Abstract
Objective
The current study aims at a functional analysis of trans-olecranon lateral pinning for displaced supracondylar fracture of the humerus (SCFH) in children.
Methods
A prospective study of 48 children (30 males, 18 females; mean age: 7.4 years) with displaced SCFH was treated at this institution with modified technique from March 2011 to September 2014. Cases were selected on the basis of inclusion criteria. The functional outcome was assessed clinically by modified Flynn's criteria along with achievement of full range of motion.
Results
All 48 children with a mean follow up of 20 months (range: 6–26 months) were assessed. All fractures united well. With modified Flynn's criteria, results were excellent in 40 children (83.3%), good in six children (12.5%), and fair in two children (4.2%). There were no poor results. Preoperative nerve palsies seen in four children recovered at ten weeks. Full range of motion was achieved on an average of 20 days after K-wire removal and no new post-operative nerve palsies were noted.
Conclusion
The modified trans-olecranon fossa four-cortex purchase (TOF-FCP) technique was promising in all cases of unstable SCFH without the complications of loss of reduction or iatrogenic ulnar nerve injury. This technique is simple, safe, and reproducible, with good clinical results in this type of fracture.
Keywords: Humeral fractures; Fracture fixation, internal; Olecranon process/injuries; Child
Resumo
Objetivo
O presente estudo teve como objetivo analisar funcionamente a fixação lateral através da fossa olecraniana em fraturas supracondilianas deslocadas do úmero (FSDU) em crianças.
Métodos
Estudo prospectivo de 48 crianças (30 do sexo masculino, 18 do sexo feminino, idade média: 7,4 anos) com FSDU, tratados nesta instituição entre março de 2011 e setembro de 2014 usando uma técnica modificada. Os casos foram selecionados com base em critérios de inclusão. O resultado funcional foi avaliado clinicamente pelos critérios de Flynn modificados, juntamente com a realização da amplitude de movimento completa.
Resultados
Todas as 48 crianças foram avaliadas, com seguimento médio de 20 meses (intervalo: 6 a 26 meses). Todas as fraturas apresentaram boa união. De acordo com os critérios de Flynn modificados, os resultados foram excelentes em 40 crianças (83,3%), bons em seis (12,5%) e razoáveis em duas (4,2%). Não foram observados resultados ruins. As paralisias nervosas pré-operatórias observadas em quatro crianças se resolveram após dez semanas. Os pacientes alcançaram amplitude completa de movimento em uma média de 20 dias após a remoção dos fios de Kirschner e não foram observadas novas paralisias nervosas pós-operatórias.
Conclusão
A técnica modificada de fixação em quatro corticais através da fossa trans-oleocraniana (FQC-FTO) foi promissora em todos os casos de FSDU instável, não apresentando complicações de perda de redução ou lesão do nervo ulnar iatrogênico. A técnica é simples, segura e reprodutível, com bons resultados clínicos nesse tipo de fratura.
Palavras-chave: Fraturas do úmero; Fixação de fraturas, interna; Processo olecraniano, lesões; Criança
Introduction
Supracondylar fractures of humerus (SCFH) represent 50–70% of all elbow fractures in children during first decade of life.1 The non-operative management of unstable SCFH including Dunlop skin traction, skeletal traction and cast application has historically been associated with a greater incidence of failure to obtain and maintain fracture reduction as well as carries higher complication rates.
Current preferred method of treatment for displaced pediatric SCFH has been closed reduction and percutaneous pin fixation which has given excellent results as reported by various authors.2, 3, 4 Among this, a continuous debate persists between cross pinning (lateral and medial K wires) and lateral only pinning (LOP). Medial pinning carries risk of iatrogenic ulnar nerve injury whereas lateral only pinning is blamed for its instability.5, 6, 7, 8, 9
Lateral only pinning may result in rotationally unstable fixation causing varus collapse and cubitus varus deformity along with additional medial comminution at the fracture site.9 Biomechanical studies have shown that chances of rotational loss of reduction in conventional lateral only constructs are high compared with cross pinning, indicating that cross pinning has greater torsional stability.10
In our study, we modified the standard two parallel LOP technique to make it a more stable construct by achieving a trans-olecranon fossa four cortical purchase, so that this technique can be used universally in all pediatric displaced SCFH including for unstable fracture patterns.
Methods and materials
Following clearance from Institutional Ethical Committee, 48 prospective children with displaced SCFH were included in our study during the period from March 2011 to September 2014.
Gartland classification was used to categorize the fractures. Willkins modification was applied to Gartland Type II subclassifying them into type A in which posterior cortex was intact with anterior humeral line passing through capitellum and type B with anterior humeral line passing anterior to capitellum with rotated distal fragment. Gartland Type III fractures were also classified as Type A (postero medial displacement) and Type B (postero lateral displacement).
Inclusion criteria
All closed type IIB and type III Gartland SCFH between age group of 3–14 years, within seven days of injury were included in the study. Children with pre-operative nerve injuries as well as pulseless pink limb were also included.
Exclusion criteria
Gartland type I and type II A, open fractures and fractures with compartment syndrome or vascular injury demanding repair were excluded.
Immediately after the patients’ arrival to the hospital a detailed clinical examination including a thorough neurovascular assessment was carried out. Standard anteroposterior and lateral radiographs of the involved elbow were taken and the fracture type was identified following which surgery was performed after obtaining informed written consent from parents or caregivers.
Operative technique
Under appropriate anesthesia, closed reduction of the fractures was done. Manual traction was given to the limb with elbow at 20° flexion to correct the medio-lateral displacement (coronal alignment) and rotation. The distal fragment “milking” was done with both thumbs of the operating surgeon on the flexed elbow of the patient leading to correction of the posterior displacement (sagittal alignment). The reduction was checked under image intensifier. Reduction was considered “acceptable” with the following criteria fulfilled: no step on medial and lateral columns and normal orientation of olecrenon fossa in the antero-posterior (AP) view, tear drop restoration and 40° anterior tilt of capitellum in the lateral view. Once satisfactory reduction was achieved, the forearm was strapped to arm with maximum possible flexion and pronation to secure the achieved reduction.
The elbow was then painted and draped. The first K wire was passed from tip of lateral epicondyle at an angle of 45°–55° directing superiorly and medially in the AP view of image intensifier. After advancing few millimeters starting from the lateral cortex, the wire position was checked in the lateral view, to confirm its position in the center of humerus. The wire was then advanced above the olecranon fossa up to medial cortex in standard fashion.
The second K wire was introduced exactly parallel and one cm inferior to the first wire and, it was confirmed that this wire passes through lateral cortex, two walls of olecranon fossa, and medial cortex in proximal fragment (four cortices in total). In this modality, as the wire was passed through the four cortices; we call it as Trans olecranon fossa four cortex purchase (TOF-FCP) technique. This K wire generally gets started from the capitellum of involved elbow. The representation of this technique in bone model is shown in Fig. 1. Third wire was added wherever needed, with the same technique, either between the previously placed two wires, or below the second wire.
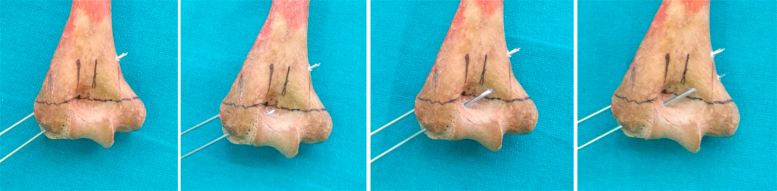
Figure 1.
Bone model representation of trans-olecranon fossa four cortex purchase technique.
The image intensifier (not the child's arm) was rotated for the AP and lateral views throughout the procedure. After adequate fixation from minimum of two pins (six cortices purchase) to maximum of three pins (ten cortices purchase), strapping was removed. The elbow was rotated and stability was confirmed. The K wires were bent and cut outside the skin leaving one centimeter. A well padded posterior splint was applied with elbow in 60°–90° of flexion as tolerated. Immediately in the post-operative period after recovery from the anesthesia effect, the neurovascular status of the limb was assessed.
Radiographs of the operated elbow were taken before discharge and assessed for quality of reduction by Baumann's and humero-capitellar angles. The children were discharged from the hospital on the same day or the following day. The children were kept under weekly follow-up for pin tract assessment and plaster care for one month. Radiographs were taken after 4 weeks in children less than seven years and five weeks in children more than seven years, to assess the fracture healing. After radiological union, wires were removed as an out-patient procedure. Child was encouraged for gradual mobilization exercises and physiotherapy was advised, till elbow full range of movement was regained.
Carrying angle was measured using goniometer once the patient achieved full elbow extension. The Baumann's angle, humero-capitellar angle was measured from the radiographs taken at that time.
Results
Among 48 children enrolled in the study, there were 30 boys and 18 girls. The age ranged from three to 14 years (mean – 7.4 years). Injury was right sided in 26 children and left sided in 22 children. On basis of Gartlands classification we had 12 children of type II B and 36 children of type III fracture pattern. The mean follow up period was 20 months (range 6–26 months).
Pre-operatively, four patients had clinical signs of nerve injury, two involving median nerve and two involving radial nerve. There was no case with preoperative ulnar nerve injury. Absent radial pulse with pink limb was seen in four children. Three children presented with associated injuries of which, two with ipsilateral fracture of distal end radius, one with associated fracture of proximal end of ulna.
The time duration between injury and surgery was from 2 to 12 h in 37 cases (77%) and more than 12 h in 11 cases (23%). Upper limit of delay was seven days. We could achieve closed reduction in all cases except two patients (0.5%). The first patient with a highly displaced type III fracture had disappearance of radial pulse during reduction. The second patient, a satisfactory closed reduction could not be achieved even after multiple attempts. In both cases, open reduction were performed through posterior approach and fixation was done with same two parallel lateral pins with TOF-FCP technique. In first patient, flexion of swollen elbow with imperfect reduction could have contributed to disappearance of radial pulse. After open reduction and fixation, radial pulse was felt well. In second patient, there was brachialis muscle interposition that prevented closed reduction.
Size of 1.5 mm K wires were used in children less than four years, 1.8 mm K wires in children between four and ten years and a combination of 2 mm and 1.8 mm K wires were used in children older than ten years. Two K wires were used in 28 children and three K wires in 20 children. The mean duration of procedure was 18 min (range 15–25 min). The procedure start time was at the onset of closed reduction and the end time was after the completion of pinning. Among 48 patients, 38 were discharged after 24 h of observation following surgery. Ten patients with limb edema were kept under observation for two to three days.
On follow up, all fractures united. Two children developed superficial pin tract infection, which healed with local wound care and oral antibiotics. There was no pin migration or breakage. K wires were removed at 4 weeks in 20 cases and at 5 weeks in 28 cases. Average timing of regaining full range of movement after K wires removal was 20 days (range 10–30 days).
At one month follow-up, X-ray was taken, Baumann's angle, humero-capitellar angle were measured and compared with the immediate post operative measurements. Radiograph of normal elbow taken and compared with the injured side. A variation of 5° in Baumann's angle between injured and uninjured side was seen in 40 children with near acceptable change in six children. Two patients showed significant change in Baumann's angle with clinical cubitus valgus deformity. There was no cubitus varus deformity.
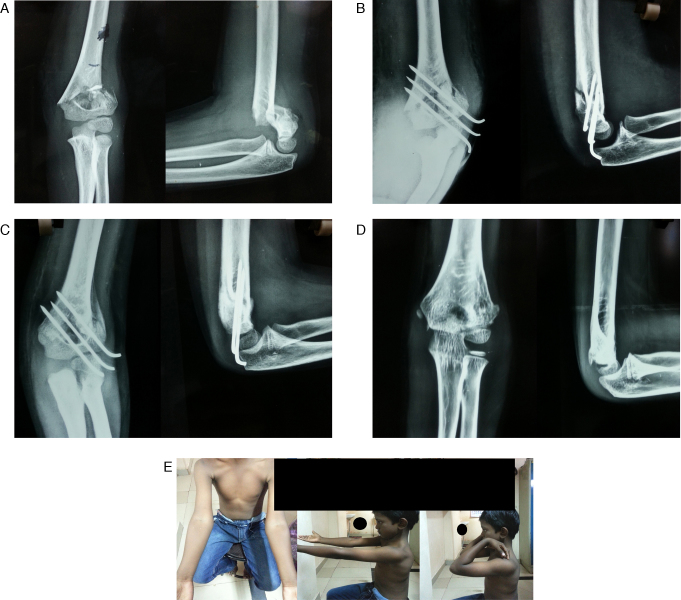
On evaluation by Flynn's criteria (Table 1) at the final follow up,11 the clinical result was excellent in 40 children (Fig. 2A–E), good in six children (Fig. 3A–D) and fair in two children. There were no poor results. Irrespective of the Gartland fracture type, most patients had excellent results (Table 2, Table 3).
Table 1.
Clinical evaluation – Flynn criteria.
| Results | Rating | Cosmetic factor: loss of carrying angle | Functional factor: loss of motion |
|---|---|---|---|
| Satisfactory | Excellent | 0–5° | 0–5° |
| Good | 6–10° | 6–10° | |
| Fair | 11–15° | 11–15° | |
| Unsatisfactory | Poor | >15° | >15° |
Figure 2.
(A) Pre-operative radiographs of 6 year old supracondylar fracture with lateral obliquity; (B) immediate post-operative radiograph showing satisfactory reduction; (C) 4 weeks follow-up radiograph showing good radiological bony union; (D) excellent radiological bony union at 10 months follow-up radiographs after pin removal; (E) clinical picture showing full range of motion with excellent rating on Flynn's criteria.
Figure 3.
(A) Pre-operative AP and lateral radiographs of 8 year old boy; (B) immediate post-operative radiograph with good reduction; (C) four weeks post-op radiograph showing good bony union; (D) clinical picture showing excellent range of motion with good rating on Flynn's criteria.
Table 2.
Final clinical results.
| Gartland fracture pattern | Treatment | Functional |
Cosmetic |
Overall |
Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| E | G | F | E | G | F | E | G | F | |||
| Type II (12) | Percutaneous pinning | 10 | 2 | 10 | 2 | 10 | 2 | 12 | |||
| Type III (34) | Percutaneous pinning | 30 | 4 | 26 | 6 | 2 | 28 | 4 | 2 | 34 | |
| Type III (2) | ORIF | 2 | 2 | 2 | 2 | ||||||
| 40 | 6 | 2 | 48 | ||||||||
E, excellent; G, good; F, fair; ORIF, open reduction internal fixation.
Table 3.
Deviation of radiographic elbow angles after surgery (compared to preoperative).
| Angle | Acceptable deviation | Abnormal deviations | ||
|---|---|---|---|---|
| Baumann angle | Angle | ±5° | −5 to −10 | >−10° |
| No of cases | 40 | 6 | 2 | |
| Humero capitellar angle | Angle | ±5° | >−5° | |
| No of cases | 36 | 12 | ||
Negative angle for Baumann's indicates valgus, and for humero-capitellar indicates extension, Positive angle for Baumann's indicates varus, and for humero-capitellar indicates flexion.
Discussion
The prime aim in management of the displaced supracondylar fracture is to reduce and immobilize the fracture to cutdown its morbidity. Management of displaced supracondylar fractures by closed reduction and percutaneous pin fixation has given consistently good results. However, controversy persists regarding the cross pinning involving medial and lateral pinning and lateral only pinning (LOP).
Lee et al. and Zionts et al. reported greater torsional rigidity with medial and lateral entry than the LOP fixation.12, 13 However, the cross pinning has the disadvantage of iatrogenic ulnar nerve palsy caused by the medial pin. The ulnar nerve injury by the medial wire can be caused by either direct injury, contusion or stretching of nerve.14, 15, 6, 16 In a meta-analysis involving 1615 supracondylar fractures in which 837 children had cross pinning and 778 children had LOP, the risk of iatrogenic ulnar nerve injury was reported 4.3 times higher in cross pinning compared with LOP.17
Lee designed a decision analysis model containing the probability of iatrogenic ulnar nerve injury in medial pinning and malunion caused by presumed unstable fixation of LOP. The functional results were evaluated using the McBride disability evaluation. Considering the facts that the iatrogenic ulnar nerve injury after medial pinning can be irreversible, whereas malunion is correctable, the authors recommended LOP for SCFH.18
The ultimate aim of the SCFH fixation therefore is to get a stable fixation without the risk of iatrogenic ulnar nerve injury. This could be achieved using a modified LOP technique than the normal method. The modified technique used in this study consisted of minimum two or more lateral wires passing through the olecranon fossa and getting four cortical purchases. This configuration was first described by Judet France as early as 1947.19
The study of 124 cases of lateral pinning by Skaggs et al. revolutionized the usage of LOP in these fractures. In their study, lateral entry pin alone was effective for even the most unstable supracondylar fractures.2, 4 There were no iatrogenic ulnar nerve injuries and no reduction was lost. They emphasized the technical points for LOP fixation as follows: (1) maximize separation of pins at fracture site; (2) engage medial and lateral column proximal to fracture; (3) engage sufficient bone in both proximal and distal fragment; (4) maintain a low threshold for use of a third lateral entry pin if there is concern about fracture stability. This can be accomplished by dividing the fracture into three columns in AP view and confirming fixation of both medial and lateral column.20
Gottschalk et al. compared two types of starting points in lateral pinning in distal humerus fracture settings in their biomechanical study: in group one, both wires entered through lateral epicondyle and in group two, one wire entered through lateral epicondyle and one through the capitellum. Results showed that the capitellar group had greater stiffness in rotations. The authors concluded that at least one wire should have capitellar starting point for improving stability.21
Balakumar et al. analyzed the factors associated with loss of reduction in pediatric SCFH treated with percutaneous pinning. They reported loss of reduction in 14 out of 77 cases (18.2%). Reduction was lost in 10 out of 29 children (34.5%) who underwent LOP fixation and 4 out of 48 (8.3%) children who had cross pinning fixation. They attributed the high rate of loss of reduction in LOP group to technical errors like insufficient purchase by the pins or reduced spread of the pins.9
Anmol Sharma et al. used Trans olecranon pinning in 30 children among a total of 90 patients who underwent percutaneous pinning for SCFH. This Trans olecranon pinning technique was completely different from our technique. The pin was passed vertically in transarticular fashion. In their results, elbow stiffness was seen in six and cubitus varus deformity in six patients.22 In our study, children developed neither elbow stiffness nor cubitus varus deformity.
In our study, although there were variations in Baumann's angle and humero-capitellar angle compared to the normal and injured side, there were no changes in the angle compared to the immediate postoperative and final follow-up radiograph. This suggests that there were minor malreduction at the time of surgery but no loss of reduction in the postoperative period. The TOF–FCP fixation was stable enough to hold the fracture throughout the period of healing.
The TOF–FCP technique has got a small learning curve. If the starting point is not central in the lateral epicondyle, single cortex of olecranon fossa can be missed. To avoid this, the central position of the starting point has to be ensured in lateral view of image intensifier before driving further. We added third wire whenever possible, particularly in older children and in the lateral oblique fracture pattern, where adequate space was available for the third wire.
In our clinical study, out of 48 cases 95% showed excellent and good results which is similar to the results of Mazda et al., study of 116 cases.3 While they had 4% poor results, we had none. However the incidence of open reduction was 26% in their study compared to 0.5% of the current study making our study superior to others. Associated injuries were seen in three children (5%) (two distal radius fractures, one proximal ulna fracture) as opposed to 1% incidence in vast review of literature.23 However, these fractures had uneventful bony union and they have not altered the final functional outcomes of our study.
The advantages of our study were that we had a good sample size and an adequate follow up. No comparison with other types of lateral pinning or cross pinning turned to be our limitation. Furthermore, large randomized controlled clinical trial between cross pinning and lateral TOF-FCP is warranted to prove the novelty of our modified LOP technique in future.
Conclusion
Use of lateral K wires with Trans olecranon fossa four cortex purchase technique was effective in displaced pediatric supracondylar fractures of humerus. This technique can be successfully employed even in comminuted and unstable fracture patterns without the fear of loss of reduction and risk of iatrogenic ulnar nerve injury. It is a safe, reliable and reproducible technique providing excellent to good clinical results with improved stability.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work performed in the KS Hospital and Vinayaka Missions Medical College and Hospital, Department of Orthopedics, Karaikal, India.
References
- 1.Wilkins K.E., Aroojis A.J. Incidence of fractures in children. In: Beaty J.H., Kasser J.R., editors. Rockwood and Wilkins’ fractures in children. 6th ed. Lippincott Williams and Wilkins; Philadelphia: 2005. pp. 10–11. [Google Scholar]
- 2.Skaggs D.L., Cluck M.W., Mostofi A., Flynn J.M., Kay R.M. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004;86(4):702–707. doi: 10.2106/00004623-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Mazda K., Boggione C., Fitoussi F., Penneçot G.F. Systematic pinning of displaced extension-type supracondylar fractures of the humerus in children. A prospective study of 116 consecutive patients. J Bone Joint Surg Br. 2001;83(6):888–893. doi: 10.1302/0301-620x.83b6.11544. [DOI] [PubMed] [Google Scholar]
- 4.Skaggs D.L., Hale J.M., Bassett J., Kaminsky C., Kay R.M., Tolo V.T. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001;83(5):735–740. [PubMed] [Google Scholar]
- 5.Belhan O., Karakurt L., Ozdemir H., Yilmaz E., Kaya M., Serin E. Dynamics of the ulnar nerve after percutaneous pinning of supracondylar humeral fractures in children. J Pediatr Orthop B. 2009;18(1):29–33. doi: 10.1097/BPB.0b013e32831960fa. [DOI] [PubMed] [Google Scholar]
- 6.Brown I.C., Zinar D.M. Traumatic and iatrogenic neurological complications after supracondylar humerus fractures in children. J Pediatr Orthop. 1995;15(4):440–443. doi: 10.1097/01241398-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Lyons J.P., Ashley E., Hoffer M.M. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children's elbows. J Pediatr Orthop. 1998;18(1):43–45. [PubMed] [Google Scholar]
- 8.Nagda T., Dhamele J., Pishin C. controversial issues in closed reduction and percutaneous pinning of supracondylar fractures of humerus in children. Int J Paediatr Orthop. 2015;1(1):11–15. [Google Scholar]
- 9.Balakumar B., Madhuri V. A retrospective analysis of loss of reduction in operated supracondylar humerus fractures. Indian J Orthop. 2012;46(6):690–697. doi: 10.4103/0019-5413.104219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee S.S., Mahar A.T., Miesen D., Newton P.O. Displaced paediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Paediatr Orthop. 2002;22(4):440–443. [PubMed] [Google Scholar]
- 11.Flynn J.C., Matthews J.G., Benoit R.L. Blind pinning of displaced supracondylar fractures of the humerus in children: sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. 1974;56(2):263–272. [PubMed] [Google Scholar]
- 12.Lee S.S., Mahar A.T., Miesen D., Newton P.O. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002;22(4):440–443. [PubMed] [Google Scholar]
- 13.Zionts L.E., McKellop H.A., Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994;76(2):253–256. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Royce R.O., Dutkowsky J.P., Kasser J.R., Rand F.R. Neurologic complications after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop. 1991;11(2):191–194. doi: 10.1097/01241398-199103000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Topping R.E., Blanco J.S., Davis T.J. Clinical evaluation of crossed-pin versus lateral-pin fixation in displaced supracondylar humerus fractures. J Pediatr Orthop. 1995;15(4):435–439. doi: 10.1097/01241398-199507000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Ikram M.A. Ulnar nerve palsy: a complication following percutaneous fixation of supracondylar fractures of the humerus in children. Injury. 1996;27(5):303–305. doi: 10.1016/0020-1383(96)00013-7. [DOI] [PubMed] [Google Scholar]
- 17.Woratanarat P., Angsanuntsukh C., Rattanasiri S., Attia J., Woratanarat T., Thakkinstian A. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma. 2012;26(1):48–53. doi: 10.1097/BOT.0b013e3182143de0. [DOI] [PubMed] [Google Scholar]
- 18.Lee K.M., Chung C.Y., Gwon D.K., Sung K.H., Kim T.W., Choi I.H. Medial and lateral crossed pinning versus lateral pinning for supracondylar fractures of the humerus in children: decision analysis. J Pediatr Orthop. 2012;32(2):131–138. doi: 10.1097/BPO.0b013e3182471931. [DOI] [PubMed] [Google Scholar]
- 19.Judet J. Traitement des fractures ´epiphysaires de l’enfant par broche trans-articulaire. Mem Acad Chir. 1947;73(27–28):562–566. [PubMed] [Google Scholar]
- 20.Herring J.A. Tachdjian's pediatric orthopaedics. 5th ed. W.B. Saunders; Philadelphia: 2014. Upper extremity injuries; p. 1278. [Google Scholar]
- 21.Gottschalk H.P., Sagoo D., Glaser D., Doan J., Edmonds E.W., Schlechter J. Biomechanical analysis of pin placement for pediatric supracondylar humerus fractures: does starting point, pin size, and number matter? J Pediatr Orthop. 2012;32(5):445–451. doi: 10.1097/BPO.0b013e318257d1cd. [DOI] [PubMed] [Google Scholar]
- 22.Sharma A., walia J.P., Brar B.S., Sethi S. Early results of displaced supracondylar fractures of humerus in children treated by closed reduction and percutaneous pinning. Indian J Orthop. 2015;49(5):529–535. doi: 10.4103/0019-5413.164039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Powell R.S., Bowe J.A. Ipsilateral supracondylar humerus fracture and Monteggia lesion: a case report. J Orthop Trauma. 2002;16(10):737–740. doi: 10.1097/00005131-200211000-00010. [DOI] [PubMed] [Google Scholar]