessary? J Oral Maxillofac Surg. 2010;68(06):1392–1395. doi: 10.1016/j.joms.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 11.Buchbinder D. Treatment of fractures of the edentulous mandible, 1943 to 1993: a review of the literature. J Oral Maxillofac Surg. 1993;51(11):1174–1180. doi: 10.1016/s0278-2391(10)80285-x. [DOI] [PubMed] [Google Scholar]
- 12.Tiwana P S, Abraham M S, Kushner G M, Alpert B. Management of atrophic edentulous mandibular fractures: the case for primary reconstruction with immediate bone grafting. J Oral Maxillofac Surg. 2009;67(04):882–887. doi: 10.1016/j.joms.2007.11.038. [DOI] [PubMed] [Google Scholar]
- 13.Carlsson G E. Clinical morbidity and sequelae of treatment with complete dentures. J Prosthet Dent. 1998;79(01):17–23. doi: 10.1016/s0022-3913(98)70188-x. [DOI] [PubMed] [Google Scholar]
- 14.Madsen M J, Haug R H, Christensen B S, Aldridge E.Management of atrophic mandible fractures Oral Maxillofac Surg Clin North Am 20092102175–183., v [DOI] [PubMed] [Google Scholar]
- 15.Ellis E, III, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. 2008;66(03):421–435. doi: 10.1016/j.joms.2007.08.042. [DOI] [PubMed] [Google Scholar]
- 16.Benech A, Nicolotti M, Brucoli M, Arcuri F. Intraoral extra-mucosal fixation of fractures in the atrophic edentulous mandible. Int J Oral Maxillofac Surg. 2013;42(04):460–463. doi: 10.1016/j.ijom.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Landa J S. Classification of mandibular resorption. Dent Radiogr Photogr. 1967;40(03):62–65. [PubMed] [Google Scholar]
- 18.Atwood D A. Reduction of residual ridges: a major oral disease entity. J Prosthet Dent. 1971;26(03):266–279. doi: 10.1016/0022-3913(71)90069-2. [DOI] [PubMed] [Google Scholar]
- 19.Mercier P, Lafontant R. Residual alveolar ridge atrophy: classification and influence of facial morphology. J Prosthet Dent. 1979;41(01):90–100. doi: 10.1016/0022-3913(79)90363-9. [DOI] [PubMed] [Google Scholar]
- 20.Seibert J S. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part I. Technique and wound healing. Compend Contin Educ Dent. 1983;4(05):437–453. [PubMed] [Google Scholar]
- 21.Lekholm U, Zarb G A. Patient selection and preparation. Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry. In: Branemark P I, Zarb G A, Albrektsson T, editors. Chicago, IL: Quintessence Publishing Company; 1985. pp. 199–209. [Google Scholar]
- 22.Misch C E, Judy K W. Classification of partially edentulous arches for implant dentistry. Int J Oral Implantol. 1987;4(02):7–13. [PubMed] [Google Scholar]
- 23.Cawood J I, Howell R A. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17(04):232–236. doi: 10.1016/s0901-5027(88)80047-x. [DOI] [PubMed] [Google Scholar]
- 24.Luhr H G, Reidick T, Merten H A.Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases J Oral Maxillofac Surg 19965403250–254., discussion 254–255 [DOI] [PubMed] [Google Scholar]
- 25.Scott R F.Oral and maxillofacial trauma in the geriatric patient Fonseca R J, Walker R V.Oral and Maxillofacial Trauma. 2nd ed2;Philadelphia, PA: Saunders; 19971045–1072. [Google Scholar]
- 26.Bruce R A, Ellis E., III The second Chalmers J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1993;51(08):904–911. doi: 10.1016/s0278-2391(10)80113-2. [DOI] [PubMed] [Google Scholar]
- 27.Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31(01):51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 28.Wittwer G, Adeyemo W L, Turhani D, Ploder O. Treatment of atrophic mandibular fractures based on the degree of atrophy--experience with different plating systems: a retrospective study. J Oral Maxillofac Surg. 2006;64(02):230–234. doi: 10.1016/j.joms.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 29.Pombo M, Luaces-Rey R, Pértega S et al. Review of 793 facial fractures treated from 2001 to 2008 in a Coruña University Hospital: types and etiology. Craniomaxillofac Trauma Reconstr. 2010;3(01):49–54. doi: 10.1055/s-0030-1249373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marciani R D. Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg. 2001;59(07):792–795. doi: 10.1053/joms.2001.24736. [DOI] [PubMed] [Google Scholar]
- 31.Nasser M, Fedorowicz Z, Ebadifar A. Management of the fractured edentulous atrophic mandible. Cochrane Database Syst Rev. 2007;24(01):CD006087. doi: 10.1002/14651858.CD006087.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Hanasono M M, Jacob R F, Bidaut L, Robb G L, Skoracki R J. Midfacial reconstruction using virtual planning, rapid prototype modeling, and stereotactic navigation. Plast Reconstr Surg. 2010;126(06):2002–2006. doi: 10.1097/PRS.0b013e3181f447e1. [DOI] [PubMed] [Google Scholar]
- 33.Broyles J M, Wallner C, Borsuk D E, Dorafshar A H. The role of computer-assisted design and modeling in an edentulous mandibular malunion reconstruction. J Craniofac Surg. 2013;24(05):1835–1838. doi: 10.1097/SCS.0b013e3182997f50. [DOI] [PubMed] [Google Scholar]


