Abstract
Objective
Analyze the percutaneous fixation technique for scaphoid fractures in the waist of the scaphoid and the proximal pole, and demonstrate its result.
Methods
A retrospective cross-cohort study conducted from January 2005 to April 2015, aiming at the consolidation time, epidemiological profile, level of function, return to work, and complications.
Results
Twenty-eight patients were selected, with a mean of eight weeks of follow-up. They presented a mean age of 30.5 years, male prevalence (25 patients; 89.2%), and no differences between dominant and non-dominant sides. The mean time from diagnosis was 4.16 weeks, but in three cases of fibrous union, the pre-operative period was over one year. The most frequent mechanism of injury was a fall on the outstretched hand, in 22 cases (78.5%). Of all fractures, 24 cases were in the waist (85.8%) and four were of the proximal pole (14.2%); seven patients had displacement (25%). There was consolidation in 26 cases (92.8%) with a mean of 7.5 weeks after surgery. In cases of non-union, radiological follow-up was up to 24 weeks, requiring a new surgical intervention.
Conclusions
Percutaneous fixation is an excellent, reproducible technique that allows early active mobility of the wrist with a low complication rate, although it requires a learning curve.
Keywords: Bone fractures, Scaphoid bone, Bone screws, Internal fixation of fractures
Resumo
Objetivo
Analisar a técnica de fixação percutânea das fraturas do escafoide em seu terço médio e terço proximal e demonstrar seu resultado.
Métodos
Estudo retrospectivo de coorte transversal, feito de janeiro de 2005 a abril de 2015, com vistas ao tempo de consolidação, perfil epidemiológico, grau de função, retorno às atividades laborais e complicações.
Resultados
Foram selecionados 28 pacientes, com seguimento médio de oito semanas. Este estudo evidenciou uma idade média de 30,5 anos, prevalência do sexo masculino em 25 pacientes (89,2%) e ausência de lado dominante. O tempo médio de diagnóstico foi de 4,16 semanas, porém três casos de união fibrosa apresentaram período pré-operatório superior a um ano. O mecanismo de trauma mais frequente foi a queda sobre o punho em 22 casos (78,5%). Das fraturas, 24 casos foram do terço médio (85,8%) e quatro casos do polo proximal (14,2%), sete casos apresentavam desvio (25%). Houve consolidação de 26 casos (92,8%) com tempo médio de 7,5 semanas de pós-operatório. Nos casos de não consolidação radiológica, o seguimento foi de até 24 semanas, foi necessária uma nova intervenção cirúrgica.
Conclusões
A fixação percutânea é uma ótima maneira de tratar esse tipo de fratura, reprodutível, permite a mobilidade ativa precoce do punho com baixo índice de complicações, embora exija curva de aprendizagem.
Palavras-chave: Fraturas ósseas, Osso escafoide, Parafusos ósseos, Fixação interna de fraturas
Introduction
Scaphoid fractures are common injuries in emergency settings, accounting for 11% of all hand fractures and 60% of carpal fractures1; 80% of the scaphoid surface is covered by cartilage, and 70%–80% of its arterial supply is provided by branches of the radial artery, entering its dorsal crest in a predominantly retrograde flow.2
Young men between the ages of 15 and 40 are the most affected; the incidence in individuals younger than 10 years is low. Hyperextension trauma with ulnar deviation is the most common mechanism of injury. Falls, automobile accidents, or sport-related accidents are the main causes of this type of fracture.3
Many minimally dislocated fractures are not visible on radiographs; these cases may present a risk of nonunion.4 In the study by Wong and von Schroeder,5 in a series of 88 cases of patients diagnosed with scaphoid nonunion, 17% of cases did not present radiographs that were conclusive of fractures at admission, i.e., many cases are not diagnosed in the emergency room.
The most common clinical sign of scaphoid nonunion is restricted wrist mobility. Furthermore, the presence of pain in the region of the anatomical snuffbox (aka radial fossa) and dorsum of the wrist (mainly during movement) and a decrease in strength can also be observed.3, 6 The natural history of non-surgically treated scaphoid fractures presents an increase in the incidence of post-traumatic arthritis in 97% of patients five years after the trauma.7, 8 Non-dislocated scaphoid waist fractures that are conservatively treated present a malunion incidence of around 5%–12%.9, 10 Conservatively treated scaphoid waist fractures with dislocation greater than 1 mm present a malunion rate that ranges from 45% to 92%.11, 12, 13, 14, 15
Finally, proximal pole fractures may have the greatest risk of nonunion or avascular necrosis. The explanation for this fact is that the artery supplying the proximal pole is injured in this type of fracture, where 70% of the circulation is retrograde.2, 6 Therefore, the incidence of nonunion reaches 90% in proximal pole fractures.16, 17, 18
However, authors such as Vinnars et al.,19 Bond et al.10 and Dias et al.20 indicate that the non-surgical treatment of scaphoid fractures is limited to cases of non-dislocated fractures, reaching 95%–100% of good consolidation in up to 12 weeks. Furthermore, the same authors warn that treatments comprising 9–12 weeks of immobilization are not free of complications, despite the good levels of bone union. This time of immobilization causes muscular atrophy and a decrease in strength, leading to an increase in the degree of joint stiffness of the wrist, which in turn requires a longer rehabilitation time. Thus, Rettig and Kollias21 recommend a more aggressive treatment in cases of non-dislocated or minimally dislocated fractures, especially in athletes.
Minimally invasive techniques may limit the arterial damage observed in open surgeries, and would theoretically increase the chance of fracture union.10, 21, 22 The reduction of surgical trauma has improved the care and recovery of these patients, and some authors have noted a rapid return to work.10, 22, 23, 24
This study is aimed at analyzing the percutaneous fixation technique for waist and proximal scaphoid fractures, considering the time of consolidation, epidemiological profile (age, gender, side, and mechanism of trauma), degree of function, complications, and return to work.
Material and methods
This retrospective cross-sectional study was submitted to and approved by the Research Ethics Committee, under No. 0258.0.398.000-11. A total of 28 patients were analyzed, totaling 28 wrists operated between January 2005 and April 2015, a number determined by the calculation of the sample size made by the Laboratory of Epidemiology and Statistics of the Dante Pazzanese Institute.25 The inclusion criteria were: (1) complete medical chart data on the analyzed variables, (2) frequent outpatient follow-up and presence of pre and postoperative imaging tests, (3) acute fractures (Herbert type A or B) or pseudoarthrosis (Herbert type D1 with fibrous union),26 (4) non-dislocated or dislocation <2 mm, those capable of reduction with non-surgical maneuvers using an image intensifier, and (5) intolerance to prolonged plaster cast use. The exclusion criteria were non-compliance with the aforementioned inclusion criteria.
The surgical method was as follows: all patients underwent sedation followed by local anesthetic blockade. They were positioned in a dorsal recumbent position with the upper limb supported on a transparent auxiliary table with an image intensifier used throughout the procedure. Percutaneous fixation techniques with compression screws were used, as described in the study by Folberg et al.27
In the postoperative period, only dressings were used, without cast immobilization, and early mobilization with load restriction was authorized. The sutures were removed after 14 days, and patients participated in ten physical therapy sessions to gain range of motion.
Postoperatively, patients were objectively assessed through the modified functional criteria of Green and O’Brien,28, 29 which are based on pain, function, mobility, and strength.
Diagnostic time and consolidation time evaluations were analyzed using SPSS v.1530 software; the t-test was used, with a 5% level of significance.
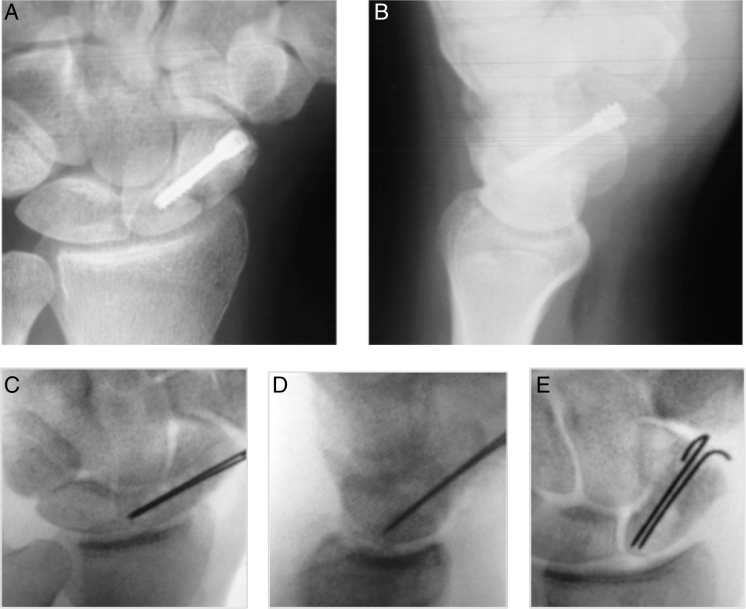
Percutaneous fixation technique for scaphoid waist fractures
The patient is placed in a supine recumbent position, and under fluoroscopy the hand is tractioned in hyperextension. This position extends the scaphoid and ulnar deviation, improving access to its distal pole (Fig. 1A and B). In most cases, longitudinal traction is sufficient to reduce the fracture (Kirschner wires can be used as joysticks to manipulate the fracture fragments to their original position in cases where traction alone is not sufficient). Once the reduction is verified by fluoroscopy, the most important step is to define the entry point of the guidewire and the position of the screw. This entry point is the scaphoid tuberosity, which can be located with a 12–14-gauge syringe needle inserted into the scaphotrapezial junction and bent to a vertical position. This needle is levered into the trapezoid and makes the distal pole of the scaphoid more radial, facilitating the insertion of the guidewire (Fig. 1C).
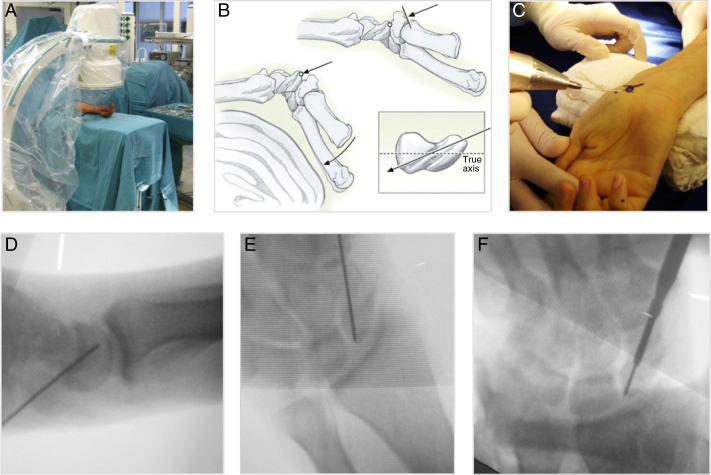
Fig. 1.
Percutaneous method for scaphoid waist fracture. A, positioning of the image intensifier regarding the hand to be operated; B, hyperextension of the wrist to visualize the entry point and the true (longitudinal) axis of the scaphoid; C, entry point of the Kirschner wire with the wrist in hyperextension; D, Kirschner wire inserted following the true axis of the scaphoid on a lateral view; E, Kirschner wire inserted following the true axis of the scaphoid, on an anteroposterior view; F, introduction of the screw following the true axis of the scaphoid.
The ideal starting point is approximately 2 mm from the vertex of the scaphoid tubercle (to achieve maximum guidewire length within the bone path). Once the direction and the entry point are confirmed, the needle is impacted into the joint, so that the fragments do not move during the passage of the guidewire. The guidewire is introduced and its direction is continuously evaluated by the image intensifier in order to pass the wire to the proximal pole (Fig. 1D and E). If the wire is in a satisfactory position, a longitudinal incision of approximately 0.5 cm is made and explored with a hemostat until the scaphoid pole. The length of the screw is determined by a gauge, and is 4–5 mm shorter to achieve the correct measurement. In rare cases, a second Kirschner wire can be applied to avoid rotation of the fragments. The needle is removed and a cannulated drill is passed through the guidewire to approximately 2 mm from the articular surface. A compression screw is passed through the guidewire and its end position is checked with the image intensifier. The incision is then closed (Fig. 1F).
Clinical case of a scaphoid waist fracture
A patient with four weeks of evolution, after a fall to the ground, presented pain at palpation of the anatomical snuffbox and with the Watson test. The fracture plane was not visible on anteroposterior and lateral radiographs of the wrist, only on a pronated oblique view (Fig. 2A–C).
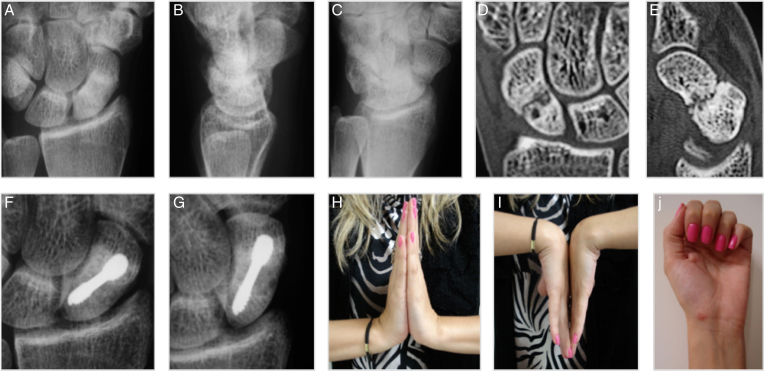
Fig. 2.
Clinical case of a scaphoid waist fracture. A, anteroposterior radiograph of the wrist; B, lateral radiograph of the wrist; C, pronated oblique radiograph of wrist; D, CT image of the wrist in coronal section; E, CT image of the wrist in sagittal section; F, anteroposterior radiograph of the wrist with seven weeks of evolution; G, anteroposterior radiograph with ulnar deviation of the wrist at seven weeks of evolution; H, complete extension; I, complete flexion; J, surgical scar.
Computed tomography (CT) images clearly show the fracture plane (Fig. 2D and E). After surgery, fracture consolidation was demonstrated at seven weeks (Fig. 2F and G). Clinical images (Fig. 2H–J).
Percutaneous fixation technique for fractures of the proximal third of the scaphoid
The patient is placed in a supine recumbent position with the arm extended on the table. The image intensifier is positioned perpendicular to the wrist. For the passing of the guidewire, after locating the central axis of the scaphoid on the anteroposterior view, the wrist should be pronated and flexed at 45 degrees or more, until the scaphoid poles are brought into line (Fig. 3A).
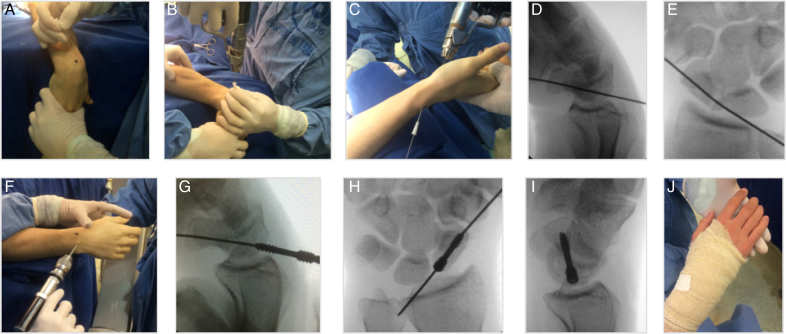
Fig. 3.
Percutaneous method for a proximal pole fracture. (A) Demarcation of the proximal pole for guidewire entry (a needle may be used for assistance); (B) guidewire introduction; (C) passing of the dorsal guidewire from dorsal to volar, so that wrist flexion occurs, facilitating screw placement; (D) lateral radiographic image of the guidewire already positioned; (E) anteroposterior radiographic image; (F) drilling of the proximal pole; (G) placement of the dorsal screw from dorsal to volar on a lateral image; (H) end of screw placement on anteroposterior (I) and lateral images; (J) dressing and elastic bandage.
A 1 mm guidewire is then introduced through a small incision in the skin toward the apex of the scaphoid (which is covered only by the dorsal capsule and subcutaneous tissue, usually with no tendons or nerves in its path), 1–2 mm radially to the scapholunate ligament insertion. A 12 or 14-gauge needle can be used to help passing the guidewire (Fig. 3B–E). If a suitable position is not achieved, a thicker guidewire can be used (1.5 mm, for example). A cannulated drill bit is introduced (Fig. 3F), and a screw 4–5 mm shorter than the measured length is used, as biomechanical studies show that the smaller the screw, the better the fixation. The final screw position and fracture compression are assessed with the image intensifier (Fig. 3G–I). Only a dressing and an elastic bandage is applied postoperatively (Fig. 3J).
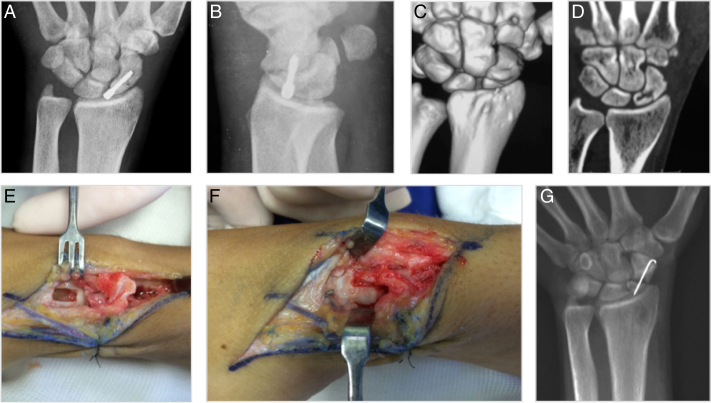
Clinical case of fracture of the proximal third of the scaphoid
A patient with three weeks of evolution, after a fall to the ground in a soccer game, presented pain at palpation of the anatomical snuffbox and with the Watson test. The anteroposterior radiograph showed the fracture plane at the proximal pole (Fig. 4A), which was confirmed by magnetic resonance imaging (MRI; Fig. 4B). Surgery was performed with percutaneous fixation using the dorsal access; at ten weeks, consolidation was demonstrated by radiographic images in anteroposterior (Fig. 4C) and lateral (Fig. 4D) views. Clinical imaging demonstrates normal healing, and normal wrist flexion and extension (Fig. 4E–G).
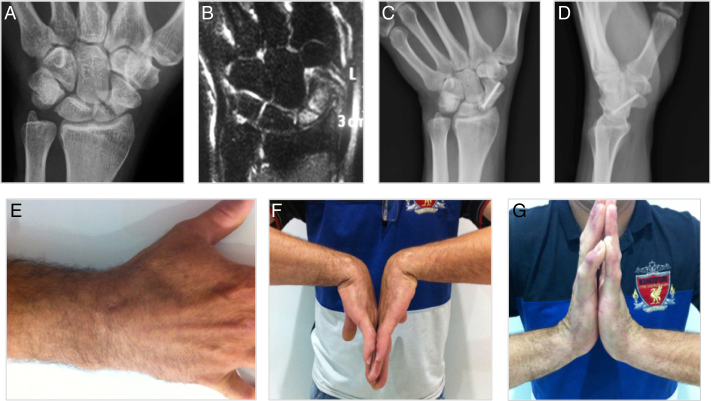
Fig. 4.
Clinical case of a proximal pole scaphoid fracture; A, anteroposterior radiograph of wrist; B, magnetic resonance imaging; C, anteroposterior radiograph, ten weeks after surgical correction; D, lateral radiograph, ten weeks after surgical correction; E, scar on the back of the wrist; F, wrist flexion; G, wrist extension.
Results
This study included 28 patients who did not present bilateral fractures and had a mean follow-up of eight weeks (ranging from 7 to 12 weeks) until fracture consolidation was confirmed. In both cases of nonunion, this follow-up was longer than 24 weeks, and a new surgical intervention was required.
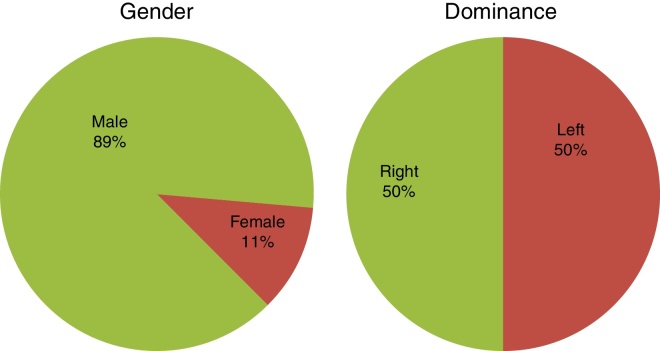
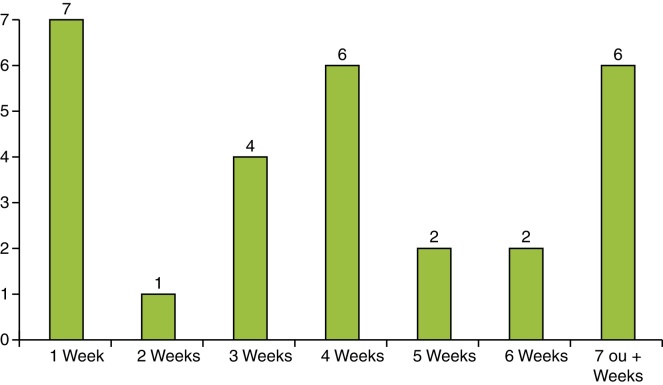
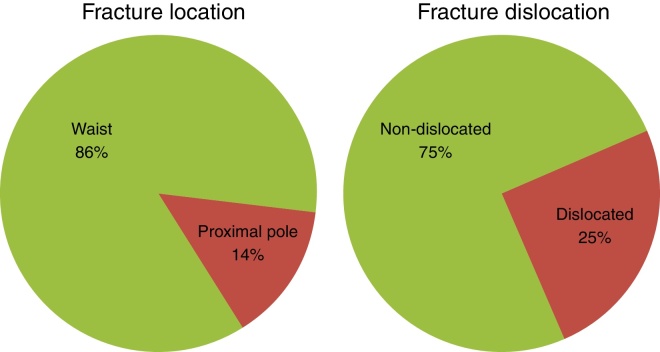
This mean age of participants was 30.5 years (range: 18–65); male prevalence was observed (25 [89.2%], with 3 females [10.8%]), with no prevalence of the dominant side (Fig. 5). The time to diagnosis was 4.16 weeks (range: 1–8 weeks; Fig. 6); however, in the three cases of fibrous union, this time was over one year. The mechanism of trauma was a fall on the wrist in 22 cases (78.5%), fracture during sports practice in five cases (17.8%), and a traffic accident in one case (3.5%). Of the total fractures, 24 cases were of the scaphoid waist (85.8%) and four were of the proximal pole (14.2%); seven cases of scaphoid waist fractures presented a dislocation of less than 2 mm (25%; Fig. 7).
Fig. 5.
Gender and dominance.
Fig. 6.
Time to diagnosis.
Fig. 7.
Fracture location and fracture dislocation.
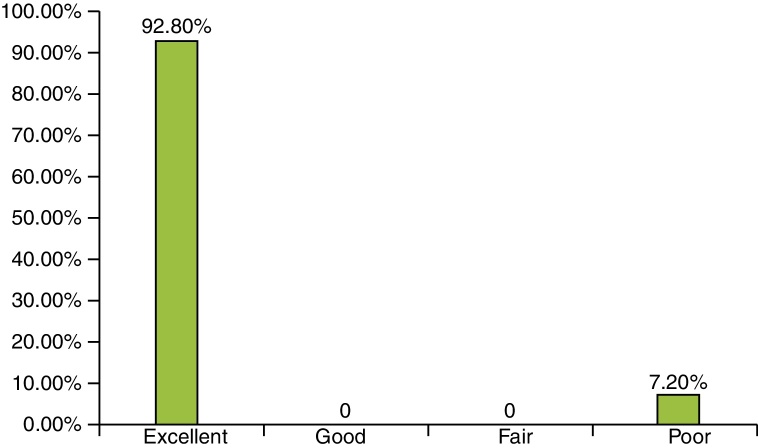
Consolidation was observed in 26 cases (92.8%), in a mean time of 7.5 weeks postoperatively. These cases presented full range of motion, and had no complaints of loss of strength or residual pain. The mean time to return to work was seven weeks, including patients with proximal pole fractures. The mean time to return to work was 5.75 days for self-employed professionals and 28.84 days for employees.
The two cases that did not present radiological union had follow-up of 24 weeks or longer. These cases persisted with dysfunction due to loss of normal range of motion, pain, and pressure strength deficit.
In the objective evaluation of patients by the functional criteria of Green and O’Brien,28, 30 26 results were considered excellent (92.8%), 0 good (0%), 0 fair (0%), and two poor (7.2%; Fig. 8).
Fig. 8.
Functional criteria of Green and O’Brien (Source: Institute of Orthopedics and Traumatology, Passo Fundo, RS, Brazil).
As complications, two patients presented nonunion, one in a case of scaphoid waist fracture (Fig. 9) and one in a case of proximal pole fracture (Fig. 10). In the case of scaphoid waist fracture, a technical failure was observed because the distal thread pitch of the compression screw did not exceed 80% of the fracture plane, so stabilization was not obtained. In the case of proximal pole fracture, a technical failure occurred because the screw head was not fully inserted into the proximal pole; stabilization was lost and consolidation was not achieved.
Fig. 9.
Scaphoid wrist fracture, showing nonunion. Patient with anatomical snuffbox pain 24 weeks after the surgical procedure. Radiographic images (A and B) showing nonunion. Images obtained through image intensifier (C–E) demonstrating new surgical intervention with the use of unstructured iliac graft and placement of two Kirschner wires. In this case, a volar approach was used.
Fig. 10.
Proximal pole scaphoid fracture showing nonunion. Patient with anatomical snuffbox pain 24 weeks after the surgical procedure. Radiographic images (A and B) showing poor screw positioning. Tomographic images (C and D) demonstrating nonunion after screw removal. A new intervention was performed, showing scaphoid excavation and elevation of the vascularized bone graft (E and F). Anteroposterior radiographic image of the wrist with ulnar deviation (G), scaphoid fixation with a Kirschner wire.
In data analysis, using SPSS software v.15,31 and the t-test, with a 5% level of significance, it was demonstrated that scaphoid waist fractures had a statistically significantly lower consolidation time (p = 0.0003) when compared with proximal pole fractures (7.65 ± 2.89 vs. 10.33 ± 0.65 weeks, respectively). The diagnostic time for waist and proximal pole fractures (3.8 ± 3.4 vs. 5.2 ± 1.6 weeks, respectively) did not differ significantly (p = 0.178; Table 1).
Table 1.
Time of consolidation and diagnosis (in weeks).
| Consolidation (weeks) | Time to diagnosis (weeks) | |
|---|---|---|
| Waist (n = 24) | 7.65 ± 2.89 | 3.8 ± 3.4 |
| Proximal pole (n = 4) | 10.33 ± 0.65 | 5.2 ± 1.6 |
| p-value | 0.0003 | 0.178 |
When comparing the dislocated fractures (<2 mm) with the non-dislocated ones, no statistically significant difference was observed regarding the time of consolidation (Table 2).
Table 2.
Consolidation time (in weeks) for dislocated and non-dislocated fractures.
| Dislocated | Consolidated (weeks) | Number |
|---|---|---|
| Yes | 22.33 ± 2.516 | 2 |
| No | 7.56 ± 0.664 | 26 |
| p-value | 0.450 |
Discussion
Scaphoid fractures continue presenting a great challenge due to their different types and methods of treatment.10, 19 In this study, it was observed that the epidemiological parameters were similar to those observed in recent literature.28, 32
According to the 28 scaphoid fractures included in this study, 92.8% presented radiological consolidation, while some authors reported 100% consolidation with the use of percutaneous fixation.31, 33, 34, 35, 36 The two cases of nonunion observed in the present study, one of the scaphoid waist and another of the proximal pole, were caused by technical failures. In the case of the scaphoid waist fracture, the distal thread pitch of the screw did not exceed 80% of the fracture plane. In the other case, a technical failure occurred because the screw head was not fully inserted into the proximal pole; stabilization was lost and consolidation was not achieved. This 92.8% consolidation rate observed in the present study is in agreement with the results by Folberg et al.27 and Brutus et al.,37 who observed a consolidation rate of 93.7% and 90%, respectively.
Regarding epidemiology, in the present study the mean age was 30.6 (18–65) years; a prevalence of males (89.2%) was observed, with no prevalence of the dominant side. As for the fracture plane, 85.7% of the cases involved the scaphoid waist and 14.3%, the proximal pole. These data are very similar to those presented in the study by Severo et al.,32 in which the mean age was 29.7 years (range: 18–55), with predominance of males (76% of cases) and the right side (54%). As for the fracture plane, 72% of the cases involved the scaphoid waist and 14%, the proximal pole.
Authors such as Vinnars et al.,19 Bond et al.,10 and Dias et al.20 indicate that the non-surgical treatment of scaphoid fracture is limited to cases of non-dislocated fractures, reaching 95%–100% of good consolidation up to 12 weeks. Furthermore, the same authors warn that treatments that prescribe nine to 12 weeks of immobilization are not free of complications, despite the good levels of bone union. This immobilization time causes muscular atrophy and a decrease in strength, leading to an increase in the degree of joint stiffness of the wrist, which in turn requires a longer rehabilitation time. Thus, Rettig and Kollias21 recommend a more aggressive treatment in cases of non-dislocated or minimally dislocated fractures, especially in athletes, high-demand workers, and patients with immobilization intolerance. Bond et al.10 reported that patients with non-dislocated scaphoid fractures randomized and treated with percutaneous screws presented a shorter consolidation time than those who underwent a conservative treatment with immobilization (seven vs. 12 weeks, respectively), as well as a shorter return to daily activities (eight vs. 15 weeks, respectively). Inoue and Shionoya,24 in their retrospective analyses of acute scaphoid fractures with a minimum follow-up of six months, demonstrated that patients treated with percutaneous screws presented fracture consolidation at six weeks vs. nine weeks, and an earlier return to work at 5.8 weeks vs. 10.2 weeks. The present results are similar with those in the literature, as consolidation was observed at a mean of 7.65 weeks for waist fractures and at 10.33 weeks for proximal pole fractures.
Regarding rehabilitation, an excellent degree of satisfaction and quality upon return to work was obtained in the present study, according to the objective criteria of Green and O’Brien28 with 92.8% excellent and 7.2% poor results. The mean time to return to work was seven weeks, including patients with proximal pole fractures, in line with the studies by Bond et al.,10 Retting and Kollias,21 and Inoue and Shionoya.24 Regarding the type of employment, the mean time to return to work was 5.75 days for self-employed professionals and 28.84 days for employees.
More comparisons about the differences between the postoperative periods, such as the use of plaster casts present in most studies, are still required, since in the present study they were not used. It is also necessary to assess the financial impact of treatment and early rehabilitation among patients treated conservatively and those who undergo percutaneous surgery.
Conclusion
Percutaneous fixation of waist and proximal scaphoid fractures with a compression screw presents good results, being a good alternative to prolonged plaster cast use. Percutaneous fixation was shown to be a good way to treat these types of fractures; despite the steep learning curve, the method is reproducible and allows early active mobility of the wrist with a low rate of complications, earlier return to work, and optimal functional results.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at Universidade Federal da Fronteira Sul (UFFS), Hospital São Vicente de Paulo (HSVP), Instituto de Ortopedia e Traumatologia, Passo Fundo, RS, Brazil.
Contributor Information
Antônio Lourenço Severo, Email: antoniolsevero@gmail.com.
Rodrigo Cattani, Email: rcattani@terra.com.br.
References
- 1.Hove L.M. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999;33(4):423–426. doi: 10.1080/02844319950159145. [DOI] [PubMed] [Google Scholar]
- 2.Gelberman R.H., Menon J. The vascularity of the scaphoid bone. J Hand Surg Am. 1980;5(5):508–513. doi: 10.1016/s0363-5023(80)80087-6. [DOI] [PubMed] [Google Scholar]
- 3.Kawamura K., Chung K.C. Treatment of scaphoid fractures and nonunions. J Hand Surg Am. 2008;33(6):988–997. doi: 10.1016/j.jhsa.2008.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osterman A.L., Mikulics M. Scaphoid nonunion. Hand Clin. 1988;4(3):437–455. [PubMed] [Google Scholar]
- 5.Wong K., von Schroeder H.P. Delays and poor management of scaphoid fractures: factors contributing to nonunion. J Hand Surg Am. 2011;36(9):1471–1474. doi: 10.1016/j.jhsa.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Pao V.S., Chang J. Scaphoid nonunion: diagnosis and treatment. Plast Reconstr Surg. 2003;112(6):1666–1676. doi: 10.1097/01.PRS.0000086090.43085.66. [DOI] [PubMed] [Google Scholar]
- 7.Mack G.R., Bosse M.J., Gelberman R.H., Yu E. The natural history of scaphoid non-union. J Bone Joint Surg Am. 1984;66(4):504–509. [PubMed] [Google Scholar]
- 8.Ruby L.K., Stinson J., Belsky M.R. The natural history of scaphoid non-union. A review of fifty-five cases. J Bone Joint Surg Am. 1985;67(3):428–432. [PubMed] [Google Scholar]
- 9.Gellman H., Caputo R.J., Carter V., Aboulafia A., McKay M. Comparison of short and long thumb-spica casts for non-displaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989;71(3):354–357. [PubMed] [Google Scholar]
- 10.Bond C.D., Shin A.Y., McBride M.T., Dao K.D. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83(4):483–488. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Brånemark P.I., Lindström J., Hallén O., Breine U., Jeppson P.H., Ohman A. Reconstruction of the defective mandible. Scand J Plast Reconstr Surg. 1975;9(2):116–128. doi: 10.3109/02844317509022776. [DOI] [PubMed] [Google Scholar]
- 12.Mayfield J.K., Johnson R.P., Kilcoyne R.K. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5(3):226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 13.Eddeland A., Eiken O., Hellgren E., Ohlsson N.M. Fractures of the scaphoid. Scand J Plast Reconstr Surg. 1975;9:234–239. doi: 10.3109/02844317509022872. [DOI] [PubMed] [Google Scholar]
- 14.Cooney W.P., Dobyns J.H., Linscheid R.L. Nonunion of the scaphoid: analysis of the results from bone grafting. J Hand Surg Am. 1980;5(4):343–354. doi: 10.1016/s0363-5023(80)80173-0. [DOI] [PubMed] [Google Scholar]
- 15.Szabo R.M., Manske D. Displaced fractures of the scaphoid. Clin Orthop Relat Res. 1988;(230):30–38. [PubMed] [Google Scholar]
- 16.Leslie B.M., O’Malley M., Thibodeau A.A. A forty-three-year follow-up of a vitallium scaphoid arthroplasty. J Hand Surg Am. 1991;16(3):465–468. doi: 10.1016/0363-5023(91)90015-4. [DOI] [PubMed] [Google Scholar]
- 17.Moritomo H., Viegas S.F., Nakamura K., Dasilva M.F., Patterson R.M. The scaphotrapezio-trapezoidal joint. Part 1: An anatomic and radiographic study. J Hand Surg Am. 2000;25(5):899–910. doi: 10.1053/jhsu.2000.4582. [DOI] [PubMed] [Google Scholar]
- 18.Capo J.T., Orillaza N.S., Jr., Slade J.F., 3rd. Percutaneous management of scaphoid nonunions. Tech Hand Up Extrem Surg. 2009;13(1):23–29. doi: 10.1097/BTH.0b013e3181877644. [DOI] [PubMed] [Google Scholar]
- 19.Vinnars B., Pietreanu M., Bodestedt A., Ekenstam F.A., Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures. A randomized clinical trial. J Bone Joint Surg Am. 2008;90(6):1176–1185. doi: 10.2106/JBJS.G.00673. [DOI] [PubMed] [Google Scholar]
- 20.Dias J.J., Wildin C.J., Bhowal B., Thompson J.R. Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am. 2005;87(10):2160–2168. doi: 10.2106/JBJS.D.02305. [DOI] [PubMed] [Google Scholar]
- 21.Rettig A.C., Kollias S.C. Internal fixation of acute stable scaphoid fractures in the athlete. Am J Sports Med. 1996;24(2):182–186. doi: 10.1177/036354659602400211. [DOI] [PubMed] [Google Scholar]
- 22.Wozasek G.E., Moser K.D. Percutaneous screw fixation for fractures of the scaphoid. J Bone Joint Surg Br. 1991;73(1):138–142. doi: 10.1302/0301-620X.73B1.1670499. [DOI] [PubMed] [Google Scholar]
- 23.Jeon I.H., Oh C.W., Park B.C., Ihn J.C., Kim P.T. Minimal invasive percutaneous Herbert screw fixation in acute unstable scaphoid fracture. Hand Surg. 2003;8(2):213–218. doi: 10.1142/s0218810403001807. [DOI] [PubMed] [Google Scholar]
- 24.Inoue G., Shionoya K. Herbert screw fixation by limited access for acute fractures of the scaphoid. J Bone Joint Surg Br. 1997;79(3):418–421. doi: 10.1302/0301-620x.79b3.7254. [DOI] [PubMed] [Google Scholar]
- 25.Laboratorio de Estatística e Epidemiologia do Dante Pazzanese. Tamanho de amostra para pesquisa em ciências da saúde. Disponível em: http://lee.dante.br/pesquisa/amostragem/amostra.html
- 26.Amadio P.C., Moran S.L. Fractures of the carpal bones. In: Green D.P., Hotchkiss R.N., Pederson W.C., Wolfe S.W., editors. Green's operative hand surgery. 5th ed. Elsevier; Philadelphia: 2005. pp. 711–768. [Google Scholar]
- 27.Folberg C.R., Ruschel P.H., Pignataro M.B. Fixação percutânea das fraturas de terço médio de escafoide. Rev Bras Ortop. 2004;39(7):363–370. [Google Scholar]
- 28.Green D.P., O’Brien E.T. Open reduction of carpal dislocations: indications and operative techniques. J Hand Surg Am. 1978;3(3):250–265. doi: 10.1016/s0363-5023(78)80089-6. [DOI] [PubMed] [Google Scholar]
- 29.Severo A.L., Mentz L., Busetto M.A., Lech O., Pinto S. Fraturas da extremidade distal do rádio tratadas pela técnica de Ulson. Rev Bras Ortop. 2003;38(8):437–445. [Google Scholar]
- 30.SPSS Inc.; Chicago: 2006. Statistical Package for the Social Sciences (SPSS). Version 15.0. Computer program. [Google Scholar]
- 31.Haddad F.S., Goddard N.J. Acute percutaneous scaphoid fixation. A pilot study. J Bone Joint Surg Br. 1998;80(1):95–99. doi: 10.1302/0301-620x.80b1.8076. [DOI] [PubMed] [Google Scholar]
- 32.Severo A.L., Dall Bosco A., Lech O.C. Scaphoid fracture: a preliminary epidemiological study. Rev Med Cienc Saúde. 2014;39(1):52–55. [Google Scholar]
- 33.Ring D., Jupiter J.B., Herndon J.H. Acute fractures of the scaphoid. J Am Acad Orthop Surg. 2000;8(4):225–231. doi: 10.5435/00124635-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Slade J.F., 3rd, Gutow A.P., Geissler W.B. Percutaneous internal fixation of scaphoid fractures via an arthroscopically assisted dorsal approach. J Bone Joint Surg Am. 2002;84(Suppl. 2):21–36. doi: 10.2106/00004623-200200002-00003. [DOI] [PubMed] [Google Scholar]
- 35.Slade J.F., 3rd, Jaskwhich D. Percutaneous fixation of scaphoid fractures. Hand Clin. 2001;17(4):553–574. [PubMed] [Google Scholar]
- 36.Ledoux P., Chahidi N., Moermans J.P., Kinnen L. Percutaneous Herbert screw osteosynthesis of the scaphoid bone. Acta Orthop Belg. 1995;61(1):43–47. [PubMed] [Google Scholar]
- 37.Brutus J.P., Baeten Y., Chahidi N., Kinnen L., Moermans J.P., Ledoux P. Percutaneous Herbert screw fixation for fractures of the scaphoid: review of 30 cases. Chir Main. 2002;21(6):350–354. doi: 10.1016/s1297-3203(02)00138-5. [DOI] [PubMed] [Google Scholar]